Abstract
Aim
This study aimed to analyse depression-related factors. The prevalence of depression has been shown in prior surveys to vary between East and West Germany. Do these differences also appear in health insurance data?
Method
The outpatient data of a large German statutory health insurance company were analysed for regional differences in (a) the prevalence of depression diagnosis, (b) prescription rates of antidepressants and (c) risk factors of being diagnosed with depression or prescribed antidepressants. Diagnosis rates of depression in outpatient care (ICD-10 diagnosis F32/33) were analysed for the first quarter of 2004, and prescription rates of antidepressants were analysed for the first half of 2004. Odds ratios were calculated for the likelihood of being diagnosed with depression and of being prescribed antidepressants whilst considering socio-demographic and regional variables.
Results
The prevalence of depression diagnosis is up to 41% lower in East Germany than the expected mean rate and 30% above the expected mean rate in Berlin. Regional distribution rates of antidepressant prescriptions largely follow the same pattern as rates for depression diagnosis, with the exception of Berlin where prescription rates are 10% below the expected mean rate. Unemployed persons in West Germany have a higher chance of being diagnosed with depression and of being prescribed antidepressants than those unemployed in East Germany.
Discussion
Results correspond greatly to findings of epidemiologic surveys. However, the lower rate of depression diagnosis and prescription rates in East Germany might also be due to fewer mental health professionals practising there and possible differences in reporting style of emotional symptoms. This might contribute to the differences in diagnosis and prescription prevalence but cannot be solely responsible for this phenomenon. Probable causes of the different depression prevalence rates in East and West Germany will be discussed in this analysis. More research into factors impacting on regional differences in the prevalence of depression is needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The German National Health Survey in 1998/99 and its precursor study in 1994 found significantly lower rates of unipolar depression in East Germany compared to West Germany [1]. These results were astonishing since living conditions are considered harsher in the east than in the west. Income and employment rates, which are known risk factors for depressive disorder [2, 3], are much lower in East Germany. In 2004, the unemployment rate in East Germany amounted to 20%, while it was only 9% in West Germany [4].
In the study presented here, we will evaluate the epidemiology of depression in Germany again; however, this time by using health insurance data. Using secondary data for measuring prevalence has the advantage over surveys in that health insurance data contains many more cases. This also allows for the analysis of differences in prevalence among smaller regions. The research presented here aims to answer the following questions:
-
Are differences in the prevalence of depressive disorder between East and West Germany also present in health insurance data?
-
Does the prevalence of depression diagnoses made in outpatient care and the prescription of antidepressants (both used as proxy for depression) in health insurance data vary among regions in Germany?
-
Are differences in the prevalence of depression diagnoses made in outpatient care and the prescription of antidepressants obtained from health insurance data related to service availability?
Method
We analysed the data of a major statutory health insurance company, the Gmünder ErsatzKasse (GEK). All over Germany, approximately 1.4 million people were insured with the GEK in 2004. This is 1.7% of the German population. The clientele of the GEK consists of a relatively high number of men of a working age. Therefore, the population represented with the GEK cannot be considered per se representative of the German population. However, prior studies have found that results from analyses of GEK data can be transferred without major distortions to the German population as a whole, if they are age and gender adjusted. For example, an analysis of GEK-data on hospital-made diagnoses corresponded well with the official data provided on diagnosis at the time of hospital discharge by the federal statistic bureau that covered the whole country [5]. Moreover, results of prior GEK-data analysis on depression diagnosis were highly consistent with survey results [6].
For the main part of our study, we included all persons insured on 1 January 2004 with a documented insurance period of at least 182 days within that year. Population-based figures were directly standardised by using the sex and age distribution of the German population as of December 2003 (Statistisches Jahrbuch 2005). To compare regional levels of depression and prescription rates of antidepressants, we estimated indirect standardised rates as follows: We first calculated nationwide gender and age-specific rates of depression diagnosis and antidepressant prescriptions. Then we used these nationwide rates to calculate expected regional rates by considering real age and gender distribution in the respective regions. We compared these expected regional rates with the true rates that were observed regionally. The results as presented in Figs. 1 and 2 show the relative deviations between observed and expected values.
Rates of depression diagnosis variations from the expected mean rate, first quarter 2004, without Schleswig-Holstein, n = 1,223, 557. The darker the grey on the map, the higher is the rate of depression diagnosis in the respective land. From north to south and west to east: SH Schleswig-Holstein, MVP Mecklenburg-Pomerania, HB Bremen (city state), HH Hamburg (city state), NDS Lower Saxony, SAN Saxony-Anhalt, BER Berlin (city state), BRA Brandenburg, NRW North Rhine-Westphalia, HES Hesse, TUE Thuringia, SAC Saxony, SAA Saarland, RPF Rhineland-Palatinate, BW Baden Wurttemberg, BAY Bavaria
Variations in rates of antidepressant prescriptions from the expected mean rate, first quarter 2004, n = 1,299,154. The darker the grey on the map, the higher is the rate of antidepressant prescription in the respective land. From north to south and west to east: SH Schleswig-Holstein, MVP Mecklenburg-Pomerania, HB Bremen (city state), HH Hamburg (city state), NDS Lower Saxony, SAN Saxony-Anhalt, BER Berlin (city state), BRA Brandenburg, NRW North Rhine-Westphalia, HES Hesse, TUE Thuringia, SAC Saxony, SAA Saarland, RPF Rhineland-Palatinate, BW Baden Wurttemberg, BAY Bavaria
As proxies for depressive disorder in the population, we used (1) diagnoses of depression made in outpatient care and (2) prescription rates of antidepressants in outpatient care:
-
1.
Diagnoses made in outpatient care have been available in statutory health insurance data in Germany since 2004. In our analysis of depression, we focused on the ICD-10 codes for depressive episode (F32) and recurrent depressive episode (F33), which were documented at the patient level within the first quarter of 2004. Diagnosis of dysthymia is rarely given in outpatient care and, thus, excluded from this analysis. All data are available on an individual basis. Thus, even if an insured person is diagnosed with depression multiple times by multiple providers, he is counted only once as suffering from depression.
-
2.
Prescription rates of antidepressants were analysed within the first half of 2004. Data on pharmacological prescriptions is only available for medication paid for by the health insurance company. Herbal medication for adults, such as St. John’s Wort, has to be paid mostly out of the patient’s own pocket and, thus, only incomplete information about its use is available in the health insurance data. Therefore, such medication generally was excluded from this analysis.
For a subgroup of the population with more detailed information being available (persons of a working age, 15–64 years old, who were either employed or unemployed) we confirmed and further studied regional influences on depression in logistic regression models. All calculations were performed using SAS-Software Version 9.1.
Results
Within the first quarter of 2004, 70% of all those insured visited outpatient medical care at least once. More than 15% received the diagnosis of having a mental disorder and 5% of having a depressive episode (ICD-10 F32 and 33).
Diagnosis of depression in the German Länder (the German states)
We analysed the rate of diagnosis of depression for each of the 16 German Länder. To minimise the influence of different age and gender structures in the Länder, indirect standardised rates were calculated. Figure 1 presents deviations in the observed rates and the expected rates of depression diagnosis in 15 of the 16 Länder. Data for Schleswig-Holstein was not available. The lowest depression diagnosis rates were found in East Germany, ranging between 24 (Saxony) and 41% (Saxony-Anhalt) below the expected mean rate. The highest diagnosis rate is found in the city state of Berlin where diagnosis rates are 30% higher than expected. Diagnosis rates that are higher than expected are also found in most West German Länder. Rates range between 5 (Rhineland-Palatinate) and 16% (Saarland) above the expected mean rate.
Prescription rates of antidepressants for depression in the German Länder
A similar pattern is found in the prescription of antidepressants. As Fig. 2 shows, lower than expected prescription rates of antidepressants are observed in East Germany, which correspond to the low diagnosis rates there. High rates are found again in Saarland, but also in Rhineland–Palatinate and North Rhine–Westphalia. Interestingly, in Berlin, where the highest diagnosis rates were found, prescription rates are 10% below the expected rate.
Risk of being diagnosed with depression and of being prescribed antidepressants
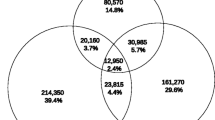
To calculate the risk of being diagnosed with depression and of being prescribed antidepressants, we built three logistic regression models (see Table 1). We used all insured persons who were available to the labour market at the beginning of 2004, meaning they were either employed or receiving unemployment benefits. This related to 606,056 persons; 3.4% (20,589) of them were diagnosed with depression at least once in the first quarter of 2004. 2.6% of them were prescribed antidepressants at least once in the first 6 months of 2004. Also included in the model were factors relating to the risk of depression, such as age (in 5-year clustersFootnote 1), gender, employment and marital status (see footnote 1), as well as place of residence within one of the three regions, i.e. Berlin, and West and East Germany. All variables were dummy coded, with one value range being selected as a reference. Odds ratios were calculated showing deviations in selected reference groups.
In model 1, the odds ratio of being diagnosed with depression was 0.57 (CI 0.55–0.60) in East Germany compared to West Germany (reference), thus showing a highly significant lower depression diagnosis rate in East Germany after controlling for other factors (see Table 1). The odds ratio of being diagnosed with depression was only slightly, yet significantly, higher in Berlin than in West Germany (1.08, CI 1.02–1.14). In addition, the odds ratio of being diagnosed with depression was significantly higher for unemployed compared to blue collar workers (1.97, CI 1.89–2.05).
Since the descriptive analysis revealed lower rates of depression diagnosis than expected in East Germany, despite known high rates of unemployment, we assumed that the effects of unemployment on depression rates might differ among regions. In model 2, we therefore introduced an additional parameter of “being unemployed in …” allowing regional effect modification to be shown. It turned out that unemployment had significantly less influence on depression diagnosis rates in both Berlin and East Germany compared to West Germany. The odds ratio for unemployed versus employed in West Germany of being diagnosed with depression was 2.21 (CI 2.11–2.31). In East Germany, it was 1.5 (=2.21 × 0.68) and in Berlin it was 1.5 (=2.21 × 0.70).Footnote 2
Model 3 is similar to model 2, but instead calculates the odds ratios of being prescribed antidepressants. The results, as shown in Table 1, vastly replicate those of models 1 and 2, calculating odds ratios for the diagnosis of depression. However, there is one exception. While the odds ratios of being diagnosed with depression were higher in Berlin, the odds ratio of being prescribed antidepressants was lower in Berlin (0.80, CI 0.74–0.88). Further, in accordance with model 2, unemployment had less influence on antidepressant prescription rates in East Germany and in Berlin. The odds ratio of being prescribed antidepressants in West Germany with respect to unemployed versus employed was 2.1 (CI 2.00–2.21), while in East Germany it was 1.5 (=2.10 × 0.86) and in Berlin it was 1.8 (=2.10 × 0.72) (see footnote 2).
Discussion
The strength of this analysis of health insurance data is that it, for the first time, presents differences in depression epidemiology on a regional, and not just a country basis. This is possible because health insurance data carry a much higher number of cases than epidemiologic surveys could ever handle. In Germany, 98% of the population has health insurance (88% through statutory health insurance) [7] which covers treatment for all ICD-10 diagnosis. As much as 90% of the population visit outpatient medical care at least once a year. Under these conditions, health insurance data can provide information about the whole of society without excluding any sub-groups, such as the institutionalised, as is the case in surveys.
The weaknesses of this analysis relate to the nature of secondary data: firstly, diagnoses recorded in health insurance data are made clinically and are not standardised, and are, thus, less reliable than those made in epidemiologic surveys. Secondly, prescription rates of antidepressants used as a proxy for the prevalence of depression are also limited in their reliability. The under-treatment of depression is a well known and often replicated fact [8, 9]. In addition, antidepressants are not only prescribed for depression, but also for other disorders, such as anxiety, pain or sleep disorder.
Despite all these limitations, it is astonishing how precisely rates of depression diagnoses and antidepressant prescriptions replicate findings from the German National Health Survey with respect to gender, age, work status and regional similarities of depression prevalence [2]. This finding is consistent with prior descriptive analysis of health insurance data for the diagnosis of depression [6, 10].
It is remarkable that antidepressant prescription rates more or less follow the same pattern as depression diagnosis rates. There is, however, the noteworthy exception of Berlin where treatment rates are 10% lower than expected, while diagnosis rates are the highest of all. In North Rhine-Westphalia and Rhineland-Palatinate, treatment rates are higher than expected while diagnosis rates are more or less at the expected level. A prior analysis of this data revealed that prescription rates of antidepressants are lower in densely populated areas and relatively higher in rural areas. In contrast to this, psychotherapists are consulted more often in densely populated areas and less in rural areas [10]. Given this, it could be that the low rates of the prescription of antidepressants in Berlin are subsidised by higher rates of psychotherapeutic treatment as the high number of psychotherapists in Berlin (one serving a population of 2,000) might imply. However, why then do the other city states of Hamburg and Bremen not show similar patterns despite having similar numbers of psychotherapists available as Berlin? Why does North Rhine-Westphalia, with the densely populated Ruhr area, have prescription rates above the expected level? More research into factors influencing the prescription of therapy for depression and the overall adequacy thereof, which could not be considered in this analysis, is needed.
Differences in depression diagnosis and antidepressant prescription rates found between East and West Germany replicate differences in depression prevalence found in the National Health Survey and its pre-study 5 and 10 years prior to our analysis [11, 12]. Odds ratios are remarkably similar. The National Health Survey in 1998/1999 (population aged 18–65) found an odds ratio for major depression between West and East (reference) of 1.52 (CI 1.20–1.93) [1]. Taking a reciprocal look at this odds ratio, the risk of suffering from depression amounts to 0.66 (0.52–0.83) in East Germany. Similarly, the health insurance data revealed an odds ratio between East and West (reference) (population aged 15–65) of being diagnosed with depression of 0.57 (CI 0.55–0.60) and an odds ratio of being prescribed antidepressants of 0.69 (CI 0.66–0.73).
Three factors probably have influenced depression diagnosis rates in the health insurance data:
-
the capability of outpatient health-care services to diagnose depression,
-
the reporting style of emotional symptoms,
-
the “true” prevalence of depression in the population.
Health-care services While survey data are independent of health-care provision, health insurance data depend on it. There is no information available on regional variations in a physician’s capability of “correctly” diagnosing depression. The lower rates of depression diagnosis in East Germany might also be related to a poorer mental health-care infrastructure there. While the number of primary care physicians does not vary considerably among regions (one serving a population of about 2,000), psychiatrists are rarer in East Germany than inWest Germany and the city states (one per 22,000, 17,000, 7,000 population). Compared to East Germany, there are twice as many psychotherapists in West Germany and six times as many in the city states (one per 2,000, 5,000, 13,000 population) [13]. These differences might in fact impact on the rates of depression diagnosis. However, the degree of the impact is not known. By looking at the city states of Bremen and Hamburg, this does not mean, however, that a high density of psychiatrists and psychotherapists inevitably leads to high rates of depression diagnosis and antidepressant prescription, as one might have thought when considering the high prevalence rates and high numbers of mental health specialists in Berlin.
Reporting style Presentation of symptoms of depression varies between cultures [14]. Also, help-seeking behaviour for mental disorders differs between cultures [15]. Although there is no research known that systematically evaluates reporting style and help-seeking behaviour in East and West Germany, there is some evidence to show that concepts of mental disorders differ between East and West Germany [16]. While this might impact on service use [17], it should not impact on the prevalence of depression measured by standardised instruments such as the German National Health Survey.
Epidemiology By taking survey results into account, a “true” difference in depression prevalence has to be considered between East and West Germany. Interestingly, this difference in prevalence does not comply with suicide rates in East and West Germany. Whilst suicide rates were much higher in East Germany at the time of reunification, today the suicide rates are almost equal. In 2004, there were 13.2/100,000 suicides reported in East Germany and 12.8/100,000 in West Germany.
Below, we will discuss further factors that might have contributed to the difference in depression prevalence between East and West:
-
1.
Unemployment In general, unemployment increases the risk of depression [2]. In East Germany, unemployment rates are double those of West Germany, but depression prevalence and diagnosis rates are lower. Moreover, those unemployed in East Germany suffer a lower risk of being depressed. This lower risk might be explained by selection hypothesis [18]. Unemployment hits the vulnerable and sick first. In a situation of long-lasting mass unemployment, as is the case in many regions of East Germany, the healthier and more resilient also lose their jobs. Thus, the prevalence of pathology decreases among the unemployed. In addition, with increasing unemployment rates, the stigma of being unemployed decreases and is, thus, less of a burden for those affected by it [19]. Whilst this explains the lower risk of depression among the unemployed in East Germany, it does not explain the difference in prevalence between East and West German populations.
-
2.
Migration Since reunification, considerable migration has occurred, predominately from East Germany to the economically stronger West Germany. During the years 1999–2004, about 10% of the East German population (calculated for the 2004 population) migrated to West Germany, while at the same time the East German population grew by about 6% through migration from West Germany (having three times the population of East Germany) [20]. The majority of migrants in both directions were below 30 years of age. Following the “healthy migrant” hypothesis, which states a selection bias for the movement of healthier individuals, in particular for younger individuals [21], the inner German migrants have to be considered as being healthier than the average population. Therefore, this migration cannot be expected to have caused lower depression rates in East Germany.
-
3.
Sociological phenomena It is also likely that sociological phenomena contribute to the difference in depression diagnosis prevalence and probably depressive disorder in East and West Germany:
-
(a)
East and West Germans seem to have different strategies for coping when confronted with insecurities regarding their future or their jobs. Whilst West Germans focus on achieving job security and, therefore, sacrifice family life, East Germans invest equally in both family and career [22]. This might impact on resilience and vulnerability.
-
(b)
When considering the theories of the French sociologist, Alain Ehrenberg, on the development of the meaning of depression for modern society, the rising public perception of depression should be understood as an expression of societal change. This change relates to a society that has moved from being one that was based on regulation, discipline and obedience to a modern society in which the main values relate to autonomy and independence, and is highly appreciative of initiative and self- realisation [23]. Ehrenberg interprets depressive symptomatology, including lack of initiative and motivation, as well as impaired communication, as the exact blueprint of the values that dominate modern society today.
The society of the former German Democratic Republic (East Germany) functioned more like the old societal model. It was shaped in a collectivistic way; traditional values were maintained, such as obedience, discipline, adaptation, submission to societal expectations and a sense of responsibility and helpfulness [24]. The societal model of the Federal Republic of Germany (West Germany) was, however, dominated by individualistic and liberal attitudes, which put the focus on the self-determined individual. Values relating to self-fulfilment, such as post-materialism and autonomy, dominated over values concerning a person’s sense of duty, such as obedience and discipline [25]. According to Ehrenberg, depression is understood to be the inability to live up to the expectations of modern individualistic society. It is, thus, considered by Ehrenberg to be the disorder of modern Western society [23].
Since reunification, East Germany is adapting more and more to the West German societal model. It will be interesting to see whether depression prevalence rates in the two parts of Germany come closer once the generation brought up in East Germany after reunification reaches middle age.
Conclusion
In a health-care system where 90% of the population is insured and low threshold access to health care is available to the vast majority of the population, health insurance data reproduce the prevalence of endemic disorder, such as depression, in a reliable manner. Prevalence of depression diagnosis differs between East and West Germany. This is probably due to differences between these regions in the epidemiology of depressive disorder and, to a lesser extent, due to the scarcity of mental health professionals in East Germany. It cannot be ruled out that difference in styles of reporting emotional symptoms also contributes to this phenomenon. The causes of the differences in depression prevalence include sociological factors such as societal values, which should be taken into consideration. Investigating more thoroughly the causes for the differences in depression prevalence might provide highly valuable information on mental health promotion and prevention.
Also, prescription rates of antidepressants vary among regions. They mostly follow the diagnosis rates (e.g. more antidepressants are prescribed in regions with high diagnosis rates) but sometimes are higher or lower. More research into factors impacting regionally on prevalence rates and outpatient health-service provision is needed when aiming to improve the treatment of depression.
Notes
Not shown in Table 1.
Please see Table 1: The modified odds ratio for effect modification is the product of the odds ratio for being unemployed and for being diagnosed with depression in a specific region.
References
Jacobi F, Hoyer J, Wittchen H-U (2004) Seelische Gesundheit in Ost und West: Analysen auf der Grundlage des Bundesgesundheitssurveys. Z Klin Psychol Psychotherapie 33:251–260
Fryers T, Melzer D, Jenkins R, Brugha T (2005) The distribution of common mental disorders: social inequalities in Europe. Clin Pract Epidemol Ment Health 1:14
Liwowsky I, Kramer D, Mergl R, Bramesfeld A, Allgaier APE, Hegerl U (2008) Screening for depression in the older long-term unemployed. Soc Psychiatry Psychiatr Epidemiol (in press)
Bundesagentur für Arbeit. Arbeitslose und Arbeitslosenquoten nach Ländern. Jahresdurchschnitte 2003 und 2004. www.bagbbw.de. 2007
Grobe T, Dörning H, Schwartz F (2004) GEK-Gesundheitsreport 2004. Schwerpunktthema: Gesundheitsstörungen durch Alkohol. Asgard-Verlag, St. Augustin
Bramesfeld A, Grobe T, Schwartz F (2007) Who is diagnosed as suffering from depression in the German statutory health-care system? An analysis of health insurance data. Euro J Epidemiol 22:397–403
Busse R, Riesberg A (2004) Health-care systems in transition: Germany. WHO Regional Office for Europe on Behalf of the European Observatory on Health Systems and Policies, Copenhagen
Alonso J, Angermeyer M, Bernert S, Bruffaerts R, Brugha T, Bryson H, de Giralamo G, de Graaf R, Demyttenaere K, Gasquet I, Haro J, Katz S, Kessler R, Kovess V, Lepine J, Ormel J, Polidori G, Rousso J, Vilagut G (2004) Psychotropic drug utilization in Europe: results from the European Study of the Epistemology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand 109 (Suppl 420):55–64
Jacobi F, Wittchen H, Holting C, Hofler M, Pfister H, Muller N, Lieb R (2004) Prevalence, co-morbidity and correlates of mental disorders in the general population: results from the German Health Interview and Examination Survey (GHS). Psychol Med 34:597–611
Bramesfeld A, Grobe T, Schwartz F (2007) Who is treated, and how, for depression? An analysis of statutory health insurance data in Germany. Soc Psychiatry Psychiatr Epidemiol 42:740–746
Wittchen H-U, Müller N, Pfisterer H, Winter S, Schmidtkurz B (1999) Affektive, somatoforme und Angsstörungen in Deutschland - Erste Ergebnisse des bundesweiten Zusatzsurveys “Psychische Störungen”. Gesundheitswesen 61(Suppl 2):216–222
Wittchen H-U (1994) Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res 28:57–84
Kassenäztliche Bundesvereinigung. Grunddaten der Kassenärztlichen Versorgung 2005. www.kbv.de. 2007
Parker G, Chan B, Tully L, Eisenbruch M (2005) Depression in the Chinese: the impact of acculturation. Psychol Med 35:1475–1483
Ho K, Hunt C, Li S (2008) Patterns of help-seeking behavior for anxiety disorders among the Chinese speaking Australian community. Soc Psychiatry Psychiatr Epidemiol 43:872–877
Beck M, Matschinger H, Angermeyer M (2003) Social representations of major depression in West and East Germany: do differences still persist 11 years after reunification? Soc Psychiatry Psychiatr Epidemiol 38:520–525
Wright A, Jorm A, Harris M, McGorry P (2007) What’s in a name? Is accurate recognition and labelling of mental disorders by young people associated with better help-seeking and treatment preferences? Soc Psychiatry Psychiatr Epidemiol 42:244–250
Elkeles T, Seifert W (1992) Arbeitslosigkeit und Gesundheit Langzeitanalysen mit dem Sozio-Ökonomischen Panel. Soziale Welt 43:278–300
Häfner H (1990) Arbeitslosigkeit—Ursachen von Krankheit und Sterberisiken? Z Klin Psychol 14:1–17
Grobecker C, Krack-Roberg E, Sommer B (2006) Bevölkerung. In: Bundesamt Statistisches (ed) Wirtschaft und Statistik. SFG Servicecenter Fachverlage, Wiesbaden, pp 1261–1272
Lu Y (2008) Test of the ‘healthy migrant hypothesis’: a longitudinal analysis of health selectivity of internal migration in Indonesia. Soc Sci Med 67:1331–1339
Bernardi L, Klärner A, Lippe v.d. H (2008) Job insecurity and the timing of parenthood: a comparison between Eastern and Western Germany. Eur J Popul 24:287–313
Ehrenberg A (2004) Das erschöpfte Selbst. Depression und Gesellschaft in der Gegenwart. Campus, Frankfurt/Main
Hammer V2cbUH (2003) Auswirkungen der Sozialisation auf die berufliche Handlungskompetenz. Eine empirische Untersuchung am Beispiel von IBM Deutschland GmbH. Magisterarbeit, Universität Konstanz
Krüger H-H1cbUH (2003) Auswirkungen der Sozialisation auf die berufliche Handlungskompetenz. Eine empirische Untersuchung am Beispiel von IBM Deutschland GmbH. Magisterarbeit, Universität Konstanz
Acknowledgments
We are grateful to the Gmünder ErsatzKasse for enabling this study by providing data and resources. Many thank are due to Sharon Allard for proofreading this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bramesfeld, A., Grobe, T. & Schwartz, F.W. Prevalence of depression diagnosis and prescription of antidepressants in East and West Germany: an analysis of health insurance data. Soc Psychiat Epidemiol 45, 329–335 (2010). https://doi.org/10.1007/s00127-009-0067-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-009-0067-8