Abstract
Purpose
We conducted a national epidemiological study to determine how mental illness and criminal offending combine to influence suicide risk in younger adults.
Methods
Using completely interlinked registers, we generated a nested case–control study from the cohort of all Danish people born 1965 and onwards. We identified 2,384 suicides aged 15–41 years during 1981–2006, and 56,016 age and sex-matched living controls. We examined all criminal charges from 1980, and all psychiatric admissions from 1969 and outpatient episodes from 1995. Exposure odds ratios were estimated using conditional logistic regression models.
Results
A quarter of male and 17 % of female suicides had histories of both criminal justice system contact and secondary care psychiatric treatment, with a marked elevation in risk seen compared with having neither risk factor: male odds ratio (OR) 34.0, 95 % confidence interval (CI) 29.1–39.6; female OR 72.7, CI 49.4–107.1. Among those treated for psychiatric illness, contact with the criminal justice system predicted higher risk: male OR 1.4, CI 1.1–1.7; female OR 1.7, CI 1.1–2.4, although these effects were attenuated and became non-significant with adjustment for socio-demographic risk factors. In men, risk was especially high if first criminal justice system contact occurred before first psychiatric treatment episode, and if these two challenging life events coalesced within a year of each other.
Conclusion
These younger age adults should be monitored carefully for signs of suicidal behaviour. The need for well coordinated multiagency care is indicated, and a broad range of psychiatric illnesses should be considered carefully when assessing their suicide risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Suicide is a major public health problem worldwide and many countries have national prevention strategies [1, 2]. The World Health Organization (WHO) has estimated the global burden as a million deaths per year [3, 4], although the annual death toll could be considerably greater than this due to incomplete case ascertainment in many countries [5]. It is an especially important cause of early premature mortality, with a substantial proportion of all suicides occurring many years prior to average life expectancy [6]. The key risk factor for suicide is mental illness, and this association has been widely reported [7–9]. Depression is most commonly linked with suicide risk, but meta-analysis has shown that almost all mental disorders, including those associated with substance misuse, confer higher risk [10]. More research is needed to increase our understanding of how co-occurring risk factors act in combination to influence suicide risk [11].
The relationship between mental illness and criminal offending is complex and controversial [12, 13], but whichever the direction of association [14], and whatever the precise causal mechanisms involved, the prevalence of mental illness is elevated in the offender population [15, 16]. Research on suicide risk among offenders has been rather limited in its scope, being focused largely on incarcerated males [17] and, more recently, in people released from prison [18–20]. There have been fewer investigations of those who have never been imprisoned, the great majority of all offenders, although a raised risk of suicide has also been shown in this group [21–23]. Evidence for suicide risk among forensic psychiatric populations is lacking [24].
In our previous analysis of this large nested case–control study, in comparison with the general population we reported elevated suicide risk in people with any criminal justice system contact, and also by specific type of judicial verdict, by type of offence, and by recency and frequency of contact [23]. In the current paper, we now address the following new research questions:
-
1.
Compared to their peers with neither risk factor, what is the relative risk of suicide in younger adults who have experienced criminal justice system contact and also have a history of secondary care-treated psychiatric illness?
-
2.
To what degree is contact with the criminal justice system a risk factor among younger adults who have also received psychiatric treatment?
-
3.
How does timing of first criminal justice system contact, in relation to first secondary care psychiatric treatment episode, influence risk?
Method
Registry data sources and variables
The Danish Data Protection Agency granted their prior approval for us to conduct the study. A number of longitudinal registers were interlinked completely using unique civil registration numbers [25]. The National Causes of Death Register was used to identify all suicides aged 15 years and over between 1st January 1981 and 13th December 2006 [26], according to the eighth revision of the International Classification of Disease, ICD-8 codes E950-959 [27], for 1981−1993, and the tenth revision, ICD-10 codes X60-X84 [28], for 1994−2006. The ninth revision was never implemented in Denmark. Unlike in other countries, such as the United Kingdom [29], Danish epidemiological studies of suicide do not combine suicide and open verdicts in their case definition, due to a perception that ascertainment levels are more accurate [30, 31].
We identified every adult charged with committing a criminal offence from 1st January 1980 onwards according to the National Criminal Register [32]. This registers all such persons after their 15th birthday, which was the age of criminal responsibility in Denmark during the study period. It covers all criminal charges and judicial outcomes, apart from small fines given out of court for unregistered minor traffic violations. The Psychiatric Central Register was used to identify all admissions since 1969 and all outpatient treatment from 1995 [33]. This constitutes a complete national secondary care record, as there are no private psychiatric hospitals in Denmark and all treatment is provided free of charge. Within the broad range of ICD codes used to identify mental illnesses (ICD-8: 290-315; ICD-10: F00-F99), we delineated the following diagnostic categories:
-
Schizophrenia and related disorders (i.e. schizophrenia, schizophrenia-like, or schizoaffective disorder): ICD-8: 295, 297, 298.2, 298.3, 298.4, 298.5, 298.6, 298.7, 298.8, 298.9, 299, 301.0, 301.2; ICD-10: F20-F29, F60.0, F60.1.
-
Affective disorders: ICD-8: 296, 298.0, 298.1, 300.4, 301.11; ICD-10: F30-F34, F38, F39.
-
Personality disorders: ICD-8: 301.3, 301.4, 301.5, 301.6, 301.7, 301.8, 301.9;
-
ICD-10: F60.2, F60.3, F60.4, F60.5, F60.6, F60.7, F60.8, F60.9
-
Alcohol or drug disorders: ICD-8: 291, 294, 303, 304; ICD-10: F10-F19.
We also assessed potential for confounding by multiple socio-demographic and socioeconomic risk factors, as observed previously in the general population [34]. These variables were civil status (married, cohabiting, single, living with family); being a parent; area of residence (central and suburban Copenhagen, other large cities, resident elsewhere); income level (in quartiles); and educational attainment level (primary school, secondary school, vocational training, degree/higher degree); and birthplace outside Denmark/non-Danish citizenship. Civil status, income quartile and educational attainment level were derived from the Integrated Database for Labour Market Research (IDA) [35] database according to the most recent annual record prior to suicide, while place of residence and being a parent were taken from the Central Population Register on the date of suicide. The covariates were 100 % complete except for educational level (cases: 78.2 %, controls: 87.0 %).
Study design and statistical analyses
All analyses were performed using Stata software version 10 (College Station, TX: StataCorp, 2008). From the national registry data, we initially identified all adult suicides during calendar years 1981–2006. As is reported in our earlier paper from this cohort [23], the total initial sample size for our case–control study was 27,219 cases and 524,899 matched controls. However, because the National Criminal Register only commenced systematic computerised registration of all charges and judicial outcomes in 1980, only those people born on January 1st 1965 and later have complete records in this register. To achieve the most accurate assessment of the combined impact of alleged or proven criminal offending and serious mental illness as risk factors for suicide in younger adults, we restricted the study dataset to the 2,384 suicide cases born after 1964, and their 56,106 matched controls.
The cases in our nested case–control study [36] were matched on date of birth and gender, with up to 25 living controls selected from a 25 % random sample of the national cohort at risk during 1981–2006. Matching on date of birth accounted for age and cohort effects by design, whilst matching on date of death (i.e. control alive when its case died) enabled us to implement incidence density sampling procedures in generating the nested case–control design. This approach ensured that the exposure odds ratios were interpretable as relative risks as would be derived from survival analysis of the whole cohort [36]. To avoid unnecessarily introducing selection bias or reducing statistical efficiency [37], and also so that we could explicitly assess confounding by psychiatric and social factors, we did not match controls to cases on any other criteria. A large number of controls per case were sampled to maximise the precision of our effect estimates [38]. We calculated exposure prevalence among cases and controls separately, and estimated relative risks as exposure odds ratios using conditional logistic regression models. In our multivariate models, we adjusted for all six of the social risk factors listed in the previous section, because we were interested in assessing their combined confounding effect, irrespective of the observed level of statistical significance of each individual variable in the model [39].
We initially estimated odds ratios in relation to criminal justice system contact and to hospital treated mental illness as separate risk factors, with the reference groups being no criminal justice system history and no psychiatric treatment, respectively. We then generated two further sets of odds ratios, with the two risk factors stratified against one another. For the first set, we estimated effects in the following exposure subgroups: criminal justice system contact only; secondary care psychiatric treatment only; criminal justice system contact and psychiatric treatment, using a common reference group of no criminal justice system contact or psychiatric treatment. For the second set, we calculated the ratio of the effect size for criminal justice system contact and psychiatric treatment against that for psychiatric treatment only. This enabled us to assess the additional effect of criminal offending on suicide risk among people with history of serious mental illness.
To address our third research question, we further stratified the data to compare relative risk according to whether first criminal justice system contact occurred before or after first secondary care psychiatric treatment episode, and whether or not these two events occurred close together in time (i.e. within a year of each other).
Results
Descriptive analyses
We examined 1,914 male suicide cases (45,169 matched controls) and 470 female cases (10,847 matched controls) born 1st January 1965 and onwards. For both genders the age range of the cases on their date of death was 15–41 years. Their median age was 25 years (interquartile range 21–30 years), with most of them (1,944, 81.5 %) dying in their 20s or 30s. In Table 1, we show the prevalence of psychiatric illness treated in secondary care settings; i.e. inpatient care since 1969 and outpatient treatment from 1995. These estimates are reported by diagnostic group and by gender and for cases and controls separately. The prevalence of having any secondary care-treated psychiatric illness was much higher in female than in male cases. Among male cases, the most common diagnostic categories were schizophrenia and related disorders followed by alcohol/drug disorders, whereas in female cases the most common groups were personality disorders then schizophrenia and related disorders and affective disorders.
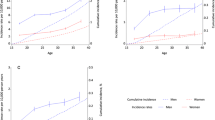
We also conducted further stratified analyses of prevalence of secondary care treated psychiatric illness among suicide cases, according to whether or not they had history of criminal justice system contact. The results are presented in Figs. 1 and 2. In both genders, the overall prevalence of treated psychiatric illness was higher in cases with criminal justice contact. Marked differences in prevalence of personality disorder and alcohol/drug disorders, between those with and without criminal justice system contact, were seen in male cases; in female cases, an especially marked difference in prevalence was observed for alcohol/drug disorders.
Separate effects of the two risk factors
Before assessing the combined effect of criminal justice system contact and serious mental illness on suicide risk, we considered the separate effects of the two risk factors. These results, stratified by gender, are shown in Table 2. In male suicide cases and living controls, contact with the criminal justice system was much more frequent than hospital psychiatric treatment. It was also the more common of the two risk factors among female controls, although the difference in prevalence between them was much smaller than was seen among male controls. Among female suicides, psychiatric treatment was the more common of the two risk factors—the opposite of what was seen in the male cases. Criminal justice system contact was linked with a higher risk of suicide in younger men, and the relative risk was even greater in younger women. Elevated risk persisted in both genders following multivariate adjustment. As expected, the effect sizes were much greater in relation to hospital treated psychiatric illness, and especially so for women.
Combined effects of both risk factors
Next we conducted a stratified analysis to compare the effects of having only one versus both of the risk factors. We calculated relative risk for having criminal justice system contact only or secondary care-treated psychiatric illness only, compared with having neither of these risk factors recorded. For these results, which are presented in Table 3, we used the common reference category ‘neither risk factor recorded’. The effect sizes were again considerably stronger in women than in men. Younger men with history of criminal justice system contact as well as psychiatric treatment had a suicide risk that was approximately 34 times greater than those with neither risk factor, with the equivalent relative risk in younger women being around 73. The statistical interaction terms fitted between the binary exposure variables for criminal justice system contact and psychiatric treatment were highly significant in both genders, with and without multivariate adjustment (p < 0.001).
We estimated relative risk linked with criminal justice system contact among people who had also received secondary care psychiatric treatment. These results, which pertain to all psychiatric diagnoses combined, are also presented in Table 3. They show a raised risk in men and women with any previous secondary care psychiatric treatment if they also had history of criminal justice system contact. With adjustment for all of the social risk factors described in the "Methods", these effects were attenuated and became non-significant (men: adjusted odds ratio 1.2, 95 % confidence interval 0.9–1.4, p = 0.17; women: adjusted odds ratio 1.3, 95 % confidence interval 0.9–2.0, p = 0.14). In the male model, birthplace outside Denmark/non-Danish citizen and being a parent and were non-significant; in the female model, area of residence/urbanicity and educational attainment level were non-significant. However, all six social risk factors were retained as covariates. In both male and female models, the strongest confounder was income level.
We also conducted the same analyses for specific diagnostic groups. Criminal justice system contact was a highly significant risk factor for suicide in men with hospital treatment for personality disorders (odds ratio 1.9, 95 % confidence interval 1.2–2.9; p = 0.006), and in women treated for affective disorders (odds ratio 4.2, 1.4–13.3; p = 0.01), with the reference group for these effects being men/women in these diagnostic subgroups with no history of criminal justice system contact. For all other specific psychiatric categories in both genders, no significant effect of criminal justice system contact was found, although there was a suggestion of an in men diagnosed with schizophrenia and related disorders (odds ratio 1.4, 1.0–1.9; p = 0.07).
Effects by timing of first criminal justice system contact versus first secondary care psychiatric treatment
Finally, in Table 4 we present relative risk estimates further stratified according to relative timing of onset for the two risk factors, and whether or not these major life events occurred within a year of each other or further apart in time. Again we applied the generic reference category’neither risk factor recorded’. Due to sparse data this fine level of stratification was not viable for women, and so in the table we show these results for men only. Elevation in risk in males was particularly large if first criminal justice system contact occurred before first psychiatric treatment, with a 40-fold increase against the reference category indicated. In this group, risk was approximately doubled compared to men whose first criminal justice system contact occurred after their first psychiatric treatment episode, and this difference in effect was highly significant (z = 5.0, p < 0.001). A previous national Danish study reported suicide risk to be especially high soon after discharge from a psychiatric unit [40]. We therefore calculated the median number of days since last inpatient or outpatient psychiatric treatment episode ended in these two groups of suicides. The average number of days was significantly lower among cases whose first criminal justice system contact preceded first psychiatric treatment, compared to those who experienced psychiatric treatment before criminal justice system contact (median 133 vs. 255 days; Wilcoxon rank-sum test: p = 0.01). We also had sufficient male cases to assess how risk was affected by the temporal closeness of these two major life events, and these results are also presented in Table 4. Risk was greatest of all if first criminal justice system contact occurred within a year before or after first psychiatric treatment episode, and this effect was significantly greater than if the time difference between the two events was greater than a year (z = 2.4, p = 0.02).
Discussion
Summary of findings
Among the younger adult Danish population as a whole, being charged with an offence and passing through the criminal justice system was a far more common experience than psychiatric treatment in a hospital setting, although the latter risk factor was more prevalent among female suicide cases. However, serious psychiatric illness was a much a stronger risk factor for suicide than criminal justice system contact. Stratified analysis of the two risk factors showed that younger men with both risk factors were around 34 times more likely to die by suicide than their peers without either risk factor, and the equivalent relative risk in younger women was approximately 73. Among those who had received secondary care psychiatric treatment, there was a significant increase in suicide risk if they had also been in contact with the criminal justice system, with increases in risk by 39 and 67 % seen in these men and women, respectively. These particular effects were attenuated, and became non-significant, following adjustment for social risk factors. Socioeconomic status, as measured using income level, had the strongest confounding effect among the six social risk factors we assessed. Serious psychiatric illness was such a strong risk factor on its own that the additional risk associated with criminal contact was relatively modest, though still statistically significant and important in terms of public health impact. Among men, suicide risk was greater if first criminal justice system contact occurred some time before first secondary care psychiatric treatment episode, and risk was especially high if the time interval between these two major adverse life events was short.
Comparison with existing evidence
A previous register-based study examined predictors of suicide among Norwegians born between 1967 and 1976 and aged 18–37 at follow-up [41]. However, criminal justice system contact was not included among the broad range of risk factors examined. Indeed very few studies have been conducted to investigate suicide risk in people with histories of both criminal offending and serious mental illness. On the basis of data collected over several decades at the Bridgewater State Hospital, in south eastern Massachusetts, a US study reported that forensic hospital populations have suicide rates that are comparable to those seen in other psychiatric populations [42]. However, these findings may not be generalisable, being from just one institution. This hospital was set up to care for the ‘criminally insane’, including sex offenders, and the study sample may not be internationally comparable. We examined the offender population in the broadest sense, with the majority of people in our study being charged with less serious forms of property and traffic offences and receiving only fines. It is also unlikely that suicide risk within an institution can be generalised to the wider group of offenders living in the community, with fewer constraints and more opportunities for taking their own lives.
We also identified two previous studies reporting elevated suicide risk in people following discharge from forensic psychiatric care. A relative risk of 4.7 post-discharge was reported from a single forensic psychiatric unit in Sweden [43]. In England, a high relative risk of 32 against the general population has recently been reported among patients discharged from a medium-secure unit during 1983–2003, with a much stronger effect size seen among women (76-fold higher risk) compared to men (22-fold increase) [24]. Although the composition of that study population was different to the one we studied, the relative risks reported are of a similar magnitude to the ones that we estimated.
We searched the literature on recent adverse life events and risk of completed and attempted suicide. Two previous published reviews of this topic did not list criminal offending or justice system contact among the risk factors examined by the empirical studies they reviewed [44, 45]. We could find only one study examining a broad list of life events that considered forensic issues [46], which were indicated as being an important proximal precipitant among young people. Future psychological autopsy studies should examine this exposure in detail, including how it acts in combination with mental illness to heighten suicide risk at younger age.
Strengths and limitations
We conducted a large epidemiological study using the robust and statistically efficient nested case–control design. Using these population-based registry sources, we precluded the two major flaws that are common in case–control studies: information bias between cases and controls in deriving explanatory variables, and biased selection of controls [47].We had complete records of criminal charges, inpatient psychiatric treatment and cause-specific mortality. Exposure data were collected prospectively, with attrition in the cohort at risk due to emigration and death from other causes identified and fully accounted for, and with complete linkage between registers due to the existence of a single unique national identifier that is mandatory for all Danish citizens and residents [25]. There are very few countries worldwide where such a study could be conducted in this way.
Although there are clear benefits in conducting epidemiological studies using national registers, including large sample sizes for examining rare exposures and outcomes, representativeness and absence of recall bias [48], they are challenging nonetheless because they do not exist primarily for academic purposes. The administrative information collected therefore has to be recoded carefully by researchers to create meaningful explanatory variables. This particular study also had some important specific limitations. Firstly, as with any registry study, there was some degree of misclassification. We restricted the study dataset to individuals born 1965 and later so that all subjects had complete criminal justice records. We also had thorough information on all subjects’ psychiatric admission histories, as comprehensive registration of these began as far back as 1969. However, computerised registration of outpatient care began only in 1995, so before that time some people will have been misclassified for that reason. Also, our datasets could not capture mental illness episodes treated purely in primary care, or disorder that is not detected or treated at all by healthcare services. Secondly, although we found a huge increase in risk among people with histories of both criminal offending and serious mental illness, compared to those with neither risk factor, this group was uncommon in the general population (using control subjects as a proxy). Furthermore, although risk was many times greater in these people, their absolute risk of suicide was nonetheless very low. This is an often acknowledged problem in suicide research, which limits the usefulness of establishing and applying suicide risk factor profiles to routine clinical practice [49, 50].
Conclusion
Our findings highlight the vulnerability of younger people who have been treated for serious mental illness and have also passed through the criminal justice system. This group has an excess suicide risk over and above that seen in people treated for mental illness but with no offending history. This excess is, however, partly explained by social risk factors, primarily socioeconomic status. Newly developed national population-based strategies should acknowledge and address the greatly elevated suicide risk in this population. For example, the forthcoming suicide prevention strategy for England recognises that all people who pass through the criminal justice system, not just current and released prisoners, are at elevated risk. It also notes that many of them are vulnerable due to mental disorder and substance misuse [51]. Public health and offender health issues are closely intertwined, because many health inequalities and social determinants of ill health are common among offenders. Our findings show that they should be monitored especially carefully for signs of depressed mood and suicidal ideation or attempts, and they should receive high quality coordinated care across multiple health and social service agencies. The impact of psychiatric illnesses other than mood disorders (including psychoses, personality disorders and alcohol/drug disorders) also requires careful consideration when assessing suicide risk in offenders. More generally, we have also shown that suicide risk is heightened markedly when multiple adverse life events coalesce in a short space of time.
References
Hawton K, van Heeringen K (2009) Suicide. Lancet 373:1372–1381
Hoven CW, Mandell DJ, Bertolote JM (2010) Prevention of mental ill-health and suicide: public health perspectives. Eur Psychiatr 25:252–256
WHO (2002) World report on violence and health. World Health Organization, Geneva
WHO. Suicide Prevention (SUPRE). http://www.who.int/mental_health/prevention/suicide/suicideprevent/en/
Rockett IRH (2010) Counting suicides and making suicide count as a public health problem. Crisis 31:227–230
Gunnell D, Middleton N (2003) National suicide rates as an indicator of the effect of suicide on premature mortality. Lancet 362:961–962
Mortensen PB, Agerbo E, Erikson T, Qin P, Westergaard-Nielsen N (2000) Psychiatric illness and risk factors for suicide in Denmark. Lancet 355:9–12
Evans J, Middleton N, Gunnell D (2004) Social fragmentation, severe mental illness and suicide. Soc Psychiatry Psychiatr Epidemiol 39:165–170
Phillips MR (2010) Rethinking the role of mental illness in suicide. Am J Psychiatry 167:731–733
Harris EC, Barraclough B (1997) Suicide as an outcome for mental disorders: a meta-analysis. Br J Psychiatry 170:205–228
Logan J, Hall J, Karch D (2011) Suicide categories by patterns of known risk factors: a latent class analysis. Arch Gen Psychiatry 68:935–941
Anckarsäter H, Radovic S, Svennerlind C, Höglund P, Radovic F (2009) Mental disorder is a cause of crime: the cornerstone of forensic psychiatry. Int J Law Psychiatry 32:342–347
Peterson J, Skeem JL, Hart E, Vidal S, Keith F (2010) Analyzing offense patterns as a function of mental illness to test the criminalization hypothesis. Psychiatr Serv 61:1217–1222
Munkner R, Haastrup S, Joergensen T, Kramp P (2003) The temporal relationship between schizophrenia and crime. Soc Psychiatry Psychiatr Epidemiol 38:347–353
Hodgins S, Mednick SA, Brennan PA, Schulsinger F, Engberg M (1996) Mental disorder and crime: evidence from a Danish birth cohort. Arch Gen Psychiatry 53:489–496
Pandiani JA, Banks SM, Carroll BB, Schuleter MR (2007) Crime victims and criminal offenders among adults with serious mental illness. Psychiatr Serv 58:1483–1485
Fazel S, Cartwright J, Norman-Nott A, Hawton K (2008) Suicide in prisoners: a systematic review of risk factors. J Clin Psychiatry 69:1721–1731
Pratt D, Piper M, Appleby L, Webb R, Shaw J (2006) Suicide in recently prisoners: a population-based cohort study. Lancet 368:119–123
Binswanger IA, Stern MF, Deyo RA, Heagerty PJ, Cheadle A, Elmore JG, Koepsell TD (2007) Release from prison: a high risk of death for former inmates. N Engl J Med 356:157–165
Spaulding AC, Seals RM, MacCallum VA, Perez SD, Brzozowski AK, Steenland NK (2011) Prisoner survival inside and outside of the institution: implications for health-care planning. Am J Epidemiol 173:479–487
Pritchard C, Cox M, Dawson A (1997) Suicide and ‘violent’ death in a six-year cohort of male probationers compared with the pattern of mortality in the general population: evidence of accumulative socio-psychiatric vulnerability. J R Soc Health 117:180–185
Sattar G (2003) The death of offenders in England and Wales. Crisis 24:17–23
Webb RT, Qin P, Stevens H, Mortensen PB, Appleby L, Shaw J (2011) National study of suicide in all people with a criminal justice history. Arch Gen Psychiatry 68:591–599
Clarke M, Davies S, Hollin C, Duggan C (2011) Long-term suicide risk in forensic psychiatric patients. Arch Suicide Res 15:16–28
Pedersen CB, Gøtzshe H, Møller JO, Mortensen PB (2006) The Danish Civil Registration System. A cohort of eight million persons. Dan Med Bull 53:441–449
Juel K, Helweg-Larsen K (1999) The Danish registers of causes of death. Dan Med Bull 46:354–357
WHO (1967) Manual of the International Classification of Diseases (ICD-8). World Health Organization, Geneva
WHO (1992) The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. World Health Organization, Geneva
Linsley KR, Schapira K, Kelly TP (2001) Open verdict vs. suicide—importance to research. Br J Psychiatry 178:465–468
Atkinson MW, Kessel N, Dalgaard JB (1975) The comparability of suicide rates. Br J Psychiatry 127:247–256
Walsh D, Mosbech J, Adelstein A, Spooner J, Dean G (1984) Suicide and self-poisoning in three countries—a study from Ireland, England and Wales, and Denmark. Int J Epidemiol 13:472–474
Kyvsgaard B (2003) The Criminal Career: the Danish Longitudinal Study. Cambridge University Press, Cambridge
Munk-Jørgensen P, Mortensen PB (1997) The Danish psychiatric central register. Dan Med Bull 44:82–84
Qin P, Agerbo E, Mortensen PB (2003) Suicide risk in relation to socioeconomic, demographic, psychiatric, and familial factors: a national register-based study of all suicides in Denmark, 1981–1997. Am J Psychiatry 160:765–772
Danmarks Statistik (Statistics Denmark) (1991) IDA—en integret database for arbejdsmarkedsforskning. [IDA—an integrated database for labor market research]. Danmarks Statistiks trykkeri, Copenhagen
Clayton D, Hills M (1993) Statistical models in epidemiology. Oxford University Press, Oxford
Rothman KJ, Greenland S (eds) (1998) Modern epidemiology, 2nd edn. Lippincott-Raven, Philadelphia
Hennessy S, Bilker WB, Berlin JA, Strom BL (1999) Factors influencing the optimal control-to-case ratio in matched case-control studies. Am J Epidemiol 149:195–197
McNamee R (2005) Regression modelling and other methods to control confounding. Occup Environ Med 62:500–506
Qin P, Nordentoft M (2005) Suicide risk in relation to psychiatric hospitalization: evidence based on longitudinal registers. Arch Gen Psychiatry 62:427–432
Gravseth HM, Mehlum L, Bjerkedal T, Kristensen P (2010) Suicide in young Norwegians in a life course perspective: population-based cohort study. J Epidemiol Community Health 64:407–412
Haycock J (1993) Double jeopardy: suicide rates in forensic hospitals. Suicide Life Threat Behav 23:130–138
Reiter K (1974) Mortality and cause of death in men found to be mentally abnormal by forensic psychiatrists. Scand J Soc Med 2:1–3
Heikkinen M, Aro H, Lonnqvist J (1994) Recent life events, social support and suicide. Acta Psychiatr Scand Suppl 377:65–72
Foster T (2011) Adverse life events proximal to adult suicide: a synthesis of findings from psychological autopsy studies. Arch Suicide Res 15:1–15
Cooper J, Appleby L, Amos T (2002) Life events preceding suicide by young people. Soc Psychiatry Psychiatr Epidemiol 37:271–275
Breslow NE, Day NE (1980) Statistical methods in cancer research, Volume I: the analysis of case–control studies. WHO/International Agency for Research on Cancer, Lyon
Mortensen PB, Allebeck P, Munk-Jørgensen P (1996) Population-based registers in psychiatric research. Nord J Psychiatry 50:67–72
Pokorny AD (1983) Prediction of suicide in psychiatric patients. Report of a prospective study. Arch Gen Psychiatry 40:249–257
Mortensen PB (1999) Can suicide research lead to suicide prevention? Acta Psychiatr Scand 99:397–398
HM Government (2011) Consulting on preventing suicide in England: a cross-government outcomes strategy to save lives. http://www.dh.gov.uk
Acknowledgments
The investigation was funded by an American Foundation for Suicide Prevention (New York, USA) and by the Stanley Medical Research Institute (Maryland, USA). The authors are also grateful to the expertise of Dr. Esben Agerbo, National Centre for Research-based Research, University of Aarhus, Denmark in generating the nested case–control dataset for the study.
Conflict of interest
Louis Appleby is National Clinical Director for Health and Criminal Justice, England, and he was formally National Clinical Director for Mental Health, England, when this study was conducted. None of the other authors have any competing interests to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Webb, R.T., Qin, P., Stevens, H. et al. Combined influence of serious mental illness and criminal offending on suicide risk in younger adults. Soc Psychiatry Psychiatr Epidemiol 48, 49–57 (2013). https://doi.org/10.1007/s00127-012-0517-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-012-0517-6