Abstract
Purpose
We examine the impact of including subthreshold disorders on estimating psychiatric morbidity burden in adolescents. To more fully understand this burden it is important to focus on both full syndrome and subthreshold disorders and the impairment associated with each, since evidence suggests prevalence of subthreshold disorders is substantial as is impairment.
Methods
Data were analyzed from a probability sample of 4,175 youths 11–17 years of age. We examine the prevalence of DSM-IV disorders (FS) and subthreshold (SUB) disorders, with and without impairment. Diagnostic categories examined were anxiety, mood, attention deficit hyperactivity disorder, disruptive, and substance use disorders in the past year.
Results
The prevalence of any FS disorders was 16.1 and 42.3 % for SUB. The combined prevalence was 58.4 %. By requiring impairment, the prevalence of any FS in the past year dropped to 8 % and for SUB to 15.7 %, with a combined overall rate of 23.7 %. For FS disorders, 49.6 % met criteria for moderate to severe impairment, compared to 37.8 % for SUB. One in four adolescents had either an FS or SUB disorder with impairment.
Conclusion
The results indicate that SUB disorders constitute a major public health burden in terms of psychiatric morbidity among adolescents. Given their substantial impairment and their high prevalence, consideration should be given to including SUB disorders in estimates of the public health burden psychiatric morbidity. Doing so would provide a more accurate estimate of psychiatric morbidity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
What is the burden of psychiatric disorders among adolescents? The aggregate burden of mental illness worldwide is estimated at 7.4 % of the world’s measureable burden of disease [1]. Major depression is the second leading cause of years living with disability (YLD) worldwide and ranks among the four largest contributors to YLDs [2]. The combined burden of YLDs attributed to mental and behavioral disorders (21.7 %) is higher than from any other disease category [2]. However, these are estimates of mental illness burden derived from many sources [3]. The only direct estimates of the prevalence, severity, and need for treatment for mental disorders have come from the WHO World Mental Health Surveys [4]. These surveys focused on adults sampled from 14 countries in the Americas, Europe, the Middle East, Africa, and Asia.
None of these estimates of global burden of disease focus specifically on mental disorders or psychiatric morbidity in children and adolescents [2–6]. Thus far, there have been no world mental health surveys of children and adolescents, nor are the estimates of YLDs for mental illness disaggregated for children and adolescents in the Global Burden of Disease 2010 Study. Evidence used to assess burden has generally focused on the prevalence of psychiatric disorders estimated for youths who meet DSM diagnostic criteria for one (or more) specific diagnoses (i.e., not including the “not otherwise specified” or subthreshold presentations). Such studies have been carried out in North Carolina, Texas, and Puerto Rico [7–9]. Without consideration of impairment, the 12-month prevalence of any disorder was 17.1 % in North Carolina for 9- to 17-year-olds, 17.7 % in Texas for 11- to 17-year-olds, and 17.3 % in Puerto Rico for 4- to 17-year-olds. Each of these studies used an omnibus interview administered by lay interviewers to assess DSM diagnoses.
Two national surveys, the National Health and Nutrition Examination Survey (NHANES) [10] and the National Comorbidity Survey Replication Adolescent Supplement (NCS-A) [11] have estimated the prevalence of psychiatric disorders among youths with divergent results. In part, the differences are due to the variations between the studies in the number of diagnoses assessed and the age composition of the study samples. The two studies also used different interview schedules and different informants (parent or youth). Using data from the 2001–2004 NHANES, Merikangas et al. [12] reported the 12-month prevalence of any disorder as 13.1 % for 8- to 15-year-olds. Kessler et al. [13] using data from the NCS-A reported a 12-month prevalence of 42.6 % for any disorder in 13- to 17-year-olds.
Taking impairment into account directly addresses the issue of severity of the disorder [13–16]. Many studies report prevalence rates for full syndrome diagnoses with and without consideration of, or adjustment for, impairment. DSM guidelines for most diagnoses specify that symptoms must cause significant impairment in social, academic, or other important areas of functioning as a necessary criterion [17]. Studies by Roberts, Roberts and Xing [18], Canino et al. [9], and Shaffer et al. [16] each showed a linear, stepwise decrease in prevalence rates among youths as one moves from prevalence of diagnoses unadjusted for impairment to those adjusted for diagnostic specific impairment and to those adjusted for global measures of impairment. In earlier work, we found prevalence rates of psychopathology in adolescents of 5–11 %, depending on the impairment criteria applied [19]. Costello et al. [20] found a median prevalence rate across studies of youths of 5.4 % for any psychiatric disorder when adjusted for impairment. Kessler et al. [13] estimated the prevalence of serious emotional disturbance [21] as 8.0 %, e.g., youths who had at least 1 DSM-IV psychiatric disorder in the past 12 months and a CGAS score of 50 or less. Merikangas et al. [22], using data from the NCS-A study, found a lifetime prevalence of 49.5 % for one or more DSM-IV disorders and 22.2 % adjusted for severe impairment. There is further evidence to suggest that youths with substantial impairment from symptoms (i.e., impairing subthreshold disorders) are as impaired as those who meet full diagnostic criteria but without impairment [23].
Another way to define the burden of psychiatric morbidity is to include subthreshold disorders (i.e., SUB, disorders that fall short of the number and/or duration of symptoms required by DSM to assign a diagnosis) in the prevalence estimates [23]. Research suggests that subthreshold disorders are common among adolescents [24], are precursors in adolescence for full syndrome disorders in adulthood [25], and are associated with functional impairment [26]. Copeland et al. [27] report similar results focusing on not otherwise specified (NOS) conditions in youth, e.g., substantial prevalence rates and levels of impairment as well as increased risk for young adult disorders. The prevalence of subthreshold disorders among adolescents appears to be much higher than that of full syndrome disorders, particularly for mood, anxiety, and disruptive disorders [24]. There remains the question of whether combining full syndrome and subthreshold disorders may provide a more accurate picture of the burden of psychiatric morbidity.
To our knowledge, only one previous study [24] has reported data on the prevalence of DSM subthreshold disorders across a range of disorders among adolescents. Their results suggest that the burden of subthreshold disorders among youths is substantial, with 52 % having at least one subthreshold disorder. These investigators did not specifically estimate the combined prevalences of full syndrome and subthreshold disorders, although perusal of their data suggests the total burden to be well in excess of double the full syndrome prevalence rate; nor did they examine impairment associated with subthreshold disorders as compared to full syndrome disorders. We submit that to understand the burden of psychiatric morbidity more fully, it is important to focus on both full syndrome (FS) and subthreshold disorders (SUB) as well as the impairment associated with each.
In DSM-IV, with very few exceptions, the same rules are used for youth as for adults for assigning a diagnosis. In addition to providing additional evidence of the burden of psychiatric disorder, studying subthreshold disorders may help clarify the validity of diagnoses as defined by DSM-IV and applied to youth. DSM-IV (and now, DSM-5) implies that SUB conditions do not reflect the same phenomena as full syndrome ones [28]. For example, regarding construct validity, if subthreshold disorders are associated with similar correlates and similar levels of impairment, then they may not represent categorically different constructs, but perhaps a more quantitative difference driven by somewhat arbitrary definitions of caseness [29]. If so, perhaps SUB (by DSM rules) or at least SUB who have impairment should be considered to be cases of psychiatric disorder for estimating morbidity burden.
The purpose of this research is to further examine SUB disorders among adolescents, comparing SUB prevalence with FS prevalence, and then estimating burden combining the prevalence of SUB and FS disorders using data from Teen Health 2000 (TH2 K). We also examine the impact on prevalence of combining DSM-IV defined diagnoses with impairment with the prevalence of SUB with impairment as possibly representing a more accurate estimate of burden. We are the first to do so.
Materials and methods
The sample was selected from households in the Houston metropolitan area enrolled in local health maintenance organizations with oversampling for African-American and Latino households. One youth, age 11–17 years, was sampled from each eligible household. Sample weights were adjusted by post-stratification to reflect the age, ethnic, and gender distribution of the 5-county Houston metropolitan area in 2000 [30].
Data were collected at baseline from sample youths and from one adult caregiver for each using computer-assisted personal interviews and self-administered questionnaires. The computerized interview contained the structured psychiatric interview (see below), demographic data on the youths and the household as well as queries about stress exposure. The interviews were conducted by trained, lay interviewers. The questionnaires contained questions on a broad array of risk and protective factors. Interviews and questionnaires were completed with 4,175 youths (66 % of those eligible) at baseline. All youths and parents gave written informed consent prior to participation in this study. All study forms and procedures were approved by the University of Texas Health Sciences Center Committee for Protection of Human Subjects and the New York State Psychiatric Institute Institutional Review Board. Sample characteristics are presented in Table 1.
Psychiatric disorders among youths were assessed using the Diagnostic Interview Schedule for Children (DISC-IV), a highly structured instrument [31], comprising two parallel forms: DISC-Y, which is administered directly to children ages 9–17 years to assess youths’ symptoms and behaviors; and DISC-P, which is administered to parents (caretakers) about the youths 6–17 years [31]. In the current report, we include data from the youth interview only. The full DISC includes over 30 DSM-IV diagnoses organized into diagnostic modules. At the end of each module, information about impairment (5 question sets) and distress (1 question set) caused by symptoms reported, age of onset of possible disorder, and receipt of or recognized need for treatment is collected.
In TH2K, all youth were interviewed about disruptive disorders, mood disorders, anxiety disorders, eating disorders, and substance use disorders. Specific disorders examined were attention deficit–hyperactivity disorder (ADHD), oppositional defiant disorder (ODD), conduct disorder (CD), major depressive episode (MDE), dysthymic disorder (DD), manic/hypomanic episode (MA–HM), generalized anxiety disorder (GAD), social phobia, panic, agoraphobia (AG), post-traumatic stress disorder (PTSD), eating disorder, and substance disorders (alcohol abuse or dependence considered as a single disorder (AL), cannabis abuse or dependence (MJ) and other substance (as a group) abuse or dependence (OTH drug). Our measure of presence of DSM-IV emotional or behavioral disorder used the DISC definition for disorder in the previous 12 months (Version N algorithms).
In defining a subthreshold disorder (SUB), we applied the rule used in the DISC that determines whether the interviewer asks questions about age of onset, impairment, and treatment; these questions typically are asked if the respondent has endorsed half (or more) of the criteria required for diagnosis. By disorder, these specific rules are as follows: ADHD: three inattention or three hyperactivity/impulsivity criteria; ODD: two criteria; CD: two criteria; MDE: concurrent criteria for 2 weeks, one of which must be mood or anhedonia; DD: mood for 1 year and one other symptom, MA–HM: mood for 4 days or hospitalization and two other symptoms coincident with mood change; GAD: one or more situations in which there is unrealistic or excessive anxiety and a period where youth was worried at least 4 days a week and one or more somatic symptoms on most days for 6 months; social phobia: embarrassed in social situation and two other symptoms; panic disorder: had a panic attack; AG: one or more situations in which youth had agoraphobic fear and either avoided going into a situation by themselves or remained nervous or upset the whole time when in a situation; PTSD: had trauma and endorsed three or more symptom criteria. For each of the substance disorders, SUB diagnoses were assigned if two dependence criteria were endorsed (note: for abuse, only one criterion is required for an FS diagnosis). Prevalence rates for FS used any FS diagnosis assigned for any diagnosis being examined and no SUB was assigned for that diagnosis. Likewise, SUB was assigned for a disorder as long as criteria were not met for an FS for that disorder. Comorbidity was not examined. We were interested in estimating the prevalence of FS and SUB and comparing them across diagnostic categories. SUB diagnoses were not assigned if the youth met the DISC definition for that full disorder.
To define “impairment” for each diagnosis, we applied the DISC impairment algorithm that requires moderate impairment in at least two areas of functioning or distress, or severe impairment or distress in at least one area.
We present results from three sets of analyses. In the first, we compare the prevalence of FS and SUB diagnoses. Subsequently, we examine rates of DISC-defined impairment (as described above) in the two groups and compare the differences in these rates (X 2 test). The Ns vary across diagnoses due to missing data. We removed from analyses any cases with missing data that prevented us from making a definitive designation. For example, when assessing FS and SUB with impairment, we dropped subjects who met diagnostic criteria, but did not have data on impairment. This also was the case for broader diagnostic categories, such as “any mood”. In this example, if any of the mood diagnoses were missing, then the umbrella diagnosis was also missing unless one of the other mood disorders was positive, in which instance we could make a positive determination. The actual sample sizes used in Table 2 vary from 4,170 to 4,175, so bias if any was trivial. Finally, we calculated the prevalence of those who had either an FS (regardless of impairment) or SUB with impairment for each diagnosis. SAS release 9.2 [32] was used for statistical analyses.
Results
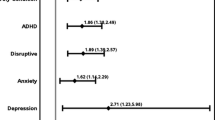
Table 2 contains data on prevalence of FS and SUB diagnoses. The prevalence of having at least one DSM-IV FS disorder (any disorder) in the last year was 16.1 %; and prevalence of having at least one SUB disorder was 42.3 % (column 2 and 3, row 5). The ratio of FS/SUB was 2.6, meaning that for every youth with an FS disorder, at least 2.6 youths met criteria for a SUB disorder (column 4, row 5). Combining FS and SUB yielded a prevalence of 58.4 % (column 5, row 5). Requiring impairment lowered these rates considerably: to 8.0 % for FS and 15.7 % for SUB (column 7 and 8, row 5), with a combined prevalence of 23.7 % and a somewhat lower FS/SUB ratio of 2.
Considering the broad categories of diagnoses (disruptive, mood, anxiety, and substance), the prevalence of SUB was substantially higher than that of FS definitions, for all but the substance disorders. For the substance use disorders, there were very few SUB diagnoses. For anxiety disorders, the prevalence of SUB, at 36.5 %, was five times that of FS disorder, for disruptive disorders, the prevalence of SUB was 0.4 %, only 1/10 that for FS; and for mood disorder, SUB (7.2 %) was over three times more prevalent than FS. Excluding the substance use disorders, there were only three specific disorders—conduct disorder, dysthymia, and agoraphobia where the rate of SUB was not at least double that of FS disorder; in most instances, the prevalence of SUB was six or more times greater than that of FS. Simply adding FS and SUB together yields very high prevalence, with well over half (59.4 %) of this community sample qualifying for either an FS or SUB diagnosis. Again, the highest rates were for anxiety disorders followed by disruptive, and then mood disorders, with little increase in the substance use disorders.
Looking at the last row of Table 2, adding the requirement of impairment lowered both the FS and SUB rates substantially: the overall rate of any FS disorder decreased by half, to 8.0 %. Looking across the broad categories for FS disorders, the largest decrease (36.4 to 5.9 or 72 %) was for anxiety disorders and substance disorders (1.4 to 0.1 or 75 %). Adding impairment had much less of an impact on decreasing the prevalence for disruptive and mood disorders—which decreased by 30 and 24 %, respectively.
Again, looking at the last row in Table 2 for the broad groups of any disruptive, any mood or any anxiety disorder, youth who met an FS disorder were significantly more likely to report impairment than youth who met a SUB disorder (all p < 0.0001). For the substance use disorders, where the number of youth fulfilling criteria was much lower, the difference did not reach significance. An examination by diagnosis revealed that although fewer youth with SUB reported impairment than those with FS in every instance; this difference was not significant for conduct disorder, generalized anxiety disorder, or agoraphobia.
Considering individual disorders, among disruptive disorders, the prevalence of FS CD without taking impairment into account was slightly higher than that of ODD. However, CD had the lowest prevalence of SUB and the lowest ratio of SUB/FS disorder, with or without impairment, while ODD had the highest prevalence of SUB (much higher than SUB CD) and the highest ratio of SUB/FS. For mood disorders, MDD had a similar pattern to CD, while mania was more similar to ODD. In the case of anxiety disorders, panic had the lowest prevalence of SUB and lowest ratio of SUB/FS disorder, with or without consideration of impairment. Social phobia had, by far, the highest prevalence for SUB, regardless of impairment, and the highest SUB/FS ratio of the anxiety disorders. Substance use disorder, whether for alcohol or marijuana use, had extremely low rates of SUB, with or without impairment, and the prevalence of FS were much higher compared to SUB than for the other disorders.
Finally, defining disorder as meeting FS criteria (without considering impairment) or meeting SUB criteria plus impairment (“Alternative Definition of Disorder”) produced an overall prevalence of any disorder of 32.1 %, nearly double the rate of FS (16.1 %). Disruptive disorders had the highest prevalence (19.9 % rather than 6.4 % for FS), followed by anxiety disorders (13.1 vs. 7.2 % for FS), mood (5.1 vs. 2.1 % for FS) and substance (4.4 vs. 4.3 % for FS). Except for the substance use disorders, all of these increases were statistically significant (all p < 0.0001).
Discussion
Combining FS with impairment and SUB with impairment yielded an overall prevalence for at least one disorder in the past year of nearly 24, 8 % for FS and almost 16 % for SUB. The combined rates were 17.9 % for any disruptive disorder, 7.9 % for any anxiety disorder, 4.6 % for any mood disorder, and 1.6 % for any substance disorder. The ratios of SUB to FS taking impairment into account were 3.03 for any disruptive disorder, 2.9 for any anxiety disorder, 0.05 for substance disorder, and 2.00 overall, meaning the prevalence of FS with impairment was twice as high as SUB with impairment. Still, 37.8 % of SUB had impairment compared with 49.6 % of FS. The prevalence rates for any FS disorder are in line with those reported elsewhere using these data [30, 33] as well as in other studies of adolescents [9, 12] using similar assessment methods, and is comparable to that reported by Angold et al. [7] for the Great Smoky Mountain Study. The prevalence of FS with impairment (7.4 %) was also comparable to that reported for NOS by Angold [7] and to the NCS-A definition of SED (8.0 %). Our prevalence of any SUB in the past year (42.3 %) was somewhat lower than that reported by Lewinsohn et al. [24] in the OADP study, which reported a SUB prevalence of 52.1 %.
Because the SUB definitions differed, perhaps the most useful way to compare results from these two studies is to examine the ratio of SUB to FS disorders. Although Lewinsohn et al. [24] did not present these data, these ratios can be calculated from their data. With the exception of MDD, substance use, and CD, the ratios in TH2K are dramatically higher than in OADP. The ratios in OADP are 1.41 for MDD, 1.99 for anxiety disorders, 2.88 for alcohol, 1.00 for substance use, 1.97 for CD, and 1.88 for ADHD. Our ratios were 2.18, 5.06, 0.18, 0.04, 1.47, and 6.71, respectively. What might account for these differences, beyond difference in time, places, and populations?
A major difference between our study and OADP was how SUB disorders were defined. For example, we defined SUB ADHD as either three inattention or three hyperactivity/impulsivity criteria, while the OADP required any five symptoms of any type. Thus, our definition is less restrictive. For anxiety disorders, in OADP the SUB definition used was any three symptoms across panic, agoraphobia, social phobia, OCD, separation anxiety, and overanxious disorders. In TH2K, the anxiety disorders included were somewhat different and the symptom thresholds were higher and set individually by diagnoses. For substance use disorders, our SUB criteria were much more restrictive. OADP defined SUB depression as mood or anhedonia plus two other symptoms, while in TH2K it was more restrictive: mood or anhedonia plus three other symptoms, all co-occurring and present for at least 2 weeks. Finally for OADP, only one symptom is required for SUB substance use disorder.
Other factors may account for these differences. The OADP sample was essentially all white American in ethnic origin, while our sample was over half African-American or Latino American. We used the DISC-IV, a highly structured interview, administered by lay interviews, which adheres very specifically to DSM-IV diagnostic criteria, with specific questions to address each part of a criterion, whereas in Oregon, the K-SADS, a semi-structured instrument somewhat less specific, was administered by clinicians. In addition, for OADP, diagnoses and SUB diagnoses categories were defined using DSM-III-R diagnostic criteria, while TH2 K used DSM-IV criteria.
Taken together, it is clear that differences in sample composition, procedures, definitions of SUB, and case ascertainment preclude drawing clear conclusions based on direct comparisons of our data with the only other population-based, epidemiologic study of adolescents which has examined prevalence of subthreshold disorders [24]. However, we would argue that direct comparisons, while they are useful, are not the main message here. The more important message worth noting is that SUB disorders are highly prevalent in adolescents (regardless of how SUB diagnoses are defined), much more prevalent than FS disorders, involve considerable impairment, and thus constitute a significant morbidity burden in their own right. When combined with FS disorders, the magnitude of the overall morbidity is striking.
Even adjusting for functional impairment, the additional burden imposed by subthreshold disorders remains high, for most specific disorders and for any disorder. Overall, one in four adolescents had either an FS or SUB disorder with impairment.
Following Helzer and Hudziak [29], it is clear that levels of impairment are lower for SUB than for FS disorders, in general. However, substantial impairment is associated with SUB disorders. For example, 76 % of FS mood disorders and 42 % of SUB mood disorders had moderate to severe impairment. For disruptive disorders, the rates were 70 % for FS and 56 % for SUB. We submit that this is clear evidence that SUB disorders are associated with impairment, but that impairment is more strongly associated with FS disorders. Thus, from this perspective, the data provide support for the validity of DSM-IV diagnoses [28, 29]. That is, DSM assumes “cases” to be more serious and more impairing than “noncases.” However, the proportion of any FS disorder with impairment was 49.6 %, compared to 37.8 % for any SUB disorder, tempering this conclusion somewhat, e.g., more impairment is still associated with FS disorders.
Our study of adolescents is the first to examine the argument by Angold et al. [22] that youths who do not meet DSM diagnostic criteria for an FS disorder but who have impairment perhaps, should be considered cases of psychiatric disorder, albeit milder cases. Clearly, our results and those of Lewinsohn et al. [24] indicate that combining SUB and FS diagnoses greatly expands our estimate of “burden.” This suggests that the usual fourfold table (diagnosis/no diagnosis and impaired/nonimpaired) used either explicitly or implicitly in psychiatric research should be modified. One recommendation would be to expand caseness categories to include diagnosis/subthreshold diagnosis/no diagnosis categories as well as severe impairment/moderate impairment/mild to no impairment in terms of functioning. This would provide more nuanced and precise estimates of burden and perhaps intervention strategies based on epidemiologic definitions of caseness. It should be noted that Carpenter and van Os [34] have discussed the utility and desirability of a diagnosis of subthreshold psychosis, with diagnostic criteria, designated attenuated psychosis syndrome. The key to the clinical utility of such SUB diagnosis is whether they can be made reliably and have predictive validity.
We should comment on our results for substance disorders, for which the results are very different from those of other disorders. FS disorder prevalence was much higher than for SUB, and thus the SUB/FS ratios were less than one. These results are the result of DSM criteria and our definition of SUB disorders. That is, in our sample the majority of youths who had symptoms met DSM-IV criteria for substance use dependence or abuse. Many fewer met the definition for SUB. One interpretation is that most youths who abuse substances meet the duration, frequency, and severity criteria and thus are FS as opposed to SUB criteria.
Our study had other limitations. We were able to complete assessments with only 66 % of those sampled at baseline, raising the possibility of nonresponse bias. We have carefully examined potential biases from these design characteristics in previous publications [30, 33] and demonstrated that bias from these sources was minimal. For example, we have examined the effect of attrition on rates of suicidal behaviors, psychiatric disorders, and other mental health indicators and found no significant effects. Further evidence is provided by highly comparable overall prevalence rates in North Carolina and Puerto Rico [7, 9]. We should note that the response rate for adolescents in the NCS-A at 75 % was higher [11].
Another potential issue is that we did not include data from parent reports of symptoms, outcomes, or predictors (with the exception of family income). (We only interviewed parents about ADHD, behavioral disorders, and substance use disorders). While there is argument that data from multiple informants are desirable, many studies attest to considerable discordance in parent–child reports of psychopathology and functioning [35]. In a previous paper, we have demonstrated substantial differences in parent–child concordance across ethnic groups, such that minority parents reported fewer problems but there were no differences among youths across ethnic groups [35]. This suggests that reliance on youth reports may be less problematic than use of parent reports, particularly for major depression. We should note that the original OADP study also relied only on youth reports of psychiatric problems [24, 36, 37].
In this paper, we did not examine comorbidity of SUB disorders. The available data indicate that comorbidity is substantial between FS and SUB disorders as well as between SUB disorders [24], this comorbidity aggregates in families [38], and homotypic as well as heterotypic continuity (comorbidity) occurs with SUB and FS disorders in youths over time [25, 39]. That will be the basis of future work using these data.
Based on results from TH2K and earlier study by Lewinsohn et al. [24], it is clear that SUB among adolescents constitutes a major source of morbidity in terms of psychiatric morbidity. For any SUB, the prevalence was 42.3 %. Thus, over half of the sample met diagnostic criteria for either SUB or FS disorder [24]. By any measure, this estimate of disease burden is substantial.
Our estimates of burden, combining FS and SUB with impairment, in concert with other epidemiologic surveys cited earlier, suggest that as high as one in four youths suffer from impairing psychiatric morbidity. This further suggests that the global burden of such morbidity may be at least as high as for adults and therefore one of the leading causes of YLDs for adolescents, along with accidents and suicide. But the true burden of mental disorders in adolescents, as well as for children, is unknown for most countries in the world [40].
The policy implications of including SUB with impairment are profound, from both the perspective of estimating need for mental health services and the costs of providing such services [2, 5, 6, 41]. Beyond the policy and treatment implications, there also are implications concerning issues of etiology. That is, are the risk or protective factors similar or dissimilar between FS and SUB? Further, are the natural histories of FS and SUB similar or dissimilar? From a clinical perspective, the treatment implications clearly are important. SUB psychiatric disorders are much more prevalent, even with impairment, suggesting a clear potential for much greater need for mental health care. This is accompanied by access issues, in particular insurance coverage for SUB in addition to FS disorders; SUB disorders currently are not covered in many insurance plans.
To expand this line of inquiry, we are focusing on two lines of research: examining differences across subgroups in FS and SUB disorders, defined by age, gender, ethnic status, and socioeconomic status, and examining risk factors for incidence of SUB disorders. Following the strategy used in an earlier paper focusing on incidence and prospective predictors of first incidence of FS disorders [41], we also are examining the incidence and predictors of SUB using the same set of predictors or risk and protective factors used in an earlier study. Epidemiologically, observations of dissimilar patterns of risk factors would further support the validity of DSM-IV (and by extension, DSM-5) FS disorders in terms of lack of construct validity; similar risk factor patterns for SUB disorders would not, suggesting that the two are epidemiologically and perhaps etiologically similar.
References
Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C et al (2012) Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859):2197–2223
Becker AE, Kleinman A (2013) Mental health and the global agenda. N Engl J Med 369(1):66–73
Murray CJ, Lopez AD (2013) Measuring the global burden of disease. N Engl J Med 369(5):448–457
Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP et al (2004) Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA J Am Med Assoc 291(21):2581–2590
Patel V, Flisher AJ, Hetrick S, McGorry P (2007) Mental health of young people: a global public-health challenge. Lancet 369(9569):1302–1313
Collins PY, Patel V, Joestl SS, March D, Insel TR, Daar AS et al (2011) Grand challenges in global mental health. Nature 475(7354):27–30
Angold A, Erkanli A, Farmer EM, Fairbank JA, Burns BJ, Keeler G, Costello EJ (2002) Psychiatric disorder, impairment, and service sse in rural african american and white youth. Arch Gen Psychiatry 59(10):893–901
Roberts RE, Roberts CR, Xing Y (2006) Prevalence of youth-reported dsm-iv psychiatric disorders among African, European, and Mexican American adolescents. J Am Acad Child Adolesc Psychiatry 45(11):1329–1337
Canino G, Shrout PE, Rubio-Stipec M, Bird HR, Bravo M, Ramirez R, Chavez L, Alegria M, Bauermeister JJ, Hohmann A, Ribera J, Garcia P, Martinez-Taboas A (2004) The DSM-IV rates of child and adolescent disorders in Puerto Rico: prevalence, correlates, service use, and the effects of impairment. Arch Gen Psychiatry 61(1):85–93
National Center for Health Statistics (2007) National Health and Nutrition Examination Survey Questionnaire, Laboratory Protocol, and Exam Protocol. http://www.cdc.gov/nchs/about/major/nhanes/nhanes01-02.htm/ Accessed 14 January 2013
Kessler RC, Avenevoli S, Costello EJ, Green JG, Gruber MJ, Heeringa S, Merikangas KR, Pennell BE, Sampson NA, Zaslavsky AM (2009) National comorbidity survey replication adolescent supplement (NCS-A): II. Overview and design. J Am Acad Child Adolesc Psychiatry 48(4):380–385
Merikangas KR, He JP, Brody D, Fisher PW, Bourdon K, Koretz DS (2010) Prevalence and treatment of mental disorders among US children in the 2001–2004 NHANES. Pediatrics 125(1):75–81
Kessler RC, Avenevoli S, Costello J, Green JG, Gruber MJ, McLaughlin KA, Petukhova M, Sampson NA, Zaslavsky AM, Merikangas KR (2012) Severity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication Adolescent Supplement. Arch Gen Psychiatry 69(4):381–389
Costello EJ, Angold A, Burns BJ, Stangl DK, Tweed DL, Erkanli A, Worthman CM (1996) The Great Smoky Mountains Study of Youth. Goals, design, methods, and the prevalence of DSM-III-R disorders. Arch Gen Psychiatry 53(12):1129–1136
Ford T, Goodman R, Meltzer H (2003) The British Child and Adolescent Mental Health Survey 1999: the prevalence of DSM-IV disorders. J Am Acad Child Adolesc Psychiatry 42(10):1203–1211
Shaffer D, Fisher P, Dulcan MK, Davies M, Piacentini J, Schwab-Stone ME, Lahey BB, Bourdon K, Jensen PS, Bird HR, Canino G, Regier DA (1996) The NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3): description, acceptability, prevalence rates, and performance in the MECA Study. Methods for the Epidemiology of Child and Adolescent Mental Disorders Study. J Am Acad Child Adolesc Psychiatry 35(7):865–877
American Psychiatric Association (2000) Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR (Text Revision), Fourth Edition edn. American Psychiatric Association, Washington
Roberts RE, Roberts CR, Xing Y (2007) Rates of DSM-IV psychiatric disorders among adolescents in a large metropolitan area. J Psychiatr Res 41(11):959–967
Roberts RE, Attkisson CC, Rosenblatt A (1998) Prevalence of psychopathology among children and adolescents. Am J Psychiatry 155(6):715–725
Costello EJ, Messer SC, Bird HR, Cohen P, Reinherz HZ (1998) The prevalence of serious emotional disturbance: a re-analysis of community studies. J Child Fam Stud 7(4):411–432
Substance Abuse and Mental Health Services Administration (1993) (Final notice establishing definitions for (1) children with a serious emotional disturbance, and (2) adults with a serious mental illness). Fed Regist 58(96):29422–29425
Angold A, Costello EJ, Farmer EM, Burns BJ, Erkanli A (1999) Impaired but undiagnosed. J Am Acad Child Adolesc Psychiatry 38(2):129–137
Pincus HA, LE McQueen, Elinson L (2003) Subthreshold mental disorders: Nosological and research recommendations. In: Phillips KA, First MB, Pincus HA (eds) Advancing DSM: Dilemmas in psychiatric diagnosis. American Psychiatric Association, Washington, pp 129–144
Lewinsohn PM, Shankman SA, Gau JM, Klein DN (2004) The prevalence and co-morbidity of subthreshold psychiatric conditions. Psychol Med 34(4):613–622
Shankman SA, Lewinsohn PM, Klein DN, Small JW, Seeley JR, Altman SE (2009) Subthreshold conditions as precursors for full syndrome disorders: a 15-year longitudinal study of multiple diagnostic classes. J Child Psychol Psychiatry 50(12):1485–1494
Kessler RC, Zhao S, Blazer DG, Swartz M (1997) Prevalence, correlates, and course of minor depression and major depression in the National Comorbidity Survey. J Affect Disord 45(1–2):19–30
Copeland W, Shanahan L, Costello EJ, Angold A (2011) Cumulative prevalence of psychiatric disorders by young adulthood: a prospective cohort analysis from the Great Smoky Mountains Study. J Am Acad Child Adolesc Psychiatry 50(3):252–261
Fechner-Bates S, Coyne JC, Schwenk TL (1994) The relationship of self-reported distress to depressive disorders and other psychopathology. J Consult Clin Psychol 62(3):550–559
Helzer JE, Hudziak JJ (2008) Defining Psychopathology in the 21st Century: DSM-V and Beyond. American Psychiatric Publishing Inc, Washington
Roberts RE, Roberts CR (2007) Ethnicity and risk of psychiatric disorder among adolescents. Res Hum Dev 4(1–2):89–118
Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME (2000) NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry 39(1):28–38
SAS Institute Inc (2009) What’s New in SAS® 9.2. SAS Institute Inc, Cary
Roberts RE, Roberts CR, Chan W (2009) One-year incidence of psychiatric disorders and associated risk factors among adolescents in the community. J Child Psychol Psychiatry 50(4):405–415
Carpenter WT, van Os J (2011) Should attenuated psychosis syndrome be a DSM-5 diagnosis? Am J Psychiatry 168(5):460–463
Roberts RE, Alegria M, Roberts CR, Chen IG (2005) Concordance of reports of mental health functioning by adolescents and their caregivers: a comparison of European, African and Latino Americans. J Nerv Ment Dis 193(8):528–534
Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA (1993) Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-r disorders in high school students. J Abnorm Psychol 102(1):133–144
Lewinsohn PM, Clarke GN, Seeley JR, Rohde P (1994) Major depression in community adolescents: age at onset, episode duration, and time to recurrence. J Am Acad Child Adolesc Psychiatry 33(6):809–818
Shankman SA, Klein DN, Lewinsohn PM, Seeley JR, Small JW (2008) Family study of subthreshold psychopathology in a community sample. Psychol Med 38(2):187–198
Costello EJ, Copeland W, Angold A (2011) Trends in psychopathology across the adolescent years: what changes when children become adolescents, and when adolescents become adults? J Child Psychol Psychiatry 52(10):1015–1025
Eisenberg L, Belfer M (2009) Prerequisites for global child and adolescent mental health. J Child Psychol Psychiatry 50(1–2):26–35
Kakuma R, Minas H, van Ginneken N, Dal Poz MR, Desiraju K, Morris JE, Saxena S, Scheffler RM (2011) Human resources for mental health care: current situation and strategies for action. Lancet 378(9803):1654–1663
Acknowledgments
This research was supported, in part, by Grant Nos. MH 49764 and MH 65606 from the National Institutes of Health awarded to the first author, by the Michael and Susan Dell Center for Healthy Living, and by the University of Texas. Work on this paper was supported by Grant No. MHI85150 awarded to the second and third authors and by Columbia University and New York State Psychiatric Institute.
Conflict of interest
There are no potential conflicts of interest for any author. Catherine R. Roberts, Ph.D., the University of Texas School of Medicine (retired) assisted in the design and conduct of the study and collection and management of the data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Roberts, R.E., Fisher, P.W., Blake Turner, J. et al. Estimating the burden of psychiatric disorders in adolescence: the impact of subthreshold disorders. Soc Psychiatry Psychiatr Epidemiol 50, 397–406 (2015). https://doi.org/10.1007/s00127-014-0972-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-014-0972-3