Abstract
Purpose
To estimate the disease burden due to 15 mental disorders at both individual and population level.
Methods
Using a population-based survey (Nemesis, N = 7,056) the number of years lived with disability per one million population were assessed. This was done with and without adjustment for comorbidity.
Results
At individual level, major depression, dysthymia, bipolar disorder, panic disorder, social phobia, eating disorder and schizophrenia are the disorders most markedly associated with health-related quality of life decrement. However, at population level, the number of affected people and the amount of time spent in an adverse health state become strong drivers of population ill-health. Simple phobia, social phobia, depression, dysthymia and alcohol dependence emerged as public health priorities.
Conclusions
From a clinical perspective, we tend to give priority to the disorders that exact a heavy toll on individuals. This puts the spotlight on disorders such as bipolar disorder and schizophrenia. However, from a public health perspective, disorders such as simple phobia, social phobia and dysthymia—which are highly prevalent and tend to run a chronic course—are identified as leading causes of population ill-health, and thus, emerge as public health priorities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mental disorders are gradually moving up to the higher levels in the hierarchy of leading causes of population ill-health [1–4]. For example, a study looking at the main contributors of years lived with disability found that the top-5 was composed of mental disorders, neurological and sense organ disorders, chronic respiratory diseases, diabetes mellitus and cardiovascular disease [3]. Nevertheless, many countries are still dedicating only a small fraction of their health-care budget to mental disorders [5, 6]. This is unlikely to be a rational manner of resource allocation. Continuation of these policies is expected to increase rather than bridge the mental health gap [5, 7], since today’s societies, with mostly knowledge-, service- and innovation-driven economies, are exerting pressure on the cognitive, social and creative skills of people, and these pressures are unlikely to decrease in the near future. At the same time, the current economies would benefit from a mentally fit and resilient population successfully engaged in today’s economies. These important issues should place burden of disease studies with a focus on mental health in the limelight of attention of policy makers across sectors such as health, social affairs, employment and education.
Our study differs from previous burden of disease studies in several ways. We estimate the burden of disease stemming from 15 DSM-III-R mental disorders and express burden of disease in terms of non-fatal disease burden, i.e. the number of years lived with disability (YLD). The YLD estimates are based on a representative population-based psychiatric survey in the Netherlands, allowing us to correct the YLD estimate for one disorder for existing comorbidities with other mental disorders or somatic illnesses. Previous burden of disease studies were mostly based on the assessment of medical experts, whereas in our research, we base our results on how the general population values the health states across a range of mental disorders and somatic illnesses. Furthermore, burden of disease will be described at both the individual (per-person) level and population level. It will be shown that ranking the disorders by disability leads to different hierarchies when taking the clinical perspective on individuals or a public health perspective on populations. A clear distinction between both perspectives is important to accurately inform decision makers, clinicians and researchers in the health care sector such that the efforts to scale up and improve the mental health services can be undertaken in a substantiated way.
Materials and methods
Sample
We used the data of the Netherlands Mental Health Survey and Incidence Study (Nemesis). This study has been described in detail elsewhere [8]. In brief, a random, stratified, multistage sample was obtained in three steps in 1996. First, municipalities were stratified by urbanisation, and 90 municipalities were drawn randomly and proportionately from these strata. Second, within each municipality, households were randomly drawn from the postal register. Finally, within each household, the person with the most recent birthday was selected on condition that he or she was aged between 18 and 65 years and was sufficiently fluent in Dutch to be interviewed. Eligible persons who were not immediately available were contacted later in the year. The response rate was 69.7 %, resulting in a sample of 7,076 people. For 20 people (0.3 %), the disability weight could not be computed and the effective sample size was, therefore, 7,056. The sample followed the same multivariate distribution over age, gender, civil status and urbanisation as the general Dutch population; however, males in the age group of 18–24 years were slightly underrepresented.
Measures
Demographics include gender, age, partner status, level of education, and employment status (working at least 8 h per week in a paid job).
Mental disorders were assessed with the Dutch 1.1 version of the Composite International Diagnostic Interview (CIDI), which was developed by the World Health Organization for use by trained interviewers who are not clinicians [9, 10]. The CIDI is a computerized psychiatric interview and generates 1-month, 1-year and life-time prevalence rates of the DSM-III-R axis-I mental disorders. WHO field trials have documented acceptable reliability and diagnostic validity [11]. To be better able to study comorbidity and its effects on the disease burden, we used the CIDI without imposing the rules for the hierarchy among the disorders, meaning that if a person manifests with two disorders, for example, both a depression and schizophrenia, we count this as two distinct disorders, and not as a single disorder (a depression as part of schizophrenia).
Somatic illnesses were self-reported by the respondents. Examples included chronic obstructive lung disease, emphysema, osteoarthritis, heart disease, diabetes mellitus. In total, the list contained 31 medical conditions. For each of the illnesses, it was also asked whether the patient received medication or another form of regular medical attention. The self-reported illnesses were deemed to be measured with a greater reliability when the illnesses were said to be under medical attention.
Health-Related Quality of Life (HRQoL) valuations were obtained from the Medical Outcome Study Short Form 6 Dimensions (SF-6D) using Brazier’s algorithm [12]. The SF-6D is a much used and well-validated instrument derived from the Medical Outcomes Study Short Form [13], and the one well-validated algorithm that was applicable to our data. It is of note that the SF-6D can describe as many as 18,000 health states, all referring to descriptive health states [i.e. all the permutations of the items (1) physical functioning, (2) role limitations, (3) social functioning, (4) pain, (5) mental health, and (6) vitality, each of which has five or six possible answers]. To obtain HRQoL valuations of all 18,000 health states would be a daunting task. Therefore, Brazier and colleagues used a sub-sample of 249 health states to elicit valuations in a representative sample (N = 836) from the general public in the UK. During a personal interview each respondent was asked to value the selected health states, and valuation was carried out using the standard gamble method, which was originally developed by Von Neumann and Morgenstern in 1953 [14]. In standard gamble, individuals are asked to choose between the certainty of living in a health state versus a treatment, which entails a chance of getting well at probability P and dying at probability 1-P. The idea is that people are more willing to accept a risky treatment that involves a higher risk of dying when their health-related quality of life is poor. The trade-off between quality of life and survival can be converted into disability weights (DWs) for each of the health states on a 0–1 scale, where 0 is the best possible health state (no disability) and 1 is the worst possible health state, equal to death [15]. Finally, Brazier and colleagues used the health state valuations thus obtained in an econometric model to predict the values of all 18,000 health states that can be described by the SF-6D. The Brazier algorithm is based on this econometric model and can be obtained from John Brazier at the Sheffield University. We employed the algorithm developed for use in the SPSS statistical package.
Analysis
We linked the disability weights to each of the DSM-III-R axis-I disorders. Here, we took two approaches: one without, and another with adjustments for comorbid mental disorders and somatic illnesses. Unadjusted DWs for each of the disorders were computed as the average DW of all respondents meeting the diagnostic criteria for a particular disorder. While this approach may portray a realistic picture of the disease burden in groups that meet the diagnostic criteria for a disorder, it can be criticised for over-estimating the disease burden attributable to a specific disorder when there are comorbid conditions that lend extra weight to the disability.
There are various ways to adjust DWs for comorbidity [16]. One is to select ‘pure’ cases presenting with a single disorder and average their DWs, but it should be mentioned that this approach has been criticised for being unrealistic, because comorbidity is the rule rather than the exception, and DWs would then be based on atypical disease patterns. A second approach is to attribute the disease burden to the hierarchically more important ‘primary’ diagnosis in the presence of ‘secondary’ disorders. However, assessing which disorders rank first and second is a difficult task, involving arbitrary decisions, and we preferred to stay clear of such complexities. Therefore, we took a third approach, adjusting for comorbidity by regressing DWs simultaneously on all the mental disorders and somatic illnesses. The regression coefficients are then interpreted as the DW of one disorder adjusted for the other disorders and illnesses in the model, thus resulting in adjusted DW estimates. The intercept (constant) in the regression model is 0.14 DW (with a standard error of 0.0015). The intercept represents the average DW, conditional on DSM-III-R disorders and illnesses. The intercept can be interpreted as the HRQoL decrement, attributable to unobserved factors affecting HRQoL such as minor illnesses, accidents and conditions that were not measured such as personality disorders. It should be noted that when a person presents with depression, he has the adjusted DW corresponding to depression (0.11) plus the base-rate DW (0.14), thus, a total DW equal to 0.25. In this way, the adjusted DWs were computed for all disorders.
Finally, YLD were computed as the DWs attributable to a specific disorder multiplied by the number of people suffering from that disorder, while taking the duration of the disorder into account. This number of people starting to suffer from a disorder multiplied by the duration of the disorder is commonly referred to as person-years, which is approximated by the point-prevalence of a disorder. Finally, to facilitate extrapolation of our results to other countries, we calculated YLD per one million population: YLD/mln = DW × pyrs/mln. For data-analytical purposes, we used the 1-month prevalence rates as the best-available proxy for the point prevalence of the mental disorders.
To account for non-response, post-stratification weights were used in all analyses, see Ref. [8] for technical details. After weighting, the sample followed exactly the same multivariate distribution over age, gender, civil status and urbanisation as the population according to Statistics Netherlands (downloadable from www.cbs.nl). The Brazier algorithm for the SF-6D was executed in SPSS (version 15.0 for Windows), while all other analyses were conducted in Stata (version 8.2 for Windows). Since the data were weighted, we used robust statistical techniques (the Huber-White Sandwich Method) to obtain correct sample errors (SE) and P values under weighting [17].
Results
Characteristics of the studied population
The whole sample has, on average, a disability weight of 0.167 (SE = 0.001) on a scale of 0 (no disability; optimal health) to 1 (completely disabled; extremely poor health) indicating that people generally do not experience quality of life to its optimum, but 16.7 % below its optimum (Table 1). For each of the groups, the average unadjusted disability weight was calculated and t tests were conducted to see whether the DWs differed significantly across categories. Differences between SF-6D based DWs are said to be clinically important when exceeding 0.041 [18]. On average, women experience poorer quality of life than men. A greater amount of disability is experienced by people who had received less education, were not living with a partner, were jobless, and suffered from a mental disorder or a somatic illness. The mean age was 39.6 years (SE = 0.196; range 18–65 years) and age was significantly associated with disability: for every additional year of age, the DW showed a linear increase by a factor of 0.00049 (SE = 0.00014; t = 3.58; P < 0.001), indicating that the quality of life decreases somewhat with increasing age. We found no evidence for a non-linear (quadratic) relationship between DW and age.
Unadjusted disability weights
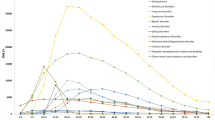
Table 2 presents the unadjusted disability weights, the number of person years spent in illness per million population (pyrs/mln), and the number of years lived with disability per one million (YLD/mln) for each of the 15 DSM-III-R axis-I disorders. It is of note that people who meet the diagnostic criteria for any mental disorder have a health-related quality of life that is 24 % lower than the theoretical maximum. Mood disorders, panic disorder, obsessive compulsive disorder, social phobia, eating disorders and schizophrenia emerged as the disorders with a relatively high disease burden at individual level: these disorders are associated with a relatively large DW.
Unadjusted years lived with disability
At population level, both the number of affected people and the actual disease duration become important drivers of disease burden. Both factors are captured in the number of person-years spent in illness. It appeared that the common mental disorders, such as anxiety and substance use disorders, emerged as prominent causes of disease burden. It is of note that simple phobia, a seemingly mild disorder, is not only associated with a relatively large number of person-years, but has in addition a markedly high average disability weight, making it the single leading cause of disability in the field of mental health. Here, we must emphasise that the YLD have not yet been adjusted for comorbidity.
Adjusted disability weights
Table 3 presents the results when statistical adjustments are made for all comorbidities including somatic illnesses, but not for demographics such as age and gender. It appears that the adjusted DWs are lower than the unadjusted ones by 28 % on average. A large reduction in the DWs was to be expected, because now we assess the unique contribution of each of the distinct disorders to disease burden. The DWs of eating disorders and simple phobias are particularly reduced after adjustment for comorbidity; somatic illnesses and drug dependence are least affected by adjustment.
Adjusted number of years lived with disability
At population level, the YLD are on average 28 % lower after adjustment, but the rank-order as causes of population ill-health remains unaffected; both the unadjusted and adjusted YLD show the same hierarchy: simple phobia emerges as the leading cause of non-fatal disability, followed by social phobia, depression, dysthymia and alcohol dependence and these are followed by eating disorders and schizophrenia (mainly due to the small number of affected people).
Discussion
Main findings
Mental disorders are a major cause of disease burden, but a distinction should be made between disease burden at individual level and at population level.
At individual level, depression, bipolar disorder, dysthymia, panic disorder, obsessive compulsive disorder and schizophrenia have a severe and adverse impact on health-related quality of life. In addition, people presenting with eating disorders and simple phobias tend to experience greatly reduced health-related quality of life, but this is largely attributable to comorbid conditions.
At population level, the number of people and the amount of time spent in an adverse health state become prominent drivers of population ill-health. Leading causes of years lived with disability are simple phobia, social phobia, depression, dysthymia and alcohol dependence—all of which are prevalent disorders or disorders that tend to persist over time. Our top-5 list remains unaltered after adjusting for comorbidity, indicating that each of these disorders significantly contribute to population ill-health in their own right, even when some of these conditions are often accompanied by concurrent disorders, as is the case for the simple phobias, social phobia and dysthymia. It may, therefore, be assumed that these disorders can be seen as priority targets for further scientific scrutiny and public health intervention.
Context and other studies
We need to place our findings in the wider context of the literature. The simple phobias are the most common mental disorders, and in our study, the phobias dominate other disorders in terms of their contribution to population ill-health. Previous Burden of Disease studies [1–4] did not specifically look into the disability caused by simple phobias.
A cost of illness study [19] shows that the simple phobias are associated with very modest health-care costs, indicating that people with simple phobia receive relatively little medical attention. Our data suggest that this might have important implications. First, many people suffer from these phobias and the phobias are often precursors of other mental disorders [20]. Treating the phobias may, thus, have preventive value. Second, the corresponding disability weight is relatively high: 0.30 (unadjusted) and 0.17 (adjusted). The fact that the adjusted disability weights are quite lower indicates that simple phobias are often comorbid with other conditions, but have, nevertheless, a fairly large disability weight in their own right. It is worth noting that our results are consistent with the literature. First, in one of our own studies [19], we demonstrated that the simple phobias are associated with remarkably high economic costs due to absenteeism from work, but not due to health-care uptake. This lends support to the impression that people with simple phobias are not often the recipients of professional care, and yet often stay away from their work, suggesting a certain amount of functional impairment stemming from this condition. The latter is also observed in the European-wide ESEMeD study: the simple phobias do not attract much medical attention, but are notoriously associated with work absenteeism [21]. A recent study on the effect of mental disorders on productivity shows that simple phobia is associated with additional days of absenteeism, although the effect is less pronounced [22].
Social phobia is a prevalent disorder with an onset typically in adolescence or early adulthood, and it is likely to run a chronic course when left untreated. These factors combine to make social phobia a disorder associated with a sizeable number of person-years spent in illness: 37,207 pyrs/mln in our study, ranking second after the simple phobias. In addition, social phobia is likely to have an adverse impact on academic achievement and professional performance, especially in the context of today’s communication and service-driven economy [23]. Its relatively large disability weight of 0.28 (unadjusted) and 0.18 (adjusted) has to be placed in this context. Social phobia featured prominently in the top-5 of leading causes of disability in the HRQoL study by Saarni et al. [23] and our evidence adds to theirs.
The presence of major depression on our top-5 list does not come as a surprise, because it has been consistently identified as a leading cause of disability [1, 4, 24–26]. Currently, depression is the single leading cause of non-fatal disease burden in high-income countries and it is projected to become the second leading cause of disability-adjusted life year (DALY) disease burden (which also accounts for mortality) by 2020, second only to ischemic heart disease [1]. More recent projections predict that depression might become the single leading cause of DALY disease burden in the high-income countries by the year 2030 [4].
Dysthymia has been under-studied as a contributor to population ill-health, possibly because its disability weight was often assumed to be equivalent to mild depression, and because major depression and dysthymia were sometimes combined into a single disease category [27]. However, more recently, Saarni et al. [24] identified dysthymia as the single leading cause of health-related quality of life decrement in Finland when basing the disability weight of dysthymia on valuations directly obtained from the target population. Saarni argued that the general population tends to weigh health states more heavily when these persist over time. Indeed, we obtained a DW for dysthymia of 0.36, adjusted to 0.22 when comorbidity was taken into account, which is still higher than the weight of 0.14 for mild depression [28] commonly used as a proxy for dysthymia in other studies. This would explain why dysthymia has not often been identified as a significant cause of disability in a population. Elsewhere, we showed that dysthymia is associated with the highest economic costs among the common mental disorders, thus, underscoring its relative importance as a disabling condition [19].
Alcohol dependence also ranks in the top-5 of our list of most disabling disorders at population level. There is no doubt about its importance as a risk factor for population ill-health and our study is more likely to under-estimate than to over-estimate its importance. After all, it is a condition associated with premature death [29], and we did not take mortality into account. Moreover, alcohol dependence is not only a clinical endpoint, but perhaps more importantly a risk factor for more than 60 medical conditions, ranging from cancer to liver sclerosis with all due consequences [30–33]. Alcohol dependence is, therefore, an important public health target and one may speculate that this is also true for the less severe but more common manifestations of alcohol misuse, such as hazardous and harmful use that are not part of the DSM classification.
Strengths and limitations
The strengths of this study include the population-based large-scale representative dataset on which the analyses were based and the use of formal DSM classifications of the mental disorders which were reliably assessed with the CIDI. The use of national, rather than regional or global, burden estimates makes our findings particularly useful to the Netherlands’ health service system.
Another strength is the disability weights being derived from the general population. This is important, because there are several ways of eliciting HRQoL valuations (e.g. from professionals in the medical field), but these are surrounded by controversy, and ultimately we need to understand how populations evaluate their own health-related quality of life [24].
A final strength is that we could compute both unadjusted and adjusted years lived with disability (YLD) either by accepting comorbidity with other mental disorders and somatic illnesses as a fact of life, or adjusting for comorbidity. Unadjusted YLD portray an accurate picture of the burden of disease in groups of people that are likely to have comorbid conditions—after all, in real life, we do not encounter people who have been adjusted for comorbidity. Therefore, unadjusted YLD may have value from a public health perspective. However, when the aim is to assess the YLD attributable to a specific disease, then adjusted estimates are preferred, because adjusted YLD give information about the amount of disability due to a specific disorder without confounding by co-occurring conditions. In our study, we explored both approaches and were, thus, able to shed light on both issues.
We acknowledge the following limitations of our study. First, people with severe conditions may have been unable to participate in this population-based survey because they were hospitalised, and this is likely to have resulted in an under-estimation of the disease burden. We expect the DW estimates of schizophrenia, bipolar disorder, severe depressions, and the more severe cases of anorexia nervosa, to be most affected by this.
Second, YLD captures only the non-fatal component of disease burden, as we did not include years of life lost (YLL) due to mortality, this results in an under-estimation of the overall disease burden, in particular, for conditions associated with excess mortality such as some of the somatic illnesses and the substance use disorders [1].
Third, we used the Brazier algorithm to calculate disability weights, but this algorithm was based on assessments in a sample of British people, while our sample was from the Netherlands. This may have distorted our outcomes somewhat, although it is unlikely to change the overall results in a substantial way, as differences in western Europe between national value sets, such as the set for the SF-6D, are small [34].
Fourth, available data made us use the 1-year prevalence rates of the somatic illnesses, while we relied on the 1-month prevalence rates of mental disorders. Thus, we could have over-estimated the YLD due to the somatic illnesses. However, the somatic illnesses were all chronic, making it unlikely that 1- and 12-month prevalence rates would differ drastically. We therefore expect that this did not substantially impact on our findings. An additional limitation is that data on somatic illnesses is based on self-report rather than diagnostic assessment, as well as the fact that not every somatic illness was adjusted for in the model. The fact that we did not adjust for every illness, but only for 31 illnesses, may have inflated DW estimates. In addition, since data on self-reported illnesses not under medical attention were excluded, further DW inflation might have occurred.
While we feel that the people should be the ultimate judges of their own health, a panel of lays may be associated with limitations that are worth noting, such as lesser consistency, and the possibility that (healthy) lays have difficulties passing judgments on the severe conditions. This may have caused some under-estimation of the disability weights associated with the more severe disorders. Indeed, regarding the severe conditions, Brazier et al. [12], pointed out that “inconsistent estimates and over prediction of the value of the poorest health states” might be seen as a limitation of their method.
A final limitation is that our data were based on DSM-III-R criteria, whereas one would prefer DSM-IV criteria or, in the future, DSM-5 criteria.
Implications
Our study showed that a clinical perspective on individual disease burden or a public health perspective on the disease burden at population level result in different health priorities. After all, the clinical approach brings individual suffering into focus, but at population level, the number of affected people and the duration of disorders become key drivers of population ill-health.
The fact that different perspectives lead to different conclusions about health priorities may not come as a complete surprise, but the difference can be quite striking. To illustrate, at individual level, one could have the impression that the simple phobia is not a priority for intervention, but the sheer number of years lived with disability due to simple phobia in the population does raise questions about the ways to alleviate its disease burden. Such paradoxes can be confusing. In debates about priorities in health care, it is important to understand how these paradoxes can arise—in particular when both clinicians and public health decision-makers are at the same table.
Our study suggests that the clinicians may need to reconsider the population-level impacts of disorders like simple phobia, social phobia and dysthymia in terms of HRQoL—especially in relatively disadvantaged groups such as women, jobless people and people with lower attained levels of education, those without a partner and those presenting with comorbid conditions—and perhaps identify phobias as targets of treatment more frequently. Conversely, decision-makers in the field of public health may have to be persuaded that for these disorders, clinical interventions may perhaps not be appropriate, but that attention should be directed to the question whether acceptable, effective and economically affordable (minimally supported) self-management interventions for these disorders can be developed (for example, as self-help interventions offered over the internet), evaluated and implemented on a scale proportional to their disease burden. Given the relatively low burden on individual level, in combination with the large burden on population-level, self-help interventions, when deemed appropriate, could play an important role in bridging the health gap for this population.
References
Murray CJL, Lopez AD (1996) The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. vol 1, Mass: Harvard School of Public Health, on behalf of the World Health Organization and the World Bank, Cambridge
Menken M, Munsat TL, Tolle JF (2000) The global burden of disease study: implications for neurology. Arch Neurol 57:418–420
Begg SJ, Vos T, Barker B, Stanley L, Lopez AD (2008) Burden of disease and injury in Australia in the new millennium: measuring health loss from diseases, injuries and risk factors. Med J Australia 188:36–40
Mathers CD, Loncar D (2006) Projections of global mortality and burden of disease from 2002 to 2030. PloS Med 3(11):e442. doi:10.1371/journal.pmed.0030442
World Health Organization (2006) Dollars, DALYs and Decisions. World Health Organization, Geneva
World Health Organization (2008) Mental Health Gap Action Programme: scaling up for mental, neurological and substance use disorders. World Health Organization, Geneva
Lancet Global Mental Health Group (2007) Scale up services for mental health: a call for action. Lancet 370:1241–1252
Bijl RV, Van Zessen G, Ravelli A (1998) The Netherlands Mental Health Survey and Incidence Study (NEMESIS): objectives and design. Soc Psychiatry Psychiatr Epidemiol 33:581–586
World Health Organization (1997) Composite International Diagnostic Interview (CIDI), version 2.1, 12-months. World Health Organization, Geneva
Ter Smitten MH, Smeets RMW, van den Brink W (1998) Composite International Diagnostic Interview (CIDI),Version 2.1, 12-months (in Dutch). World Health Organization, Amsterdam/Geneva
Wittchen HU (1994) Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res 28:57–84
Brazier J, Roberts J, Deverill M (2002) The estimation of a preference-based measure of health from the SF-36. J Health Econ 21:271–292
Ware JE, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36): i. Conceptual framework and item selection. Med Care 3:473–483
Von Neumann J, Morgenstern O (1953) Theory of games and economic behavior. Wiley, New York
Gafni A (1994) The standard gamble method: what is being measured and how it is interpreted. Health Serv Res 29:207–224
Andrews G, Sanderson K, Beard J (1998) Burden of disease: methods of calculating disability from mental disorder. Brit J Psychiatry 173:123–131
Hox JJ (2010) Multilevel Analysis: Techniques and Applications. Taylor and Francis Group, New York
Walters SJ, Brazier JE (2005) Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual Life Res 14:1523–1532
Smit F, Cuijpers P, Oostenbrink J, Batelaan N, De Graaf R, Beekman A (2006) Costs of nine common mental disorders: implications for curative and preventive psychiatry. J Ment Health Policy Econ 9:193–200
De Graaf R, Bijl RV, Spijker J, Beekman ATF, Vollebergh WAM (2003) Temporal sequencing of lifetime mood disorders in relation to comorbid anxiety and substance disorders. Soc Psychiatry Psychiatr Epidemiol 38:1–11
ESEMeD (2004) Disability and quality of life impact of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand 109(suppl):38–46
de Graaf R, Tuithof M, van Dorsselaer S, ten Have M (2012) Comparing the effects on work performance of mental and physical disorders. Soc Psychiatry Psychiatr Epidemiol: doi:10.1007/s00127-012-0496-7
Weehuizen R (2008) Mental capital: the economic significance of mental health. University of Maastricht, Dissertation
Saarni SI, Ari JS, Sintonen H, Pirkola S, Koskinen S, Aroma A, Lönnqvist J (2007) Impact of psychiatric disorders on health-related quality of life: general population survey. Brit J Psychiatry 190:326–332
Bowie C, Beck S, Bevan G, Raftery J, Silverton F, Stevens A (1997) Estimating the burden of disease in an English region. J Public Health Med 19:87–92
Mathers CD, Vos T, Stevenson E, Begg SJ (2001) The burden of disease and injury in Australia. Bull World Health Organ 79:1076–1084
Vos T, Mathers CD (2000) The burden of mental disorders: a comparison of methods between the Australian burden of disease studies and the Global Burden of Disease study. Bull World Health Organ 78:427–438
Stouthard M, Essink-Bot M-L, Bonsel G, Barendregt J, Kramers P, Van de Water H, Gunning-Schepers M-L, Van der Maas P (1997) Disability weights for diseases in the Netherlands. Department of Public Health, Erasmus University, Rotterdam
Gmel G, Gutjahr E, Rehm J (2003) How stable is the risk curve between alcohol and all-cause mortality and what factors influence the shape? A precision-weighted hierarchical meta-analysis. Eur J Epidemiol 8:613–642
Rehm J, Room R, Monteiro M, Gmel G, Graham K, Rehn N, Sempos CT, Jernigan D (2003) Alcohol as a risk factor for global burden of disease. Eur Addict Res 9:157–164
Chisholm D, Rehm J, Van Ommeren M, Monteiro M (2004) Reducing the global burden of hazardous alcohol use: comparative cost-effectiveness analysis. J Stud Alcohol 65:782–793
Konnopka A, König H–H (2009) The health and economic consequences of moderate alcohol consumption in Germany 2002. Value Health 2:253–261
Pillai A, Nayak MB, Greenfield TK, Bond JC, Nadkarni A, Patel V (2012) Patterns of alcohol use, their correlates, and impact in male drinkers: a population-based survey from Goa India. Soc Psychiatry Psychiatr Epidemiol 48(2):275–282
Craig BM, Busschbach JJ, Salomon JA (2009) Keep it simple: ranking health states yields values similar to cardinal measurement approaches. J Clin Epidemiol 62:296–305
Acknowledgments
The Nemesis study was financially supported by the Netherlands’ Ministry of Health (VWS).
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
Nemesis was conducted with the approval of the ethics committee of the Netherlands Institute of Mental Health and Addiction, Utrecht, the Netherlands. Respondents provided informed consent according to the prevailing Dutch law of 1996 after having been informed about the aims of the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lokkerbol, J., Adema, D., de Graaf, R. et al. Non-fatal burden of disease due to mental disorders in the Netherlands. Soc Psychiatry Psychiatr Epidemiol 48, 1591–1599 (2013). https://doi.org/10.1007/s00127-013-0660-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-013-0660-8