Abstract
Purpose
Maternal schizophrenia is associated with adverse birth outcomes, but the reasons for this remain unclear. In a population-based cohort of infants born to women with schizophrenia, we determined the occurrence of key perinatal outcomes and explored whether factors identifiable in our datasets explained any elevated risk.
Methods
Using population-level health administrative data linked to clinical birth-registry data in Ontario, Canada (2006–2011), we examined the relative risk (RR) of preterm birth (< 37 weeks), small for gestational age (SGA), and Apgar scores < 8 in infants of women with schizophrenia (n = 4279) versus infants of unaffected women (n = 286,147). Generalized estimating equations determined whether reproductive history, maternal health conditions, pregnancy exposures, and complications explained elevated RRs.
Results
Among infants of women with schizophrenia, risk was higher for prematurity (11.4% vs. 6.9%, aRR 1.64, 95% CI 1.51–1.79), SGA (3.5% vs. 2.5%, aRR 1.40, 95% CI 1.20–1.64), and Apgar score < 8 at 1 (19.0% vs. 12.8%, aRR 1.49, 95% CI 1.40–1.59) and 5 min (5.6% vs. 3.0%, aRR 1.90, 95% CI 1.68–2.16). Smoking, fourfold more common among women with schizophrenia, was the variable that explained the greatest proportion of the elevated aRR for prematurity (9.9%), SGA (28.7%), and Apgar < 8 at 1 and 5 min (9.8%, 5.6%). Illicit substance use, certain reproductive history variables, and pregnancy complications also contributed to the elevated aRR for preterm birth.
Conclusions
Elevated risks of preterm birth, SGA, and low Apgar scores in infants of women with schizophrenia are partly explained by potentially modifiable factors such as smoking and illicit drug use, suggesting opportunities for targeted intervention.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Infants born to women with schizophrenia are at high risk of several adverse perinatal outcomes, including preterm, small for gestational age, and other serious neonatal morbidities implicated as markers for chronic diseases across the lifespan [1,2,3]. Schizophrenia has a population prevalence of about 1%, and many women with the illness become new mothers, signalling that this issue has both clinical and public health implications [4, 5]. Unfortunately, the mechanisms driving the relation between maternal schizophrenia and these adverse perinatal outcomes are not well understood. So, targeted interventions to improve outcomes have not been developed.
Risk factors for poor perinatal outcomes in schizophrenia include maternal poverty, smoking, and substance use; women with schizophrenia may also be less likely to receive optimal antenatal care, especially when untreated [1,2,3, 6,7,8]. Maternal psychiatric symptoms may impact foetal development, as can medications used to treat the illness [9,10,11]. Most epidemiological research focused on pregnant women with schizophrenia has lacked detailed information on factors such as smoking, substance use, and other potentially modifiable risk factors that could be mediating risk of adverse perinatal outcomes. More knowledge in this area would inform the development of targeted interventions for this high-risk group.
In Ontario, Canada, health administrative data where women with schizophrenia can be accurately identified have recently been linked to data from a clinical perinatal health registry that records data on both potentially modifiable risk factors for adverse perinatal outcomes and detailed data on the outcomes themselves. This has created a key opportunity to advance knowledge around maternal schizophrenia and pregnancy outcomes in a way that could drive the development of key interventions to improve perinatal outcomes in this vulnerable population.
Herein, the primary aim was to examine the occurrence of specific perinatal outcomes (preterm birth, small for gestational age, and abnormal Apgar scores) among all pregnant women with schizophrenia in Ontario, Canada, over a 6-year period, compared to those without a psychiatric disorder, and use statistical mediation analysis to determine whether any of a large set of specific identifiable risk factors contained in the clinical health registry explains any observed increased risk of the outcomes in the maternal schizophrenia group.
Methods
Study design and data sources
This population-based cohort study used multiple linked population-based health administrative databases housed at ICES in Toronto, Ontario. ICES is an independent, non-profit research organization that evaluates universally available healthcare services in Ontario using a variety of administrative health databases (www.ices.on.ca). The databases, which date back to 1988, contain patient-level records that are de-identified and linked to every Ontario resident through a unique coded identifier. These datasets were linked using unique encoded identifiers and analysed at ICES. The following ICES databases were used in the current study: (1) the Registered Persons Database (RPDB) captures the sex, age, postal code, dates of birth and death (when applicable) for all Ontario residents with a provincial health card number (approximately 13 million individuals); (2) the Canadian Institute of Health Information (CIHI) Discharge Abstract Database (DAD) and (3) the Ontario Mental Health Reporting System Database (OMHRS) capture hospital-related data; (4) the National Ambulatory Care Reporting System Database (NACRS) holds emergency department data, and (5) the Ontario Health Insurance Plan Database (OHIP) contains outpatient physician service use data. The data quality in these administrative databases is accurate and complete regarding demographic information, primary diagnoses for inpatient services, and billing claims for physician services [12].
A major advantage to the current study was the recent linkage of the ICES health administrative data with Ontario’s Better Outcomes Registry and Network (BORN), a prescribed registry where clinical data are entered into a standardized system by hospital and midwifery staff during several healthcare encounters during and up to 6 weeks after pregnancy. The system has automated algorithms and discrepancy reports during data entry to enhance validity [13]. Data relevant to the behavioural context of perinatal outcomes that are not routinely collected in administrative data, including smoking and substance use (based on sensitive maternal inquiry during the clinical encounter), are available. BORN data are securely transferred to ICES under a Data Sharing Agreement. The first set of BORN data transferred into ICES comprised births from 2006 to 2011, so these are the years of data analysed for the current study.
Participants
The cohort included all Ontario women aged 15–49 years who gave birth to a live or stillborn singleton infant between 1 January 2006 and 31 December 2011. Non-Ontario residents, and those with an invalid health card number or mother–infant matching, were excluded due to an inability to link across databases. When women had more than one obstetrical delivery during the study period, one pregnancy was selected at random for the current analysis.
Maternal schizophrenia was defined as > 1 maternal hospitalization or > 3 outpatient contacts for schizophrenia within 3 years of each other since database inception and prior to conception of the index pregnancy [14] (ICD-9 codes: 295, 297-8; ICD-10 codes: F20, 22-25, 28-29; sensitivity [Sn] 90.1%, specificity [Sp] 68.0%, positive predictive value [PPV] 77.1%, negative predictive value [NPV] 88.7% in our data). From the remaining pregnancies, we selected an unexposed comparison group of pregnancies where no psychiatric disorder of any type was documented at any time in the 5 years preceding conception of the index pregnancy.
Study variables
Study outcomes were, as recorded in the BORN dataset: (1) preterm birth at less than 37 weeks of gestation; (2) small for gestational age (SGA; defined as a same-sex, same-gestational age birthweight below the third percentile); (3) Apgar score of less than 8 at 1 min post-birth; and (4) Apgar score of less than 8 at 5 min post-birth. The outcomes were selected as they are standard perinatal health indicators in our jurisdiction, and are often considered markers of short-term and longer-term child health outcomes across the lifespan [13, 15,16,17].
Covariates measured included maternal sociodemographic characteristics at the time of the index birth (age and parity; neighbourhood income quintile; urban vs. rural residence, according to each woman’s residential postal code at the time of delivery [18]); maternal chronic medical conditions (diabetes mellitus, chronic hypertensive disorders, thyroid disease, renal disease, HIV, most using validated ICES disease registries) [19, 20]; maternal reproductive history (prior preterm birth, Caesarean section, surgical abortion; assisted reproduction); pregnancy exposures (smoking, alcohol, substance use comprising opiates, cocaine and amphetamine as recorded at any time during the pregnancy); and pregnancy complications (e.g. preeclampsia, placental disorders, premature rupture of membranes, labour induction and delivery type). In the current study [21], sociodemographic characteristics were considered confounders, as they are factors distal to the outcomes of interest. Factors selected as potential mediators were measurable covariates considered to be well-known risk factors for outcomes under study and included maternal chronic medical conditions, reproductive history, pregnancy exposures, and pregnancy complications [22,23,24,25,26,27,28,29,30,31,32,33] (see Table 1 and Fig. 1).
Hypothesized relations between maternal schizophrenia and birth outcomes. Shown in black font are variables measurable in our datasets. The variables shown are, by no means, exhaustive, and the specific variables for each potential mediator category for each outcome are shown in Table 1
Statistical analysis
Modified Poisson regression was used to estimate unadjusted relative risks (RR) and 95% confidence intervals (CI) for each outcome, comparing women with schizophrenia to those without a psychiatric disorder for each outcome [34]. Adjusted relative risks (aRR) and 95% CI were then generated, controlling for confounders (i.e. maternal age, parity, neighbourhood income quintile, rural/urban residence, infant sex, and year of birth).
Mediation analyses were conducted to understand potential explanatory factors for elevated aRRs observed among women with schizophrenia, compared to women with no psychiatric disorder. Specifically, we used mediation analyses to determine whether certain variables might explain a portion of any increased risk that was observed for a given outcome in pregnancies affected by schizophrenia compared to unaffected pregnancies. In mediation analysis, the effect of a given exposure (in this case maternal schizophrenia) can be partitioned into “direct” effects (an effect related to something inherent to the exposure itself) and “indirect” effects, where the effect works through a mediator of interest that may be causally related to the outcome. The direct and indirect effects are summed to equal the “total” effect of the exposure, and the percentage of the total effect explained by a specific mediator is calculated by dividing the indirect effect by the total effect. In the current study, generalized estimating equations were used to test the statistical significance of the difference between coefficients from a full model that included the mediator and a reduced model that excluded the mediator [35]. This difference represents the indirect effect of the exposure, acting through the mediator, on the outcome. One of the prerequisites for mediation is that there is a statistically significant association between the exposure and the outcome and between the exposure and the mediator [35]. Therefore, we only conducted mediation analyses for (a) perinatal outcomes that were statistically significant in the multivariable regression models described above and (b) potential mediators for which there was a statistically significant difference in occurrence between pregnancies exposed and unexposed to maternal schizophrenia in the bivariable analysis. For this latter criterion, we used Pearson’s χ2 tests, with Bonferroni-corrected p values to account for multiple comparisons. We planned to aggregate potential mediators into composite variables (i.e. maternal chronic conditions, maternal reproductive history, pregnancy exposures, and pregnancy complications) and enter these into the mediation analysis one by one, with statistically significant mediation analyses, followed by examining the individual mediators included in the composite. Mediation analyses adjusted for the same covariates as the multivariable regression models. SAS V.9.2 (SAS Institute Inc., Cary, North Carolina, USA) was used for statistical analyses.
The use of data in this project was authorized under section 45 of Ontario’s Personal Health Information Protection Act, which does not require review by a Research Ethics Board. The study was therefore exempt from research ethics approvals and was approved by the ICES privacy office (ICES logged study: 2016 0900 300 024).
Results
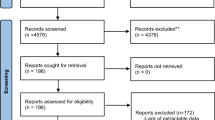
From 738,972 obstetrical deliveries in Ontario (2006–2011), 6708 (0.9%) were excluded due to restrictions in the maternal age criteria and due to inability to link across datasets, resulting in 732,264 deliveries to 574,495 unique women. Of these, there were 4279 obstetrical deliveries among unique women with schizophrenia. From the remainder, the 65,960 pregnancies with evidence of a diagnosed maternal mood disorder and the 218,109 pregnancies with evidence of another psychiatric disorder in the 5 years prior to conception were not included, leaving 286,147 pregnancies for the comparison group of pregnancies unexposed to maternal mental illness. Maternal age was similar between women with schizophrenia and the referent group, but women with schizophrenia were more likely to be multiparous than women without a psychiatric disorder, and to live in a low-income neighbourhood (Table 2).
Compared to women with no psychiatric disorder, infants exposed to maternal schizophrenia were at elevated risk of being born preterm (11.4% vs. 6.9%), small for gestational age at less than the third centile (3.5% vs. 2.5%), to have an Apgar score < 8 at 1 min after birth (19.0% vs. 12.8%) and at 5 min after birth (5.6% vs. 3.0%) (Fig. 1). After adjusting for maternal age at delivery, parity, neighbourhood income quintile, region of residence, infant sex, and year of childbirth, risk remained elevated for each of preterm birth with an aRR of 1.64 (95% CI 1.51–1.77), small for gestational age, aRR 1.40 (95% CI 1.20–1.64), Apgar score < 8 at 1 min, aRR 1.49 (95% CI 1.40–1.59), and Apgar score < 8 at 5 min, aRR 1.90 (95% CI 1.68–2.16) (Fig. 2).
Perinatal outcomes for 4279 infants born to women with schizophrenia and 286,147 infants born to women with no evidence of mental illness in the 5 years preceding pregnancy, presented as N (% with outcome) and adjusted relative risks (RR) with 95% confidence intervals. *Relative risk adjusted for maternal age at delivery, parity, neighbourhood income quintile, region of residence, infant sex (male/female), and year of birth
All potential maternal chronic condition mediators except for thyroid disease and thromboembolic disease were more common among women with schizophrenia than those without. History of preterm birth and surgical abortion was also more common, while assisted reproduction in the current pregnancy was less common (see Table 2). Pregnancy complication rates and mode of delivery were similar between groups, except for the relatively uncommon complications of venous thromboembolism, preeclampsia/eclampsia, and placental abruption which were more common among women with schizophrenia. Caesarean sections were also slightly more common in that group. With respect to the pregnancy exposures category, there was a substantial amount of missing data for maternal body mass index (BMI) so this potential mediator was not examined. Other pregnancy exposures were much more common in the schizophrenia group, especially smoking during pregnancy (28.5% vs. 7.30%, corrected p < 0.0001). Given the limitation of missing data for maternal BMI, and because of the large differences between women with and without schizophrenia observed for the other variables in the pregnancy exposure category, we elected to enter each of smoking, alcohol, and illicit drug use into the mediation analysis separately rather than as a composite variable.
For preterm birth, maternal chronic conditions explained 4.9% of the excess risk associated with maternal schizophrenia, with hypertensive disorders prior to pregnancy being the most important pathway variable, explaining 2.8% of the aRR. Reproductive history explained 8.8% of the excess risk, with prior preterm birth and prior surgical abortion being the only significant pathway variables (3.0%, 2.4%). Smoking and illicit substance use explained 9.9% and 5.3% of the aRR respectively (Table 3). For SGA, maternal chronic conditions explaining less than 1% of the elevated aRR associated with maternal schizophrenia, and the reproductive history category and pregnancy complications each explained about 3% of the risk. Smoking explained the largest proportion of the excess risk of SGA associated with maternal schizophrenia (28.7%), with illicit substance use at 3.0% (also in Table 3). For Apgar scores of less than 8 at 1 min and 5 min post-birth, pregnancy exposures also explained the largest proportion of excess risk, with smoking having the greatest contribution (9.8% and 5.6% respectively), and illicit substance use explaining some risk (3.9%) of Apgar < 8 at 1 min. Other categories explained less of the risk.
Discussion
This study confirmed increased risk of the key adverse perinatal outcomes of preterm birth, small for gestational age, and low Apgar scores in a large population-based cohort of women with schizophrenia. Pregnancy exposures, in particular smoking but also illicit drug use, consistently emerged as factors that explained the greatest proportion of the excess risk of poor outcomes, suggesting potential modifiable targets for intervention. For preterm birth in particular, maternal chronic conditions, and mostly chronic hypertension, were also mediating factors, supporting the argument that optimal management of chronic maternal conditions in the preconception period may also be important.
Our findings with respect to the elevated risk of adverse perinatal outcomes are consistent with previous studies conducted in Australia, Denmark, Sweden, Taiwan, and the USA examining perinatal health outcomes related to maternal schizophrenia in both magnitude and direction, and with previous Canadian studies [8, 36,37,38,39,40,41,42,43,44]. Although most prior studies did not investigate the specific mediating contribution of various factors, those that examined the specific effects of smoking had similar results to those observed herein for both preterm birth and low birthweight outcomes [3, 45, 46]. A small retrospective review of the medical history of 112 women diagnosed with schizophrenia (n = 63) and bipolar disorder (n = 49) between 2008 and 2012 in Australia also found that preterm birth was predicted by illicit drug use [3].
The risk factors identified in this study, including maternal health conditions, reproductive history variables, and pregnancy exposures such as smoking, are well-known risk factors for preterm birth, small for gestational age, and low Apgar scores in general (non-schizophrenia) populations. What the results of the analyses in the current study add to the current literature is whether and to what extent some of these risk factors are specifically responsible for the elevated risk of these outcomes in pregnancies exposed to maternal schizophrenia. Following from this, the findings strongly suggest that there is a need for a public health approach to the management of physical illness and behavioural risk factors for physical illness in pregnant and pregnancy-planning women with severe and persistent mental illness. Preconception care initiatives are increasingly becoming focused on the management and control of maternal chronic conditions prior to and during pregnancy [47,48,49]. Specific health improvement interventions targeting key risk factors (e.g. smoking cessation, substance use) during pregnancy have also been shown to be moderately effective [50,51,52,53]. For example, two studies found that pregnant smokers randomized to nicotine replacement therapies vs. non-nicotine replacement treatment had infants born at higher birthweight [52, 53]. To our knowledge, however, no interventions have been specifically adapted for and evaluated in pregnant women with serious mental illness (SMI, for example, schizophrenia and bipolar disorder). This may be an important gap since adaptations for this population are likely to be necessary due to the cognitive and other symptoms often associated with the illness [54, 55]. Outside of pregnancy, health improvement interventions have been adapted for SMI and have been shown to increase smoking cessation rates and improve weight and eating, at least in the short term [56,57,58,59,60,61]. Given the significant desire that many women with schizophrenia demonstrate for achieving healthy pregnancy and motherhood, the preconception and pregnancy period may be ideal for such types of interventions [62]. Even short-term improvements in chronic maternal health conditions such as hypertension, or reduction of cessation of smoking, could improve pregnancy outcomes. Successful smoking cessation preconception or during pregnancy might also increase the chances that a woman remains smoke-free longer term, with the resultant benefit to her health, and also to the health of any children living in her home. That being said, intervention adaptations for women with severe mental illness are likely to require significant collaboration and integration between physical health and mental health services in order to meaningfully engage this harder to reach group.
While the datasets used in this study were novel in the combination of health administrative and clinical data provided on a population level, we were only able to explain about one-quarter of the excess risk of any of the outcomes with the measured mediators. Schizophrenia itself is associated with low activity of plasminogen activator, and this could contribute to placental insufficiency in pregnant women to drive increased risk of the outcomes under study [63, 64]. There could also be genetic risk or propensity to adverse perinatal outcomes associated with schizophrenia itself—individuals with schizophrenia are more likely to have been born small, early, and to have experienced perinatal complications around the time of birth themselves [65, 66]. However, there were limitations in the details that we were able to collect. The influence of poverty, economic stress, unsafe living conditions, domestic violence, and lack of social support may all interact to create a suboptimal state for maternal well-being that was not perfectly captured by the measured variables [7]. We were not able to examine the potential contribution of maternal BMI, or other factors such as prescription drug use since these were not available for the entire cohort. We were also unable to examine the possible impact of other comorbid non-psychotic disorders since these were not present in the referent group. For example, active comorbid mood disorders may have explained part of the excess risk, although likely not all. In prior research by members of our team and others, the excess outcome risk in maternal mood disorder populations is generally less than what was observed in maternal schizophrenia populations, including that of the current study [67]. The complex interplay of psychiatric comorbidity is an important direction for future analyses. Finally, we were not able to quantify the extent of smoking or the exact nature and extent of illicit drug use.
In conclusion, combining clinical datasets with health administrative data can serve to enrich population-based studies to provide more context and guidance about potential targets for intervention, especially for vulnerable populations where it is difficult to enrol large samples in clinical studies. Our methodology allowed us to confirm the contribution of some key risk factors for elevated risk of adverse perinatal outcomes in pregnancies complicated by maternal schizophrenia, and generate ideas for supports and services that have potential to reduce that risk.
References
Bennedsen BE (1998) Adverse pregnancy outcome in schizophrenic women: occurrence and risk factors. Schizophr Res 33(1–2):1–26
Conde A et al (2010) Mother’s anxiety and depression and associated risk factors during early pregnancy: effects on fetal growth and activity at 20–22 weeks of gestation. J Psychosom Obstet Gynaecol 31(2):70–82
Judd F et al (2014) Adverse obstetric and neonatal outcomes in women with severe mental illness: to what extent can they be prevented? Schizophr Res 157(1–3):305–309
Vigod SN et al (2012) Temporal trends in general and age-specific fertility rates among women with schizophrenia (1996–2009): a population-based study in Ontario, Canada. Schizophr Res 139(1–3):169–175
Ng R et al (2015) Brain disorders in Ontario: prevalence, incidence and costs from health administrative data. Institute for Clinical Evaluative Sciences, Toronto, Ontario, Canada
Lasser K et al (2000) Smoking and mental illness: a population-based prevalence study. JAMA 284(20):2606–2610
Hudson CG (2005) Socioeconomic status and mental illness: tests of the social causation and selection hypotheses. Am J Orthopsychiatr 75(1):3–18
Lin HC, Chen YH, Lee HC (2009) Prenatal care and adverse pregnancy outcomes among women with schizophrenia: a nationwide population-based study in Taiwan. J Clin Psychiatr 70(9):1297–1303
Buss C et al (2012) The Role of stress in brain development: the gestational environment’s long-term effects on the brain. Cerebrum 2012:4
Beijers R et al (2010) Maternal prenatal anxiety and stress predict infant illnesses and health complaints. Pediatrics 126(2):e401–e409
Dunkel Schetter C, Tanner L (2012) Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Curr Opin Psychiatr 25(2):141–148
Williams J et al (1996) Patterns of health care in Ontario: the ICES Practice Atlas. Canadian Medical Association, Ottawa
Ray JG et al (2012) Birth weight curves tailored to maternal world region. J Obstet Gynaecol Can 34(2):159–171
Kurdyak P et al (2015) Validation of a population-based algorithm to detect chronic psychotic illness. Can J Psychiatr 60(8):362–368
Razaz N et al (2016) Five-minute Apgar score as a marker for developmental vulnerability at 5 years of age. Arch Dis Child Fetal Neonatal Ed 101(2):F114–F120
Health Canada, M.o.P.W.a.G.S.C. (2000) Perinatal health indicators for Canada: a resource manual, Ottawa
Ehrenstein V et al (2009) Association of Apgar score at 5 min with long-term neurologic disability and cognitive function in a prevalence study of Danish conscripts. BMC Pregnancy Childbirth 9:14
Urquia ML et al (2007) Birth outcomes by neighbourhood income and recent immigration in Toronto. Health Rep 18(4):21–30
Hux JE et al (2002) Diabetes in Ontario: determination of prevalence and incidence using a validated administrative data algorithm. Diabetes Care 25(3):512–516
Quan H et al (2009) Validation of a case definition to define hypertension using administrative data. Hypertension 54(6):1423–1428
McCarthy J, Maine D (1992) A framework for analyzing the determinants of maternal mortality. Stud Fam Plann 23(1):23–33
Saccone G, Perriera L, Berghella V (2016) Prior uterine evacuation of pregnancy as independent risk factor for preterm birth: a systematic review and metaanalysis. Am J Obstet Gynecol 214(5):572–591
Steer P (2005) The epidemiology of preterm labour. BJOG 112(Suppl 1):1–3
Gravett MG et al (2010) Global report on preterm birth and stillbirth (2 of 7): discovery science. BMC Pregnancy Childbirth 10(Suppl 1):S2
Sheehan PM et al (2015) Maternal thyroid disease and preterm birth: systematic review and meta-analysis. J Clin Endocrinol Metab 100(11):4325–4331
Aagaard-Tillery KM et al (2008) In utero tobacco exposure is associated with modified effects of maternal factors on fetal growth. Am J Obstet Gynecol 198(1):66.e1–66.e6
Patra J et al (2011) Dose-response relationship between alcohol consumption before and during pregnancy and the risks of low birthweight, preterm birth and small for gestational age (SGA)-a systematic review and meta-analyses. BJOG 118(12):1411–1421
Maeda A et al (2014) Opioid abuse and dependence during pregnancy: temporal trends and obstetrical outcomes. Anesthesiology 121(6):1158–1165
Gouin K et al (2011) Effects of cocaine use during pregnancy on low birthweight and preterm birth: systematic review and metaanalyses. Am J Obstet Gynecol 204(4):340.e1–340.e12
Gorman MC et al (2014) Outcomes in pregnancies complicated by methamphetamine use. Am J Obstet Gynecol 211(4):429.e1–429.e7
Hingson R et al (1982) Maternal cigarette smoking, psychoactive substance use, and infant Apgar scores. Am J Obstet Gynecol 144(8):959–966
Vahanian SA et al (2015) Placental implantation abnormalities and risk of preterm delivery: a systematic review and metaanalysis. Am J Obstet Gynecol 213(4 Suppl):S78–S90
Ananth CV et al (1999) Placental abruption and adverse perinatal outcomes. JAMA 282(17):1646–1651
Zou G (2004) A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 159(7):702–706
Schluchter MD (2008) Flexible approaches to computing mediated effects in generalized linear models: generalized estimating equations and bootstrapping. Multivariate Behav Res 43(2):268–288
Bennedsen BE et al (1999) Preterm birth and intra-uterine growth retardation among children of women with schizophrenia. Br J Psychiatr 175:239–245
Bennedsen BE et al (2001) Obstetric complications in women with schizophrenia. Schizophr Res 47(2–3):167–175
Nilsson E et al (2002) Women with schizophrenia: pregnancy outcome and infant death among their offspring. Schizophr Res 58(2–3):221–229
Zhong QY et al (2018) Adverse obstetric and neonatal outcomes complicated by psychosis among pregnant women in the United States. BMC Pregnancy Childbirth 18(1):120
Lee HC, Lin HC (2010) Maternal bipolar disorder increased low birthweight and preterm births: a nationwide population-based study. J Affect Disord 121(1–2):100–105
Nguyen TN et al (2013) Obstetric and neonatal outcomes of pregnant women with severe mental illness at a specialist antenatal clinic. Med J Aust 199(3 Suppl):S26–S29
Schneid-Kofman N, Sheiner E, Levy A (2008) Psychiatric illness and adverse pregnancy outcome. Int J Gynaecol Obstet 101(1):53–56
Vigod SN et al (2014) Maternal and newborn outcomes among women with schizophrenia: a retrospective population-based cohort study. BJOG 121(5):566–574
Matevosyan NR (2011) Pregnancy and postpartum specifics in women with schizophrenia: a meta-study. Arch Gynecol Obstet 283(2):141–147
Simoila L et al (2018) Obstetric and perinatal health outcomes related to schizophrenia: a national register-based follow-up study among Finnish women born between 1965 and 1980 and their offspring. Eur Psychiatr 52:68–75
Jablensky AV et al (2005) Pregnancy, delivery, and neonatal complications in a population cohort of women with schizophrenia and major affective disorders. Am J Psychiatr 162(1):79–91
Berger H et al (2016) Diabetes in pregnancy. J Obstet Gynaecol Can 38(7):667
Butalia S et al (2018) Hypertension Canada’s 2018 guidelines for the management of hypertension in pregnancy. Can J Cardiol 34(5):526–531
Association A. D (2018) Management of diabetes in pregnancy. Diabetes Care 41(Suppl 1):S137–S143
Bérard A, Zhao JP, Sheehy O (2016) Success of smoking cessation interventions during pregnancy. Am J Obstet Gynecol 215(5):611.e1–611.e8
Hand DJ et al (2017) Contingency management interventions for tobacco and other substance use disorders in pregnancy. Psychol Addict Behav 31(8):907–921
Oncken C et al (2008) Nicotine gum for pregnant smokers: a randomized controlled trial. Obstet Gynecol 112(4):859–867
Wisborg K et al (2000) Nicotine patches for pregnant smokers: a randomized controlled study. Obstet Gynecol 96(6):967–971
Kilbourne AM et al (2014) SMI life goals: description of a randomized trial of a collaborative care model to improve outcomes for persons with serious mental illness. Contemp Clin Trials 39(1):74–85
Vaez K et al (2017) Evaluating diabetes care for patients with serious mental illness using the chronic care model: a pilot study. Health Serv Res Manag Epidemiol 4:2333392817734206
Dickerson F et al (2013) Cigarette smoking among persons with schizophrenia or bipolar disorder in routine clinical settings, 1999-2011. Psychiatr Serv 64(1):44–50
Faulkner G, Cohn T, Remington G (2007) Interventions to reduce weight gain in schizophrenia. Cochrane Database Syst Rev 1:CD005148
Gilbody S et al (2015) Bespoke smoking cessation for people with severe mental ill health (SCIMITAR): a pilot randomised controlled trial. Lancet Psychiatr 2(5):395–402
Hauck Y et al (2008) Healthy babies for mothers with serious mental illness: a case management framework for mental health clinicians. Int J Ment Health Nurs 17(6):383–391
Tsoi DT, Porwal M, Webster AC (2013) Interventions for smoking cessation and reduction in individuals with schizophrenia. Cochrane Database Syst Rev 2:CD007253
Bennett ME, Bradshaw KR, Catalano LT (2017) Treatment of substance use disorders in schizophrenia. Am J Drug Alcohol Abuse 43(4):377–390
Seeman MV (2008) Prevention inherent in services for women with schizophrenia. Can J Psychiatry 53(5):332–341
Hoirisch-Clapauch S, Nardi AE (2014) Markers of low activity of tissue plasminogen activator/plasmin are prevalent in schizophrenia patients. Schizophr Res 159(1):118–123
Hoirisch-Clapauch S, Brenner B, Nardi AE (2015) Adverse obstetric and neonatal outcomes in women with mental disorders. Thromb Res 135(Suppl 1):S60–S63
Mittal VA, Ellman LM, Cannon TD (2008) Gene-environment interaction and covariation in schizophrenia: the role of obstetric complications. Schizophr Bull 34(6):1083–1094
Suvisaari JM et al (2013) Obstetric complications as risk factors for schizophrenia spectrum psychoses in offspring of mothers with psychotic disorder. Schizophr Bull 39(5):1056–1066
Mei-Dan E, Ray JG, Vigod SN (2015) Perinatal outcomes among women with bipolar disorder: a population-based cohort study. Am J Obstet Gynecol 212(3):367e1–367e8
Acknowledgements
We thank the Ontario Ministry of Health and Long-Term Care for their data. Parts of this material are based on data and/or information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions, and statements expressed herein are those of the authors and not necessarily those of the CIHI. This study is based in part on data provided by Better Outcomes Registry and Network (“BORN”), part of the Children’s Hospital of Eastern Ontario. The interpretation and conclusions contained herein do not necessarily represent those of BORN Ontario.
Funding
This work was supported by the ICES, which is funded by an annual Grant from the MOHLTC. It was also supported by the Mental Health and Addictions Scorecard and Evaluation Framework Grant from the MOHLTC (Grant number 04601A14-19). The opinions, results, and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
In terms of author disclosures, Dr. Vigod receives royalties for authorship of chapters related to depression and pregnancy from UpToDate Inc. The other authors have declared that there are no conflicts of interest in relation to the subject of this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vigod, S.N., Fung, K., Amartey, A. et al. Maternal schizophrenia and adverse birth outcomes: what mediates the risk?. Soc Psychiatry Psychiatr Epidemiol 55, 561–570 (2020). https://doi.org/10.1007/s00127-019-01814-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-019-01814-7