Abstract
Purpose
Patients’ nonadherence to antidepressant treatment hampers cost and efficacy of depression-specific treatment. However, previous studies have failed to find consistent findings in economic effect on nonadherence and also failed to reach consensus in how to measure nonadherence to treatment. The study attempts to investigate income effect on nonadherence to selective serotonin reuptake inhibitors (SSRIs) treatment with clear definitions of nonadherence: self discontinuation of SSRIs (nonpersistence) and under-dose of SSRIs (noncompliance).
Methods
The study extracted data from the National Comorbidity Survey-Replication (NCS-R). The study sample (n = 280) includes adults between the ages of 18 and 64 who were diagnosed with Diagnostic Statistics Manual IV Major Depressive Episode (MDE) at some point during their lifetime and medicated with SSRIs in the past 12 months.
Results
Just above poverty level of family income and no health insurance increased the risk of medication nonpersistence in SSRIs treatment. The study findings confirmed that African Americans were at higher risk of medication noncompliance than Whites (odds ratio, 4.53) and MDE comorbidity was positively associated with medication noncompliance (odds ratio, 4.25).
Conclusions
Low income level, combined with health insurance status, and race/ethnicity, predict nonadherence to antidepressant treatment. The study findings would help physicians and hospitals developing interventional strategies and programs to increase patients’ adherence rates in antidepressant treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
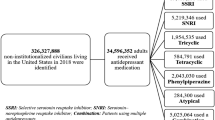
Approximately 27 million Americans, ages 6 years and older, were on antidepressants as of 2005 and the use of antidepressants has constantly increased in the past two decades [1–3]. This trend is partly due to the introduction of the second-generation antidepressants, mostly selective serotonin reuptake inhibitors (SSRIs) [1], which have better tolerability than the first-generation antidepressant, tricyclic antidepressants (TCAs) [4–7]. However, the effectiveness of antidepressant treatment, measured by remission of depressive symptoms and prevention of relapses, has been challenged by patients’ nonadherence to treatment recommendations [8–11]. Patients’ nonadherence to antidepressant treatment accounts for poor outcomes [12, 13] and cost ineffectiveness of the treatment [5, 14, 15]. Nonadherence to antidepressant treatment can be observed in two types of behaviors: self premature discontinuation and taking less or more amounts of medication than prescribed. Previous studies [16, 17] have suggested definitions and terminology to clearly distinguish self premature discontinuation of antidepressants from under- or over-dosing behavior. After carefully reviewing the existing literature on nonadherence in pharmacotherapy [16–22], this study used the terminology suggested by Cramer and colleagues [17] and Sawada and colleagues [16] to define self premature discontinuation of medication as “medication nonpersistence” and under- or over-dosing of medication as “medication noncompliance.” Self premature discontinuation is defined as patients’ discontinuing medication on their own without doctor’s consent. This study considered only under-dosing for noncompliance measured by missed or under-dosed medication days. However, no consensus has been reached in medication noncompliance criteria, i.e., minimum days and minimum amount of medication allowed to be missed to be compliant [14, 20, 23–25].
Factors determining nonadherent behaviors in antidepressant treatment are characteristics of prescribers, patients, and drugs [10, 19, 26]. Prescribers could contribute to patients’ nonadherence to treatment by poorly communicating with patients about the drug therapy and by prescribing inadequate dosage for inadequate medicated duration [26]. Certain characteristics of patients with depression contributing to nonadherence are poor motivation [27], experiencing stigma associated with medication [28], drawing a premature conclusion of full recovery [29], receiving weak social support [30], and not being able to afford medication [15, 19]. In addition, there are drug-specific reasons for nonadherence such as side effects, delayed onset of action, complicated dosing schedule, and drug efficacy [10]. Previous studies [23, 31] have identified risk and mediating factors for nonadherence in antidepressant treatment and have recommended strategies for communing with patients [32], as well as sequences and dosage of antidepressants [33]. While having success in improving antidepressant treatment adherence caused by physician and drug characteristics, patient-related nonadherence issues remain poorly understood. One important patient attribute to nonadherent behaviors in antidepressant treatment, which has been previously overlooked, is family income. Family income is a good gauge to measure cost-effectiveness of, and attitudes toward, antidepressant treatment [34]. Thus, understanding the effect of family income on patients’ nonadherent behaviors would augment efforts in minimizing nonadherence in antidepressant treatment. However, few studied income effect on nonadherent behaviors due to lack of data. Most previous studies examined nonadherence issues with data sets from clinical trials, medical records, and medication monitoring systems [23], which commonly lack information on family income. Information on family income would help to identify individuals at risk for nonadherence and to assist them in more efficient use of limited resources. Studying family income effect on nonadherence in treatment systematically is especially important when physicians perceive low-income patients are less adherent to treatment [35, 36]. This study will also examine other factors that contribute to nonadherent behaviors in antidepressant treatment.
Studying only one class of drug would eliminate the effect of different drug classes on nonadherence. I selected SSRIs to study as antidepressants in treating depressive symptoms and have limited attention to Fluoxetine, Paroxetine, Citalopram, Sertraline, and Fluvoxamine which were available in the US market during 2002 and 2003 [37, 38].
Methods
Data and samples
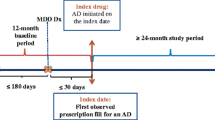
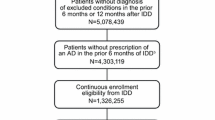
This study extracted data from National Comorbidity Survey-Replication (NCS-R), a nationally representative survey conducted between February 2002 and April 2003 [39, 40]. To examine factors affecting nonadherence to SSRIs treatment for depressive symptoms, this study first selected NCS-R survey adult respondents between the ages of 18 and 64 who met diagnostic criteria for Diagnostic and Statistical Manual IV Major Depressive Episode (MDE) at anytime during their lifetime (n = 1,652). The study then limited samples to only those who had been medicated with one or more SSRIs in the past year at the time of the study (n = 297). NCS-R survey respondents reported antidepressants using either generic or commercial brand names: Prozac is a commercial brand name for Fluoxetine; Paxil for Paroxetine; Celexa for Citalopram; Zoloft for Sertraline; and Luvox for Fluvoxamine. I later excluded those who listed Medicare as their current health insurance, yielding a final sample size of 280. My study sample included a higher proportion of females, Whites, and younger participants than the NCS-R survey sample and participants represented in the study sample were better educated than the NCS-R survey respondents. There were no statistical differences in marital status or family income.
Variables of interest
Patients’ nonadherence to SSRIs treatment was measured in the full year time frame by selecting samples who were on SSRIs treatment within the past year and separately by two behaviors, medication nonpersistence and medication noncompliance. This study used two questions about self discontinuation of the medication, “Did your doctor ask you to stop the medication?” and “Did your doctor agree to stop medication?” to measure medication nonpersistence. If the respondent responded “no” to both of the self discontinuation of medication questions and was no longer on SSRIs at the time of the study, then he or she was defined as a medication nonpersistent respondent.
Medication noncompliance was defined as taking medication for fewer days or at lower amounts than prescribed. The question, “How many days out of 30 did you typically either forget to take it or take less of it than you were supposed to?” was used to measure medication noncompliance. Unfortunately, there is no consensus on medication compliance-rate thresholds to define medication noncompliance. Previous studies have used compliance rates between 80 and 95 % [23] to define noncompliance. This study considered two types of medication noncompliance, strict and liberal, using two different compliance rates, 90 and 80 %, respectively. Ninety-percent compliance rate is 3 days/month as maximum days allowed to miss or under-dose SSRIs to be compliant; 80 % compliance rate is 6 days/month as maximum days allowed to miss or under-dose SSRIs to be compliant.
In this study, I examined effects of comprehensive sets of demographic, economic, and clinical factors as determinants for nonadherent behaviors, nonpersistence and noncompliance, following the literature in medication nonadherence [10, 26, 32, 41, 42]. Demographic and economic characteristics analyzed in the study were sex, age, family income, education, race, current marital status, and health insurance status. Table 1 identifies the demographic and economic variables and presents definitions and descriptive statistics. Sex group had females and males, and four age groups were created with the youngest group comprised individuals between the ages of 18 and 29 years and the oldest group comprised individuals between 55 and 64 years of age. Family income was recoded as very low, low, middle, and high income classes using a poverty index. The poverty index was calculated using annual household income divided by 2001 Federal government poverty threshold [43] with a minimum value of 0 and a maximum value of 17. A respondent was assigned to a very-low-income class if the poverty index was less than 1.5; a respondent was assigned to a low-income class if the poverty index was between 1.5 and less than 3; a respondent was assigned to a middle-income class if the poverty index was between 3 and less than 6; and a respondent was assigned to a high-income class if the poverty index was greater or equal to 6 [39]. The education variable included four categories: less than 12 years (no high-school diploma); 12 years (high-school diploma or GED); 13–15 years (associate degree, vocational degree, or college drop-outs); and 16 years (Bachelor’s degree) of education. Race was redefined to identify four groups: Whites, African Americans, Latinos/as, and other race. The current marital status group was recoded to married and not married groups and health insurance status was re-categorized into three groups: public insurance obtained through government or military programs, private insurance obtained through employers or private purchase, and no health insurance.
Clinical characteristics included types of prescribers, MDE comorbid with other psychiatric disorders within the past 12 months, daily SSRIs dose, and use of other classes of antidepressants besides SSRIs in the past year (Table 1). The types of prescribers were psychiatrists, family doctors, and no information on prescribers. I used MDE comorbid with other psychiatric disorders in the past year as a proxy variable to measure the severity of MDE and treatment response. The respondent was classified as 12-month MDE comorbid if he or she first met the criteria for 12-month DSM-IV MDE, as well as DSM-IV criteria for one or more other psychiatric disorders in the past 12 months [39, 44, 45]. The daily dosage was recoded to four categories: low, medium, high, and unknown dosage groups using recommended minimum and high dose amounts per SSRIs in treating Major Depression by the American Psychiatric Association [46]. If the daily dosage was less than or equal to a minimum dose of recommendation, I assigned the respondent to a low dose group. If the reported daily dosage was greater than a minimum of recommended dosage (>20 mg) but less than 40 mg per day for Fluoxetine, Paroxetine, and Citalopram [47] or greater than a minimum (>50 mg) but less than 100 mg per day for Sertraline [48–50] and Fluvoxamine [51], I assigned the respondent to a medium-dose group. If greater than 40 mg for Fluoxetine, Paroxetine, and Citalopram, or greater than 100 mg for Sertraline and Fluvoxamine, I assigned the respondent to a high-dose group [52]. If the information on daily dosage was missing or unknown, I assigned the respondent to an unknown dose group. The variable for 12-month use of other classes of antidepressants had two categories: use of SSRIs only and use of SSRIs plus other classes of antidepressants, TCAs and/or selective serotonin and norepinephrine reuptake inhibitors (SSNIs), in the past year.
Statistical analysis
Chi-square statistics was used to examine associations between each demographic, economic, and clinical characteristic and the likelihood of nonadherence in SSRIs treatment. Logistic regression was used to obtain maximum likelihood estimates of the patients’ nonadherence to SSRIs treatment controlling for covariates of demographic, economic, and clinical characteristics. Odds ratios and 95 % confidence intervals were reported as logistic regression results. Both Chi-square statistics and logistic regression results were weighted using NCS-R sample weights [53]. Sensitivity analyses were conducted to test whether results on medication noncompliance would change with different compliance criteria, 87 and 83 % compliance rates. Sensitivity analysis results were presented in Appendix. SAS 9.2 version was used for all statistical analyses.
Results
Fifteen percent (n = 41) of the study sample discontinued SSRIs treatment on their own (medication nonpersistence). Thirty-six percent (n = 101) of the study respondents missed or under-dosed SSRIs medication at least 1 day/month; 29 % (n = 80) missed or under-dosed 2 days and more, 18 % (n = 52) missed or under-dosed 3 days and more (strict medication noncompliance), and 9 % (n = 24) missed or under-dosed 6 days and more (liberal medication noncompliance). Almost one-third of the study respondents (31 %) were nonadherent either in medication nonpersistence or in strict medication noncompliance and one-fifth (21 %) were nonadherent in either medication nonpersistence or in liberal medication noncompliance. Medication nonpersistent and noncompliant behaviors were not significantly correlated and only 2 % of the study samples reported both nonpersistent and noncompliant behaviors in the past year.
The average duration of MDE among the study samples was 16 years with the median of 13 years. Sixty-five percent of the sample had experienced a MDE as recently as less than a year ago. The average duration of SSRIs intake was 215 days with the median of 240 days.
Table 2 shows the results for medication nonpersistence. Economic factors, family income and health insurance status, predicted sample respondents’ nonpersistent behaviors in SSRIs treatment. While very low and middle-income class respondents did not significantly differ from high-income class respondents in medication nonpersistence, low-income class respondents were more likely to be nonpersistent in SSRIs treatment than high-income class respondents (odds ratio, 5.93). Respondents without health insurance were significantly less persistent than those with private or employer sponsored health insurance (odds ratio, 5.73). None of the sex, age, education, race, or marital status variables was significantly associated with medication nonpersistence.
Clinical characteristics, daily dosage and 12-month use of SSRIS plus other classes of antidepressants, significantly accounted for SSRIs nonpersistent behaviors. Respondents who could not recall daily dose of SSRIs were at higher risk of nonpersistence than those with low dose (odds ratio, 6.15), while respondents with low dose were at higher risk of nonpersistence than respondents with medium dose (odds ratio, 5.27). Respondents who medicated with other classes of antidepressants in addition to SSRIs in the past 12 months were more likely to be nonpersistent in SSRIs medication than those who were medicated with SSRIs only (odds ratio, 7.14).
Other clinical characteristics, types of prescribers and having 12-month MDE comorbidity, were significantly associated with medication nonpersistent behavior, however, the effects of prescribers and 12-month MDE comorbidity on medication nonpersistence was not significant after controlling for other demographic, economic, and clinical characteristics.
Tables 3 and 4 show results for strict and liberal medication noncompliance, respectively. Racial background of respondents and 12-month MDE comorbidity condition predicted respondents’ medication noncompliant behavior. African Americans were at higher risk of strict medication noncompliance than Whites (odds ratio, 4.53). SSRIs users who were 12-month MDE comorbid with other psychiatric disorders were at higher risk of liberal medication noncompliance than the SSRIs users without 12-month MDE comorbidity condition (odds ratio, 4.25). None of the economic characteristics significantly accounted for either strict or liberal medication noncompliant behavior.
Sensitivity analyses
This study further analyzed different compliance rates of 87 and 83 %, 4 and 5 days per month as maximum days to miss or under-dose medication to be compliant, respectively, to investigate whether main results in medication compliance would change with different compliance rate criteria. Results of these analyses are shown in Appendix. Results of 87 % compliance criterion medication noncompliance were almost identical to ones of strict medication noncompliance and 83 % compliance criterion medication noncompliance results identified no significant factors for medication noncompliance.
Discussion
One-third to one-fifth of the study sample was nonadherent to SSRIs treatment in either medication nonpersistence or noncompliance. This study demonstrated that antidepressant treatment nonadherent behaviors were significantly accounted for by economic factors and racial background. Income and health insurance explained medication nonpersistent behavior in SSRIs treatment, and racial background predicted medication noncompliant behavior [54, 55]. Low-income class respondents were at higher risk of nonpersistence of SSRIs treatment than high-income class respondents, while very-low and middle-income class respondents were not. The finding of a nonlinear income effect on medication nonpersistence may be due to health insurance status. Very-low-income respondents may be eligible for public insurance programs provided by governments, thus, antidepressants could be available to them at no or little cost. However, low-income respondents may not meet the poverty threshold to be eligible for government-sponsored public insurance programs, so out-of-pocket cost of antidepressants may force them to stop medications prematurely. The very-low-income class with public health insurance reported the lowest out of pocket expense to receive mental health treatment. Among the very-low-income class, 56 % had public health insurance and this very-low-income class with public insurance spent $239 on average out of packet in receiving treatment for mental illness not restricted to SSRIs. Meanwhile, the low-income class with a private health insurance paid on average $1,350 out of pocket and those without a health insurance paid on average $895. Out-of-pocket expense may explain why the very-low-income class had a higher adherence rate than the low-income class.
That African Americans were less likely to be compliant in SSRIs treatment than Whites [56] may be explained by a general mistrust among African Americans toward doctors [57] and the medical system [58–60], as well as the prevalence of stigma against mental disorders and fear of dependence among African Americans [61]. However, generalization of this finding is limited due to a small sample size of African Americans in the study.
The study findings, that both low-income class and no health insurance respondents and respondents without knowledge of dosage were at risk of nonpersistence in SSRIs treatment, are one of a few studies in nonadherence to antidepressant treatment that identified patient-related characteristics, income and racial background, as risk factors for patients’ nonadherence to treatment.
This study also confirmed that clinical characteristics, such as therapeutic dose and use of multiple classes of antidepressants, determined medication persistence. Respondents who were medicated with more than a minimum dose of SSRIs were less likely to be nonpersistent in SSRIs treatment than those who took a minimum or less recommended dose [10, 47]. SSRIs treatment with therapeutic dosing may reduce the risk of nonpersistence. However, those with less severe depressive symptoms were likely to be on a minimum dose or less. Thus, the less severely depressed may be at higher risk of nonpersistence than the severely depressed.
That substantial numbers (44 %) of the study samples were on a minimum dose or less may reflect a common practice of antidepressant treatment—initiating treatment with a minimum dose of SSRIs or less, evaluating in 4 weeks whether the dose needed to be adjusted, and increasing the dose if there is absolutely no response to the initial dose [33, 62]—which may contribute to medication nonadherence.
Respondents who were medicated with SSRIs plus other classes of antidepressants in the past year were more likely to be nonpersistent in SSRI treatment than those medicated with SSRIs only in the past year. Use of multiple classes of antidepressants may indicate difficulty in treating depressive symptoms and ineffectiveness of SSRIs treatment, which may contribute to patients’ nonpersistence [13, 63].
This study findings linked nonadherence in SSRIs treatment to MDE comorbidity with multiple psychiatric disorders [11, 64]. Patients diagnosed with MDE comorbidity with anxiety disorder might be at higher risk of side effects and poor response to antidepressant treatment [32]. Side effects and poor response are one of the main reasons for patients’ nonadherence to the treatment [10, 42, 65]. Respondents with MDE comorbidity were at higher risk of both medication nonpersistence and liberal medication noncompliance than those with non comorbid MDE, however, the MDE comorbidity effect on medication nonpersistence weakened after controlling for other factors. This may be explained by weak correlations of MDE comorbidity with other clinical characteristics, daily dose, and 12-month use of multiple classes of antidepressants. Respondents with MDE comorbidity might have been on multiple psychotropic medications, in addition to SSRIs, to treat other psychiatric disorders. The use of multiple medications may increase the risk of noncompliance because of a complicated dosing schedule and/or intention to save cost by taking less than prescribed. When choosing next-step options after failure of SSRIs treatment in relieving depressive symptoms, physicians may consider prescribing once daily dose [23, 66, 67] and generic antidepressants to decease the risk of medication noncompliance.
Findings on prescriber effect on either medication persistence or medication compliance were not strong. A significant association between types of prescribers and medication nonpersistence was found but after controlling for other patient and clinical characteristics, no significant correlation was found between types of prescribers and medication nonpersistence. This contradicts the findings in previous studies that showed combining psychotherapy with antidepressant treatment was effective [68–70]. However, this may be explained by the association of prescribers with therapeutic dose that increases respondents’ persistence in SSRIs treatment. Psychiatrists may be more likely to prescribe therapeutic dose than family doctors [71].
This study found no sex, age, or education effects on either medication nonpersistence or medication noncompliance, which is consistent with previous studies. Demographic variable relation to antidepressant treatment nonadherence has been studied but was found either not significant or inconsistent [41, 42, 65, 72–75].
Unlike many previous studies that have found inconsistent or non-significant economic effects on nonpersistent behaviors in antidepressant treatment [76–80], this study supports that income and cost of antidepressants indeed accounted for nonpersistent behaviors in antidepressant treatment. The study findings also confirmed that racial background and the severity of psychiatric illness condition might contribute to medication noncompliance [10, 32]. Furthermore, this study provided some insights in explaining reasons for inconsistent findings in economic and demographic effects on medication noncompliance in the previous studies—use of different criteria and measurements were reasons for inconsistent findings. As the study findings demonstrate, different criteria for medication compliance identified different risk factors in noncompliance. Clear and consistent criteria in medication compliance research are much needed.
The limitation of the study is a potential selection bias resulting from a small sample size of SSRIs users and a smaller percentage of respondents who reported nonadherence to SSRIs treatment. Medication nonpersistence (15 %) and noncompliance rates to antidepressant treatment (9 to 18 %) in this study were much smaller than reported in the previous studies [9, 14, 41]. These differences may be due to sampling; these study samples were extracted from a survey of respondents representing the general population, not from a treatment population or medical record database. The majority of antidepressant nonadherence studies used data collected from those who received antidepressant treatment or data generated from medical records and databases. NCS-R survey respondents may have under-reported nonpersistent and noncompliant behaviors as well. Although some have suggested monitoring medication intake data to be more accurate in measuring nonadherent behaviors in pharmacotherapy [23], self-report data on nonadherence are as accurate as medical records and databases [81], with additional information on income and other aspects of socioeconomic background.
While this study did not include self-report reasons for medication nonadherence in the analysis due to incomplete responses, the reasons included side effects, attitude or belief on efficacy of medication, and affordability of medication identified in the previous studies [10, 23].
Conclusion
Low income level, combined with health insurance status and race/ethnicity, predict nonadherence to antidepressant treatment. Physicians need to consider patients’ medication nonadherence when prescribing antidepressants and educational intervention built in a routine clinical practice would help reduce risk of nonadherence [23, 66]. Suggested intervention based on the study findings includes discussing medication affordability with patients and investing time in communicating with patients of minority background on the importance of taking dose as instructed. This study’s findings, specific to SSRIs treatment, without loss of generalization, would apply to other class antidepressant treatment, and physicians and hospitals would find them useful in developing interventional strategies and programs to increase patients’ adherence rates in antidepressant treatment.
References
Olfson M, Marcus SC, Druss B, Elinson L, Tanielian T, Pincus HA (2002) National trends in the outpatient treatment of depression. JAMA 287(2):203–209. doi:10.1001/jama.287.2.203
Mojtabai R, Olfson M (2010) National trends in psychotropic medication polypharmacy in office-based psychiatry. Arch Gen Psychiatry 67(1):26–36. doi:10.1001/archgenpsychiatry.2009.175
Olfson M, Marcus SC (2009) National patterns in antidepressant medication treatment. Arch Gen Psychiatry 66(8):848–856. doi:10.1001/archgenpsychiatry.2009.81
Anderson IM (2000) Selective serotonin reuptake inhibitors versus tricyclic antidepressants: a meta-analysis of efficacy and tolerability. J Affect Disord 58(1):19–36. doi:10.1016/s0165-0327(99)00092-0
Montgomery SA, Kasper S (1995) Comparison of compliance between serotonin reuptake inhibitors and tricyclic antidepressants: a meta-analysis. Int Clin Psychopharmacol 9(Suppl 4):33–40
Beasley CM, Koke SC, Nilsson ME, Gonzales JS (2000) Adverse events and treatment discontinuations in clinical trials of fluoxetine in major depressive disorder: an updated meta-analysis. Clin Ther 22(11):1319–1330. doi:10.1016/s0149-2918(00)83028-3
Keller MB, Hirschfeld RMA, Demyttenaere K, Baldwin DS (2002) Optimizing outcomes in depression: focus on antidepressant compliance. Int Clin Psychopharmacol 17(6):265–271
Chakraborty K, Avasthi A, Kumar S, Grover S (2009) Attitudes and beliefs of patients of first episode depression towards antidepressants and their adherence to treatment. Soc Psychiatry Psychiatr Epidemiol 44(6):482–488
Demyttenaere K, Haddad P (2000) Compliance with antidepressant therapy and antidepressant discontinuation symptoms. Acta Psychiatr Scand 101:50–56. doi:10.1111/j.1600-0447.2000.tb10948.x
Masand PS (2003) Tolerability and adherence issues in antidepressant therapy. Clin Ther 25(8):2289–2304
DiMatteo MR, Lepper HS, Croghan TW (2000) Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med 160:2101–2107
Melfi CA, Chawla AJ, Croghan TW, Hanna MP, Kennedy S, Sredl K (1998) The effects of adherence to antidepressant treatment guidelines on relapse and recurrence of depression. Arch Gen Psychiatry 55(12):1128–1132. doi:10.1001/archpsyc.55.12.1128
Melartin TK, Rytsälä HJ, Leskelä US, Lestelä-Mielonen PS, Sokero TP, Isometsä ET (2005) Continuity is the main challenge in treating major depressive disorder in psychiatric care. J Clin Psychiatry 66:220–227
Cantrell CR, Eaddy MT, Shah MB, Regan TS, Sokol MC (2006) Methods for evaluating patient adherence to antidepressant therapy: a real-world comparison of adherence and economic outcomes. Med Care 44(4):300–303
Tournier M, Moride Y, Crott R, Galbaud du Fort G, Ducruet T (2009) Economic impact of non-persistence to antidepressant therapy in the quebec community-dwelling elderly population. J Affect Disord 115(1–2):160–166. doi:10.1016/j.jad.2008.07.004
Sawada N, Uchida H, Suzuki T, Watanabe K, Kikuchi T, Handa T, Kashima H (2009) Persistence and compliance to antidepressant treatment in patients with depression: a chart review. BMC Psychiatry 9:38. doi:10.1186/1471-244X-9-38
Cramer JA, Roy A, Burrell A, Fairchild CJ, Fuldeore MJ, Ollendorf DA, Wong PK (2008) Medication compliance and persistence: terminology and definitions. Value Health 11(1):44–47. doi:10.1111/j.1524-4733.2007.00213.x
Lingam R, Scott J (2002) Treatment non-adherence in affective disorders. Acta Psychiatr Scand 105(3):164–172. doi:10.1034/j.1600-0447.2002.1r084.x
Mitchell AJ, Selmes T (2007) Why don’t patients take their medicine? Reasons and solutions in psychiatry. Adv Psychiatr Treat 13(5):336–346. doi:10.1192/apt.bp.106.003194
McHorney CA, Spain VC, Alexander CM, Simmons J (2009) Validity of the adherence estimator in the prediction of 9-month persistence with medications prescribed for chronic diseases: a prospective analysis of data from pharmacy claims. Clin Ther 31(11):2584–2607. doi:10.1016/j.clinthera.2009.11.030
Claesson S, Morrison A, Wertheimer AI, Berger ML (1999) Compliance with prescribed drugs: challenges for the elderly population. Pharm World Sci 21(6):256–259
Peterson AM, Nau DP, Cramer JA, Benner J, Gwadry-Sridhar F, Nichol M (2007) A checklist for medication compliance and persistence studies using retrospective databases. Value Health 10(1):3–12. doi:10.1111/j.1524-4733.2006.00139.x
Osterberg L, Blaschke T (2005) Adherence to medication. N Engl J Med 353(5):487–497. doi:10.1056/NEJMra050100
Martin BC, Wiley-Exley EK, Richards S, Domino ME, Carey TS, Sleath BL (2009) Contrasting measures of adherence with simple drug use, medication switching, and therapeutic duplication. Ann Pharmacother 43(1):36–44. doi:10.1345/aph.1K671
Hess LM, Raebel MA, Conner DA, Malone DC (2006) Measurement of adherence in pharmacy administrative databases: a proposal for standard definitions and preferred measures. Ann Pharmacother 40(7):1280–1288. doi:10.1345/aph.1H018
Demyttenaere K (1998) Noncompliance with antidepressants: who’s to blame? Int Clin Psychopharmacol 13(Suppl. 2):S19–S25
Bentall RP, Powell P, Nye FJ, Edwards RHT (2002) Predictors of response to treatment for chronic fatigue syndrome. British J Psychiatry 181(3):248–252. doi:10.1192/bjp.181.3.248
Sirey JA, Bruce ML, Alexopoulos GS, Perlick DA, Raue P, Friedman SJ, Meyers BS (2001) Perceived stigma as a predictor of treatment discontinuation in young and older outpatients with depression. Am J Psychiatry 158(3):479–481. doi:10.1176/appi.ajp.158.3.479
Demyttenaere K, Enzlin P, Dewé W, Boulanger B, De Bie J, De Troyer W, Mesters P (2001) Compliance with antidepressants in a primary care setting, 1: beyond lack of efficacy and adverse events. J Clin Psychiatry 62(Suppl 22):30–33
Bosworth HB, Voils CI, Potter GG, Steffens DC (2008) The effects of antidepressant medication adherence as well as psychosocial and clinical factors on depression outcome among older adults. Int J Geriatr Psychiatry 23(2):129–134. doi:10.1002/gps.1852
Sawamura K, Ito H, Koyama A, Tajima M, Higuchi T (2010) The effect of an educational leaflet on depressive patients’ attitudes toward treatment. Psychiatry Res 177(1–2):184–187
Shelton C (2009) Factors impacting the selection of antidepressant treatment in patients with major depressive disorder at risk for nonadherence. CNS Spectr 14(suppl 12):15–19
Rush AJ (2007) Star*d: what have we learned? Am J Psychiatry 164(2):201–204. doi:10.1176/appi.ajp.164.2.201
Isacson D, Bingefors K (2002) Attitudes towards drugs—a survey in the general population. Pharm World Sci 24(3):104–110. doi:10.1023/a:1016127320051
van Ryn M, Burke J (2000) The effect of patient race and socio-economic status on physicians’ perceptions of patients. Soc Sci Med 50(6):813–828. doi:10.1016/s0277-9536(99)00338-x
Woo JKH, Ghorayeb SH, Lee CK, Sangha H, Richter S (2004) Effect of patient socioeconomic status on perceptions of first- and second-year medical students. CMAJ 170(13):1915–1919. doi:10.1503/cmaj.1031474
Dobscha S, Winterbottom L, Snodgrass L (2007) Reducing drug costs at a veterans affairs hospital by increasing market-share of generic fluoxetine. Community Ment Health J 43(1):75–84
Fischer JF, Mowers RM, Ormerod DJ, Burris ES (2001) Driving market share in an integrated health system without therapeutic interchange. J Manag Care Pharm 7(4):283–286
Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC (2005) Twelve-month use of mental health services in the United States: results from the national comorbidity survey replication. Arch Gen Psychiatry 62(6):624–629
Kessler RC, Merikangas KR, Wang PS (2007) Prevalence, comorbidity, and service utilization for mood disorders in the united states at the beginning of the twenty-first century. Annu Rev Clin Psycho 3(1):137–158. doi:10.1146/annurev.clinpsy.3.022806.091444
Burra TA, Chen E, McIntyre RS, Grace SL, Blackmore ER, Stewart DE (2007) Predictors of self-reported antidepressant adherence. Behav Med 32(4):127–134
Brook OH, van Hout HPJ, Stalman WAB, de Haan M (2006) Nontricyclic antidepressants: predictors of nonadherence. J Clin Psychopharmacol 26(6):643–647
Proctor BD, Dalaker J (2002) Current population reports. In: Poverty in the united states: 2001. US Government Printing Office, Washington, DC
Kessler RC, Demler O, Frank RG, Olfson M, Pincus HA, Walters EE, Wang P, Wells KB, Zaslavsky AM (2005) Prevalence and treatment of mental disorders, 1990 to 2003. N Engl J Med 352(24):2515–2523
Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS (2003) The epidemiology of major depressive disorder: results from the national comorbidity survey replication (ncs-r). JAMA 289(23):3095–3105. doi:10.1001/jama.289.23.3095
American Psychiatric Association (2000) Practice guideline for the treatment of patients with major depression. American Psychiatric Association, Arlington
Robinson RL, Long SR, Chang S, Able S, Baser O, Obenchain RL, Swindle RW (2006) Higher costs and therapeutic factors associated with adherence to ncqa hedis antidepressant medication management measures: analysis of administrative claims. J Manag Care Pharmacy 12(1):43–54
Rush AJ, Trivedi MH, Wisniewski SR, Stewart JW, Nierenberg AA, Thase ME, Ritz L, Biggs MM, Warden D, Luther JF, Shores-Wilson K, Niederehe G, Fava M (2006) Bupropion-sr, sertraline, or venlafaxine-xr after failure of ssris for depression. N Engl J Med 354(12):1231–1242. doi:10.1056/NEJMoa052963
Kocsis JH, Schatzberg A, Rush AJ, Klein DN, Howland R, Gniwesch L, Davis SM, Harrison W (2002) Psychosocial outcomes following long-term, double-blind treatment of chronic depression with sertraline vs placebo. Arch Gen Psychiatry 59(8):723–728. doi:10.1001/archpsyc.59.8.723
Keller MB, Kocsis JH, Thase ME, Gelenberg AJ, Rush AJ, Koran L, Schatzberg A, Russell J, Hirschfeld R, Klein D, McCullough JP, Fawcett JA, Kornstein S, LaVange L, Harrison W, For the Sertraline Chronic Depression Study Group (1998) Maintenance phase efficacy of sertraline for chronic depression: a randomized controlled trial. JAMA 280(19):1665–1672. doi:10.1001/jama.280.19.1665
Terra JL, Montgomery SA (1998) Fluvoxamine prevents recurrence of depression: results of a long-term, double-blind, placebo-controlled study. Int Clin Psychopharmacol 13(2):55–62
RTI International-University of North Carolina Evidence-based Practice Center (2007) Comparative effectiveness of second-generation antidepressants in the pharmacologic treatment of adult depression: comparative effectiveness review. Agency for Healthcare Research and Quality, Rockville
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE (2005) Lifetime prevalence and age-of-onset distributions of dsm-iv disorders in the national comorbidity survey replication. Arch Gen Psychiatry 62(6):593–602. doi:10.1001/archpsyc.62.6.593
Fleck DE, Hendricks WL, DelBello MP, Strakowski SM (2002) Differential prescription of maintenance antipsychotics to African American and white patients with new-onset bipolar disorder. J Clin Psychiatry 63(8):658–664
Diaz E, Woods SW, Rosenheck RA (2005) Effects of ethnicity on psychotropic medications adherence. Community Ment Health J 41(5):521–537
Wu C-H, Erickson SR, Piette JD, Balkrishnan R. The association of race, comorbid anxiety, and antidepressant adherence among medicaid enrollees with major depressive disorder. ResSoc Adm Pharmacy. doi:10.1016/j.sapharm.2011.04.002
Armstrong K, Ravenell KL, McMurphy S, Putt M (2007) Racial/ethnic differences in physician distrust in the United States. Am J Public Health 97(7):1283–1289. doi:10.2105/ajph.2005.080762
Boulware LE, Cooper LA, Ratner LE, LaVeist TA, Powe NR (2003) Race and trust in the health care system. Public Health Rep 118(4):358–365
Gamble VN (1997) Under the shadow of Tuskegee: African Americans and health care. Am J Public Health 87(11):1773–1778. doi:10.2105/ajph.87.11.1773
Chakraborty A, King M, Leavey G, McKenzie K (2011) Perceived racism, medication adherence, and hospital admission in african-caribbean patients with psychosis in the United Kingdom. Soc Psychiatry Psychiatr Epidemiol 46(9):915–923. doi:10.1007/s00127-010-0261-8
Fleck DE, Keck PE, Corey KB, Strakowski SM (2005) Factors associated with medication adherence in African American and white patients with bipolar disorder. J Clin Psychiatry 63(8):658–664
Papakostas GI (2009) Managing partial response or nonresponse: switching, augmentation, and combination strategies for major depressive disorder. J Clin Psychiatry 70(Suppl 6):16–25
Thacher JA, Morey E, Craighead WE (2005) Using patient characteristics and attitudinal data to identify depression treatment preference groups: a latent-class model. Depression Anxiety 21(2):47–54
Olfson M, Mojtabai R, Sampson NA, Hwang I, Druss B, Wang PS, Wells KB, Pincus HA, Kessler RC (2009) Dropout from outpatient mental health care in the United States. Psychiatr Serv 60(7):898–907. doi:10.1176/appi.ps.60.7.898
Bull SA, Hu XH, Hunkeler EM, Lee JY, Ming EE, Markson LE, Fireman B (2002) Discontinuation of use and switching of antidepressants: influence of patient–physician communication. JAMA 288(11):1403–1409. doi:10.1001/jama.288.11.1403
Masand PS, Roca M, Turner MS, Kane JM (2009) Partial adherence to antipsychotic medication impacts the course of illness in patients with schizophrenia: a review. Prim Care Companion J Clin Psychiatry 11(4):147–154
McLaughlin T, Hogue SL, Stang PE (2007) Once-daily bupropion associated with improved patient adherence compared with twice-daily bupropion in treatment of depression. American J Therapeutics 14 (2):221-225 210.1097/1001.mjt.0000208273.0000280496.0000208273f
Croghan TW, Melfi CA, Dobrez DG, Kniesner TJ (1999) Effect of mental health specialty care on antidepressant length of therapy. Medical Care 37(Suppl 4):AS20–AS23
Van Voorhees BW, Cooper LA, Rost KM, Nutting P, Rubenstein LV, Meredith L, Wang NY, Ford DE (2003) Primary care patients with depression are less accepting of treatment than those seen by mental health specialists. J Gen Intern Med 18(12):991–1000
Olfson M, Marcus SC, Tedeschi M, Wan GJ (2006) Continuity of antidepressant treatment for adults with depression in the United States. Am J Psychiatry 163(1):101–108. doi:10.1176/appi.ajp.163.1.101
Mcmanus P, Mant A, Mitchell P, Britt H, Dudley J (2003) Use of antidepressants by general practitioners and psychiatrists in Australia. Aust N Z J Psychiatry 37(2):184–189. doi:10.1046/j.1440-1614.2003.01132.x
Tamburrino MB, Nagel RW, Chahal MK, Lynch DJ (2009) Antidepressant medication adherence: a study of primary care patients. J Clin Psychiatry 11(5):205–211
Demyttenaere K, Enzlin P, Dewé W, Boulanger B, De Bie J, De Troyer W, Mesters P (2001) Compliance with antidepressants in a primary care setting, 2: influence of gender and types of impairment. J Clin Psychiatry 62(Suppl 22):34–37
Shigemura J, Ogawa T, Yoshino A, Sato Y, Nomura S (2010) Predictors of antidepressant adherence: results of a Japanese internet-based survey. Psychiatry Clin Neurosci 64:179–186
Lee M-S, Lee H-Y, Kang S-G, Yang J, Ahn H, Rhee M, Ko Y-H, Joe S-H, Jung I-K, Kim S-H (2010) Variables influencing antidepressant medication adherence for treating outpatients with depressive disorders. J Affect Disord 123(1–3):216–221
Kobak KA, Taylor L, Katzelnick DJ, Olson N, Clagnaz P, Henk HJ (2002) Antidepressant medication management and health plan employer data information set (hedis) criteria: reasons for nonadherence. J Clin Psychiatry 63(8):727–732
Lin EH, Von Korff M, Katon W, Bush T, Simon GE, Walker E, Robinson P (1995) The role of the primary care physician in patients’ adherence to antidepressant therapy. Med Care 33(1):67–74
van Geffen E, van der Wal S, van Hulten R, de Groot M, Egberts A, Heerdink E (2007) Evaluation of patients’ experiences with antidepressants reported by means of a medicine reporting system. Eur J Clin Pharmacol 63(12):1193–1199
Demyttenaere K (1997) Compliance during treatment with antidepressants. J Affect Disord 43(1):27–39
Bulloch A, Patten S (2010) Non-adherence with psychotropic medications in the general population. Soc Psychiatry Psychiatr Epidemiol 45(1):47–56. doi:10.1007/s00127-009-0041-5
Rickles NM, Svarstad BL (2007) Relationships between multiple self-reported nonadherence measures and pharmacy records. Res Soc Adm Pharmacy 3(4):363–377. doi:10.1016/j.sapharm.2006.11.001
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Jeon-Slaughter, H. Economic factors in of patients’ nonadherence to antidepressant treatment. Soc Psychiatry Psychiatr Epidemiol 47, 1985–1998 (2012). https://doi.org/10.1007/s00127-012-0497-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-012-0497-6