Abstract
Background
Sleep problems may lead to, or be symptomatic of, depression and other mental illnesses yet few studies have investigated their association with suicide risk.
Design
Prospective cohort study.
Setting
Taiwan.
Participants
393,983 men and women aged 20 or above participating in the MJ health check-up programme.
Results
There were 335 suicides over a mean of 7.4 years follow-up. There was a reverse J-shaped association between sleep duration and suicide risk. When compared with those sleeping 6–8 h per night the adjusted hazard ratios (95 % confidence intervals) for suicide associated with 0–4, 4–6 and >8 h sleep were 3.5 (2.0–6.1), 1.5 (1.1–1.9) and 1.5 (1.1–2.0), respectively. People requiring sleeping pills to get to sleep (1.2 % participants) were at over 11-fold increased risk; difficulty falling asleep (11.5 % participants), frequent dreaming (16.7 %) and being easily awoken (30.6 %) were associated with a 2.0-, 1.6- and 1.3-fold increased risk of suicide, respectively.
Conclusions
Less than 6 h sleep duration, sleep disturbances and reported use of sleep medicines are markers of suicide risk. Sleep problems should be assessed when evaluating suicide risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Disturbed or excessive sleep is a common feature of many psychiatric disorders as well as being a relatively frequent experience in the general population with a prevalence of 10–30 % [18]. There is evidence that sleep disturbance may also be important in the aetiology of depression. In a 4-year follow-up of people without depression and not taking antidepressants at baseline, insomnia symptoms were associated with a two- to fivefold increased risk of depression [24]. In another study, both trouble falling asleep and sleeping too much at baseline were found to be associated with increased risk of depression 1 year later [21].
There has been growing interest in the usefulness of symptoms of sleep disturbance in suicide risk assessment. Studies dating back over 30 years have found that amongst people with psychiatric illness, sleep disturbance distinguishes those who go on to kill themselves from non-suicides [1]. However, relatively few studies have investigated the association of sleep disturbance with suicide in general population samples. In a general population cohort from Finland, there was a graded association between the frequency of nightmares and suicide risk; other aspects of sleep disturbance were not investigated [26]. In a US study of older people living in the community, poor sleep quality was shown to be associated with increased risk of suicide [27]. A Japanese prospective study found a twofold increased risk of suicide in people reporting difficulties maintaining sleep, but no associations with difficulties with sleep initiation or early morning waking [11]. A recent prospective study of a French occupational cohort showed a fivefold increase in suicide risk amongst men with three or more sleep disturbances; the risk remained highly elevated even after adjusting for depression [22]. Another recent study based on a Norwegian population cohort reported a twofold increased risk of suicide amongst people experiencing sleep problems almost every night, when baseline anxiety and depression symptoms were controlled for [2]. However, none of these prospective studies have investigated the association of sleep duration with risk of suicide [2, 11, 22, 26, 27].
To clarify the importance of sleep and sleep patterns in the aetiology of suicide, we have investigated the association of self-reported sleep duration and sleep problems with suicide in a large cohort of Taiwanese men and women.
Methods
Participants
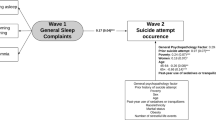
The study cohort is based on the records of approximately 540,000 Taiwanese adults aged 20 years or above who underwent health check-ups using a standard protocol between 1994 and 2008 (Fig. 1) [7, 29]. The check-up programme is run by a private company, the MJ Health Management Institution, Taiwan (https://www.mjclinic.com.tw). Since 1996 these check-ups have included questions about sleep; this analysis is based on the 393,983 (73 %) participants who attended check-ups between 1996–2008 and who have full information on sleep duration, sleep problems and potential confounding variables including sociodemographic and life style factors. A subset of participants (39 %) has attended the clinics more than once, but our analysis is restricted to data recorded at the first attendance. From 1998, the baseline questionnaire started to include questions about the use of medicines and 293,673 (75 % of 393,983) participants had full information (Fig. 1). The study participants had given written consent for the use of their data from the health check-up for research. The study was approved by the National Health Research Institutes, Taiwan, and the MJ Health Management Institution.
Sleep assessment
Participants completed two questions concerning their sleep: (1) “How long do you sleep for?”—there were four response categories: (a) <4 h; (b) 4–6 h; (c) 6–8 h and (d) >8 h and (2) “How have you slept in the past month?”—there were five response categories: (a) I had difficulties falling asleep, (b) I had no problem falling asleep, but was easily awoken, (c) I dreamt a lot, (d) I needed sleeping pills and (e) I slept well.
Possible confounding factors
Data on the following possible confounding factors were also recorded at baseline: education (middle school or below, high school, junior college, college or higher), marital status (single, married, divorced or separated, widowed), smoking (never, former, current), alcohol consumption (no or occasional use, former drinking, regular drinking), physical activity (inactive, low, moderate or high), and the use of psychotropic drugs and sedatives/hypnotics (daily use or not). Participants’ weight (to the nearest 0.1 kg) and height (to the nearest mm) were measured using an auto-anthropometer, Nakamura KN-5000A (Nakamura, Tokyo, Japan); their body mass index (BMI) were calculated (kg/m2), and its sex-specific z score was calculated as the number of standard deviations above (positive values) or below (negative values) the mean.
Ascertainment of suicide mortality
The vital status of all study participants was obtained through linkage of the cohort national identification numbers with Taiwan’s national cause-of-death register, which records the date of death and the underlying cause of death, coded using the International Classification of Diseases, Ninth Revision (ICD-9). ICD-9 codes used to identify suicides were E950–E959. Previous research has shown that, in keeping with patterns seen in the West, many deaths coded as undetermined whether deliberately or purposely inflicted (E980–E989), accidental pesticide poisoning (E863) and accidental suffocation (E913) are likely to be misclassified suicides [6]. We therefore included these latter deaths within our definition of suicide. In a sensitivity analysis, we included certified suicides coded as E950–E959 only.
Statistical analysis
We used Cox proportional hazards models to investigate the association of sleep with suicide mortality. Time at entry was the date of recruitment; time of exit was December 31, 2008 or the date of death if earlier. All analyses in this study were conducted using SAS software, version 9.1 (SAS Institute).
We carried out analyses in three steps. In our initial models, we estimated the association of sleep with suicide controlling for age (in 5 year groups) and sex only. We then examined the impact on the associations of controlling for the potential confounding factors listed above, except medicine use. Both BMI (z (standard deviation) score) and its quadratic term were modelled as a previous study showed a quadratic relationship of BMI with suicide (i.e. suicide risk increased in both underweight and very obese individuals) [7]. Third, we additionally included use of medicines (sedatives/hypnotics and psychotropic drugs) in the models; these variables may act as confounders or mediators because their use could influence the effect of sleep problems and, possibly, reduce the risk of suicide if they are effective in overcoming sleeping problems. This analysis was based on a subsample of the MJ participants with complete information on medicine use.
We investigated whether associations differed in men and women by fitting appropriate interaction terms and conducting likelihood ratio tests in which models with and without interaction terms were compared. Likewise, as poor sleep is more frequent in older individuals (and may be considered an accompaniment of aging), we investigated whether associations differed in those above or below 45 years of age. We also investigated whether there was a linear association of sleep duration with suicide by carrying out likelihood ratio tests in which models with the sleep duration variable as a linear term and a categorical term were compared. To examine any quadratic relationship, we also included a quadratic term for this variable in separate models. The proportional hazards assumption was examined by plotting Schoenfeld residuals with time and examining their correlation. We found no strong evidence for the violation of the assumption.
Psychiatric disorders could confound the association of sleep with suicide as they may cause both sleep problems and suicide. To assess their possible impact on the associations of our exposures with suicide, we conducted a sensitivity analysis by excluding all suicides occurring in the first 2 years of follow-up as these participants’ sleep patterns were more likely to be influenced by any psychiatric disorders at baseline.
Results
Participant characteristics
Altogether there were 190 male and 145 female suicides over a mean of 7.4 years follow-up amongst the 393,983 participants. The average time period between sleep data collection and suicide death was 5.6 years. The crude male suicide rate was 13.3 per 100,000 per year and the female rate was 9.8 per 100,000 per year. Table 1 shows the characteristics of the participants. In the subsample with complete data on medicine use (n = 293,673), there was 94 male and 76 female suicides over a mean of 5.9 years follow-up; the crude suicide rates were 11.2 per 100,000 for males and 8.6 per 100,000 for females. In this subsample, female participants were more likely than males to report daily use of sedatives/hypnotics (1.8 vs. 1.0 %) and psychotropic drugs (0.8 vs. 0.6 %). When compared with the total sample, participants of this subsample were slightly younger (39.4 vs. 40.2 years) but had similar sex composition (males 49.3 vs. 49.5 %).
Sleep duration and suicide
Around 20 % of participants slept for <6 h a day and around 10 % for more than 8 h; these figures were similar for both males and females (Table 1). There was a reverse J-shaped association of sleep duration with suicide risk—there was strong evidence for a non-linear or quadratic association (Table 2). In the total sample with sleep information both short (<6 h) and long (>8 h) sleep durations were associated with an increased risk of suicide. When compared with those sleeping 6–8 h per night age- and sex-adjusted hazard ratios (HRs) for suicide associated with 0–4, 4–6 and >8 h sleep were 4.1 [95 % confidence intervals (CI) 2.4–7.1], 1.5 (95 % CI 1.2–2.0) and 1.8 (95 % CI 1.3–2.4), respectively. The association was somewhat attenuated in models controlling for social class and behavioural risk factors. In the subsample with information on medicine use, when additionally controlling for the use of psychotropic drugs and sedatives/hypnotics the increased risk associated with 0–4 h sleep was attenuated by about one-third, but there was little impact on the increased risk associated with 4–6 h sleep; prolonged sleep was not associated with suicide risk in this sub-sample (Table 3).
Flow chart of participants of the MJ health check-up program, Taiwan, 1994–2008. aData for participants with complete information on sleep and potential confounding variables, used in the main multivariable analyses. From 1996 the program included a self-completed questionnaire to collect information on socio-demographic and health-related factors, including sleep variables. bData used in sensitivity analyses additionally controlling for psychotropic drug and use of sedatives/hypnotics. From 1998 the questionnaire contained questions on the use of medicines, including psychotropic drugs and sedatives/hypnotics
There was weak evidence that associations of sleep duration with suicide differed in males and females (p(interaction) = 0.061, fully adjusted model in the total sample), but no evidence was found for differences between the younger and older participants (p(interaction) = 0.88). The main sex difference was in relation to the increased risk of suicide amongst those sleeping 4–6 h—an increase in risk was seen in males, but not females (Table 4).
Sleep problems and suicide
The most frequently reported sleep problems were being easily awoken (30.6 %) and frequent dreaming (16.7 %), followed by difficulty falling asleep (11.5 %) and the need for sleeping pills (1.2 %). These measures of sleep problems were associated with increased suicide risk, in particular the need for sleeping pills (age- and sex-adjusted HR 14.2, 95 % CI 9.5–21.1) (Table 2). These associations weakened to some extent after controlling for potential confounders.
There was no strong evidence for sex differences in the association of suicide with sleep problems (p(interaction) = 0.30, fully adjusted model in the total sample), whilst there was some weak evidence that the associations differed in young versus older participants (p(interaction) = 0.10). Amongst participants aged <45 years, in the fully adjusted models based on the data for the total sample with information on sleep, difficulty falling asleep (HR 1.8, 95 % CI 1.1–2.9), frequent dreaming (HR 1.6, 95 % CI 1.0–2.5) and the need for sleeping pills (HR 17.9, 95 % CI 9.9–32.4) were all strongly associated with increased suicide risk (Table 4). In older participants aged ≥45 years, risks associated with difficulty falling asleep and frequent dreaming were similar to those seen in young participants, whilst the need for sleeping pills was associated with less increased risk (HR 8.0, 95 % CI 4.6–13.8).
Overall, the results were similar when restricting analyses to certified suicides only (i.e. excluding deaths of undetermined intent) or excluding all suicides occurring in the first 2 years after baseline measurements (data not shown).
Sleep and all-cause mortality
Altogether 9,873 cohort participants died from all causes, including suicide, over the follow-up period. Associations of sleep patterns with all-cause mortality were considerably lower than those for suicide. When compared with those sleeping 6–8 h per night the fully adjusted hazard ratios for all cause mortality associated with 0–4, 4–6 and >8 h sleep were 1.4 (95 % CI 1.2–1.6), 1.0 (95 % CI 1.0–1.1) and 1.4 (95 % CI 1.3–1.4), respectively. When compared with those reporting no sleeping problems risk of death from all-causes in relation to difficulty falling asleep, being easily awoken, dreaming a lot and the need for sleeping pills were 1.3 (1.2–1.3), 1.1 (1.0–1.1), 1.0 (0.9–1.1) and 1.5 (1.4–1.7), respectively.
Discussion
This is the largest study to investigate the association of sleep with suicide risk. We found a strong, revere J-shaped association between sleep duration and suicide. Risks were generally similar in men and women and in those aged <45 and >45 years. The greatest risks were seen amongst the small number of participants (1.0 % of cohort members) who slept less than 4 h (HR 3.5). Nineteen percent of participants slept between 4–6 h and they too had an increased risk of suicide, although this increase was seen in males only (HR 1.8). The lowest risks were seen amongst the 70 % of participants, who slept 6–8 h per night. Similar patterns were seen for all-cause mortality, but risks were much lower.
Approximately 1 % of participants reported requiring sleeping pills to help them sleep—these participants were at over tenfold increased risk of suicide, these risks were higher in younger than older cohort members. Approximately 10 % of participants reported difficulties getting to sleep—such difficulties were also associated with an approximately twofold increase in suicide risk.
Strengths and limitations
The main strengths of this study are its large size (>390,000 participants), the record of sleep duration as well as an indication of participants’ specific sleep problems. Furthermore, the detailed information collected at baseline enabled us to assess the impact on the observed associations of a range of possible confounding factors. However, the lack of a formal psychiatric assessment meant we were unable to determine the extent to which the sleep–suicide associations resulted from pre-existing psychiatric illness. We used information on whether participants were taking psychotropic medication at baseline (0.7 % of participants) as a crude indicator of psychiatric illness and the strengths of most associations weakened, but remained considerable in relation to short sleep duration, after controlling for this proxy indicator.
Further limitations of the study were the absence of a measure of early morning wakening and difficulty getting back to sleep, both of which are common features of depression [21]. Furthermore, the questions concerning sleep problems allowed only one response; thus subjects with more than one difficulty (e.g. both having difficulty getting to sleep and being easily awoken) were unable to record the range of their problems. Information on sleep was recorded as a one-off measure at baseline only and it is likely that participant’s sleep patterns changed over the follow-up period; however, our checks of the proportional hazards assumption found no evidence that the hazard ratios associated with sleep disturbance differed over the follow-up period. Although the study cohort came from a slightly more advantaged socioeconomic background compared to Taiwan’s general population, other characteristics such as smoking in this cohort was similar to that shown in a national survey [28] and suicide rate in this cohort was only slightly lower than that for Taiwan’s population (11.7 vs. 12.5 per 100,000) [25]. Selection bias is not generally a problem in cohort studies unless associations between exposure and outcome differ in cohort members as compared to the general population.
Findings in the context of previous research
Suicide is a major cause of potentially preventable mortality accounting for approximately 1 million deaths worldwide every year. In many industrialized countries suicide is the most frequent cause of death in young men. Despite this high burden, our understanding of its aetiology is limited. Although serious psychiatric disorders; particularly depression, psychosis and substance misuse—underlie many suicides, most people with these conditions do not take their lives. Key factors in the clinical assessment of psychiatric disorder are a past history of self-harm and serious suicidal thoughts. Other factors are less well characterized. Emerging data indicate that sleep disturbances may not only be associated with an increased risk of suicide, but also that amongst individuals with psychiatric disorder sleep disturbance may be an additional indicator of suicide risk: recent studies have reported associations of sleep problems with suicidal thoughts [3, 20], suicide attempts [3, 5, 20] and suicide [2, 22] that are independent of measures of psychiatric symptoms.
Our findings of an increased risk of suicide in relation to frequent dreaming are consistent with those from a cohort of Finnish men and women, amongst whom those who experienced frequent nightmares had a twofold increased suicide risk as compared to those who did not [26]. We are not aware of previous investigations of the association between sleep duration and suicide—although in the long-term follow-up of the American Cancer Society cohort associations with suicide mortality were reported as being similar to those seen for all-cause mortality—an increased risk was seen amongst those with both short <7 and long >8 h sleep as compared to individuals who slept 7–8 h [14]. A recent meta-analysis also reported increased risks of all-cause mortality amongst those who both sleep little (odds ratio 1.12) and those with excessive sleep (odds ratio 1.30) [4]. In keeping with this several recent cross-sectional studies showed that short [10, 13, 15, 17] or long [10] sleep durations were associated with increased suicidal thoughts or acts.
Possible explanations for associations
Several possible explanations have been suggested for the association of sleep disturbance with suicide risk. First, it could be due to uncontrolled confounding by co-existing psychiatric disorders. However, as described above, studies that have controlled for measures of psychiatric illness and substance misuse in multivariable models find relatively strong independent associations of sleep with suicidal thoughts and behaviours. As the associations have been reported in a number of well-conducted studies using prospective designs with measures of sleep patterns recorded well before suicide, it seems unlikely that the findings are due to biases inherent in the study design/exposure or outcome measurement.
If the associations of sleep with suicide are real, a number of possible biological pathways may contribute to the observed patterns of risk. Sleep deprivation is thought to increase the risk of impulsive and aggressive behaviour in adolescence, both of which are risk factors for suicide [8]. Second, rather than simply being a symptom of psychiatric disorder, sleep disturbance may also be a risk factor for the development of mental illness, which in turn is strongly associated with suicide risk and such a bi-directional relationship between sleep disturbance and psychiatric disorder has been suggested in several recent studies [21, 23, 24]. In keeping with a possible causal effect of disturbed sleep on mood, a recent study carried out amongst school age adolescents found that those whose parents set earlier bed times had lower levels of depression [12]. Lastly, sleep disturbances affect a number of endocrine and metabolic pathways, including those involving cortisol, leptin and ghrelin and it is possible that perturbations in these pathways impact on suicide risk [9].
There is no clear explanation for the heightened risk of suicide amongst those who sleep for >8 h. Hypersomnia is a feature of depression in some people and this may contribute to the observed patterns.
Implications
Further research is required before the implications for these findings can be translated into clinical advice and such research could usefully include follow-up studies with more detailed measures of incident psychiatric illness, to allow the relative impact of sleep on their incidence and vice versa to be distinguished. Furthermore, studies are required to better understand the mechanisms underlying the associations of prolonged sleep with suicide. It is uncertain from the present analysis whether pharmacological treatment of sleep disorders reduces the risk of depression and suicide although such an impact has been suggested in previous studies [2]. Further research in this area is required [19]. Recent work showing the beneficial impact on mental health of parental regulation of adolescents’ bed time may provide useful information for parenting classes and the prevalence of mental disorder in childhood [12]. Lastly, it is possible that disturbed sleep may help distinguish psychiatric patients at high from those at low risk of suicide [16], although more research is required to test this possibility.
References
Barraclough BM, Pallis DJ (1975) Depression followed by suicide: a comparison of depressed suicides with living depressives. Psychol Med 5:55–61
Bjorngaard JH, Bjerkeset O, Romundstad P, Gunnell D (2011) Sleeping problems and suicide in 75,000 Norwegian adults: a 20 year follow-up of the HUNT I study. Sleep 34:1155–1159
Brower KJ, McCammon RJ, Wojnar M, Ilgen MA, Wojnar J, Valenstein M (2011) Prescription sleeping pills, insomnia, and suicidality in the National Comorbidity Survey Replication. J Clin Psychiatry 72:515–521
Cappuccio FP, D’Elia L, Strazzullo P, Miller MA (2010) Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep 33:585–592
Carli V, Roy A, Bevilacqua L, Maggi S, Cesaro C, Sarchiapone M (2011) Insomnia and suicidal behaviour in prisoners. Psychiatry Res 185:141–144
Chang SS, Sterne JA, Lu TH, Gunnell D (2010) ‘Hidden’ suicides amongst deaths certified as undetermined intent, accident by pesticide poisoning and accident by suffocation in Taiwan. Soc Psychiatry Psychiatr Epidemiol 45:143–152
Chang SS, Wen CP, Tsai MK, Lawlor DA, Yang YC, Gunnell D (2012) Adiposity, its related biologic risk factors, and suicide: a cohort study of 542,088 Taiwanese adults. Am J Epidemiol 175:804–815
Dahl RE, Lewin DS (2002) Pathways to adolescent health sleep regulation and behavior. J Adolesc Health 31:175–184
Ferrie JE, Kumari M, Salo P, Singh-Manoux A, Kivimaki M (2011) Sleep epidemiology—a rapidly growing field. Int J Epidemiol 40:1431–1437
Fitzgerald CT, Messias E, Buysse DJ (2011) Teen sleep and suicidality: results from the youth risk behavior surveys of 2007 and 2009. J Clin Sleep Med 7:351–356
Fujino Y, Mizoue T, Tokui N, Yoshimura T (2005) Prospective cohort study of stress, life satisfaction, self-rated health, insomnia, and suicide death in Japan. Suicide Life Threat Behav 35:227–237
Gangwisch JE, Babiss LA, Malaspina D, Turner JB, Zammit GK, Posner K (2010) Earlier parental set bedtimes as a protective factor against depression and suicidal ideation. Sleep 33:97–106
Goodwin RD, Marusic A (2008) Association between short sleep and suicidal ideation and suicide attempt among adults in the general population. Sleep 31:1097–1101
Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR (2002) Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry 59:131–136
Liu X (2004) Sleep and adolescent suicidal behavior. Sleep 27:1351–1358
McCall WV, Blocker JN, D’Agostino R Jr, Kimball J, Boggs N, Lasater B, Rosenquist PB (2010) Insomnia severity is an indicator of suicidal ideation during a depression clinical trial. Sleep Med 11:822–827
McKnight-Eily LR, Eaton DK, Lowry R, Croft JB, Presley-Cantrell L, Perry GS (2011) Relationships between hours of sleep and health-risk behaviors in US adolescent students. Prev Med 53:271–273
Ohayon MM (2002) Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev 6:97–111
Pigeon WR, Caine ED (2010) Insomnia and the risk for suicide: does sleep medicine have interventions that can make a difference? Sleep Med 11:816–817
Ribeiro JD, Pease JL, Gutierrez PM, Silva C, Bernert RA, Rudd MD, Joiner TE Jr (2012) Sleep problems outperform depression and hopelessness as cross-sectional and longitudinal predictors of suicidal ideation and behavior in young adults in the military. J Affect Disord 136:743–750
Roberts RE, Shema SJ, Kaplan GA, Strawbridge WJ (2000) Sleep complaints and depression in an aging cohort: a prospective perspective. Am J Psychiatry 157:81–88
Rod NH, Vahtera J, Westerlund H, Kivimaki M, Zins M, Goldberg M, Lange T (2010) Sleep disturbances and cause-specific mortality: results from the GAZEL cohort study. Am J Epidemiol 173:300–309
Staner L (2010) Comorbidity of insomnia and depression. Sleep Med Rev 14:35–46
Szklo-Coxe M, Young T, Peppard PE, Finn LA, Benca RM (2010) Prospective associations of insomnia markers and symptoms with depression. Am J Epidemiol 171:709–720
Taiwan Suicide Prevention Center (2010) Trends in suicide rates in Taiwan, 1994–2009. http://www.tspc.doh.gov.tw/tspc/portal/know/index.jsp?type=2 (Accessed 25 Jan 2011)
Tanskanen A, Tuomilehto J, Viinamaki H, Vartiainen E, Lehtonen J, Puska P (2001) Nightmares as predictors of suicide. Sleep 24:844–847
Turvey CL, Conwell Y, Jones MP, Phillips C, Simonsick E, Pearson JL, Wallace R (2002) Risk factors for late-life suicide: a prospective, community-based study. Am J Geriatr Psychiatry 10:398–406
Wen CP, Levy DT, Cheng TY, Hsu CC, Tsai SP (2005) Smoking behaviour in Taiwan, 2001. Tob Control 14:i51–i55
Wen CP, Wai JP, Tsai MK, Yang YC, Cheng TY, Lee MC, Chan HT, Tsao CK, Tsai SP, Wu X (2011) Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet 378:1244–1253
Acknowledgments
This study is supported in part by Taiwan Department of Health Clinical Trial and Research Center of Excellence (DOH102-TD-B-111-004). Professor David Gunnell is a UK National Institute for Health Research Senior Investigator. Dr. Shu-Sen Chang’s fellowship at the University of Bristol was funded by the National Science Council, Taiwan (NSC-98-2917-I-564-162). Dr. Shu-Sen Chang was supported by the Hong Kong Research Grants Council (RCG) General Research Fund (HKU784210M and HKU784012M). We thank the institutional support from the National Health Research Institutes, Taiwan. The views in this manuscript are those of the authors and not necessarily any funding bodies or of the MJ Health Management Institution.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gunnell, D., Chang, SS., Tsai, M.K. et al. Sleep and suicide: an analysis of a cohort of 394,000 Taiwanese adults. Soc Psychiatry Psychiatr Epidemiol 48, 1457–1465 (2013). https://doi.org/10.1007/s00127-013-0675-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-013-0675-1