Abstract
Aim
To examine the association between mental disorders and work disability in the adult resident population in Singapore.
Method
Data are from the Singapore Mental Health Study, which was a household survey of a nationally representative sample. The main instrument used was the Composite International Diagnostic Interview (CIDI). Employment-related information was collected using the modified employment module of the CIDI.
Results
A total of 6,429 respondents were included in the analysis, 71 % (n = 4,594) were employed, 24.5 % (n = 1,522) were economically inactive and 4.5 % (n = 313) were unemployed. Among the employed, 2.3 % had a 12-month prevalence of at least one mental disorder, while 5.3 % of the unemployed had at least one mental disorder. The average number of work loss days (absenteeism) per capita among those with a mental disorder was 0.5 per month that is equivalent to an annualized national projection of approximately 0.3 million productivity days. The average work-cutback days (presenteeism) were 0.4 days among this group. Of the mentally ill in the workforce, a high proportion (86.5 %) did not ever seek help for problems related to mental health.
Conclusion
Our findings provide information on the significant consequences of mental disorders on the workforce in terms of lost work productivity, which could pave the way for a more rational allocation of scarce resources.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
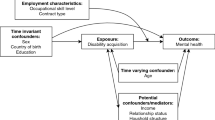
It is an almost universal finding that not only the employment rates among those with mental disorders is significantly lower, but also reduced work hours and lower earnings are common among the mentally ill [1–6]. The relationship between mental disorders and unemployment is complex and probably bidirectional. Unemployment can result from the functional impairment arising from mental disorders on one hand, and on the other, it has been implicated as an important contributor to poor mental health [7–11]. Regardless of the nature of the association, the magnitude of unemployment and work disability among people with mental disorders are especially important in that they represent costs to workers, employers, and to the whole economy. Depression, for example, has been estimated to cause the US economy billions of dollars each year [12–14]. The cost to the economy may also result from the need to give public income support to the unemployed, who in the USA constitute the largest group of recipients [1].
This strong association between unemployment and mental disorders might erroneously lead to the belief that the active labor force is healthy and productive [15]; however, studies have shown that a sizeable proportion of the labor force has mental disorders which in turn is associated with considerable absenteeism [13, 16–20]. A less obvious effect on productivity of the workforce is from work cutback or presenteeism which could also have a significant detrimental effect on work productivity [18, 19].
Mental disorders are often associated with chronic physical conditions [21, 22]. Chronic physical conditions by themselves have significant detrimental effects on functioning [23–25], but the comorbidity of mental and physical conditions is likely to be even more (additively or synergistically) disabling. This would lead to greater societal costs from increased work disability and increased use of health services—an issue that is relevant to policy makers [26].
Singapore’s per capita gross national product (GNP) is among the highest in the world—despite having no natural resources of its own. A cornerstone of its thriving and resilient economy is a well-educated, trained and disciplined workforce, which has been viewed as its most valuable resource; hence, a better understanding of the mental health status of this workforce is important for the country’s economy.
In December 2009, a national mental health survey was carried out among the resident population of Singapore to establish the prevalence rates of a number of selected mental disorders. Using the data from this survey, this paper aims to (1) examine the rate of unemployment among those with these mental disorders as compared to those without, and (2) to estimate the extent of work disability of these different mental disorders among the employed population.
Methods
The Singapore Mental Health Study (SMHS) was a cross-sectional epidemiological survey of a nationally representative population of the adult Singapore residents (citizens and permanent residents) aged 18 years and above. A disproportionate stratified sampling was used where the three main ethnic groups (Chinese, Malays, and Indians) were sampled in equivalent proportion of about 30 % each rather than in proportion to the ethnic distribution in the general population. Face-to-face interviews were conducted by professional survey interviewers. Those residents who were incapable of doing an interview due to severe physical or mental health conditions, language barriers, living outside the country, institutionalized or hospitalized at the time of the survey, and those who were not contactable due to incomplete or incorrect address were excluded from the survey. The study was approved by the relevant institutional ethics committee (National Healthcare Group, Domain Specific Review Board) and written informed consent was obtained from all participants and parent/guardian of participants who were between 18 and 21 years of age. In all, 6,616 respondents completed the survey from December 2009 to December 2010 giving a response rate of 75.9 %. A detailed description of the survey design is provided elsewhere [27].
Mental disorders were assessed by the Composite International Diagnostic Interview (CIDI) [28] which is designed to ascertain current and lifetime prevalence of mental disorders through the measurement of symptoms and their impact on day-to-day activities. This instrument enabled mental disorders to be defined in terms of the 10th Edition of the International Classification of Diseases (ICD-10) and the Diagnostic and Statistical Manual, Fourth Edition, of the American Psychiatric Association (1994) (DSM-IV) diagnoses. The mental disorders assessed in the SMHS were major depressive disorder (MDD), bipolar disorder, generalized anxiety disorder (GAD), obsessive compulsive disorder (OCD), alcohol abuse, and alcohol dependence. We also used a modified version of the CIDI checklist of chronic medical disorders wherein respondents were asked to indicate if they were ever diagnosed with any of 15 chronic conditions which are considered prevalent in Singapore’s population.
The CIDI included a series of questions reflective of work loss and work-cutback days. The first question asked respondents how many days out of the past 30 that they were totally unable to work or carry out their normal activities due to “your emotions, nerves, mental health, or your use of alcohol or drugs?” Another question asked about days out of the past 30 when respondents were able to work ‘but had to cut back on what they did or did not get as much done as usual’.
Employment status was classified as ‘employed’ (includes those working full and part time). One published description of a person who is “economically inactive” is a “person, at or above the minimum age for full time employment and below the state retirement age, is not employed or looking for work…those doing full time unpaid domestic work, early retirees, and a small group of persons of private means who do not want to work.” [29]. Building on this definition, we further divided this group into: ‘economically inactive’—comprising homemakers, students, and retirees; and ‘unemployed’ (includes those looking for work/unemployed, temporarily laid off, never worked, and disabled). These data were collected using a modified version of the employment module of the CIDI.
Statistical analysis
All estimates were weighted to adjust for oversampling and post-stratified for age and ethnicity distributions between the survey sample and the Singapore resident population in 2007. Mean and standard deviations were calculated for continuous variables, and frequencies and percentages for categorical variables. We used negative binomial (NB) regression to model the main effect of DSM-IV lifetime mental disorders, physical disorder, and comorbid mental–physical disorder on the rate of work-lost days (absenteeism) and work-cut days (presenteeism) with and without adjustment for age and gender, as there were evidence of over-dispersion of the data using Poisson regression. Standard error of estimates was generated using Taylor series linearization method to adjust for the weighting and stratification in the sample design. Statistical significance was evaluated at the <0.05 level using two-sided tests. All statistical analyses were carried out using the Statistical Analysis Software (SAS) System version 9.2 (Cary, NC, USA) and STATA (version 10.0).
Results
Out of the 6,616 respondents who completed the survey, 6,429 were included in this analysis, as they had provided full information on their employment and work status. Of these, 71 % (n = 4,594) were employed, 24.5 % (n = 1,522) were economically inactive, and 4.5 % (n = 313) were unemployed. Among those who were employed, 87.8 % were working full time and the remaining 12.2 % were working part time. Table 1 shows the distribution of socio-demographic and clinical characteristics of the sample by employment status. The 12-month prevalence of any mental disorders alone (excluding those with comorbid physical disorders) in those who were employed was 2.3 versus 5.3 % among the unemployed (χ 2 = 87.3, P < 0.001). Significantly higher rates of MDD, dysthymia, GAD, and OCD were found among the unemployed compared to the economically inactive and employed groups. MDD was the commonest mental illness across the three groups.
Table 2 shows the estimate of rate ratios (RR) of work-lost days (absenteeism) and work-cutback days (presenteeism) for those with and without mental disorders among employed respondents. The mean days of absenteeism among those without any mental and physical disorders was significantly lower compared to those with any physical disorder only and comorbid mental–physical disorders. Multivariate NB regression models adjusted for age and gender showed that those with any physical disorders only and comorbid mental–physical disorder have significantly higher RR of work-lost days as compared to those without any mental and physical disorders. The RR of absenteeism was lower among those with any mental disorder than those with physical disorder. However, the rates between the two groups were not significantly different.
The mean days of presenteeism among those without any mental and physical disorders were significantly lower as compared to those with any mental disorders only and comorbid mental–physical disorders. Multivariate NB regression models adjusted for age and gender showed that those with mental disorder only, any physical disorder only, and comorbid mental–physical disorder have significantly higher RR of presenteeism days as compared to those without any mental and physical disorders: respondents with comorbid mental–physical disorder have 3.5 times higher risk of presenteeism. The RR of presenteeism was higher among those with comorbid mental–physical disorders than those with physical disorder and mental disorder. However, the rates between the groups were not significantly different.
Of those in the active labor force with a history of 12-month mental disorder, 86.5 % had never sought treatment (Table 3).
Discussion
Our findings are consistent with those in the extant literature regarding the significantly higher rate of unemployment among the mentally ill, as well as the presence of considerable work disability (in terms of absenteeism and presenteeism) [15, 18]. The prevalence of mental illnesses in Singapore’s population is relatively lower as compared to that reported in the Western countries [30] which are reflected in the relatively low rates of mental illnesses among those employed. Similar to the recent report by de Graaf et al. [31], we found MDD to be the most prevalent disorder among the employed, although our rate of 2.2 % (12-month prevalence) was lower than their reported rate of 4.2 %. The average absenteeism from this group with mental disorders was 0.5 days of work loss per month per capita and is equivalent to an annualized national projection of approximately 0.3 million lost productivity days in the workforce of those aged 18 years and above.
The high rate of unemployment among those with mental illness is probably due to a number of reasons. It could be a consequence of the direct disabling effect of mental disorder on vocational functioning leading to loss of work, or a less direct effect through how mentally ill people perceive themselves and how they are perceived by co-workers and employers—the latter have often been shown to be reluctant to hire a person with a history of mental disorder [32, 33] Mentally ill people may be reluctant to seek employment for fear of having to disclose their illness; a Scottish survey found that 43 % of the respondents had not sought work because of such a fear [34]. In an US national survey of people with disabling mental disorders, 32 % reported that they were turned down for a job after disclosing their mental disorder [35], others were either dismissed, demoted, shunned, or harassed by co-workers [36].
The assessment of productivity should include both absenteeism—which is easier to measure and translate into economic loss, and presenteeism, which will provide a more realistic estimate of the magnitude of lost productivity. We found that physical and mental disorders are related to presenteeism and absenteeism, both independently and as comorbid disorders, with the greatest loss of absenteeism and presenteeism being among those with comorbid disorders. Kessler et al. [37] found that the mean impairment days among those patients with physical disorders were equivalent to those with mental disorders. In terms of presenteeism, the presence of comorbidities has the greatest effect, which might imply that the treatment of the physical disorder alone might not restore the individual to a full return to productivity.
Not only do mentally ill people continue to work despite having symptoms albeit cutting back on their work, the majority of them also do not seek help. This is especially of concern given the availability of effective treatments and the positive effect as shown by a study demonstrating that the improvement in productivity following treatment is more than enough to offset the costs of treatment [17].
There is a need for further research to understand why they do not seek help. Possible reasons include personal traits like stoicism, a work climate that discourages taking medical leave [38], lack of recognition or denial of a mental disorder, and/or fear of stigma and discrimination. The latter might be justified in that strong negative responses to people with mental disorder in their place of employment have been reported [32]. In a number of surveys, employers have expressed more negative attitudes about employing people with a history of mental disorders than about almost any other group [39–41].
Our findings ought to be interpreted in the context of the limitations of the study.
As with most studies of this nature, much of the information is dependent on the respondent’s recall, which other than being affected by memory, is subjected to other recall bias, and the possibility that some types of mental disorders lead to negative and distorted perceptions about personal self-worth [42], including biased reports about vocational functioning. We were also unable to differentiate if those working part time did so out of choice, as compared to those compelled to do so—this latter group would be classified as underemployment, which also includes those substantially overqualified for the work one does, and/or earning very low income [43, 44]. Lastly, presenteeism and absenteeism were measured by brief self-report questionnaires included in the 30-day functioning module of the CIDI. We were unable to corroborate the reported days of absenteeism with any administrative database or employment records, thus the data is subject to recall bias and under-reporting. The strength of this study was the use of an internationally recognized diagnostic tool (the CIDI) to identify cases according to standard classifications in a nationally representative sample, and although it is based on interviews with respondents, studies have shown that self-reported data from people with mental disorders are generally reliable [45].
The results reported here have important clinical, economic, and social implications. In the light of the high unemployment rate among the mentally ill, numerous studies have indicated that individuals with mental disorders do want to work or consider themselves able to work, and have also expressed the need for vocational rehabilitation [46–49]. Vocational rehabilitation and supported employment have established themselves as evidence-based practice and an important intervention in community psychiatry [50]. Currently in Singapore, a few Voluntary Welfare Organizations (VWOs) as well as the Institute of Mental Health, which is a tertiary care provider of mental health, offer both sheltered and supported employment. However, considerable work still needs to be done to reduce stigmatization and discrimination of those who are mentally ill in the workplace. Research of the employment needs of the mentally ill in Singapore needs to be done, as well as the cost-effectiveness of workplace interventions to screen and treat workers who are mentally unwell.
The high proportion of mentally unwell and untreated workers indicates the need for a raft of interventions: this would include mental health literacy programmes, implementing non-stigmatizing and non-discriminatory screening, and early detection mechanisms in the workplace, and making clinical care affordable and accessible. However, clinical treatment on its own might not be enough if the work environment is the cause or contributor to a person’s poor mental health [16, 51, 52]. Improving working environment requires action and commitment from employers who could be persuaded to act based on a business case of the net economic benefit of improved productivity [18, 53]. At a national level, these findings could contribute to policy formulation by providing information on the differential consequences of mental disorders on the workforce in terms of lost work productivity and paving the way for a more rational allocation of scarce resources.
References
Cook JA (2006) Employment barriers for persons with psychiatric disabilities: update of a report for the President’s Commission. Psychiatr Serv 57:1391–1405
Lahelma E (1992) Unemployment and mental well-being: elaboration of the relationship. Int J Health Serv 22:261–274
Scheid T (1993) An investigation of work and unemployment among psychiatric clients. Int J Health Serv 23:763–782
Claussen B, Bjorndal A, Hjort P (1993) Health and re-employment in a two year follow up of long term unemployed. J Epidemiol Community Health 47:14–18
Broadhead WE, Blazer DG, George LK, Kit Tse C (1990) Depression, disability days, and days lost from work in a prospective epidemiologic survey. JAMA 264:2524–2528
Stansfeld S, Feeney A, Head J, Canner R, North F, Marmot M (1995) Sickness absence for psychiatric illness: the Whitehall II Study. Soc Sci Med 40:189–197
Mathers CD, Schofield DJ (1998) The health consequences of unemployment: the evidence. Med J Aust 168:178–182
Morrell SL, Taylor RJ, Kerr CB (1998) Unemployment and young people’s health. Med J Aust 168:236–240
Jin RL, Shah CP, Svoboda TJ (1995) The impact of unemployment on health: a review of the evidence. CMAJ 153:525–540
Hammarstrom A, Janlert U (1997) Nervous and depressive symptoms in a longitudinal study of youth unemployment—selection or exposure? J Adolesc 20:293–305
Montgomery SM, Bartley MJ, Cook DG, Wadsworth MEJ (1996) Health and social precursors of unemployment in young men in Great Britain. J Epidemiol Community Health 50:415–422
Conti DJ, Burton WN (1994) The economic impact of depression in a workplace. J Occup Med 36:983–988
Kouzis AC, Eaton WW (1994) Emotional disability days: prevalence and predictors. Am J Public Health 84:1304–1307
Greenberg PE, Stiglin LE, Finkelstein SN, Berndt ER (1993) The economic burden of depression in 1990. J Clin Psychiatry 54:405–418
Lim D, Sanderson K, Andrews G (2000) Lost productivity among full-time workers with mental disorders. J Ment Health Policy Econ 3:139–146
Sanderson K, Andrews G (2006) Common mental disorders in the workforce: recent findings from descriptive and social epidemiology. Can J Psychiatry 51:63–75
Zhang M, Rost K, Fortney J, Smith R (1999) A community study of depression treatment and employment. Psychiatr Serv 50:1209–1213
Kessler R, Frank G (1997) The impact of psychiatric disorders on work loss days. Psychol Med 27:861–873
Dewa C, Lin E (2000) Chronic physical illness, psychiatric disorder and disability in the workplace. Soc Sci Med 51:41–50
Laitinen-Krispijn S, Bijl RV (2000) Mental disorders and employee sickness absence: the NEMESIS study. Soc Psychiatry Psychiatr Epidemiol 35:71–77
Alegria M, Jackson JS, Kessler RC, Takeuchi D (2003) National Comorbidity Survey Replication (NCS-R), 2001–2003. Inter-university Consortium for Political and Social Research, Ann Arbor
Kessler RC, Berglund P, Chiu WT, Demler O, Heeringa S, Hiripi E et al (2004) The US National Comorbidity Survey Replication (NCS-R): design and field procedures. Int J Methods Psychiatr Res 13:69–92
Sprangers MAG, de Regt EB, Andries F, van Agt HM, Bijl RV, de Boer JB et al (2000) Which chronic conditions are associated with better or poorer quality of life? J Clin Epidemiol 53:895–907
Stewart A, Greenfield S, Hays RD, Well SK, Roger WH, Berry SD et al (1989) Functional status and well-being of patients with chronic conditions: results from the medical outcomes study. JAMA 262:907–913
Hays RD, Wells KB, Sherbourne CD, Rogers W, Spritzer K (1995) Functioning and well-being outcomes of patients with depression compared with chronic general medical illnesses. Arch Gen Psychiatry 52:11–19
Wilson RW, Drury TF (1984) Interpreting trends in illness and disability: health statistics and health status. Annu Rev Public Health 15:83–106
Subramaniam M, Vaingankar J, Heng D, Kwok KW, Lim YW, Yap M, Chong SA (2012) The Singapore Mental Health Study: an overview of the methodology. Int J Methods Psychiatr Res. doi:10.1002/mpr.1351
Kessler RC, Ustun TB (2004) The World Mental Health (WMH) Survey Initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res 13:93–121
Bartley M, Ferrie J (2001) Glossary: unemployment, job insecurity, and health. J Epidemiol Community Health 55:776–781
Chong SA, Abdin E, Vaingankar JA, Heng D, Sherbourne C, Yap M, Lim YW, Wong HB, Ghosh-Dastidar B, Kwok KW, Subramaniam M (2012) A population-based survey of mental disorders in Singapore. Ann Acad Med Singap 41:49–66
de Graaf R, Tuithof M, van Dorsselaer S, Ten Have M (2012) Comparing the effects on work performance of mental and physical disorders. Soc Psychiatry Psychiatr Epidemiol [Epub ahead of print]
Schulze B, Angermeyer MC (2003) Subjective experiences of stigma. A focus group study of schizophrenic patients, their relatives and mental health professionals. Soc Sci Med 56:299–312
Stuart H (2006) Mental illness and employment discrimination. Curr Opin Psychiatry 19:522–526
See Me Scotland. See me so far: A Review of the First Four Years of the Scottish Anti-Stigma Campaign. Scottish Executive 2006. http://www.docs.csg.ed.ac.uk/EqualityDiversity/see_me_so_far.pdf. Accessed 25 May 2012
Wahl O (1999) Mental health consumers’ experience of stigma. Schizophr Bull 25:467–478
Wahl O (1999) Telling is risky business: mental health consumers confront stigma. Rutgers University Press, New Brunswick
Kessler RC, Greenberg P, Mickelson K, Meneades L, Wang P (2001) The effects of chronic medical conditions on work loss and work cutback. J Occup Environ Med 43:218–225
McKevitt C, Morgan M, Dundas R, Holland WW (1997) Sickness absence and ‘working through’ illness: a comparison of two professional groups. J Public Health Med 19:295–300
Cook JA, Razzano L, Straiton DM, Ross Y (1994) Cultivation and maintenance of relationships with employers of persons with severe mental illness. Psychosoc Rehabil J 17:103–116
Diksa E, Rogers ES (1996) Employer concerns about hiring persons with psychiatric disability: results of the Employer Attitude Questionnaire. Rehabil Couns Bull 40:31–44
Manning C, White PD (1995) Attitudes of employers to the mentally ill. Psychiatr Bull 19:541–543
Coyne JC, Gotlib IH (1983) The role of cognition in depression: a critical appraisal. Psychol Bull 94:472–505
Dooley D, Prause J, Ham-Rowbottom KA (2000) Underemployment and depression: longitudinal relationships. J Health Soc Behav 41:421–436
Friedland DS, Price RH (2003) Underemployment: consequences for the health and well-being of workers. Am J Community Psychol 32:33–45
Fresco DM, Coles ME, Heimberg RG, Liebowitz MR, Hami S, Stein MB et al (2000) The Liebowitz Social Anxiety Scale: a comparison of the psychometric properties of self-report and clinician-administered formats. Psychol Med 31:1025–1035
Campbell J, Schreiber R, Temkin T (1989) The well-being project: mental health clients speak for themselves. California Department of Mental Health, Office of Prevention, Sacramento
Rogers ES, Walsh D, Masotta L, Danley K, Smith K (1991) Massachusetts survey of client preferences for community support services. Final Report, Center for Psychiatric Rehabilitation, Boston University, Boston
Uttaro T, Mechanic D (1994) The NAMI consumer survey analysis of unmet needs. Hosp Community Psychiatry 45:372–374
Van Dongen CJ (1996) Quality of life and self-esteem in working and nonworking persons with mental illness. Community Ment Health J 32:535–548
Drake RE, Becker DR, Bond GR (2003) Recent research on vocational rehabilitation for persons with severe mental illness. Curr Opin Psychiatry 16:451–455
Van Der Doef M, Maes S (1999) The job demand–control (support) model and psychological well-being: a review of 20 years of empirical research. Work Stress 13:87–114
North FM, Syme SL, Feeney A, Shipley M, Marmot M (1996) Psychosocial work environment and sickness absence among British civil servants: the Whitehall II study. Am J Public Health 86:332–340
Jenkins R (1994) Mental illness and work. In: Floyd M, Povall M, Watson G (eds) Mental health at work. Jessica Kingsley, London, pp 77–79
Acknowledgment
This research was supported by funding from the Singapore Millennium Foundation and the Ministry of Health, Singapore.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chong, S.A., Vaingankar, J.A., Abdin, E. et al. Mental disorders: employment and work productivity in Singapore. Soc Psychiatry Psychiatr Epidemiol 48, 117–123 (2013). https://doi.org/10.1007/s00127-012-0526-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-012-0526-5