Abstract
Background
In recent years there has been increased interest in the role played by families in the treatment of patients with schizophrenia. Some family interventions may significantly reduce clinical difficulties and may have a positive impact, both emotionally and economically. The aim of this study is to assess the efficacy of a family psychoeducational program in changing attitude and health perceptions in relatives of patients with schizophrenia.
Methods
Sample: 45 relatives, key caregivers of patients with schizophrenia seen at a public mental health outpatient centre in Arica (Chile).
Instruments
Attitudes of Relatives toward Schizophrenia Questionnaire and General Health Questionnaire SF-36.
Procedure
The sample was randomly divided into a control group, in which caregivers received the usual treatment (a monthly interview with a psychiatric nurse), and an experimental group, which participated in a family psychoeducational intervention program in addition to the usual treatment. Medication of patients remained unchanged in both groups.
Results
The psychoeducational program was effective in modifying caregivers’ attitudes. However, it had no effect on their health perceptions.
Conclusions
This family psychoeducational treatment program modifies the negative attitudes of relatives towards schizophrenia. However, programs of this kind may not improve health problems; alternatively, their effects may only be seen in the long term.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years there has been increased interest in the role played by families in the community treatment of mental disorders. Some psychosocial family interventions in schizophrenia have suggested that a combination of family treatment and ideal doses of medicine may significantly reduce clinical, social and family difficulties and may have a positive impact, both emotionally and economically [24].
The initial focus of interest was the influence of the family environment on relapse in patients who had already experienced an episode of schizophrenia. That is to say, the emphasis was placed on the role of the domestic background in the course, rather than in the aetiology, of the disorder. Once identified, factors in the family context that trigger relapses can be modified and relapses may thus be prevented [3]. In recent years, more attention has been paid to the impact on the family [30] and especially the impact of schizophrenia on caregivers’ quality of life, attitudes, and coping styles [23, 27].
Providing information is recognized as an essential component of intervention programs, for both patients and relatives [14]. Psychoeducational interventions not only provide training but give important emotional reinforcement; they are normally carried out in small groups, providing information and psychological and social support in order to reduce the feelings of anxiety and to intensify feelings of trust. There is no evidence of superiority of one program over any other [24]. Leff et al. [18] suggest that gathering families together is the most cost-effective procedure, since in this way the therapist can treat a larger number of cases at the same time.
Psychoeducational interventions relieve the negative feelings characteristic of relatives of patients with schizophrenia, such as burden and remorse (though a recent study found that caregiver burden correlated positively with knowledge of schizophrenia: the greater the level of knowledge, the greater the level of burden [31]).
Psychoeducational programs are likely to enhance the relatives’ commitment to establishing cooperative relationships and therapeutic alliances and to broaden their knowledge and understanding of the disorder [39]. The insights gained may help change their attitudes to the illness and provide them with useful strategies for conflict resolution [6, 26]. Several investigations have associated relatives’ attitudes with variables such as patients’ relapses [7, 17, 25, 38], their social interaction [9], and caregiver burden [6, 8]. It has been found that empathic attitudes promote the social and occupational functioning of the patient and also facilitate conflict resolution [9].
Measures of these relatives’ health perceptions provide important information for health services. In most cases, it is the mother who takes on almost all the care of the patient with schizophrenia. Not surprisingly, female caregivers report the most negative perceptions of their own health status and the highest level of burden [1, 13].
The effects of schizophrenia on the family range in intensity, though the disorder inevitably leaves its mark on all family members. Moreover, some relatives may show strong features of schizotypy, complicating communication at home even more [12]. Anderson et al. [2] state that, as a consequence of the chronic stress associated with caregiving, the family experiences a series of conflicts and tends to show emotional responses such as anguish, fear, burden, stigma, frustration, rage, and sadness. Families may respond in many different ways: adapting to the situation, resorting to begging and praise, searching for the meaning of interactions with the patient, ignoring their behaviour, or taking on additional responsibilities that may increase burden. To a large extent, these responses are provoked by relatives’ attitudes towards the disorder. Berenstein [5] suggests that when a family group is organized along the health/disease axis, its social, economic, religious and psychological organization is modified.
In view of the importance of caregivers’ attitudes and quality of life, the current study was designed to measure the efficacy of a group family psychoeducational program in changing caregivers’ attitudes to schizophrenia and their general health perceptions. In a previous study [11], we found that this psychoeducational program was effective for reducing caregiver burden, assessed with the Zarit Caregiver Burden Scale.
Method
Subjects
We recruited the key caregivers of patients with schizophrenia who had undergone medical supervision at the health service during a three-month period. Key caregiver was defined as the relative who took care of the patient daily. All those invited to participate gave informed consent. The participants had not attended family groups or other support services before this intervention. The diagnoses of the patients were assessed by the Psychiatry staff of the public mental health centre, using ICD-10 criteria. A description of the sample is presented in the results section.
Instruments
The Cuestionario de Actitudes hacia la Esquizofrenia para Familiares (Relatives’ Attitudes toward Schizophrenia Questionnaire) [10] is a 37-item scale scored on a five-point Likert scale ranging from strongly disagree (1) to strongly agree (5). Most of the items have been taken from the Family Attitude Scale (FAS) [15], the Questionnaire of Family Opinions (QFO) [21], and the Family Coping Questionnaire (FCQ) [22]. It was decided to combine items from these instruments with a number of new items in order to produce a questionnaire that addressed the three components of attitudes (cognitive, behavioural and affective). A number of changes were also introduced as some of the statements in the abovementioned questionnaires refer to customs or behaviours which are not common in Chilean culture. The score ranges from 37 to 185, with lower scores indicating better attitudes towards the patient and the disorder. The instrument has a Cronbach’s alpha greater than 0.9. This questionnaire is available on request. Annex 1 gives examples of some of the items.
The second scale administered was the SF-36 General Health Questionnaire , a generic instrument comprising 36 items which cover eight dimensions of health status and yield a corresponding profile. The questionnaire items detect both positive and negative states of health. For each dimension the items are coded, grouped and transformed into a scale ranging from 0 (the worst state of health for that dimension) to 100 (the best state of health). Its content, which refers to both physical and mental health, its psychometric robustness, and its relative simplicity are all factors which make it easy to use in research [40]. The instrument has a Cronbach’s alpha greater than 0.85.
Procedure
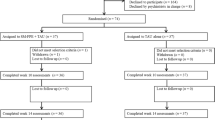
The sample was randomly divided into two groups. The assessment instruments were applied on an individual basis before and after the intervention in both groups.
The control group received standard treatment in the form of a monthly appointment with the psychiatric nurse, while in the experimental group carers took part in a multi-family psycho-educational program consisting of eighteen weekly sessions. The aim of this intervention was to change the attitudes and health perceptions of relatives of persons with schizophrenia, to teach family members to improve their coping and communication styles, and to reduce the emotional burden on families. The program was based around five modules dealing with the following topics: (1) the family’s experience of schizophrenia: families were encouraged to talk about the difficulties of living with a patient with schizophrenia and to share their experiences with families of other patients, in order to break down the sensation of “being alone”. (2) psycho-education: psychologists and psychiatrists worked together to help caregivers identify the causes, symptoms, signs of the illness, medications and side effects. (3) skills to improve communication: caregivers took part in role plays and discussions localized to the Chilean environment, reproducing Chilean customs, eating habits, and activities, and reflecting many aspects of Chilean life today (for example, how to cope with limited economic resources, how to ask for help, and so on). (4) relatives’ self-care, stressing how important it is for caregivers to take care of themselves, since their ability to care for others depends largely on their own well-being. Ways to share the burden and the importance of free time and of doing other activities were discussed in detail. This module, in particular, was planned to change the health perceptions of the participants. Session 16 focused on relaxation training, learning to relax and to eliminate corporal tensions, and the importance of breathing for relaxation. (5) evaluation of the intervention.
Three psychologists led the sessions, each of which lasted approximately one-and-a-half hours. A detailed description of the program can be found in a previous publication [11].
Patients in both groups continued to take their prescribed medication.
Statistical analysis
The efficacy of treatment was tested by applying repeated measures designs, with the experimental and control groups as the main between subjects factor, and the attitude measures and perception of health measures, before and after the intervention, as the within subjects factor. The corresponding ANOVAs were performed with SPSS version 15.
Results
The majority of patients were male (26 men vs. 15 women) and the age ranged from 19 to 66 years (mean 33.2 years, SD = 8.4). The mean age for the first episode of schizophrenia requiring hospitalization was 19.6 years (SD = 2.9). The diagnosis was paranoid schizophrenia in 63.9% of cases; residual in 14.6%; catatonic in 7.3%; hebephrenic in 7.3%; and simple in 7.3%. All patients except one were receiving pharmacological treatment. Of the total sample, 65.9% had not been admitted during the previous three years. Finally, regarding the educational level of patients, 73.2% had basic or intermediate studies and 26.9% had received higher education. Most patients had no work outside the home (90.2%) and the majority did not receive a state pension (58.5%).
Regarding relatives, all the key caregivers of patients with schizophrenia who supervised in the health service during a period of three months initially agreed to participate in the study (45). They were randomly assigned to two groups: 23 to the control group and 22 to the experimental group. In the latter group, four relatives (18.1%) subsequently dropped out of the intervention. The final sample therefore consisted of 41 main carers (31 women and 10 men) with a mean age of 54.2 years (SD = 15). Of these, 58.5% were married or lived with a partner; 43.9% worked outside the home. In terms of educational level, 80.5% had basic-intermediate studies, 14.6% held a technical diploma and 4.9% had received higher education. As regards the kinship relationship 63.4% were mothers, 14.6% fathers, 9.8% siblings, 4.9% spouses or partners and 2.4% children of the patient. In 4.9% of cases, the carer was a sheltered accommodation staff member. The mean time living with the patient was 28.6 years (SD = 9.7).
Efficacy of the program in terms of modifying the attitudes of carers
The results revealed a significant interaction between the groups and the evaluation time (F = 8.054; P = 0.007), showing that the treatment had a significant effect in terms of lowering scores on the attitude questionnaire. The significant interaction indicates that the improvement in attitude was only observed in the experimental group. Table 1 shows the means and standard deviations for the experimental and control groups on the attitude questionnaire, both before and after the intervention.
There was also a significant interaction between the groups, the evaluation time and the sex of the patient (F = 4.703; P = 0.037), indicating that the intervention was more effective among carers of female patients. An interaction was also observed between the groups, the evaluation time and the number of years living together (F = 4.377; P = 0.043): the improvement in attitudes toward the mental disorder, as a result of the psycho-educational program, was greater among carers who had lived longer with patients. The remaining variables (sex, age, occupation, type of kinship, marital status, and educational level of the carer, and age, educational level, receipt of pension and occupation of the patient) did not influence the effect of treatment on the attitudes of carers in this study.
In order to test the efficacy of treatment for each one of the questionnaire’s components (cognitive, affective and behavioural) the data were again entered into a repeated measures design. For the behavioural component we observed a significant interaction between evaluation time (before and after the intervention) and groups (F = 8.80; P = 0.005), indicating that the experimental group had improved significantly on this aspect by the end of the program, whereas this was not the case for the control group. There was also a significant interaction between evaluation time and group for the cognitive component (F = 12.99; P = 0.001), as the experimental group also improved significantly on this aspect, in contrast to controls. As regards the affective component, the interaction between evaluation time (before and after the intervention) and the groups (experimental and control) was significant (F = 3.59; P = 0.06), the results presenting the same trend as those for the other two components of attitude. Table 2 shows the means for each of the components of attitude for both groups, before and after the intervention.
Efficacy of the program in terms of carers’ perception of general health
The intervention had no effect on carers’ perception of health. Table 3 shows the treatment effect values for each subscale of the SF-36 questionnaire.
Table 4 shows the means and standard deviations for the three state-of-health subscales in the experimental and control groups before and after the program, as well as the treatment effect values for each of the questionnaire’s subscales. The intervention had no significant effect on any of the three areas of the SF-36.
Discussion
The psycho-educational program produced an improvement in the attitudes of relatives toward schizophrenia. This means that carers have learnt how to act, feel and think in a more positive and flexible way with respect to the disorder. This more positive attitude has direct repercussions on the relationship with the patient, as well as on carers themselves, who will thus have better and greater control over the various situations which arise when living with a schizophrenic relative. The results of the present research corroborate previous reports which showed that attitudes can be changed through family intervention, and also that they may differ according to the ethnic and cultural group of the relative or main carer [6, 20, 26, 28, 37].
It should be noted that the treatment effect was significant for all three components of attitude (behavioural, cognitive and affective), in other words, those participating in the program showed a more positive attitude on these three components by the end of the intervention than did the carers in the control group. The results also indicate that the intervention was more effective among carers of female patients; that is, these carers showed a greater change in attitude after completing the program. This may be due to the fact that the relatives and carers of male patients generally present higher levels of burden [29] which might make them more resistant to a change in attitude. As already mentioned, the carers of male patients have to deal with more episodes of violence, aggression and/or substance abuse, and thus the patient requires greater supervision. We also observed that the treatment was more effective in carers who had lived longer with patients, and their attitudes by the end of the program were similar to those who had lived with an ill relative for fewer years. Psycho-educational groups are known to improve levels of self-efficacy among relatives who have not previously participated in such groups [16, 32, 34]. Given that the carers in the present sample had not been exposed to any previous psycho-educational programs, and had been living with their situation for many years, they may have been more sensitive to the intervention and thus show a greater willingness to change their attitudes. Solomon et al. [33] suggest that the benefit of these initial experiences with other relatives of schizophrenic patients may be as important as the theoretical content of the psycho-educational program. The exposure to and exchange of experiences with other relatives is a highly significant stimulus which may motivate carers to change their attitudes [4]. It may also be that carers who have lived for fewer years with a patient have not yet had time to process all the changes taking place in the family milieu, and thus have yet to develop a negative attitude towards the disorder.
The present intervention had no influence over relatives’ perceptions of state of health. The data suggest that perception of health, regarded as an important component of quality of life, is a broader-ranging phenomenon and that any modifications it may undergo will not be immediately apparent at the end of an intervention. It remains to be seen whether an effect appears in the longer term; as Losada et al. [19] suggest, some carers may need more time to practise and use the strategies they have been taught, and thus any effect on perception of health will not be detected by an evaluation conducted at the end of an intervention. Moreover, the fact that carers are continually putting their own health-related needs on hold may make it more difficult to improve their perception with regard to both physical and psychological health.
Conclusions
Considering the relatively poor outcome of a large number of persons with schizophrenia, it is of great interest to explore the impact of psychoeducational programs that might contribute directly or indirectly to improving the course and the quality of life of these persons and of their relatives. It is also important to assess the efficacy of such programs in different countries and cultures. This is the main contribution of our study. Due to the procedure followed for the selection of the sample (we recruited caregivers of patients with schizophrenia who had medical supervision in the health service during a period of three months), it is not possible to assess whether this sample was or not representative of all the relatives/patients treated in the public mental health centre in Arica. This is a limitation of the study.
The results show the program to be an effective way of changing attitudes among relatives caring for a schizophrenic family member. Our findings for this Chilean sample are consistent with reports from other continents with different socio-economic and healthcare conditions [6]. Upon completion of the program the three components of attitude (behavioural, cognitive and affective) all improved notably. The reduction in negative attitudes may increase the family’s commitment to treatment, and even make them feel less pessimistic about the patient’s rehabilitation.
Despite these encouraging results with respect to changing attitudes, the intervention did not change the relatives’ perception of state of health. This is consistent with previous reports which have suggested that health problems cannot always be modified through such programs [35, 36]. It may be that the effect of the intervention is not immediately apparent upon its completion, since any effects on health due to application of new skills may take longer to emerge. It would useful to follow up the participants in this study within one or two years in order to test this hypothesis.
References
Alonso J, Prieto L, Antó J (1995) La versión española del SF-36 Health Survey (Cuestionario de Salud SF-36): un instrumento para la medida de los resultados clínicos. Med Clin (Barc) 10:771–776
Anderson C, Reiss D, Hogarty G (1986) Taller de supervivencia. In: Anderson C, Reiss D, Hogarty G (eds) Esquizofrenia y familia. Guía práctica de psicoeducación. Amorrortu, New York, pp 110–190
Barrowclough C, Terrier N (1995) Intervención con las familias. In: Barrowclough C, Tarrier N (eds) El tratamiento psicológico de la Esquizofrenia. Editorial Ariel, Barcelona, pp 69–99
Belloso J, García B, de Prado E (2000) Intervención psicoeducativa en un centro de rehabilitación psicosocial. Rev Asoc Esp Neuropsiquiatr XX(73):23–40
Berenstein I (1987) Familia y Enfermedad mental. Editorial Paidós, Buenos Aires
Berglund N, Olof J, Edman A (2003) Family intervention in schizophrenia. Impact on family burden and attitude. Soc Psychiatry Psychiatr Epidemiol 38:116–121
Butzlaff R, Hooley J (1998) Expressed emotion and psychiatric relapse. Arch Gen Psychiatry 55(6):547–551
Caqueo-Urízar A, Gutiérrez-Maldonado J (2006) Burden of care in families of patients with schizophrenia. Qual Life Res 15(4):719–724
Girón M, Gómez M (2004) Relationship between family attitude and social functioning in schizophrenia. J Nerv Ment Dis 192(6):414–420
Gutiérrez-Maldonado J, Caqueo-Urízar A (2003) Cuestionario de Actitudes hacia la Esquizofrenia para Familiares (unpublished manuscript)
Gutiérrez-Maldonado J, Caqueo-Urízar A (2007) Effectiveness of a psycho-educational intervention for reducing burden in latin american families of patients with schizophrenia. Qual Life Res 16(5):739–747
Gutiérrez-Maldonado J, Caqueo-Urízar A, Ferrer-García M (2006) Esquizotipia en familiares de pacientes con esquizofrenia en una muestra latinoamericana. Psicothema 18(3): 433–438
Gutiérrez-Maldonado J, Caqueo-Urízar A, Kavanagh DJ (2005) Burden of care and general health in families of patients with schizophrenia. Soc Psychiatry Psychiatr Epidemiol 40: 899–904
Hare R, Rogers H, Lester H, McManus R, Mant J (2006) What do stroke patients and their carers want from community services? Fam Pract 23(1):131–136
Kavanagh D, O’Halloran P, Manicavasagar V, Clark D, Piatkowska O, Tennant C, Rosen A (1997) The family attitude scale: reliabity and validity of a new scale for measuring the emotional climate of families. Psychiatry Res 70:185–195
Kazarian SS, Vanderheyden DA (1992) Family education of relatives of people with psychiatric disability: a review. Psychosoc Rehabil J 15:67–84
King S (2000) Is expressed emotion cause or effect in the mothers of schizophrenic young adults? Schizophr Res 45:65–78
Leff J, Berkowitz R, Shavit N, Strachan A, Glass I, Vaughn C (1990) A trial of family therapy versus a relatives group for schizophrenia. Two-year follow-up. Br J Psychiatry 157:571–577
Losada A, Izal M, Montorio I, Márquez M, Pérez G (2004) Eficacia de dos intervenciones psicoeducativas para cuidadores de familiares con demencia. Rev Neurol 38(8):701–708
Magliano L, Fadden G, Economou M, Held T, Xavier M, Guarneri M, Malangone C, Marasco C, Mm Maj (2000) Family burden and coping strategies in schizophrenia: 1-year follow-up data from the BIOMED I study. Soc Psychiatry Psychiatr Epidemiol 35:109–115
Magliano L, Marasco C, Guarneri M, Malangone C, Lacrimi G, Zanus P, Maj M (1999) A new questionnaire assessing the opinions of the relatives of patients with schizophrenia on the causes and social consequences of the disorder: reliability and validity. Eur Psychiatry 14:71–75
Magliano L, Veltro F, Guarneri M, Marasco C (1995) Clinical and social-demographic correlatos of coping strategies in relatives of schizophrenic patients. Eur Psychiatry 10:155–158
Martínez J, Nadal S, Beperet M, Mendióroz P, Psicot Group (2000) Sobrecarga de los cuidadores familiares de pacientes con esquizofrenia: factores determinantes. An Sist Sanit Navar 23(1):101–110
Montero I (1995) Tratamientos familiares y programas psicoeducativos en la esquizofrenia. In: Gutiérrez M, Escurre J, Pichot P (eds) Esquizofrenia entre la sociogénesis y el condicionamiento biológico (II). Ediciones en neurociencias, Barcelona, pp 219–227
Muela J, Godoy J (1998) Programa de Intervención Familiar en Esquizofrenia. Tesis Doctoral no publicada. Universidad de Granada, Granada
Mueser K, Sengupta A, Schooler N, Bellack A, Xie H, Glick I et al (2001) Family treatment and medication dosage reduction in schizophrenia: effects on patient social functioning, family attitude, and burden. J Consult Clin Psychol 69(1):3–12
Rakesh K, Singh T, Ganguly K (2007) Caregiver burden and coping. Soc Psychiatry Psychiatr Epidemiol 42:923–930
Ran M, Xiang M, Wan Chan C, Leff J, Simpson P, Huang M et al (2003) Effectiveness of psychoeducational intervention for rural Chinese families experiencing schizophrenia. A randomised controlled trial. Soc Psychiatry Psychiatr Epidemio 38:69–75
Samele C, Manning N (2000) Level of caregiver burden among relatives of the mentally ill in South Verona. Eur Psychiatry 15(3):196–204
Sayers S, White T, Zubritsky C, Oslin D (2006) Family involvement in the care of healthy medical outpatients. Fam Pract 23(3):317–324
Sefasi A, Crumlish N, Samalani P, Kinsella A, O’Callagahn E, Chilale H (2008) A little knowledge: caregiver burden in schizophrenia in Malawi. Soc Psychiatry Psychiatr Epidemiol 43:160–164
Solomon P (1996) Moving from psychoeducation to family education for families of adults with serious mental illness. Psychiatr Serv 47(12):1364–1370
Solomon P, Draine J, Mannion E (1996) The impact of individualized consultation and group work shop family education interventions in ill relative’s outcomes. J Nerv Ment Dis 184(4):252–255
Solomon P, Draine J, Mannion E, Meisel M (1997) Effectiveness of two models of brief family education: retention of gains by family members of adults with serious mental illness. Am J Orthopsychiatry 67(2):177–186
The Scottish Schizophrenia Research Group (1987) The Scottish First Episode Schizophrenia Study IV. Psychiatric and social impact on relatives. Br J Psychiatry 150:340–344
The Scottish Schizophrenia Research Group (1992) The Scottish First Episode Schizophrenia Study VIII. Five-years follow-up: clinical and psychosocial finding. Br J Psychiatry 161:496–500
Thompson M, Goldstein M, Lebel M, Mintz L, Marder S, Mintz J (1995) Schizophrenic patients’ perceptions of their relatives’ attitudes. Psychiatry Res 57:155–167
Tomaras V, Mavreas V, Economou M, Ionnovich E, Karydi V, Stefanis C (2000) The effect of family intervention on chronic schizophrenic under individual psychosocial treatment: a 3-year study. Soc Psychiatry Psychiatr Epidemiol 35:487–493
Vallina O, Lemos S (2001) Tratamientos psicológicos eficaces para la esquizofrenia. Psicothema 13(3):345–364
Ware J, Snow K, Kosinski M, Gandek B (1993) SF-36 Health Survey. Manual and Interpretation Guide. The Health Institute, New England Medical Center, Boston
Acknowledgments
This work was supported by Ministerio de Educación y Ciencia, Spain. Grants: SEJ2006-14301. Consolider Project “Nuevas tecnologías de la información y la comunicación: integración y consolidación de su uso en ciencias sociales para mejorar la salud, la calidad de vida y el bienestar”, and the research project SEJ2005-09170-C04-01.
Author information
Authors and Affiliations
Corresponding author
Annex 1: Attitudes of relatives toward schizophrenia questionnaire
Annex 1: Attitudes of relatives toward schizophrenia questionnaire
Main examples of its items. The questionnaire is available on request
Dr. José Gutiérrez-Maldonado and Dra. Alejandra Caqueo-Urízar
jgutierrezm@ub.edu
University of Barcelona
Below you will find a series of statements. Please choose and circle the response that best reflects your opinion. Please answer as honestly as possible, and remember that all the information you provide will be treated confidentially.
Rights and permissions
About this article
Cite this article
Gutiérrez-Maldonado, J., Caqueo-Urízar, A. & Ferrer-García, M. Effects of a psychoeducational intervention program on the attitudes and health perceptions of relatives of patients with schizophrenia. Soc Psychiat Epidemiol 44, 343–348 (2009). https://doi.org/10.1007/s00127-008-0451-9
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-008-0451-9