Abstract
Purpose
Chronic somatic complaint (CSC) can cause significant impairment of psychosocial functioning and therefore is of considerable interest in medicine, psychology, and related health sciences. To date, the type, distribution, and associated factors of CSC have been examined in only a limited number of studies. Main research questions of this investigation focused on the prevalence of CSC, the predictive validity of parent reports, and the associations with social class, health status, and psychosocial distress.
Methods
Data were obtained from a population-based, German-wide representative Health Survey (N = 1,027 self-reports, and parent reports from 11- to 18-year-olds). In addition to study-specific items, the standardized Giessen Physical Complaints Inventory for Children and Adolescents was used (GPCI).
Results
The most frequent CSCs in self-report forms were skin impurities/pimples, cold hands, and fatigue; older adolescents, especially females, were at a higher risk for CSC. The sensitivity of parent reports in all complaints observed was very low (Med = 0.21) and specificity varied between 0.94 and 1.00. Parents significantly underestimated CSC that were not externally observable, as well as CSC in males. Across different predictors and CSC dimensions, psychosocial distress showed the highest predictive value.
Conclusions
The results provide data regarding the subjective physical health of adolescents, as well as an empirical reference to evaluate the distribution of chronic symptoms in specific clinical populations (which is needed for prevention and treatment).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Somatic complaints can be understood as body-related sensations or perceptions with subjectively experienced unpleasant qualities (dysesthesias). They range from pain to other physical sensations, such as burning, prickling, itching, and irritating changes in bodily functions or areas [29]. When no sufficient organic etiology can be found, the term “somatic complaint” is often replaced by terms such as “dissociative,” “functional,” “psychosomatic,” “somatoform,” or “medically unexplained,” depending on etiological presuppositions [14, 23]. Brief and self-limiting somatic complaints can be seen as normal phenomena (no pathological quality in itself), and can thus be settled through self-management or parent management (“normal life is not pain-free” [4]). Chronic and recurrent complaints, on the other hand, can cause considerable impairment of psychosocial functioning, and can lead to frequent healthcare utilization requiring intensive diagnostic and therapeutic efforts [14, 18, 31].
Compared with somatic complaints in adults or mental health problems in adolescents, the type, distribution, age, and sex dependencies have only been examined in few studies to date [14, 23]. To summarize, the following results have been obtained: Physical complaints occur just as often in adolescence as in adulthood, although estimated prevalences vary greatly between studies according to the type of complaints observed and the methods used [14, 20, 26]. Fatigue, headaches, backache, stomachache/bellyache, and nervousness/agitation constitute the most frequently occurring complaints [7, 17, 30, 31]. The frequency and heterogeneity of complaints increase with age, and girls display higher scores than boys [28, 30]. With regard to specific complaints, particular age and sex dependencies are evident [7, 20, 21, 34]. Different complaints do not appear in isolation from one another, but rather constitute specific clusters [13, 37]. Existing results of factor analyses and structural equation models differ significantly (in terms of both the number and meaning of the dimensions found) according to the item and/or questionnaire selection that constitutes the basis of the analysis [20, 33].
It is an established standard in psychosocial medicine and in child/adolescent clinical psychology to gather information from multiple perspectives. The child’s self-report is often complemented by a parent report, and sometimes the latter even replaces the former. The reason for this is the assumption that the ability to perceive and assess the different symptoms depends on age and developmental stage [14, 18]. In addition, there are gender-dependent tendencies for dramatization and trivialization. On the other hand, parent reports are influenced by the external observability of the complaints and the quality of the patient–child relationship [25]. Thus, existing studies show a low to medium correlation between the self and parent reports regarding somatic complaints [16, 32, 35]. An analysis of the predictive value of parent reports across a large number of different CSC with special consideration of the complaint’s external observability and the child’s gender is not yet available.
So far, the risks and predictive factors of somatic complaints have not been systematically investigated in empirical research. However, some studies on cross-sectional correlates do exist, e.g., low socio-economic status and poverty [9, 12, 17], everyday hassles such as familial conflicts, peer problems or problems at school [5, 28, 37], or parental physical and mental illness [11, 22]. More complex multiple-predictive models might involve the mother’s health, the child’s mental health, chronic illnesses, social contacts, and socioeconomic status [5, 6], or early negative emotionality, negative relationship experiences, and low perceived control [19]. However, it is as yet unclear to which extent different CSC dimensions are affected by socioeconomic background variables, physical health, or psychosocial distress.
In summary, the following research questions result from the current scientific status:
-
(1)
What is the prevalence of chronic somatic complaints (CSC) in adolescents?
-
(2)
How are the dimensions of CSC distributed?
-
(3)
What relationship exists between self-reports and parent reports with regard to CSC? Hypothesis 1: Parents systematically underestimate adolescents’ statements, particularly in cases of male adolescents or those in which the CSC are not visible.
-
(4)
How are CSC related to social class, health status, and psychosocial distress? Hypothesis 2: In addition to the different CSC predictors and sub-dimensions, psychosocial distress (e.g., stressful life events) shows the highest predictive value.
Methods
Design
The data presented here were obtained from the population-based, German-wide representative Hamburg Health Survey, in which information concerning not only somatic complaints, but also a wide range of other health-related characteristics, was collected. The methods used are described in more detail elsewhere [1, 3]. Questionnaire booklets for parents (mother and father combined) as well as for children and adolescents above the age of 10 years were employed as instruments. Both booklets comprised study-specific items (socio-demographics, life circumstances, health status, and health care utilization) and standardized psychometric questionnaires.
Instruments
Somatic complaints were assessed using a symptom checklist consisting of 59 items presented as keywords (see Table 1 for item examples). Subjects were asked to rate each individual complaint on a five-point response scale according to how often the symptoms generally appear (a 6-month prevalence timeframe was established for the present study). This checklist is well known within the German-speaking research community as the Giessen Physical Complaints Inventory for Children and Adolescents (GPCI; German: Giessener Beschwerdebogen GBB-KJ [8]). In contrast to similar questionnaires, such as the Children′s Somatization Inventory (CSI [36]), it comprises more items and is not restricted to somatoform symptoms. Seven items constitute each of the five scales (dimensions of complaints): “exhaustion,” “gastric problems,” “limb pain,” “cardiovascular problems,” and “common cold problems.” Summing the five scales provides a total problem score. Internal consistencies of the scales range from Cronbach’s α = 0.74 to 0.90. Content, criterion, and construct validity of the questionnaire have been proven [2]. The chronic or recurrent course was operationalized by dichotomizing the response scale (often or always, no-yes).
Sampling
The study population was comprised of 11- to 18-year-olds with a habitual residence in Germany. Sample size was determined by a compromise between a tolerable level of inaccuracy and costs of sampling [1]. Sample demographic data were compared with population data from the Federal Statistics Office in order to ensure its representativeness. Data collection was carried out by a professional institute for survey research (PSYDATA, Frankfurt). A three-step sampling procedure was chosen: (1) random selection of interviewers stratified according to federal state and size of community by PSYDATA, (2) selection of families with children according to sex and age quotas by interviewer, and (3) in families with more than one adolescent the subject was chosen at random (day and month of birth closest to the date of surveying). Participants signed an informed consent form. The rate of return for parent and adolescent questionnaires amounted to 70.8%, which led to a total sample size of N = 1,027.
Statistical analyses
In order to ensure the stability of the five established GPCI scales with the dichotomized data, a linear structural equation analysis was calculated beforehand (Unweighted Least Square Method [2]). The total fit of the 35 items (5 factor, 1 metafactor model for the existence/non-existence of chronic complaints) can be described as acceptable to good (RMSEA = 0.07, SRMR = 0.06, GFI = 0.92), and shows an adjustment comparable to that of the original five-step response scaling. Because of the high number of symptoms, only the most frequent are presented in tables; further results are reported in the text. The odds ratio was chosen to explore bivariate associations. The predictive validity of the parent reports was defined using sensitivity, specificity, and the positive and negative predictive values. The external observability of somatic complaints by parents was defined by means of an expert rating. Seven independent experts in the fields of child and adolescent psychiatry and psychology were asked to estimate the observability of the 59 complaints without direct oral reports from the adolescents (Kappa = 0.78). As a result, n = 29 symptoms were judged as externally observable (e.g., skin impurities), and n = 30 complaints were assessed as non-observable (e.g., headaches). The hypothesis formulated thereto was tested by analyses of variance (see results). The relationship between chronic complaints and socio-economic status, health status, and psychosocial distress was determined through a multiple binomial logistic regression analysis. Statistical significance was calculated for the most important parameter estimations—two-sided, with a local α-error of 5%. Following the conventions of Cohen [10], at least small effects were expected in hypothesis 1 and 2. Data were processed using LISREL 8.5, SPSS 14.0, and Excel 2003.
Results
Prevalence of chronic somatic complaints
Table 1 shows the prevalences as well as the age and gender associations for the 19 most frequent chronic somatic complaints in 11- to 18-year-olds (p ≥ 5.0%). The self-reports show that skin impurities/pimples, cold hands, and fatigue occurred most frequently. Across all assessed CSC, significant age effects showed that 15- to 18-year-olds were at a higher risk than 11- to 14-year-olds. The highest values were scored for complaints indicating “exhaustion” or “tiredness.” For instance, 15- to 18-year-olds showed almost four times the likelihood of “excessive need for sleep” (Odds ratio (OR) = 3.84; p = 6.1%, cp. Table 1). A third of all CSC declined with age, but the effects were not statistically significant. In comparison to age effects, gender effects were considerably more pronounced; 32 of the 59 odds ratios were significant (vs. 10 with regard to age). All significant effects showed a higher risk for girls as opposed to boys. Regarding the ranking of prevalences, parent reports were consistent with self-reports (Table 1). However, parents’ absolute scores were consistently below absolute self-report scores. The age effects in the parent reports were distributed similarly to those of the self-reports, but were also lower (only six significant odds ratios). With regard to gender, parent reports showed higher risks in approximately one-third (12 of 32) of all the effects that were significant in the self-report.
Dimensions of chronic complaints and multiple symptoms
Table 2 shows the complaint dimensions for 11- to 18-year-olds, according to both self-reports and parent reports. Percentages indicate cases in which at least one complaint of the given dimension was classified as chronic. According to age and gender groups, between one- and two-thirds of all 11- to 18-year-olds showed at least one dimension of chronic complaints (31.8% for 11- to 14-year-old boys, 59.8% for 15- to 18-year-old girls, cp. Table 2). Common cold complaints were the most frequent, while cardiovascular complaints were the rarest. Girls presented higher prevalences of CSC than did boys. Some dimensions increased with age (e.g., exhaustion), some decreased (e.g., stomach problems), and others exhibited interdependencies of age and gender (e.g., limb pain). In the parent reports, age and gender effects were relatively similar to those exhibited in the self-report, but percentages of CSC were significantly lower (about half). According to the self-reports, multiple chronic complaint complexes, defined as chronic complaints in two or more different complaint dimensions, appeared in 21.3% [CI95% = 18.8; 23.8] of all adolescents. According to the parent reports, however, they were only present in 7.7% [CI95% = 6.1; 9.3] of adolescents. In the self-reports, the cases above the 90th percentile showed three or more different chronic complaint complexes, while the 90th percentile in the parent reports was reached with one or more complaint complexes.
Predictive validity of parent reports
Table 3 shows the different statistics that describe the relationship between the parent- and self-reports on chronic physical complaints in adolescents. The sensitivity of parent reports has a median of 0.21 for the 59 complaints observed (Min = 0.00, Max = 0.53). The specificity oscillates between Spec = 0.94 and 1.00 (Med = 0.98). The prevalence-dependent positive and negative predictive values are of PPV = 0.50 and NPV = 0.97 in the median. The proportion of altogether consistently classified cases averaged out at Acc = 92.6%. The same analyses were performed with the five chronic complaint dimensions (stratified according to age and gender), but no differences were found (not represented). Finally, tests were conducted to determine whether parents yielded particularly low assessments for boys in externally observable CSC, by means of a 2 × 2 × 2 ×-factorial variance analysis with repeated measurement on one factor (observable y/n, male/female, parent report/self-report). Results show that parents indicate (1) significantly lower prevalences for CSC than the children and adolescents themselves (F = 145.66, df = 1, p = 0.000, η2 = 0.56); (2) observable CSC significantly more frequently than non-observable (F = 6.104, df = 1, p = 0.015, η2 = 0.05); and (3) significantly lower prevalences for boys than for girls (F = 26.88, df = 1, p = 0.000, η2 = 0.19). No interdependence was found for observability and gender (F = 0.57, df = 1, p = 0.452, η2 = 0.01).
Associations with socioeconomic status, health status, and psychosocial distress
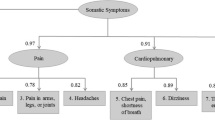
Figure 1 shows the age- and gender-adjusted risks for the five dimensions of CSC in the areas of socioeconomic status, health status, and psychosocial distress. Single predictors (nationality, socioeconomic status, somatic illness, mental illness, treatment status, medication, problems in school, and stressful life events) were assessed via parent reports of standardized items. The chosen prevalence period was 6 months. The scale “socio-economic status” (SES, Cronbach’s α = 0.76) was constructed through the unweighted addition of the education, occupation, and income variables. The represented OR was calculated using multiple binomial logistic regression, which included all ten predictors listed. In the cases of limb pain and cardiovascular problems, no cases with mental illnesses were present; therefore, this predictor had to be omitted in these two regression analyses.
Results of the multiple binomial logistic regression analyses per dimension of CSC (for model fit see lower left part) including ten predictors from the areas of socio-economic status, health status, and psychosocial distress; *Statistical significant effects; N = 1,027; e.g. exhaustion is significantly predicted by age, sex, and school problems
Highly significant predictive models were found for all five complaint dimensions (cf. Fig. 1). The explained variance ranged from 7 (for the prediction of chronic limb pain) to 17% (for the prediction of chronic gastric problems). The different predictors show different predictive values for the different complaint dimensions. However, some effects were not significant due to inappropriate cell frequencies. Across all five complaint complexes, mental illness, gender, and stressful life events showed the highest OR (Med = 3.48, 2.34 and 2.10), while SES and treatment status showed the lowest OR (Med = 1.05 und 1.22). The highest significant individual effects were shown by “somatic illness” and “gender” for gastric problems (OR = 5.55 and 4.67, respectively), as well as by “treatment status” in limb pain (OR = 0.20). Age had a significant effect on exhaustion in particular, while gender significantly influenced all dimensions.
Discussion
The data presented here are the very first to provide information concerning the distribution of CSC in adolescents in Germany. Because almost 60 different symptoms were evaluated, the probability of false-negative data was considerably decreased. As a result, it became clear that not headaches and stomachaches, but rather skin impurities, pimples, and cold hands were the most frequent complaints in the observed age groups. Besides this, the prevalences and their age and gender associations in the self-reports of German children and adolescents were in accordance with those of other countries [7, 17, 28, 31]. Results show an age-related increasing risk of CSC; the greatest effects were an over three times increased chance of “excessive need for sleep” and “fatigue” in 14- to 17-year-old adolescents. Higher scores for girls and lower scores for boys correspond to typical expectations for this stage of development in terms of biological and social changes experienced in puberty [30].
In general, the analyses of the complaint dimensions confirmed the age and gender dependency observed in the individual complaints, but differential effects were also noticeable (e.g., exhaustion increases with age, decrease in stomach complaints, limb pain shows an interactional association). Because of the partially large overlap of individual symptoms (e.g., abdominal pain and bellyache), multiple complaints were assessed more reliably and validly on the level of grouped complaint dimensions. This revealed that a fifth of all adolescents presented two or more chronic complaint dimensions. The particular clinical relevance of this result is that multiple complaints constitute a core criterion for somatization disorders [15]. Existing studies [17, 27] found comparably high prevalences of multiple complaints.
For the first time, the predictive validity of parent reports was analyzed for a multitude of different chronic physical complaints. The mean sensitivity indicates that only one-fifth of existing CSC was reported by parents, while the specificity was very high. Clinically, this means that parent reports were particularly valid when no CSC was reported. Therefore, it is to be principally regarded with care when CSCs are reported. The prevalence-dependent predictive values confirm this association; only every second CSC reported by a parent was an actual CSC. The coefficients of inter-rater agreement reported in other studies support these results [16, 32, 35]. This relationship and its direction are of high clinical relevance: Parent reports should be primarily sensitive and less specific, as they can trigger the assessment of the self-report by a clinical expert [14, 24]. The initially formulated hypothesis could be proven after all: Parents systematically underestimated adolescents’ reports of CSC, particularly when they were not visible and/or in boys. The non-significant interaction term shows that latent CSC in boys was not underestimated by their parents beyond the simple additive effect.
The explained variance of 7–17% yielded for the different CSC dimensions through socioeconomic background, physical health, or psychosocial distress was substantial, but not high. The highest prediction was reached for stomach problems, which corresponds with the classic role of this dimension as a major psychosomatic symptom area [15]. Published studies on predictive models reach comparable effect sizes [6]. Differences in the weights of the single predictors between the different complaint dimensions refer to their differential effectiveness. The predictor of “treatment status,” for instance, showed a risk-decreasing factor for limb pain and cardiovascular problems, while other dimensions did not show any correlation. According to the tested hypothesis, it is evident that psychosocial distress, such as mental illness and stressful life events, caused the greatest effects. This result is in accordance with other studies regarding correlates and predictors of physical symptoms [14, 23].
The internal and external validity of the results are particularly limited by three factors. First, the cross-sectional design did not allow any temporal or causal interpretations of relationship beyond simple statements of statistical association. This design was particularly susceptible to bias and confounds. Secondly, the exclusive assessment of CSC carried the danger of false positive results. Due to the subjective nature of somatic complaints, an objective validation could not be obtained. Although a question concerning the existence of a current physical or mental illness was included, this information could not be confirmed by experts. Thirdly, the analysis is based on complaints that were voiced repeatedly or continuously during the last 6 months. An alternative case definition would have been to focus solely on continuous symptoms. This approach led to a reduction of maximum symptom prevalences to 0.3% for skin impurities/pimples, 0.2% for cold hands, and 0.1% for fatigue. The prevalence of the five complaint dimensions were then as follows: 1.0% for exhaustion, 0.5% for stomach complaints, 0.3% for aching limbs, 0.1% for circulatory problems and 2.5% for problems relating to a cold. Age and gender related effects, the correspondence of self- and parental assessment, as well as the predictive validity of the parent report were similar to the results presented here. The effect profiles for psycho-social risk factors could not be interpreted due to inadequate cell frequencies.
Conclusion
Summarizing, the following conclusions can be drawn: The systematic, comprehensive and standardized surveying of a wide range of somatic complaints prevents exclusive reporting of selected complaints and thus evades possible false negative anamnestic data. Individual CSC occur frequently in adolescents and represent (statistically speaking) a relatively normal phenomenon. In contrast, two or more CSC from different complexes are clinically relevant and therefore warrant particular attention. Since parents systematically underestimate their children’s CSC, the self-report should be collected simultaneously whenever possible. Across all different predictors and CSC dimensions, psychosocial distress exhibits the highest predictive value. Future research efforts should focus on the assessment of CSC profiles in specific patient populations, as well as on correlations with other constructs (using longitudinal approaches).
References
Barkmann C, Schulte-Markwort M (2005) Emotional and behavioral problems of children and adolescents in germany—an epidemiological screening. Soc Psychiatry Psychiatr Epidemiol 40:357–366
Barkmann C, Mack B, Braehler E, Schulte-Markwort M (2008) The “Gießener Beschwerdebogen für Kinder und Jugendliche” (GBB-KJ): factorial validity, reliability, and standardization of the self- and parent report form for 4- to 18-year-olds. Diagnostica 54:99–111
Barkmann C, Schulte-Markwort M, Braehler E (2007) Physical complaints of children and adolescents in germany—results of a population-based survey. Z Klin Psychol Psychiatr Psychother 55:49–58
Barsky AJ, Borus JF (1999) Functional somatic syndromes. Ann Intern Med 130:910–921
Bernstein GA, Massie ED, Thuras PD, Perwien AR, Borchadt CM, Crosby RD (1997) Somatic symptoms in anxious-depressed school refusers. J Am Acad Child Adolesc Psychiatry 36:661–668
Berntsson LT, Gustafsson JE (2000) Determinants of psychosomatic complaints in Swedish schoolchildren aged seven to twelve years. Scand J Public Health 28:283–293
Berntsson LT, Kohler L, Gustafsson JE (2001) Psychosomatic complaints in schoolchildren: a Nordic comparison. Scand J Public Health 29:44–54
Braehler E (1992) The Giessen Physical Complaints Inventory for Children and Adolescents (GPCI). Manual, Huber, Bern
Campo JV, Comer DM, Jansen-McWilliams L, Gardner W, Kelleher KJ (2002) Recurrent pain, emotional distress, and health service use on childhood. J Pediatr 141:576–583
Cohen J (1988) Statistical power analysis for the behavioral sciences. Lawrence Erlbaum Associates, Hillsdale
Craig TKJ, Cox AD, Klein K (2002) Intergenerational transmission of somatization behaviour: a study of chronic somatizers and their children. Psychol Med 32:805–816
Dhossche D, Ferdinand R, van der Ende J, Verhulst F (2001) Outcome of self-reported functional-somatic symptoms in a community sample of adolescents. Ann Clin Psychiatry 13:191–199
Egger HL, Costello EJ, Erkanli A, Angold A (1999) Somatic complaints and psychopathology in children and adolescents: stomach aches, musculoskeletal pains, and headaches. J Am Acad Child Adolesc Psychiatry 38:852–860
Eminson M (2007) Mecically unexplained symptoms in children and adolescents. Clin Psychol Rev 27:855–871
Fritz GK, Fritsch S, Hagino O (1997) Somatoform disorders in children and adolescents: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry 36:1329–1338
Garber J, van Slyke DA, Walker LS (1998) Concordance between mothers’ and children’s reports of somatic and emotional symptoms in patients with recurrent abdominal pain or emotional disorders. J Abnorm Child Psychol 26:381–391
Garber J, Walker LS, Zeman J (1991) Somatization symptoms in a community sample of children and adolescents: further validation of the children’s somatization inventory. Psychol Assess 3:588–595
Gledhill J, Garralda ME (2006) Functional symptoms and somatoform disorders in children and adolescents: the role of standardised measures in assessment. Child Adolesc Ment Health 11:208–214
Hagekull B, Bohlin G (2004) Predictors of middle childhood psychosomatic problems: an emotion regulation approach. Infant Child Dev 13:389–405
Haugland S, Wold B (2001) Subjective health complaints in adolescence—reliability and validity of survey methods. J Adolesc 24:611–624
Hessel A, Geyer M, Schumacher J, Braehler E (2003) Somatoforme Beschwerden bei Jugendlichen in Deutschland. Psychotherapeut 48:109–116
Hotopf M (2002) Childhood experience of illness as a risk factor for medically unexplained symptoms. Scand J Psychol 43:139–146
Husain K, Browne T, Chalder T (2007) A review of psychological models and interventions for medically unexplained somatic symptoms in children. Child Adolesc Ment Health 12:2–7
Janicke DM, Finney JW, Riley A (2001) Children’s health care use: a prospective investigation of factors related to care-seeking. Med Care 39:990–1001
Laurell K, Larsson B, Eeg-Olofsson O (2005) Headache in schoolchildren: association with other pain, family history and psychosocial factors. Pain 119:150–158
Lieb R, Mastaler M, Wittchen HU (1998) Are there somatoform disorders in adolescents and young adults? First epidemiological findings based on a representative population sample. Verhaltenstherapie 8:81–93
Livingston R, Martin-Cannici C (1985) Multiple somatic complaints and possible somatization disorder in prepubertal children. J Am Acad Child Adolesc Psychiatry 24:603–607
Murberg TA, Bru E (2004) School-related stress and psychomatic symptoms among Norwegian adolescents. Sch Psychol Int 25:317–332
Pennebaker JW (1982) The psychology of physical symptoms. Springer, Berlin
Rhee H (2005) Relationships between physical symptoms and pubertal development. J Pediatr Health Care 19:95–103
Roth-Isigkeit A, Thyen U, Stoeven H, Schwarzenberger J, Schmucker P (2005) Pain among children and adolescents: restrictions in daily living and triggering factors angela. Pediatrics 115:e152–e162
Sundblad GM, Saartok T, Engstroem LM (2006) Child–parent agreement on reports of disease, injury and pain. BMC Public Health 6:276. doi:10.1186/1471-2458-6-276.PMCID:PMC1654155
Takata Y, Sakata Y (2004) Development of a psychosomatic complaints scale for adolescents. Psychiatry Clin Neurosci 58:3–7
Tanaka H, Tamai H, Terashima S, Takenaka Y, Tanaka T (2000) Psychosocial factors affecting psychosomatic symptoms in Japanese schoolchildren. Pediatr Int 42:354–358
Taylor DC, Satzmari P, Boyle MH, Offord DR (1996) Somatization and the vocabulary of everyday bodily experiences and concerns: a community study of adolescents. J Am Acad Child Adolesc Psychiatry 35:491–499
Walker LS, Garber J, Greene JW (1991) Somatization symptoms in pediatric abdominal pain patients: relation to chronicity of abdominal pain and parent somatization. J Abnorm Child Psychol 19:379–394
Walker LS, Garber J, Smith CA, van Slyke DA, Claar R (2001) The relation of daily stressors to somatic and emotional symptoms in children with and without recurrent abdominal pain. J Consult Clin Psychol 69:85–91
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Barkmann, C., Braehler, E., Schulte-Markwort, M. et al. Chronic somatic complaints in adolescents: prevalence, predictive validity of the parent reports, and associations with social class, health status, and psychosocial distress. Soc Psychiatry Psychiatr Epidemiol 46, 1003–1011 (2011). https://doi.org/10.1007/s00127-010-0273-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-010-0273-4