Abstract
Purpose
Mental disorders are common in young people, yet many do not seek help. Being able to label the problem may facilitate effective help-seeking, but it is not clear which labels are best. This study aims to examine which labels commonly used by young people are associated with a preference for recommended sources of help and treatment.
Method
A national telephone survey was conducted with a randomly selected sample of 2,802 Australian young people aged 12–25 years. Respondents were read out one of three vignettes describing symptoms of a mental disorder, and asked a series of questions regarding labelling of the problem described and related help-seeking preferences and beliefs. Binary logistic regression analyses were used to measure the association between type of label used and help-seeking preferences and beliefs.
Results
Use of the accurate label to describe the problem in the vignette predicted a preference for recommended sources of help with greater consistency than any other labels commonly used by young people. Inaccurate mental health labels did predict some preferences for recommended sources of help and treatment, but not to the extent of the accurate label. Lay labels such as “stress”, “paranoid” and “shy” predicted less intention to seek any help for the problem described in the vignette.
Conclusions
Labelling a disorder accurately does predict a preference for recommended sources of help and a belief in the helpfulness of recommended treatments. Importantly, it is also apparent that some commonly used lay labels cannot do this and indeed may limit appropriate help-seeking and treatment acceptance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
While mental disorders commonly have first onset during adolescence and early adulthood [1–3], and they are most prevalent in this age group [4], it is striking that young people have a low rate of service use [5, 6]. International studies reveal that, across all ages, 35.5–50.3% of “serious” cases in developed countries received no treatment in a 12-month period [7]. Those who receive treatment may do so only after a long delay, varying from months to years [8–10]. Strategies to promote earlier help-seeking are clearly warranted.
There are many factors that influence help-seeking for mental disorders in young people [11–14]. One of these is being able to label or identify a disorder accurately, which has been found to be associated with a preference for recommended forms of help [15]. Indeed, self-diagnosis or labelling of the problem is considered to be a key aspect of the help-seeking process [16–18].
The literature on labelling of mental disorders by the public dates back to the 1950s and is diverse in its definitions, theoretical constructs and applications [16, 19, 20]. For the purpose of this study, ‘labelling’ refers to the lay use of unprompted terms or descriptors to characterise the symptoms of a mental disorder being experienced by a hypothetical or actual person. The term ‘recognition’ has also been used to describe this concept [21]. However, ‘labelling’ is preferred in this instance as it more clearly specifies what is involved, viz. applying a term to the symptoms described, observed or experienced, as opposed to more general acknowledgement that the symptoms are familiar or simply recognised as an unspecified problem.
The importance of labelling has been highlighted in two help-seeking studies. In a study of delay in help-seeking, Thompson et al. [22] found that the average time taken to recognise that the problem was related to anxiety or depression accounted for the majority of the total delay to seek help. Labelling may also assist recognition once professional help is sought. This is demonstrated in a study of young people presenting to general practitioners (GPs) [23]. It found that those young people who identified their problem as a mental illness of some kind at presentation were six times more likely to have their mental health problem correctly identified by the GP compared to those who did not consider that they had a mental illness.
The only vignette-based study to focus on labelling and help-seeking in young people found that accurate labelling of both depression and psychosis was the predictor variable most often associated with the choice of a range of appropriate forms of help or treatment for the person described in the vignette, even when other factors such as age, gender, exposure to someone else with the illness and exposure to campaigns were included in the logistic regression [15]. Accurate labelling of a psychosis vignette was associated with an unprompted choice of a recommended source of help, and with a belief that a psychiatrist, psychologist, antipsychotics and counselling would be helpful for the person described in the vignette. Accurate labelling of depression was associated with the treatment preferences of getting help in less than 1 week, and a belief in the helpfulness of a psychologist, social worker, anti-depressants and counselling. Studies of adults have also reported an association between accurate labelling of disorder (depression and psychosis) and perceived helpfulness of a psychiatrist [24, 25], psychotropic medication [24] and psychotherapy [24].
What is not clear is the degree to which using accurate labels may be any better in facilitating help-seeking compared to a range of other labels commonly used by young people [26]. For example, it is not clear whether using the accurate label for depression is more effective in facilitating help-seeking than the lay term “stress”. In addition, little is known about how these labels affect unprompted help-seeking preferences for oneself, as opposed to a fictional person described in a vignette. Furthermore, the degree to which labelling is associated with help-seeking may vary between disorders. While there is some information about labelling and its association with help-seeking for depression and psychosis [15], little is known about labelling and help-seeking for anxiety disorders. These disorders are of prime importance given they are the most prevalent of all disorder classes in this age group [4] and delays into treatment are the longest [9, 22].
The aim of this study, therefore, was to examine which labels are associated with the choice of help-seeking and treatment options for depression, psychosis and social phobia recommended by mental health professionals [27–29], whilst controlling for a range of other variables known to be associated with help-seeking by young people, including age [11, 14], gender [14, 30] and ethnicity [12, 31]. Treatment choices were assessed using both unprompted responses (where the person gives their choices in response to an open-ended question) and prompted responses (where specific help-seeking options are listed). Unprompted preferences reflect the options that spontaneously come to mind when a young person is put in a hypothetical situation where some sort of help for a mental health problem is warranted. By contrast, prompted ratings of the helpfulness of various kinds of formal and informal help sources, medicines and actions may be more indicative of the acceptability of recommended treatments.
Method
Sample
On behalf of the investigators, the survey company, The Social Research Centre, conducted a computer-assisted telephone survey of 3,746 Australians aged 12–25 years. The sample was contacted using random-digit dialling to cover all of Australia during June to August 2006. Details of the methodology have been reported previously [32].
From the random-digit dialling database, 153,942 calls were made, and just over half of these, 77,951 (50.6%), were unusable as they were businesses, fax machines, modems, or disconnected numbers, and no contact was made with a further 20,390 (13.2%) due to no answer, answering machine or engaged. A further 10,833 (7%) could not have their scope status confirmed due to household refusal or because an appointment made to screen the household was not later needed, and 38,681 (25.1%) were confirmed as out of scope, leaving 6,087 (4%) potential participants. The final response rate was 61.5%, defined as completed interviews (3,746) out of a sample of 6,087 potential participants. There were 835 males and 798 females in the age group 12–17 years, and 958 males and 1,155 females in the 18–25-year age group. The mean age for the 12–17-year age group was 14.64 (SD = 1.67) and for the 18- to 25-year age group, the mean was 21.01 (SD = 2.27). Of the whole sample of young people, 52.1% were female, 16.6% spoke a language other than English at home, and 3.3% were of Aboriginal and/or Torres Strait Islander origin.
There was little variation in response rate by geographic region (state), with response rates ranging from 57.4 to 69.9%, and a very small difference in response rate between metropolitan (61.6%) and regional/rural (61.3%) locations. The age and gender differences between responders and non-responders are not available, as the respondents’ specific age and gender could not be determined before in-scope status was established. However, the age and gender proportions in the sample are similar to the national population: 43.6% of 12- to 17-year-olds in the sample compared to 42.4% in the population, and 47.9% of males in the sample compared to 51.2% in the population.
Interview
The interview was based on a vignette of a young person with a mental disorder [32]. On a random basis, respondents were read out one of four vignettes: depression, depression with alcohol misuse, social phobia and psychosis. The present paper focusses on the depression (n = 929), psychosis (n = 968) and social phobia (n = 905) vignettes as they each represent single diagnostic groups. The vignettes were written to satisfy DSM-IV [33] criteria and validated against clinician diagnosis [26]. Respondents were read out a vignette of the same gender and age group as their own. Respondents aged 12–17 years were read out a version of the vignette describing a 15-year-old; 18- to 25-year-olds were read out a version of the vignette portraying a 21-year-old. The details of the vignette were altered slightly to be age appropriate (e.g. reference to functioning at school vs. on a course).
After being presented with the vignette, respondents were asked a series of questions to assess a number of areas, including their labelling of the disorder in the vignette; what they would do to seek help if they had the problem; beliefs about sources of help and treatments; and socio-demographic characteristics.
Labelling of the problem
Description of the vignette was followed by an open-ended question asking, “What, if anything, do you think is wrong with John (male version)/Jenny (female version)?” for which unprompted responses were recorded. Interviewers recorded responses according to pre-coded response categories (depression, schizophrenia, psychosis, mental illness, stress, nervous breakdown, psychological/mental/emotional problem, has a problem, cancer, nothing, do not know) derived from a content analysis of responses to the same questions in earlier surveys [34, 35]. A content analysis of responses that did not fit these pre-coded categories led to post-coding of 56 other categories. Many of these responses were used to describe the social phobia vignette, which had not been used in surveys previously. For simplicity, the post-coded response categories that are amongst the four most common and the most accurate responses for each vignette are described here, as these are the focus of analysis in this paper. They include anxiety/anxious, drugs, eating disorder (including the responses anorexia, bulimia, eating disorder), low self-confidence/low self-esteem, physical problem (including the responses glandular fever, chronic fatigue syndrome, diabetes), shy, and social phobia (including the responses social phobia, social anxiety or anxiety disorder).
Help-seeking items
Respondents were then read a range of help-seeking questions that included two components. Firstly, there was a question to ascertain the respondent’s help-seeking preferences without prompting as an indicator of the kind of help they might seek of their own accord and, secondly, there was a series of questions that sought their opinion about the helpfulness of a range of different sources of help and treatment for the person described in the vignettes in order to measure acceptability of treatments. Whilst a broad range of help-seeking and treatment items were covered in the interview, those selected for analysis in this paper are based on a consensus of mental health professionals about which interventions are likely to be helpful for the young people portrayed in the vignettes. This consensus was based on the results of a postal survey of health professionals (GPs, psychologists, psychiatrists and mental health nurses) conducted between September 2006 and January 2007 to determine the sources of help, treatment options and self-help actions that professionals recommend. Details of the methodology and sample are reported elsewhere [27–29].
Following the labelling question, the young people were asked “If you had a problem right now like (John/Jenny), would you go for help?” Responses were coded as either “yes”, “no”, “don’t know” or “refused”. Respondents were then asked “Where would you go?” for which unprompted responses were recorded. Interviewers recorded responses according to pre-coded response categories according to the source of help that the respondent would seek help from: both parents, mother, father, other person (which was then specified), a service (which was then specified).
This was followed by the prompted help-seeking items: “There are a number of people who could possibly help John/Jenny. I’m going to read out a list and I’d like you to tell me whether they would be helpful, harmful or neither to John/Jenny”. Then the following list was read out: a general practitioner or family doctor, a counsellor, a telephone counselling service, a psychologist, and a psychiatrist.
The same helpfulness rating scale was used for two further sets of questions. The young person was asked “Do you think the following medicines are likely to be helpful, harmful or neither for John/Jenny? Again, if you are unsure, that’s fine, just let me know”. A range of medicines was read out including anti-depressants and antipsychotics. This was followed by the question “Do you think the following are likely to be helpful, harmful or neither for John/Jenny?” A range of actions were read out including: becoming physically more active, getting relaxation training, receiving counselling, receiving cognitive behaviour therapy (CBT), joining a support group of people with similar problems, as well as cutting down on use of alcohol, cigarettes and marijuana.
Socio-demographic items
Respondents were asked a range of socio-demographic questions to ascertain their age, gender, and language spoken at home. Apart from asking respondents about their current involvement in education or employment, highest level of education was not recorded due to the high correlation of years of education with age in this age group.
Ethics approval
Ethics approval was obtained from The University of Melbourne Human Research and Ethics Committee.
Data analysis
All analyses were carried out using PASW Statistics version 18.0 and SPSS Version 17.0. Only the accurate label and the four most common labels for each vignette are reported here, as these are the labels most commonly used in the community and therefore the findings that relate to these are most relevant. Accurate labelling is defined as those labels that approximate the DSM-IV [33] diagnosis upon which the vignettes were based and validated. The rate of accurate labelling, as well as the rate of use of all other labels to describe the vignettes, was analysed using percent frequencies for each of the three vignettes and is described in detail elsewhere [26].
To ensure the reliability of the coding of the labels used, a preliminary reliability study was needed to measure inter-rater agreement in regard to the 56 post-coded response categories. A second rater reviewed a random sample of 100 uncoded responses to the labelling question for each of the three vignettes and coded these responses according to the 56 post-coded response categories. Responses that were assigned to the pre-coded response categories were excluded. The selected 300 uncoded responses were randomly ordered and the second rater was blinded to the vignette upon which the responses were based. The two sets of 300 responses were then analysed using the kappa measure of agreement to assess agreement in coding the labels used.
To provide a measure of population uncertainty in regard to labelling of the three disorders described in the vignettes, an analysis of the frequency of the number of different labels used to identify the problem in the vignette per respondent was also undertaken. A further analysis was undertaken to determine whether number of labels used varied according to age, gender or vignette. Because the distribution of number of labels was highly skewed, non-parametric Mann–Whitney U and Kruskal–Wallis tests were used.
The principal form of analysis was then a series of univariate and multipredictor binary logistic regression analyses to examine the association between label use and help-seeking preferences whilst controlling for other known predictors of help-seeking. The accurate and most common labels for each vignette were the predictor variables of primary interest. However, as previously highlighted, some respondents used more than one label to describe the problem in the vignette; hence, a check was carried out for multicollinearity by examining the degree of correlation between the labels for each vignette. The only significant correlation found was for the social phobia vignette between the labels “depression” and “anxiety” (r = 0.177).
The covariates in the logistic regression analyses were the socio-demographic factors known to be associated with help-seeking, that is age, gender and language spoken at home (ethnicity). All predictor variables were dichotomous except for age (12–25 years) which was analysed as a continuous variable.
The help-seeking preference outcome variables were derived from the unprompted help-seeking items and the prompted rating of a range of help-seeking and treatment options. In regard to the unprompted items, the first question was “If you had a problem right now like (John/Jenny), would you go for help?”. Responses were dichotomized into “yes” and “no”/“do not know”. From the sub-set of respondents who answered “yes” to this question, unprompted preferences regarding sources of help were derived from the pre-coded verbatim responses to the question “Where would you go?” which included parent, family member, friend, doctor/General Practitioner, counsellor, and mental health specialist. Ratings of the prompted help-seeking and treatment items were dichotomized for the analysis into “helpful” versus “other responses”.
Univariate binary logistic regression analyses examined the association between each of the predictor variables and each of the help-seeking outcome variables. Multipredictor binary logistic regression analyses were then used to examine which of the predictor variables remained significant in their association with each of the help-seeking and treatment outcome variables, adjusting for other predictors and covariates. Although some of the associations that were significant in the univariate binary logistic regression analysis became non-significant in the multipredictor binary logistic regression analysis, the regression coefficients did not differ greatly in magnitude, hence no further sequential regression analyses were conducted and only the significant results of the multipredictor logistic regression analyses are reported here. The regression analyses generated a large number of odds ratios. In order to summarise these and show where there was consistency of results, the findings were summarised in tables, with the magnitude of associations indicated as small, medium, or large according to Rosenthal’s criteria [36].
Results
Inter-rater agreement on coding of labels
The kappa value for inter-rater agreement on coding of most labels analysed in this paper was above 0.8, representing very good agreement. The exceptions were 0.72 for “physical problem” and 0.66 for “psychological problem”, representing good and moderate agreement, respectively.
Number of labels used
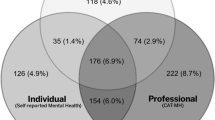
The frequency distribution of the number of respondents who used 1 through to 5 or more labels was analysed for the total sample and showed that 67.4% of respondents used one label, 24.2% used two labels, 6.5% used three labels, 1.4% used four labels, and 0.4% used 5 or more labels. A Mann–Whitney U Test revealed a significant difference in number of labels used per respondent according to gender, with females using significantly more labels than males (females, mean = 1.47; males, mean = 1.39; Z = −3.83; p < 0.001), and a significant difference according to age group, with those aged 18–25 years using more labels than 12- to 17-year-olds (12–17 years, mean = 1.41; 18–25 years, mean = 1.45; Z = −2.76; p = 0.006). A Kruskal–Wallis test revealed a significant difference in the number of labels used according to vignette, with the most labels used for the social phobia and psychosis vignettes and the least for the depression vignette (social phobia vignette, mean = 1.45; psychosis vignette, mean = 1.45; depression vignette, mean = 1.37; χ 2 = 12.50; p = 0.002).
Unprompted preferences for sources of help
Results from the multipredictor binary logistic regression analyses are summarised in Table 1. Results of analyses regarding the outcome variable “parent” are not included as all findings were non-significant.
For the depression vignette, use of the accurate label “depression” predicted a preference for help from a counsellor (OR = 1.76, p = 0.024), and the label “physical problem” predicted a preference for help from a doctor/GP (OR = 2.68, p = 0.003). The label “stress” predicted less intention to seek any help for the hypothetical situation described in the vignette (OR = 0.49, p = 0.021).
For the psychosis vignette, use of the accurate label “schizophrenia/psychosis” predicted preference for doctor/GP as a source of help (OR = 1.77, p = 0.001), as did the label “mental illness”, although the strength of the association for the latter was lower (OR = 1.59, p = 0.021). The accurate label also predicted a preference for not seeking help from a friend (OR = 0.37, p < 0.001), whereas those who used the label “depression” were more likely to prefer informal sources of help including family member (OR = 1.51, p = 0.012) and friend (OR = 2.09, p < 0.001). “Depression” was also the only label that predicted an intention to seek any help for the hypothetical vignette scenario (OR = 1.56, p = 0.035), whereas the label “paranoid” predicted less intention to seek any help (OR = 0.40, p = 0.028).
For the social phobia vignette, the correct label predicted an intention to seek any help (OR = 2.34, p = 0.049) and a preference for help from a doctor/GP (OR = 2.31, p = 0.025) and especially a mental health specialist (OR = 4.99, p < 0.001). The only other label that predicted a preferred source of help was the label “anxiety/anxious” for doctor/GP (OR = 2.15, p = 0.007). The label “shy” predicted less intention to seek any help for the hypothetical vignette scenario (OR = 0.59, p = 0.008).
Prompted responses regarding the helpfulness of professionals
Significant results from the multipredictor logistic regression analyses are listed in Table 2. Results of analyses regarding the outcome variable “telephone counsellor” are not included as all findings were non-significant. Overall, the accurate label for both the depression and psychosis vignettes predicted a belief in the helpfulness of the most number of recommended professionals compared to other labels. For the depression vignette, the label “depression” predicted a belief in the helpfulness of a counsellor (OR = 2.00, p = 0.01) and a psychologist (OR = 1.83, p < 0.001). The only other significant association was for the label “eating disorder” that predicted a belief in the helpfulness of a psychologist (OR = 2.49, p = 0.035). The accurate label for the psychosis vignette predicted a belief in the helpfulness of a GP (OR = 2.07, p = 0.002), psychologist (OR = 1.52, p = 0.035) and psychiatrist (OR = 1.86, p < 0.001). “Mental illness” was the only other label to predict a belief in the helpfulness of a professional (psychiatrist) (OR = 1.59, p = 0.021), although again the association was not as strong.
Results for the social phobia vignette reveal that the label “depression” predicted a belief in the most professionals, GP (OR = 2.46, p = 0.004) and psychiatrist (OR = 1.56, p = 0.046), whereas the accurate label predicted a belief in the helpfulness of one type of professional, a psychologist (OR = 3.67, p = 0.034). The label “shy” predicted a belief in the helpfulness of a counsellor (OR = 2.03, p = 0.045).
Prompted responses regarding the helpfulness of medications
As outlined in Table 2, results from the multipredictor binary logistic regression analyses regarding a belief in the helpfulness of medications reveal that while the accurate labels for all the vignettes predicted a belief in the helpfulness of medication, so too did a number of other labels. For the psychosis vignette, the accurate label predicted a belief in the helpfulness of both anti-depressants (schizophrenia/psychosis: OR = 1.53, p = 0.004) and antipsychotics (schizophrenia/psychosis: OR = 3.32, p < 0.001) The label “paranoid” also predicted a belief in the helpfulness of antipsychotics (OR = 2.25, p = 0.048). For the social phobia vignette, the labels “social phobia” (OR = 2.815, p = 0.002) and “depression” (OR = 2.80, p < 0.001) predicted a belief in the helpfulness of anti-depressants. In contrast, for the depression vignette, “depression” was the only label to predict a belief in the helpfulness of anti-depressants (OR = 2.39, p < 0.001), while other common lay labels, that is, “stress” (OR = 0.53, p = 0.047), “drugs” (OR = 0.31, p = 0.004), and “physical problem” (OR = 0.47, p = 0.04), predicted a belief that they would not be helpful.
Prompted responses regarding the helpfulness of particular actions
As outlined in Table 3, the accurate labels for each of the vignettes were the only labels to predict a belief in the helpfulness of psychological therapies, that is, counselling (depression: OR = 2.09, p = 0.006; psychosis: OR = 3.23, p = 0.003) and CBT (social phobia: OR = 3.58, p < 0.001). The only other action predicted by the accurate labels was a belief in the helpfulness of cutting down on use of alcohol for the depression vignette (OR = 1.84, p = 0.012) and the psychosis vignette (OR = 2.11, p = 0.006). For the psychosis vignette, the label “depression” predicted the most number of beliefs in recommended actions, including the helpfulness of physical activity (OR = 2.07, p = 0.004), and cutting down on the use of alcohol (OR = 2.04, p = 0.014), cigarettes (OR = 1.84, p = 0.025) and marijuana (OR = 1.88, p = 0.04), while the label “mental illness” predicted a belief in the helpfulness of relaxation training (OR = 1.96, p = 0.019) and a support group (OR = 2.56, p = 0.015). Labelling the depression vignette as “stress” was strongly associated with a belief in the helpfulness of relaxation training (OR = 8.44, p = 0.036).
Discussion
This is the first study to examine the relative effectiveness of a range of common labels used by young people in predicting help-seeking preferences. Of all the common labels a young person might use, the accurate labels were the ones that most consistently predicted a preference for professionally recommended forms of help. This is particularly the case for professional sources of help, medications and psychological therapies. These findings were consistent across the three different mental disorder vignettes. Whilst inaccurate mental health labels did predict some preferences for recommended sources of help and treatment for the psychosis and social phobia vignettes, this was not to the extent of the accurate label.
Most concerning is that lay labels such as “stress”, “paranoid” and “shy” were associated with reduced likelihood of seeking any help if the young person themselves were to have a problem like the one described in the vignette. In addition, the use of more general lay labels such as “stress”, “drugs” and “physical problem” were associated with the young persons sampled considering anti-depressants to not be helpful in the case of depression.
This is the first study to examine which labels predict a preference for recommended forms of help and treatment for an anxiety disorder. Compared to the depression and psychosis vignettes, accurately labelling the social phobia vignette predicted a preference for a more specific source of help, which is a mental health specialist, and a specific treatment, CBT, with large and medium effect sizes, respectively. Using the label “depression” was almost as effective as the accurate label in predicting a preference for recommended sources of help, although the associations were less consistent and the effect sizes tended to be smaller. However, these labels were amongst the least common [26], hence the potential benefits of accurate labelling at a population level will not be fully realised until community education efforts targeting anxiety disorders are enhanced, particularly given their high prevalence [4].
In regard to the depression and psychosis vignettes, many of the findings from this study replicate earlier findings from a study of young people regarding the association between accurate label use and belief in the helpfulness of recommended sources of help including, for depression, a belief in the helpfulness of a psychologist, anti-depressants and counselling, and for psychosis, a belief in the helpfulness of a psychologist, a psychiatrist, antipsychotics (anti-depressants not tested) and counselling [15]. A similar pattern of findings has also been reported in adult studies, that is, an association between accurate labelling and the belief in the helpfulness of a psychiatrist [24, 25], psychotropic medication [24] and psychotherapy [24]. Another similarity is that when “depression” is used to label the problem in a vignette, its association with help-seeking preferences and treatment beliefs differs between vignettes and has the most associations when applied accurately. Interestingly, in this study, the phenomenon has been found to apply to social phobia as well. It may be that the term “depression” has become a ubiquitous label for any mental health problem, but is more effective when applied accurately to a depressive disorder.
The key differences in findings to the earlier youth study mainly relate to the psychosis vignette. In the previous study other mental health labels, particularly “mental illness”, were more often associated with a belief in recommended sources of help and treatment and the association between the accurate label and GP was non-significant. Furthermore, the earlier study did not find an association between accurate labelling of depression and psychosis and a belief in the helpfulness of cutting down on alcohol use. These differences in results may reflect an improvement in mental health literacy over time, as evidenced by an increase in accuracy of labelling for depression from 48.7% in 2001, to 69.1% in 2006, and for psychosis an improvement from 25.3 to 33.4% [26, 35], or differences in the range of covariates adjusted for in the two studies.
The present study has a number of strengths including use of a large national sample covering the age range when onset is most likely to occur, use of vignettes with validated labels, and high inter-rater reliability regarding label coding. A focus on labels in common use maximises the relevance of the findings. Although the in-scope status of some households contacted could not be established and this limits the capacity to absolutely define the representativeness of the survey, the similarity of the sample to the national population in regard to age, gender and residential location supports the potential generalizability of the results. However, the results must also be considered in light of a number of limitations. This study has focused on help-seeking intentions and preferences rather than actual help-seeking behaviour. While the likelihood that these translate into behaviour has been supported [14, 37, 38], it has also been questioned [25, 39]. It could be argued that the large number of associations examined could lead to Type I errors. Excluding associations with covariates, significant associations were found for 15.2% of the help-seeking preferences variables, 20.9% of the belief in professional and medications variables, and 10% of the belief in particular actions variables, compared to an expected 5% by chance if the null hypothesis was true. The fact that these associations are in the expected direction and replicate earlier findings further leads to greater confidence in the findings. Another limitation concerns the way the questions eliciting prompted and unprompted responses were framed. A comparison of findings between unprompted and prompted results within the study is difficult, as the former asked questions in relation to the respondent themselves having the problem and the latter in relation to the person described in the vignette. It would be expected that given the tendency of young people to have a higher threshold of perceived need for help for self than for a peer [40], that more associations may have been found if the unprompted questions were asked in relation to the vignette character. Finally, the majority of effect sizes were small to medium and this might potentially limit their public health significance. However, this must also be considered in relation to the relative cost of changing knowledge about labelling disorders, which can be achieved at a relatively low cost through targeted community awareness initiatives. Given the cost, even small effects may be important for guiding public health action.
When designing studies of recognition and labelling, it has been argued that “From a population perspective, recognition that someone has a mental health problem is more important than the recognition of a specific diagnosis” [39]. The results of the current study indicate that this may not be so. While being able to accurately label a disorder is unlikely in itself to be sufficient in guiding a person to appropriate help, it may be an indicator of good mental health literacy [21], and as such it may be a vital trigger for accessing a schema of how to deal with a certain kind of mental disorder. However, further research regarding the role of labelling in help-seeking relative to other known mediators of help-seeking is required. A consideration of these factors in the context of actual cases of help-seeking would also be beneficial in clarifying the extent to which labelling facilitates help-seeking in real life.
In conclusion, labelling a disorder accurately does predict a preference for recommended sources of help and a belief in the helpfulness of recommended treatments above and beyond all other common labels used by young people. Importantly, it is also apparent that commonly used lay labels may limit appropriate help-seeking and treatment acceptance. Improving the accuracy of labelling of mental disorders, along with a consideration of other factors that facilitate help-seeking, may improve the effectiveness of community awareness initiatives in reducing the gap between young people’s need for treatment and receipt of treatment.
References
Amminger GP, Harris MG, Conus P, Lambert M, Elkins KS, Yuen HP, McGorry PD (2006) Treated incidence of first-episode psychosis in the catchment area of EPPIC between 1997 and 2000. Acta Psychiatr Scand 114:337–345
Australian Bureau of Statistics (2007) National survey of mental health and wellbeing, 2007. Confidentialised Unit Record File (CURF) No 2826
Kessler RC, Angermeyer M, Anthony JC, De Graaf R, Demyttenaere K, Gasquet I, De Girolamo G, Gluzman S, Gureje O, Haro JM, Kawakami N, Karam A, Levinson D, Medina Mora ME, Oakley Browne MA, Posada-Villa J, Stein DJ, Adley Tsang CH, Aguilar-Gaxiola S, Alonso J, Lee S, Heeringa S, Pennell B-E, Berglund P, Gruber MJ, Petukhova M, Chatterji S, Ustun TB (2007) Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry 6:168–176
Australian Bureau of Statistics (2007) National survey of mental health and wellbeing: summary of results, Cat. no. 4326.0. http://www.abs.gov.au/AUSSTATS/abs@.nsf/mf/4326.0. Accessed 23 November 2008
Slade T, Johnston A, Oakley Browne MA, Andrews G, Whiteford H (2009) 2007 National Survey of Mental Health and Wellbeing: methods and key findings. Aust N Z J Psychiatry 43:594–605
Verger P, Guagliardo V, Gilbert F, Rouillon F, Kovess-Masfety V (2010) Psychiatric disorders in students in six French universities: 12-month prevalence, comorbidity, impairment and help-seeking. Soc Psychiatry Psychiatr Epidemiol 45:189–199
The WHO World Mental Health Survey Consortium (2004) Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. J Am Med Assoc 291:2581–2590
Schimmelmann BG, Conus P, Cotton S, McGorry P, Lambert M (2007) Pre-treatment, baseline, and outcome differences between early onset and adult-onset psychosis in an epidemiological cohort of 636 first-episode patients. Schizophr Res 95:1–8
Wang PS, Angermeyer M, Borges G, Bruffaerts R, Chiu WT, de Girolamo G, Fayyad J, Gureje O, Haro JM, Huang YQ, Kessler RC, Kovess V, Levinson D, Nakane Y, Browne MAO, Ormel JH, Posada-Villa J, Aguilar-Gaxiola S, Alonso J, Lee S, Heeringa S, Pennell BE, Chatterji S, Ustun TB (2007) Delay and failure in treatment seeking after first onset of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry 6:177–185
O’Callaghan E, Turner N, Renwick L, Jackson D, Sutton M, Foley SD, McWilliams S, Behan C, Fetherstone A, Kinsella A (2010) First episode psychosis and the trail to secondary care: help-seeking and health-system delays. Soc Psychiatry Psychiatr Epidemiol 45:381–391
Gasquet I, Chavance M, Ledoux S, Choquet M (1997) Psychosocial factors associated with help-seeking behavior among depressive adolescents. Eur Child Adolesc Psychiatry 6:151–159
Zwaanswijk M, Verhaak PFM, Bensing JM, van der Ende J, Verhulst FC (2003) Help seeking for emotional and behavioural problems in children and adolescents––a review of recent literature. Eur Child Adolesc Psychiatry 12:153–161
Sheffield JK, Fiorenza E, Sofronoff K (2004) Adolescents’ willingness to seek psychological help: promoting and preventing factors. J Youth Adolesc 33:495–507
Rickwood D, Deane FP, Wilson CJ, Ciarrochi J (2005) Young people’s help-seeking for mental health problems. AeJAMH (Australian e-Journal for the Advancement of Mental Health) 4:[3] www.auseinet.com/journal/vol4iss3suppl/rickwood.pdf. Accessed 21 April 2006
Wright A, Jorm AF, Harris MG, McGorry PD (2007) What’s in a name? Is accurate recognition and labelling of mental disorders by young people associated with better help-seeking and treatment preferences? Soc Psychiatry Psychiatr Epidemiol 42:244–250
Angel RJ, Thoits P (1987) The impact of culture on the cognitive structure of illness. Cult Med Psychiatry 11:465–494
Vogel DL, Wester SR, Larson LM, Wade NG (2006) An information-processing model of the decision to seek professional help. Prof Psychol Res Pr 37:398–406
Biddle L, Donovan J, Sharp D, Gunnell D (2007) Explaining non-help-seeking amongst young adults with mental distress: a dynamic interpretive model of illness behaviour. Sociol Health Illn 29:983–1002
D’Arcy C, Brockman J (1976) Changing public recognition of psychiatric symptoms? Blackfoot revisited. J Health Soc Behav 17:302–310
Link BG, Cullen FT, Struening EL, Shrout PE, Shrout PE, Dohrenwend BP (1989) A modified labeling theory approach to mental disorders: an empirical assessment. Am Sociol Rev 54:400–423
Jorm AF (2000) Mental health literacy: public knowledge and beliefs about mental disorders. Br J Psychiatry 177:396–401
Thompson A, Issakidis C, Hunt C (2008) Delay to seek treatment for anxiety and mood disorders in an Australian clinical sample. Behav Change 25:71–84
Haller DM, Sanci LA, Sawyer SM, Patton GC (2009) The identification of young people’s emotional distress: a study in primary care. Br J Gen Pract 59:e61–e70
Angermeyer M, Holzinger A, Matschinger H (2009) Mental health literacy and attitude towards people with mental illness: a trend analysis based on population surveys in the eastern part of Germany. Eur Psychiatry 24:225–232
Goldney RD, Dunn KI, Dal Grande E, Crabb S, Taylor A (2009) Tracking depression-related mental health literacy across South Australia: a decade of change. Aust N Z J Psychiatry 43:476–483
Wright A, Jorm AF (2009) Labels used by young people to describe mental disorders: factors associated with their development. Aust N Z J Psychiatry 43:946–955
Lubman DI, Hides L, Jorm AF, Morgan AJ (2007) Health professionals’ recognition of co-occurring alcohol and depressive disorders in youth: a survey of Australian general practitioners, psychiatrists, psychologists and mental health nursesusing case vignettes. Aust N Z J Psychiatry 41:830–835
Jorm AF, Morgan AJ, Wright A (2008) A comparison of clinician, youth and parent beliefs about helpfulness of interventions for early psychosis. Psychiatr Serv 59:1115–1120
Jorm AF, Morgan AJ, Wright A (2008) Interventions that are helpful for depression and anxiety in young people: a comparison of clinicians’ beliefs with those of youth and their parents. J Affect Disord 111:227–234
Biddle L, Gunnell D, Sharp D, Donovan JL (2004) Factors influencing help seeking in mentally distressed young adults: a cross-sectional survey. Br J Gen Pract 54:248–253
Hsu L, Alden LE (2008) Cultural influences on willingness to seek treatment for social anxiety in Chinese- and European-heritage students. Cultur Divers Ethnic Minor Psychol 14:215–223
Jorm AF, Wright A, Morgan AJ (2007) Beliefs about appropriate first aid for young people with mental disorders: findings from an Australian national survey of youth and parents. Early Interv Psychiatry 1:61–70
American Psychiatric Association (1994) Diagnostic and statistical manual for mental disorders: 4th edition (DSM-IV). American Psychiatric Association, Washington
Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, Pollitt P (1997) “Mental health literacy”: a survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Med J Aust 166:182–186
Wright A, Harris MG, Wiggers JH, Jorm AF, Cotton SM, Harrigan SM, Hurworth RE, McGorry PD (2005) Recognition of depression and psychosis by young Australians and their beliefs about treatment. Med J Aust 183:18–23
Rosenthal JA (1996) Qualitative descriptors of strength of association and effect size. J Soc Serv Res 21:37–59
Ajzen I (1991) The theory of planned behaviour. Organ Behav Hum Decis Process 50:179–211
Wilson CJ, Deane FP, Marshall KL, Dalley A (2008) Reducing adolescents’ perceived barriers to treatment and increasing help-seeking intentions: effects of classroom presentations by general practitioners. J Youth Adolesc 37:1257–1269
Klineberg E, Biddle L, Donovan J, Gunnell D (2010) Symptom recognition and help seeking for depression in young adults: a vignette study. Soc Psychiatry Psychiatr Epidemiol. doi:10.1007/s00127-010-0214-2
Raviv A, Raviv A, Vago-Gefen I, Fink AS (2009) The personal service gap: factors affecting adolescents’ willingness to seek help. J Adolesc 32:483–499
Acknowledgments
Financial support was provided by the National Health and Medical Research Council, the Sidney Myer Health Fund, the Colonial Foundation, and “beyondblue: the national depression initiative”. Amy Morgan and Anna Kingston assisted with components of the data analysis. Nicholas Allen provided advice regarding data analysis and development of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wright, A., Jorm, A.F. & Mackinnon, A.J. Labels used by young people to describe mental disorders: which ones predict effective help-seeking choices?. Soc Psychiatry Psychiatr Epidemiol 47, 917–926 (2012). https://doi.org/10.1007/s00127-011-0399-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-011-0399-z