Abstract
Purpose
Study drop-out during follow-up and service disengagement frequently occur in patients at clinical high risk for psychosis (CHR-P). However, little is known about their predictors. Therefore, we aimed to analyze the rate and reasons for drop-out and service disengagement in CHR-P patients and investigate their sociodemographic and clinical predictors.
Methods
Data from 200 patients of the prospective Früherkennung von Psychosen (FePsy) study were analyzed with competing risks survival models, considering drop-out and transition to psychosis as competing events. To investigate whether symptoms changed immediately before drop-out, t tests were applied.
Results
Thirty-six percent of patients dropped out within 5 years. Almost all drop-outs also disengaged from our service. Hence, study drop-out was used as a proxy for service disengagement. Patients with more severe baseline disorganized symptoms and a late inclusion into the study were significantly more likely to disengage. Immediately before disengagement, there was significant improvement in negative symptoms only.
Conclusion
A considerable proportion of CHR-P patients disengaged from our clinical study and service. Patients who were included during a later study period with more assessments disengaged more often, which might have been due to more frequent invitations to follow-up assessments and thereby increasing participation burden. Hence, our study provides a cautionary note on high-frequency follow-up assessments. Larger-scale studies evaluating predictors on multiple domains would help to further elucidate drop-out and disengagement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Psychotic disorders such as schizophrenia are serious mental disorders, which occupy the sixth largest share of disability-adjusted life years (DALYs) in European adults [1, 2]. Schizophrenia is associated with high premature mortality rates leading to about 15 years of potential life lost and increased rates of multiple somatic disorders [3, 4]. In the last decades, there has been growing interest in the early detection and intervention regarding psychotic disorders, as it has been shown that early treatment can improve outcomes in those affected [2, 5]. Even patients at clinical high risk for psychosis (CHR-P) may suffer from a high symptomatic burden and functional decline [for meta-analysis, see 6]. The establishment of CHR-P services has shown that early detection and intervention is beneficial to this patient group in many respects. Specifically, it has been associated with symptom reduction, improvement of functional outcomes and a reduction of the risk of transition to frank psychosis [2, 5, 7].
However, an unresolved issue in studying CHR-P patients is that a considerable proportion of these patients drop out during the study follow-up. Recent studies reported drop-out rates ranging from 36% at 2 years of follow-up [8] to 68% at 3 years [9]. Only few studies investigated predictors of study drop-out and those existing reported inconsistent results. While one study reported that higher baseline negative symptoms significantly predicted later study drop-out [9], another study could not detect any significant relationship between baseline clinical variables and later study drop-out [8]. However, in both studies, sociodemographic and clinical variables such as age, gender, marital status, ethnicity, positive psychotic or depressive symptoms, social and role functioning, antipsychotic or antidepressant medication, as well as years of education were not associated with study drop-out [8, 9].
At the same time, many CHR-P patients disengage from clinical early intervention services. It has previously been described that service disengagement may be associated with poorer outcomes and higher health care costs across mental health services [10, 11]. To our knowledge, only one study has explicitly focused on service disengagement in CHR-P patients [12]. In this study, data on patients referred to the Outreach and Support in South London (OASIS) were collected indirectly from clients’ general practitioners and electronic patient files. It was found that over one-fifth (21.2%) of referred patients did not attend or engage with the service. Furthermore, those who did not engage with the clinical service were more often unemployed at the time of referral than engagers [12]. No differences with regard to ethnicity, age, gender, or marital status were found.
While only few studies have investigated predictors of service disengagement and study drop-out in CHR-P patients, a number of studies have been performed in first episode psychosis (FEP) patients [for systematic review, see 13], which might provide further indications for potential predictors in CHR-P patients. Studies analyzing service disengagement in FEP patients found that disengagement was significantly predicted by substance abuse or dependence [13,14,15], poor medication compliance [14, 16], history of self-harm or suicidal attempts [14], lack of insight [13], lower symptom severity at baseline [13, 15], missing support or involvement of a family member [13], as well as having milder psychopathology, and being employed or a student [15]. Conflicting findings have been reported regarding duration of untreated psychosis (DUP), since shorter as well as longer DUP [13, 14] has been associated with service disengagement.
There are still several open questions regarding service disengagement and/or study drop-out in CHR-P patients. So far, it is not clear if some of the factors associated with service disengagement in FEP patients (e.g., substance abuse/dependence or lack of illness insight) are also associated with service disengagement in CHR-P patients. Furthermore, it is unknown whether patients who disengage from services show symptom worsening or improvement immediately before service disengagement and/or study drop-out.
Thus, the present study aimed to analyze the rate, self-reported reasons and predictors for service disengagement and/or study drop-out in CHR-P patients. Due to our study design, we were able to analyze predictors of both service disengagement and study drop-out at the same time, as these two outcomes were highly correlated in our study. Specifically, we aimed to replicate previous findings and examine additional predictors of service disengagement which have previously not been analyzed in this patient group. Based on previous studies in FEP patients, we hypothesized that lack of insight and cannabis use would significantly predict service disengagement in CHR-P patients. Additionally, we hypothesized that clinical variables would possibly predict service disengagement. We especially tested if service disengagement is associated with recent change in symptoms.
Materials and methods
Setting and recruitment
Study participants were recruited between March 1, 2000 and May 31, 2017 within the prospective “Früherkennung von Psychosen” (FePsy; early detection of psychosis) study. A detailed description of the overall study design can be found elsewhere [17, 18]. Recruitment took place via the FePsy Clinic, University of Basel Psychiatric Hospital, Switzerland, where patients suspected to be at risk for psychosis were referred to by general practitioners, parents, teachers, as well as mental health professionals. All patients referred to our service and meeting inclusion criteria (see below) were asked to participate in our prospective study. All study participants provided written informed consent. The study was approved by the ethics committee of Northwestern and Central Switzerland (EKNZ) and was conducted in accordance with the Declaration of Helsinki.
Screening
CHR-P patients were identified using the Basel Screening Instrument for Psychosis (BSIP), which is a semi-structured interview developed by Riecher-Rössler et al. [19]. The BSIP allows the identification of CHR-P or FEP patients. It is composed of the prodromal symptoms of the Diagnostic and Statistical Manual of Mental Disorders [DSM-III-R; 20], other risk factors such as young age or drug abuse derived from previous studies [19, 21], and the Personal Assessment and Crisis Evaluation (PACE) criteria by Yung et al. [22]. Additionally, the BSIP defines an unspecific risk category (URC) for patients thought to be at lower risk because of presenting with less specific symptoms and risk factors for psychosis. The instrument has been shown to have a high reliability and predictive validity [18, 19]. A more detailed description of the BSIP as well as an English version of the instrument can be found in Peralta et al. [23].
Patients were included in this study if they met CHR-P criteria according to the BSIP, which occurred if one of the following criteria was met: (1) attenuated psychotic symptoms (APS); (2) brief limited intermittent psychotic symptoms (BLIPS); (3) genetic risk and deterioration syndrome (GRD): genetic risk in combination with two or more other risk factors such as social decline; and (4) URC: a combination of risk factors according to the BSIP, which can be found in Peralta et al. [23]. Patients fulfilling the criteria for APS, BLIPS or GRD are considered at “high risk” because of presenting a more psychosis-related risk set; whereas, patients fulfilling the URC criteria were considered at “lower risk” because of the unspecific nature of their symptoms [17, 19, 23].
Exclusion criteria were: age < 18, insufficient knowledge of German, IQ < 70, current or previous episode of schizophrenic psychosis according to the BSIP criteria (i.e., transition criteria according to Yung et al. [22] fulfilled), antipsychotic treatment for > 3 weeks (lifetime) and/or a total amount of ≥ 2500 mg chlorpromazine equivalent, or psychotic symptomatology within a clearly diagnosed affective psychosis or borderline personality disorder [17].
Baseline assessments
Sociodemographic variables and illness insight were assessed with the Basel Interview for Psychosis [BIP; 24], a semi-structured interview designed to assess indicators of emerging psychosis and the temporal development of psychiatric symptoms over the entire life span. Illness insight in the BIP was categorically rated as “absent”, “fully present”, or “questionable”.
Baseline negative symptoms were assessed with the Scale for the Assessment of Negative Symptoms [SANS; 25]. The SANS total score and its five original subscales (i.e., affective flattening, alogia, avolition/apathy, asociality/anhedonia and inattention) were used for statistical analyses. Baseline psychotic symptoms were assessed with the Brief Psychiatric Rating Scale Expanded version [BPRS-E; 26], and BPRS-E subscales were calculated according to the five-factor structure (positive symptoms, negative symptoms, activation, affect and disorganization) proposed by Shafer et al. [27]. Functioning was measured with the Global Assessment of Functioning (GAF) scale [28]. To assess comorbid psychopathology, we applied the Structured Clinical Interview for DSM-IV Axis I Disorders [SCID-I; 29] and additionally applied the SCID-II for personality disorders if screening was positive [30].
Follow-up assessments
CHR-P patients were reassessed and followed up at regular intervals for up to 5–7 years to examine whether transition to psychosis had occurred. However, since only few patients had a follow-up duration of more than 5 years, these patients were treated as right-censored at the 5-year follow-up. From 2000 to 2008, follow-up frequency depended upon the estimated risk set. Specifically, during the first follow-up year, “high-risk” patients were assessed monthly, while “low-risk” patients fulfilling only the URC criteria were assessed at 3-month intervals. During the second and third follow-up years, all patients were assessed every 3 months and thereafter annually. In the year 2009, methodological changes were applied to the FePsy study. To provide uniform follow-up assessments to all CHR-P patients, “low-risk” patients were followed up in the same intervals as “high-risk” patients and were also assessed monthly during the first follow-up year. Assessment intervals during the second and third years did not change.
During follow-up, all patients received supportive counseling and clinical management. A small fraction (n = 9) of the included patients also participated in the Neurapro study [31, 32] and thus were treated with omega-3 fatty acids or placebo. Transition to psychosis was monitored applying the transition criteria of Yung et al. [22] using the four BPRS items “suspiciousness”, “unusual thought content”, “hallucinations” and “conceptual disorganization”. Follow-up assessments were terminated in case of transition to psychosis, or if no transition occurred after 5–7 years.
Outcome assessment
Study drop-out during follow-up was defined as the primary outcome variable and was assessed prospectively. CHR-P patients were considered as drop-out when no contact could be established for at least 1 year after several contact attempts had not been successful. Contact attempts included phone calls, letters, e-mails, text messages or contact with family members or general practitioners and other medical professionals, if release from medical confidentiality had been provided previously. CHR-P patients were also considered as having dropped out from our study when they explicitly refused to further participate in the study. In this case, drop-out reasons were assessed and documented on specific drop-out protocols. For those patients who dropped out, the drop-out date was defined as the date of their last visit.
To test whether study drop-out could be used as a proxy for service disengagement, we additionally assessed whether patients dropping out of our study also disengaged with our clinical service. To this end, electronical medical records of a subset of our sample were inspected.
Statistical analyses
All statistical analyses were conducted using the R environment for statistical computing [33]. Drop-out was the primary outcome measure. However, according to the FePsy study design, follow-up assessment could be ceased either due to drop-out or due to transition to psychosis. Drop-out and transition were treated as competing events, since CHR-P patients could only experience one of the two event types over follow-up.
In a first step, we investigated rates of drop-out and transition to psychosis over the whole course of follow-up using cumulative incidence curves (CIC), which are the competing risks analogs of Kaplan–Meier survival curves [34, 35].
To discriminate between CHR-P patients with and without drop-out, and to test sociodemographic and clinical predictors, we applied competing risks survival analysis. We, therefore, fitted a cause-specific Cox proportional hazard model where the competing event “transition to psychosis” was treated as a censored category. We previously checked that the proportionality-of-hazards assumption was met. Univariable models were fitted for each potential predictor. Predictor variables included sociodemographic variables (age, sex, relationship status, living situation, occupation, functioning, level of education) as well as clinical variables (Axis-I diagnoses, type of CHR-P status (any of APS, BLIPS or GRD vs. URC only), cannabis use, current intake of antidepressants, BRPS and SANS subscales and illness insight). We additionally used inclusion date (i.e., inclusion from 2000 to 2008 vs. inclusion from 2009 to 2017) as a binary predictor because of the previously described methodological changes in study design in 2009. Ten patients had been treated with antipsychotics during the follow-up, which could have altered their natural disease course, and were, therefore, considered right-censored at the time when treatment with antipsychotics started. Five patients could no longer participate because they had moved too far away and were, therefore, considered right-censored at the time of relocation. For each univariable model, likelihood ratio p values were estimated. Testing was two-tailed at a 5% significance level and missings were excluded pairwise.
To examine whether patients presented with increasing or decreasing symptoms immediately before drop-out, we assessed a potential change in symptoms over time. We, therefore, compared BPRS sub- and total scales of the last and second-last assessments and applied dependent sample t tests. For this analysis, we only included CHR-P patients with study drop-out and a maximum time difference of 120 days between the last and second-last assessment.
Results
Sample characteristics
A total of 739 patients with suspected CHR-P were screened, of whom 310 were identified as having a CHR-P, 308 met criteria for FEP, and 121 were not at-risk for psychosis. Of the 310 CHR-P patients, 277 met our inclusion criteria. Of these, 200 provided written informed consent and thus were included in this study (see Table 1 for sociodemographic and clinical sample characteristics). The 77 patients who refused to participate did not differ from the 200 included patients with regard to gender and years of education but they were significantly older (MParticipants = 25.1 years; MRefusers = 29.5 years).
Rate and reasons of drop-out
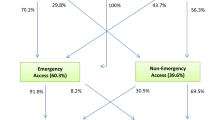
Within 5 years, 53 patients dropped out from the study and 43 transitioned to psychosis. An inspection of medical records revealed that only two patients with study drop-out still remained in our clinical service. The estimated cumulative incidence curves for both drop-out and transition are displayed in Fig. 1. The risk of dropping out within 1, 2, 3, 4, and 5 years of the follow-up was estimated as 0.13, 0.20, 0.26, 0.33 and 0.36, respectively. The respective transition risk was estimated as 0.15, 0.18, 0.22, 0.24, and 0.28. The mean follow-up time of patients with later drop-out was 1.55 years and 1.23 years of patients with a subsequent transition to psychosis.
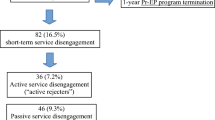
Of those with drop-out, 41 patients (77.4%) explicitly requested to discontinue follow-up assessments. The identified reasons for refusal were: symptomatic improvement, and therefore no more need for service (6 patients, 14.6%), transition to another mental health service or psychotherapist (3 patients, 7.3%), lack of time and interest (4 patients, 9.8%), being annoyed by requests for study participations (8 patients, 19.5%) and no specific reason (16 patients, 39.0%). Information was missing for 4 patients (9.8%). Twelve out of 53 patients (22.6%) could not be reached for at least 1 year after several attempts and were, therefore, considered as drop-out.
Baseline predictors of study drop-out
Results of competing risks survival analysis are presented in Table 2. Univariate cause-specific hazard models revealed that patients with a late inclusion into the service (2009–2017) were significantly more likely to drop out than patients with an early inclusion (2000–2008). Furthermore, patients with a higher baseline score in the BPRS disorganization scale were significantly more likely to drop out. Notably, no other baseline sociodemographic or clinical predictors significantly predicted study drop-out. Results of the cause-specific hazard models for transition to psychosis can be found in the supplementary material.
Change in symptoms from second-last to last assessment in patients with study drop-out
Twenty-five patients were found to have a maximum time difference of 120 days between the second-last and last assessment before study drop-out, and thus were included in this analysis. When examining a potential change in symptoms, we observed that only BPRS-negative symptoms had significantly improved over time (Msecond-last = 4.18 and SD = 1.55; Mlast = 3.56 and SD = 1.16; p = 0.019). There were no significant differences from the second-last to last assessment in BPRS total score (Msecond-last = 33.00 and SD = 8.82; Mlast = 30.90 and SD = 6.10; p = 0.097), BPRS positive symptoms (Msecond-last = 4.52 and SD = 1.71; Mlast = 4.08 and SD = 1.55; p = 0.156), BPRS activation (Msecond-last = 3.40 and SD = 0.91; Mlast = 3.42 and SD = 0.84; p = 0.918), BPRS affect (Msecond-last = 4.90 and SD = 1.85; Mlast = 4.56 and SD = 1.47; p = 0.356) and BPRS disorganization (Msecond-last = 3.62 and SD = 1.09; Mlast = 3.48 and SD = 0.92; p = 0.577). The results of the dependent sample t tests can be found in Fig. 2.
Discussion
The present study is one of the first to study rates, reasons and predictors of study drop-out and service disengagement in CHR-P patients. We found that 36% of CHR-P patients dropped out from the study within 5 years and almost all of them also disengaged from our clinical service after study drop-out. Hence, in this study drop-out can be used as proxy for service disengagement. We found that study drop-out and service disengagement during follow-up were significantly associated with higher levels of baseline disorganized symptoms and with being included in the study after 2009. Moreover, we found that negative symptoms had significantly improved from the second-last to the last assessment before study drop-out, whereas positive symptoms had not changed.
The drop-out and disengagement rate of 36% after 5 years of follow-up in our study is rather low compared to previous studies, which reported drop-out rates of 36% after 2 years of follow-up [8] and 68% after 3 years [9]. Our low rate might be attributed to methodological differences regarding the operationalization of study drop-out. In our study, patients were considered as having dropped out when no contact could be established for at least 1 year. However, clear and widely accepted definitions of study drop-out and service disengagement are lacking both for ARMS and FEP patients so far [11, 13]. Other studies have used lower [15, 16, 36, 37], as well as higher thresholds [38, 39], analyzed different follow-up durations [8, 9], or defined different types of disengagement [14]. Engagement and disengagement are often measured through attendance [11], as we did in our study. Yet, there are also studies describing service engagement and disengagement as multidimensional, multifaceted constructs comprising more than just service attendance [10, 11, 40, 41]. A multidimensional understanding of service disengagement as proposed by Tindall et al. [41], for example, could have provided further useful insights. The authors suggest understanding engagement as a process incorporating different stages. In these, circumstances can push a person towards engagement (e.g., fear of relapse or a good relationship with the case manager), or pull them from engagement (e.g., not wanting to open up, or a change in case manager).
Interestingly, we found a significant association between the study inclusion date and drop-out/service disengagement. CHR-P patients who were included between 2009 and 2017 dropped out significantly more often than those included between 2000 and 2008. This might be due to changes in the study design applied in 2009. Specifically, whereas CHR-P patients with a low risk were followed-up three-monthly in the first year when included before 2009, they were followed up monthly (i.e., treated equally as high risk patients) when included after 2009. Additionally, in 2011, we implemented an e-mail reminder system to facilitate the management of follow-up time points for care givers. Our case managers set their schedule for follow-up visits according to weekly reminder e-mails, which might have resulted in patients being contacted more often and especially in shorter intervals. Moreover, starting in 2011, patients were asked to additionally participate in two further multicenter studies on the early detection and treatment of psychosis [31, 32, 42]. We, therefore, speculate that contacting patients too often or burdening them with too many assessments might lead to unintended effects, such as patients being annoyed by it and therefore disengaging from the clinical service. In line with this, some patients even declared being annoyed by requests for study participations when asked about a specific reason for service disengagement.
Although lack of insight has been associated with service disengagement in FEP patients, we could not find any such association in CHR-P patients. One possible explanation is that illness insight in CHR-P patients is relatively intact compared to FEP patients [43]. Accordingly, in our sample only 21.6% of CHR-P patients were considered to have lacking or questionable insight according to the BIP [24]. Therefore, it seems possible that insight does not play a major role in service disengagement in the at-risk population.
Contrary to our hypotheses, we could not demonstrate any association between cannabis consumption and study drop-out/service disengagement. Substance abuse and dependence are among the most robust predictors of disengagement in FEP patients, with cannabis use in particular increasing risk of disengagement [13]. Notably, although not significant, the association between cannabis use and service disengagement in our study was in the same direction as in studies with FEP patients. It might be possible that cannabis consumption only leads to service disengagement in combination with more severe symptoms in later stages of psychotic disorders [13]. Alternatively, our non-significant finding might also be the result of low statistical power, as only 14 of 53 patients with service disengagement reported cannabis use at baseline. Further studies addressing the association between cannabis use and disengagement in larger CHR-P patient samples are warranted.
Regarding baseline clinical and sociodemographic variables, there were almost no associations with study drop-out/service disengagement. These results are largely consistent with previous studies investigating study drop-out/service disengagement in CHR-P patients [8, 9, 12]. Regarding the lacking influence of negative symptoms, our results are consistent with those of a large study by Stowkowy et al. [8] in 764 CHR-P patients, although another study did report an association with service disengagement [9]. On the other hand, our finding that higher baseline disorganized symptoms significantly elevated disengagement risk was rather unexpected. The only available study that explicitly reported findings regarding disorganized symptoms in CHR-P patients [8] could not demonstrate an association with service disengagement. Our contrasting finding may be attributed to the use of different instruments assessing disorganized symptom severity and different methods of dealing with patients with a subsequent transition in the statistical analysis.
For the first time, we investigated whether a change in symptoms had occurred immediately before study drop-out. While positive symptoms and all other subscales from the BPRS had not significantly worsened, negative symptoms had significantly improved between the second-last and last assessment. Thus, it appears unlikely that patients disengaged from the service because of increased suspiciousness or a transition to psychosis. Our results rather suggest that an improvement of negative symptoms and thus better social functioning might lower the need for treatment, and thereby increases the likelihood of dropping out. Hence, the duration of follow-up might have been too long for patients experiencing significant symptomatic improvement during the follow-up, which might have artificially increased the drop-out rate at later follow-up time points. However, it should be emphasized that in our study, positive symptoms remained relatively stable from the second-last to last appointment. This indicates that at least some patients might still suffer from subthreshold psychotic symptoms at the time of disengagement and still be at-risk for psychosis. This would be in line with our recent ultra-long-term follow-up study, which showed that some patients still transit to psychosis after many years [44]. Hence, it might be difficult to strike the right balance between capturing late transitions and not imposing a burden on patients. It might, therefore, be prudent to extend follow-up visit intervals with increasing follow-up duration, as has already been done in this study, or to flexibly adapt the frequency and length of follow-ups according to the symptom severity.
Strengths and limitations
Strengths of this study were the longitudinal design and the application of competing risk survival models, which allowed us to take transition to psychosis and the time to event into account. Furthermore, we evaluated a large number of predictor variables, including cannabis use and illness insight, regarding their association with service disengagement in this specific patient group for the first time. Additionally, to the best of our knowledge, this study is the first to investigate changes in symptoms immediately before study drop-out.
A limitation of this study is that we did not assess further potential predictors previously associated with service disengagement in FEP patients such as forensic history [13, 14, 45] or therapeutic alliance and quality of the relationship with the case manager, which have earlier been described as vital engagement reasons [11, 41].
Conclusion
In conclusion, sociodemographic and clinical baseline variables in great part did not predict study drop-out/service disengagement during follow-up in CHR-P patients. However, we observed that patients with a later inclusion into our project were at significantly greater risk for study drop-out/service disengagement, which might have occurred because the patients were burdened with increased assessments during the later time period. Hence, our study provides a cautionary note on high frequency follow-up assessments in this specific patient group. Larger-scale studies using multidimensional assessments to evaluate predictors on multiple levels (e.g., clinical, sociodemographic, therapist) would help to further elucidate study drop-out and service disengagement in CHR-P patients.
References
Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jonsson B, Olesen J, Allgulander C, Alonso J, Faravelli C, Fratiglioni L, Jennum P, Lieb R, Maercker A, van Os J, Preisig M, Salvador-Carulla L, Simon R, Steinhausen HC (2011) The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol 21(9):655–679. https://doi.org/10.1016/j.euroneuro.2011.07.018
Riecher-Rössler A, McGorry PD (2016) Early detection and intervention in psychosis. In: Riecher-Rössler A, McGorry PD (eds) Early detection and intervention in psychosis: state of the art and future perspectives, vol 181. Karger Libri, Basel, pp 179–189
Hjorthøj C, Stürup AE, McGrath JJ, Nordentoft M (2017) Years of potential life lost and life expectancy in schizophrenia: a systematic review and meta-analysis. Lancet Psychiatry 4(4):295–301. https://doi.org/10.1016/S2215-0366(17)30078-0
Laursen TM (2019) Causes of premature mortality in schizophrenia: a review of literature published in 2018. Curr Opin Psychiatry 32(5):388–393. https://doi.org/10.1097/YCO.0000000000000530
McGorry PD, Hartmann JA, Spooner R, Nelson B (2018) Beyond the “at risk mental state” concept: transitioning to transdiagnostic psychiatry. World Psychiatry 17(2):133–142. https://doi.org/10.1002/wps.20514
Fusar-Poli P, Rocchetti M, Sardella A, Avila A, Brandizzi M, Caverzasi E, Politi P, Ruhrmann S, McGuire P (2015) Disorder, not just state of risk: meta-analysis of functioning and quality of life in people at high risk of psychosis. Br J Psychiatry 207(3):198–206. https://doi.org/10.1192/bjp.bp.114.157115
Riecher-Rössler A, Studerus E (2017) Prediction of conversion to psychosis in individuals with an at-risk mental state: a brief update on recent developments. Curr Opin Psychiatry 30(3):209–219. https://doi.org/10.1097/YCO.0000000000000320
Stowkowy J, Liu L, Cadenhead KS, Tsuang MT, Cannon TD, Cornblatt BA, McGlashan TH, Woods SW, Perkins DO, Seidman LJ, Walker EF, Bearden CE, Mathalon DH, Addington J (2018) Exploration of clinical high-risk dropouts. Schizophr Res 195:579–580. https://doi.org/10.1016/j.schres.2017.09.018
Hengartner MP, Heekeren K, Dvorsky D, Walitza S, Rossler W, Theodoridou A (2017) Checking the predictive accuracy of basic symptoms against ultra high-risk criteria and testing of a multivariable prediction model: evidence from a prospective three-year observational study of persons at clinical high-risk for psychosis. Eur Psychiatry 45:27–35. https://doi.org/10.1016/j.eurpsy.2017.05.026
Lal S, Malla A (2015) Service engagement in first-episode psychosis: current issues and future directions. Can J Psychiatry 60(8):341–345. https://doi.org/10.1177/070674371506000802
O’Brien A, Fahmy R, Singh SP (2009) Disengagement from mental health services. A literature review. Soc Psychiatry Psychiatr Epidemiol 44(7):558–568. https://doi.org/10.1007/s00127-008-0476-0
Green CE, McGuire PK, Ashworth M, Valmaggia LR (2011) Outreach and support in South London (OASIS). Outcomes of non-attenders to a service for people at high risk of psychosis: the case for a more assertive approach to assessment. Psychol Med 41(2):243–250. https://doi.org/10.1017/s0033291710000723
Doyle R, Turner N, Fanning F, Brennan D, Renwick L, Lawlor E, Clarke M (2014) First-episode psychosis and disengagement from treatment: a systematic review. Psychiatr Serv 65(5):603–611. https://doi.org/10.1176/appi.ps.201200570
Lau KW, Chan SKW, Hui CLM, Lee EHM, Chang WC, Chong CS, Lo WT, Chen EYH (2017) Rates and predictors of disengagement of patients with first-episode psychosis from the early intervention service for sychosis service (EASY) covering 15 to 64 years of age in Hong Kong. Early Interv Psychiatry. https://doi.org/10.1111/eip.12491
Solmi F, Mohammadi A, Perez JA, Hameed Y, Jones PB, Kirkbride JB (2018) Predictors of disengagement from early intervention in psychosis services. Br J Psychiatry 213(2):477–483. https://doi.org/10.1192/bjp.2018.91
Maraj A, Veru F, Morrison L, Joober R, Malla A, Iyer S, Shah J (2017) Disengagement in immigrant groups receiving services for a first episode of psychosis. Schizophr Res. https://doi.org/10.1016/j.schres.2017.07.054
Riecher-Rössler A, Gschwandtner U, Aston J, Borgwardt S, Drewe M, Fuhr P, Pfluger M, Radu W, Schindler C, Stieglitz RD (2007) The Basel early-detection-of-psychosis (FEPSY)-study—design and preliminary results. Acta Psychiatr Scand 115(2):114–125. https://doi.org/10.1111/j.1600-0447.2006.00854.x
Riecher-Rössler A, Pflueger MO, Aston J, Borgwardt SJ, Brewer WJ, Gschwandtner U, Stieglitz RD (2009) Efficacy of using cognitive status in predicting psychosis: a 7-year follow-up. Biol Psychiatry 66(11):1023–1030. https://doi.org/10.1016/j.biopsych.2009.07.020
Riecher-Rössler A, Aston J, Ventura J, Merlo M, Borgwardt S, Gschwandtner U, Stieglitz RD (2008) The Basel Screening Instrument for Psychosis (BSIP): development, structure, reliability and validity. Fortschr Neurol Psychiatr 76(4):207–216. https://doi.org/10.1055/s-2008-1038155
American Psychiatric Association (1987) Diagnostic and statistical manual of mental disorders DSM-III-R, 3rd edn. American Psychiatric Association, Washington, DC
Riecher-Rössler A, Gschwandtner U, Borgwardt S, Aston J, Pflüger M, Rössler W (2006) Early detection and treatment of schizophrenia: how early? Acta Psychiatr Scand 113(s429):73–80. https://doi.org/10.1111/j.1600-0447.2005.00722.x
Yung AR, Phillips LJ, McGorry PD, McFarlane CA, Francey S, Harrigan S, Patton GC, Jackson HJ (1998) Prediction of psychosis: a step towards indicated prevention of schizophrenia. Br J Psychiatry 172(Suppl 33):14–20
Peralta D, Studerus E, Andreou C, Beck K, Ittig S, Leanza L, Egloff L, Riecher-Rossler A (2018) Exploring the predictive power of the unspecific risk category of the Basel Screening Instrument for Psychosis. Early Interv Psychiatry. https://doi.org/10.1111/eip.12719
Riecher-Rössler A, Ackermann T, Uttinger M, Ittig S, Koranyi S, Rapp C, Bugra H, Studerus E (2015) The Basel Interview for Psychosis (BIP): structure, reliability and validity. Fortschr Neurol Psychiatr 83(2):99–108. https://doi.org/10.1055/s-0034-1398999
Andreasen NC (1989) The Scale for the Assessment of Negative Symptoms (SANS): conceptual and theoretical foundations. Br J Psychiatry Suppl 7:49–58
Ventura J, Lukoff D, Nuechterlein K, Liberman R, Green M, Shaner A (1993) Manual of the expaned brief psychiatric rating scale. Int J Methods Psychiatr Res 3:227–243
Shafer A, Dazzi F, Ventura J (2017) Factor structure of the Brief Psychiatric Rating Scale-Expanded (BPRS-E) in a large hospitalized sample. J Psychiatr Res 93:79–86. https://doi.org/10.1016/j.jpsychires.2017.05.011
Jones SH, Thornicroft G, Coffey M, Dunn G (1995) A brief mental health outcome scale-reliability and validity of the Global Assessment of Functioning (GAF). Br J Psychiatry 166(5):654–659
First MB, Spitzer RL, Gibbon M, Williams JB (2002) Structured clinical interview for DSM-IV-TR axis I disorders, research version, patient edn. SCID-I/P, New York, NY, pp 94–1
Gibbon M, Spitzer RL, Williams JB, Benjamin LS, First MB (1997) Structured clinical interview for DSM-IV Axis II personality disorders. American Psychiatric Press Inc, Washington, D.C.
Markulev C, McGorry PD, Nelson B, Yuen HP, Schäfer M, Yung AR, Thompson A, Berger G, Mossaheb N, Schlogelhofer M, Smesny S, de Haan L, Riecher-Rössler A, Nordentoft M, Chen EYH, Verma S, Hickie I, Amminger GP (2017) NEURAPRO-E study protocol: a multicentre randomized controlled trial of omega-3 fatty acids and cognitive-behavioural case management for patients at ultra high risk of schizophrenia and other psychotic disorders. Early Interv Psychiatry 11(5):418–428. https://doi.org/10.1111/eip.12260
McGorry PD, Nelson B, Markulev C, Yuen HP, Schäfer MR, Mossaheb N, Schlogelhofer M, Smesny S, Hickie IB, Berger GE, Chen EY, de Haan L, Nieman DH, Nordentoft M, Riecher-Rössler A, Verma S, Thompson A, Yung AR, Amminger GP (2017) Effect of omega-3 polyunsaturated fatty acids in young people at ultrahigh risk for psychotic disorders: the NEURAPRO randomized clinical trial. JAMA Psychiatry 74(1):19–27. https://doi.org/10.1001/jamapsychiatry.2016.2902
R Development Core Team (2017) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Kim HT (2007) Cumulative incidence in competing risks data and competing risks regression analysis. Clin Cancer Res 13(2 Pt 1):559–565. https://doi.org/10.1158/1078-0432.CCR-06-1210
Kleinbaum DG, Klein M (2001) Survival analysis a self-learning text
Stowkowy J, Addington D, Liu L, Hollowell B, Addington J (2012) Predictors of disengagement from treatment in an early psychosis program. Schizophr Res 136(1–3):7–12. https://doi.org/10.1016/j.schres.2012.01.027
Anderson KK, Fuhrer R, Schmitz N, Malla AK (2013) Determinants of negative pathways to care and their impact on service disengagement in first-episode psychosis. Soc Psychiatry Psychiatr Epidemiol 48(1):125–136. https://doi.org/10.1007/s00127-012-0571-0
Chan TC, Chang WC, Hui CL, Chan SK, Lee EH, Chen EY (2014) Rate and predictors of disengagement from a 2-year early intervention program for psychosis in Hong Kong. Schizophr Res 153(1–3):204–208. https://doi.org/10.1016/j.schres.2014.01.033
Schimmelmann BG, Conus P, Schacht M, McGorry P, Lambert M (2006) Predictors of service disengagement in first-admitted adolescents with psychosis. J Am Acad Child Adolesc Psychiatry 45(8):990–999. https://doi.org/10.1097/01.chi.0000223015.29530.65
Becker KD, Buckingham SL, Rith-Najarian L, Kline ER (2016) The Common Elements of treatment engagement for clinically high-risk youth and youth with first-episode psychosis. Early Interv Psychiatry 10(6):455–467. https://doi.org/10.1111/eip.12283
Tindall R, Francey S, Hamilton B (2015) Factors influencing engagement with case managers: perspectives of young people with a diagnosis of first episode psychosis. Int J Ment Health Nurs 24(4):295–303. https://doi.org/10.1111/inm.12133
European Network of National Networks studying Gene-Environment Interactions in S, van Os J, Rutten BP, Myin-Germeys I, Delespaul P, Viechtbauer W, van Zelst C, Bruggeman R, Reininghaus U, Morgan C, Murray RM, Di Forti M, McGuire P, Valmaggia LR, Kempton MJ, Gayer-Anderson C, Hubbard K, Beards S, Stilo SA, Onyejiaka A, Bourque F, Modinos G, Tognin S, Calem M, O’Donovan MC, Owen MJ, Holmans P, Williams N, Craddock N, Richards A, Humphreys I, Meyer-Lindenberg A, Leweke FM, Tost H, Akdeniz C, Rohleder C, Bumb JM, Schwarz E, Alptekin K, Ucok A, Saka MC, Atbasoglu EC, Guloksuz S, Gumus-Akay G, Cihan B, Karadag H, Soygur H, Cankurtaran ES, Ulusoy S, Akdede B, Binbay T, Ayer A, Noyan H, Karadayi G, Akturan E, Ulas H, Arango C, Parellada M, Bernardo M, Sanjuan J, Bobes J, Arrojo M, Santos JL, Cuadrado P, Rodriguez Solano JJ, Carracedo A, Garcia Bernardo E, Roldan L, Lopez G, Cabrera B, Cruz S, Diaz Mesa EM, Pouso M, Jimenez E, Sanchez T, Rapado M, Gonzalez E, Martinez C, Sanchez E, Olmeda MS, de Haan L, Velthorst E, van der Gaag M, Selten JP, van Dam D, van der Ven E, van der Meer F, Messchaert E, Kraan T, Burger N, Leboyer M, Szoke A, Schurhoff F, Llorca PM, Jamain S, Tortelli A, Frijda F, Vilain J, Galliot AM, Baudin G, Ferchiou A, Richard JR, Bulzacka E, Charpeaud T, Tronche AM, De Hert M, van Winkel R, Decoster J, Derom C, Thiery E, Stefanis NC, Sachs G, Aschauer H, Lasser I, Winklbaur B, Schlogelhofer M, Riecher-Rössler A, Borgwardt S, Walter A, Harrisberger F, Smieskova R, Rapp C, Ittig S, Soguel-dit-Piquard F, Studerus E, Klosterkotter J, Ruhrmann S, Paruch J, Julkowski D, Hilboll D, Sham PC, Cherny SS, Chen EY, Campbell DD, Li M, Romeo-Casabona CM, Emaldi Cirion A, Urruela Mora A, Jones P, Kirkbride J, Cannon M, Rujescu D, Tarricone I, Berardi D, Bonora E, Seri M, Marcacci T, Chiri L, Chierzi F, Storbini V, Braca M, Minenna MG, Donegani I, Fioritti A, La Barbera D, La Cascia CE, Mule A, Sideli L, Sartorio R, Ferraro L, Tripoli G, Seminerio F, Marinaro AM, McGorry P, Nelson B, Amminger GP, Pantelis C, Menezes PR, Del-Ben CM, Gallo Tenan SH, Shuhama R, Ruggeri M, Tosato S, Lasalvia A, Bonetto C, Ira E, Nordentoft M, Krebs MO, Barrantes-Vidal N, Cristobal P, Kwapil TR, Brietzke E, Bressan RA, Gadelha A, Maric NP, Andric S, Mihaljevic M, Mirjanic T (2014) Identifying gene-environment interactions in schizophrenia: contemporary challenges for integrated, large-scale investigations. Schizophr Bull 40(4):729–736. https://doi.org/10.1093/schbul/sbu069
Lappin JM, Morgan KD, Valmaggia LR, Broome MR, Woolley JB, Johns LC, Tabraham P, Bramon E, McGuire PK (2007) Insight in individuals with an at risk mental state. Schizophr Res 90(1–3):238–244. https://doi.org/10.1016/j.schres.2006.11.018
Beck K, Studerus E, Andreou C, Egloff L, Leanza L, Simon AE, Borgwardt S, Riecher-Rössler A (2019) Clinical and functional ultra-long-term outcome of patients with a clinical high risk (CHR) for psychosis. Eur Psychiatry 62:30–37. https://doi.org/10.1016/j.eurpsy.2019.08.005
Conus P, Lambert M, Cotton S, Bonsack C, McGorry PD, Schimmelmann BG (2010) Rate and predictors of service disengagement in an epidemiological first-episode psychosis cohort. Schizophr Res 118(1–3):256–263. https://doi.org/10.1016/j.schres.2010.01.032
Acknowledgements
We thank all patients who participated in the study as well as the referring specialists.
Funding
This project was supported by Grants of the Swiss National Science Foundation (nos. 3200-057 216.99, 3200-0572 216.99, PBBSB-106 936, and 3232BO-119 382) and the Nora van Meeuwen-Haefliger Stiftung, Basel (CH). These institutions had no further role in the study design; collection, analysis and interpretation of data; in the writing of the report and in the decision to submit the paper for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Leanza, L., Studerus, E., Mackintosh, A.J. et al. Predictors of study drop-out and service disengagement in patients at clinical high risk for psychosis. Soc Psychiatry Psychiatr Epidemiol 55, 539–548 (2020). https://doi.org/10.1007/s00127-019-01796-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-019-01796-6