Abstract
Background
Excess mortality among people with schizophrenia due to natural and unnatural causes, especially due to suicides, is a well-known fact. It has been suggested that deinstitutionalization increases suicide mortality but there are also contradictory results. We studied the changes in mortality and causes of death among schizophrenia sufferers during and after the years of deinstitutionalization process in Finland.
Method
The sample, identified from the Finnish hospital discharge register (FHDR), consisted of patients aged 15–65 and hospitalized for the first time due to schizophrenia. We focused on the 5-year follow-up from inclusion years 1980–1998 (N = 23,959). Changes in 5-year follow-up mortality during the study period were explored for both genders and for different causes of death separately using multivariate logistic regression analyses.
Results
During the study period 1,926 deaths occurred. Suicide was the major cause of death in both genders. A significant reduction in overall 5-year mortality was observed among persons hospitalized in 1995–1998 when compared to people hospitalized 1980–1984. In males a significant reduction was seen in all mortality (P = 0.025) due to suicides (P = 0.007) but not in the case of natural deaths. In females no significant changes in mortality were found.
Conclusions
Our study confirms a reduction in suicide mortality of male schizophrenia sufferers after the deinstitutionalization process. However the overall mortality is still very high and the attention needs to be focused on the general well-being of schizophrenia patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Excess mortality in schizophrenia has been constant for the last decades according to numerous studies. Continuing excess mortality is due to suicides, physical disorders and accidental deaths. Mortality is elevated both in men and women [5, 22, 33, 53]. The calculated risk rates vary across studies. In a recent meta-analysis of 37 studies on schizophrenia mortality [53] the risk of dying was 2.5 fold compared to the general population. In Finland the risk has been estimated to be threefold compared to that of general population and the risk seems to be highest during the first 5 years after onset. The risk seems to decrease among those with more than 10 years duration of illness [20]. Nevertheless there are studies reporting that the mortality risk of long-stay psychiatric patients is likewise high, possibly due to inadequate somatic care and patients´ limited ability to describe their symptoms [52].
The risk of unnatural deaths is heightened during the first years after discharge from hospital [55], suicide being the most common cause of premature mortality. According to a Finnish nationwide register study the risk of suicide was ten-fold compared to that of general population [20]. The results of a recent meta-analysis [53] confirm the high suicide risk in schizophrenia and are in line with the Finnish finding. The first year after diagnosis of schizophrenia and the first days after discharge have been associated with suicide in recent studies [41, 50]. Rossau and Mortensen noted [50] that being admitted to a general hospital for physical disorders increased the risk of later suicide. Excess mortality caused by suicides is a matter of great concern in young age-groups, especially in men [4, 20, 43, 46].
Excess mortality in schizophrenia due to natural causes like cerebrovascular, respiratory and alcohol related diseases, metabolic disorders and malignancies has been confirmed by several studies [5, 18, 22]. In the case of cancer studies have shown mixed results [8, 17, 19, 30, 34]. Ischaemic diseases among psychiatric patients have been a matter of interest among researchers for the past two decades due to rising death rates. Mortality among general population has decreased but the mortality rate trend due to ischaemic diseases has been increasing among female psychiatric patients and has remained unchanged in men [29]. Recent studies have shown the prevalence of diabetes type 2 increasing among schizophrenia patients over the course of illness compared to that of the general population [9, 11, 61]. Koro et al. [27] have connected the risk of diabetes with the use of olanzapine and Arranz et al. [3] have shown an association between glucose metabolism and antipsychotic medication. On the other hand abnormal glucose metabolism seems to occur even among first-episode patients [11, 51]. Among chronic schizophrenia patients mortality due to natural causes has been shown to be predicted by age, physical illness and number of hospital days [58].
It has been suggested that atypical antipsychotic drugs as well as conventional neuroleptics and antipsychotic polypharmacy contribute to an elevated mortality risk [1, 23, 41, 47, 48, 57]. However, a recent nationwide Finnish study points to an elevated suicide risk in patients not taking antipsychotics when compared patients taking antipsychotics [62]. Unhealthy lifestyle factors like heavy smoking, inadequate physical activity and over-weight due to medication and poor diet also cause comorbidity and premature deaths [6, 7, 39]. A recent study on the health habits of schizophrenia patients revealed that unemployment combined with schizophrenia is associated with unhealthy behaviour [49].
The deinstitutionalization process in Finland has cut the number of psychiatric beds to one fourth of the number available in the early 1970s [37]. In Finland the development of outpatient care in connection with deinstitutionalization was complicated by a severe economic recession in the early 1990s. In spite of this, the use of outpatient care and housing services provided by entrepreneurs and non-governmental organizations has increased [59]. There has been concern about how outpatient care is able to respond to the challenge of shortening hospital periods and taking care of more seriously ill patients. A significant notion is that the reduction of psychiatric beds has led to an increase in daily neuroleptic medication among those treated in out-patient clinics [57]. It has been suggested that deinstitutionalization increases suicide mortality [33, 42], but there are contradictory results, too [20, 45], particularly regarding post-discharge suicide mortality [44].
In Finland the process of deinstitutionalization has gone relatively fast and begun later than in many other western countries. A comprehensive evaluation of the effect of deinstitutionalization has not so far been conducted in Finland. The objective of this study is to analyse the changes in 5-year mortality and the causes of death among schizophrenia patients hospitalized for the first time with schizophrenia diagnosis between 1980 and 1998 during and after the deinstitutionalization process.
Materials and methods
Materials
Our study is a part of a larger register data project on the treatment situation of schizophrenia in Finland between the years 1980 and 2003. The study population, a total of 30,278 new hospitalized schizophrenia patients, is based on the nation-wide Finnish hospital discharge register (FHDR). The data consists of all those hospitalized for the first time with a primary or secondary diagnosis of schizophrenia during the period 1980–2003. Patients aged 15 to 65 at index hospitalization were included in the study. Of the total sample 53.5% were males.
Methods
The FHDR provided the information on all hospital treatment periods and information on diagnoses. The FHDR covers all mental and general hospitals as well as wards of local health centres, military wards, prison hospitals and private hospitals. The psychiatric diagnostic classification used in Finland was ICD-8 [64] until 1986, from 1987 to 1995 ICD-9 based on DSM-III-R [2] criteria and from 1996 ICD-10 [65]. Of the schizophrenia diagnoses both primary and secondary diagnoses were considered in our data: ICD-8 and ICD-9 codes 295, ICD-10 codes F20 and F25. The Registers of the Social Insurance Institution (RSII) provided information concerning the dates of disability pensions granted due to schizophrenia. Of the subjects 2,704 had already been granted a disability pension because of schizophrenia before the first hospital treatment for it.
The information on dates, places and causes of death were obtained from the data of Statistics Finland. Causes of death were classified into natural, i.e. deaths from diseases and medical conditions (subdivided into malignancies, diseases of the circulatory system and other somatic diseases) and unnatural, i.e. deaths from external causes (subdivided into alcohol-related reasons, suicides and other unnatural causes). Of the subjects 5,358 died before the 31 December 2003.
Statistical methods
The study focused on mortality during 5-year follow-up. For the analyses to be able to follow each subject for the whole of five years, only data from inclusion years 1980–1998(n = 23,959) was used. Inclusion year was classified into four categories: 1980–1984 (reference class in analyses), 1985–1989, 1990–1994 and 1995–1998. Age at inclusion was categorized into 3 groups: 15–29 (reference class in analyses), 30–44 and 45–65. The sociodemographic backgrounds and 5-year mortality of the subjects are shown in Table 1.
To evaluate the association between mortality and inclusion year and age at inclusion, multivariate logistic regression analyses were performed. The multivariate analyses were carried out for both genders and for different causes of death separately. P value < 0.05 was used to denote statistical significance. Data were analysed with SPSS for Windows, version 13.00
Results
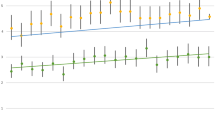
Within the 5-year follow-up 1,926 deaths occurred, 8% of the study sample (yearly mortality is presented in Table 1). The proportion of deaths was significantly (P < 0.001) higher in males (n = 1,292, 10.1%) than in females (n = 634, 5.7%). Natural causes of death accounted for 38.6% of the 5-year mortality. Of all deaths detected, 42.0% (n = 809) were due to suicides, 20.9% (n = 403) to diseases of the circulatory system, 13.7% (n = 263) to accidental deaths, 7.1% (n = 136) to metabolic causes, 6.7% (n = 129) to malignancies, 3.9% (n = 75) to respiratory diseases and 3.5% (n = 67) to alcohol-related reasons. Suicide was the major cause of deaths in both males (44.5%) and females (36.9%) and mortality due to diseases of the circulatory system the second largest (males 19.1% and females 24.8%). 5-year mortality by each inclusion year and causes of death can be seen in Fig. 1.
There was a diminishing trend in mortality of schizophrenia sufferers during the study years (P = 0.062) and a significant reduction during the last observation period: OR 1.00, 95% CI 0.88–1.13 for inclusion years 1985–1989, OR 1.02, 95% CI 0.90–1.16 for inclusion years 1990–1994 and OR 0.85, 95% CI 0.73–0.97 for inclusion years 1995–1998. In the case of natural causes the trend was parallel, but not significant. Age was associated significantly (P < 0.001) with all-cause mortality (OR 1.15, 95% CI 1.02–1.30 for age group 30–44 and OR 2.70, 95% CI 2.41–3.02 for age group 45–65) and natural-cause mortality (OR 3.03, 95% CI 2.16–4.25 for age group 30–44 and OR 22.39, 95% CI 16.55–30.30 for age group 45–65). In the case of unnatural causes the trend was controversial (OR 0.97, 95% CI 0.85–1.11 for age group 30–44, OR 0.85, 95% CI 0.72–1.00 for age group 45–65).
In males a significant reduction was found in all-cause mortality (see Table 2) due to the last inclusion year category (1995–1998). This reduction was seen in unnatural causes of death, but not in natural causes. In the case of suicides a significant reduction was found in 1995–1998 and in the case of other unnatural causes (i.e. accidents, homicide) an increase was seen in 1990–1994. Age was associated with all-cause mortality and with natural causes. In more detailed analyses the same age association was found in malignancies, diseases of the circulatory system, other somatic causes, alcohol-related reasons and other unnatural causes of death. In the case of male suicides the age association was reversed; the highest mortality risk was in the youngest age-group (15–29).
In the observation of female deaths, the inclusion year was not statistically significantly associated with any cause of death studied. Age predicted all-cause mortality and natural causes of death. In more detailed analyses in the case of malignancies, diseases of the circulatory system and other somatic causes an age association was found.
Discussion
The main finding of our study was that the mortality of Finnish schizophrenia patients did not increase during a very rapid deinstitutionalization process, when economic recession, reduction of psychiatric beds and simultaneous lack of capacity to increase out-patient care was the prevailing reality. Instead, in males we found a reduction in mortality due to fewer suicides. In the case of circulatory diseases in males the mortality decreased in the two last study periods. There was no reduction in female mortality during the periods under observation.
Earlier studies conducted in Denmark [33] and Sweden [42] reported that reduction of psychiatric beds led to an increase in mortality among schizophrenia patients. However, two earlier Finnish studies from the reduction era 1980–1996 [19, 58] concur with our results showing diminishing mortality. An explanation for the better situation in Finland may be the number of psychiatric beds still remaining high in the middle of the 1990’s; 1.3 beds per 1,000 inhabitants [58]. In 2003 there were slightly less than 1.0 bed per 1,000 inhabitants [37].
The period of the first 15 years in this study (1980–1995) does not show changes in all-cause mortality of schizophrenia patients either in males or in females. The last era, meaning people hospitalized with schizophrenia for the first time in 1995–1998, indicated a significant reduction in all-cause mortality in males mainly caused by suicides compared to the first inclusion year category 1980–1984. The trend is similar to what has previously been found concerning suicides in Finnish population [40, 44]; the reduction was 24% from 1990 to 2001. The most significant decrease was seen among those who had not recently been hospitalized [44]. Among schizophrenia patients the risk of suicide decreased during the first year after discharge [44]. The treatment of depression in population has been an ongoing source of concern in primary health care in Finland and the use of antidepressive drugs has grown sevenfold during the period 1990–2006 [15]. According to Korkeila et al. [26] there is an association between the falling number of suicides and growing use of antidepressive drugs in population. It is possible that schizophrenia patients suffering from depression may benefit from this trend.
In the present study the risk of committing suicide diminished as subjects aged. The effect of gender was as expected; males committed suicide more commonly than females. When comparing schizophrenia patients to the general population Mortensen and Juel [33] in their register-based study found that relative suicide risk for females was higher than among males under 60 but the absolute rate of suicides was higher in males. Rossau and Mortensen [50] in their case-control study among schizophrenics found that male gender was related to increased suicide risk while Nordentoft et al. [38] found that the suicide rate had fallen in both sexes.
Diseases of the circulatory system play an important role when discussing mortality in schizophrenia irrespective of gender. In line with earlier studies [33, 41] we found high mortality from diseases of the circulatory system, especially in the older age-groups. Räsänen et al. [52] in a study on long-stay patients (80.2% had schizophrenia) in Northern Finland also found that diseases of the circulatory system caused most excess deaths in both genders. Ösby et al. [42] found the risk of death in males to increase 4.7 fold and the risk of females 2.7 fold in case of cardiovascular disease during the follow-up period. According to another Swedish study [41] cardiovascular disease was the major cause of death in females while suicide was the main cause of excess mortality in males. Recently Fors et al. [16] in a register- and interview-based study reported no gender difference in causes of mortality in general but that cardiovascular mortality was significantly associated with schizophrenia in males. During the time period 1980–2003 mortality due to natural causes among Finnish working age population diminished markedly among both men and women. In our study no significant reduction was found. It must be kept in mind, however, that it is extremely difficult to compare the yearly statistics of deaths from Statistics Finland to the results of the present 5-year follow-up study. Our subjects were chosen according to inclusion year and were followed up for the whole of five years for the analyses.
It has been suggested that schizophrenia patients receive inadequate somatic care and that they suffer from lack of proper treatment [10, 21, 28]. Druss et al. [14] studied the association between severe mental disorders, quality of health care and mortality from cardiovascular diseases among older patients with schizophrenia. They concluded—like Young and Foster [66]—that practices of cardiac procedures after infarction differ for patients with or without mental disorders. Munk-Jørgensen et al. [36] observed (according to admissions to somatic departments) that the diseases of schizophrenia patients remain undiagnosed until the acute phase of physical illness. Connolly and Kelly [9] have pointed out that schizophrenia sufferers have difficulties in recognizing or expressing the early symptoms of physical illness in contrast to the results of self-report data [12]: the seriously ill psychiatric patients utilized basic medical services (excluding the specialist care in schizophrenia) equally as much as general population. Dixon et al. [13] in their study based on inpatient interviews questioned the argument of mental patients not being capable of considering health questions.
It is obvious, even though mortality from diseases of the circulatory system seems to have decreased in Finland, that schizophrenia and other serious mental illnesses challenge staff in primary care and psychiatric care to be more aware of the physical health and ill-health of schizophrenia patients. Our result suggests that the gap in mortality due to natural causes is widening between schizophrenia patients and other people. In other words, this group of patients has not benefitted from better services and care. According to a recent comprehensive review [53] this unfortunate finding seems to occur in other countries, too, and is a challenge for caregivers. A recent Finnish HealthQUEST country report [63] has highlighted that inequality and barriers to access to general healthcare among people with mental disorders should be identified and removed in order to prevent excess mortality. Muir-Cochrane [35] has concluded that nursing care practices should be broadened to concern the mental and the physical ill-health of schizophrenia sufferers. In Finland we have in primary care nurses specialized in depression or alcohol abuse—why not in combinations of schizophrenia and any somatic illness? We did not find any changes in mortality with malignancies among patients suffering from schizophrenia. However, Harris and Barraclough [19] in a comprehensive review found a slight deficit of cancer in males and a slight excess of mortality in females. In a study by Cohen et al. [8] female gender was one of the risk factors in cancer mortality.
In all, the mortality in the present study was 8%, being higher compared to an earlier Finnish five-year follow-up study [56]. Moreover, a third of deaths in males occurred between the ages of 15 and 44 the proportion being slightly smaller for women. In a previous 2-year follow-up study of first-contact schizophrenia patients Salokangas and Stengård [55] found that males had more negative beliefs about their future life situation, a prediction which had some influence on outcomes regarding their premorbid development.
Limitations and strengths of the study
The present study was based on register data; therefore it was impossible to study the interaction of medication and somatic diseases. On the other hand, the reliability of the FHDR [25] has been proven in various studies to be high, especially regarding schizophrenia [32]. In theory it is possible that subjects who were disability pensioned before 1980 had their first treatment after 1980. Traditionally the treatment for schizophrenia in Finland has started with hospitalization, with a small proportion of patients being treated in out-patient care. The data was supplemented by a sample of subjects already on pension due to schizophrenia also aiming to include in the sample those schizophrenia patients who were treated solely in out-patient care. The proportion of the pension group remained constant. The sample of the present study was large and nationally representative and the observation period was exceptionally long (almost 20 years).
Conclusions
The resources of health care and psychiatric health care to cover the medical needs of schizophrenia patients have been questioned, especially in light of the deinstitutionalization process [31, 36, 60]. On the other hand, the proportion of psychiatric treatment in primary healthcare wards has increased over the period in question [24] and schizophrenia patients (especially males) are commonly discharged into rehabilitation homes [54], which may be a protective factor in the course of their illness. This kind of housing prevents, at least to some extent, unhealthy lifestyle, especially alcohol and drug abuse and offers support (also peer-support) in daily life.
The results of our study support the conclusion that concerning outcomes of treatment of schizophrenia, the Finnish psychiatric health-care system operates at the same level as it used to before the deinstitutionalization process. On the other hand, there is much to do concerning the excess mortality among schizophrenia sufferers. The somatic care of schizophrenia patients needs to be highlighted both in psychiatric inpatient and out-patient care and in primary health care.
References
Auquier P, Lancon C, Rouillon F, Lader M, Holmes C (2006) Mortality in Schizophrenia. Pharmacoepidemiol Drug Saf 15:873–879
American Psychiatric Association (1987) DSM-III-R: diagnostic and statistical manual of mental disorders. 3rd edn. APA, Washington, DC
Arranz B, Rosel P, Ramírez N, Dueñas R, Fernández P, Sanchez JM, Navarro MA, San L (2004) Insulin resistance and increased leptin concentrations in noncompliant schizophrenia patients but not in antipsychotic-naïve first-episode schizophrenia patients. J Clin Psychiatry 65:1335–1342
Babidge NC, Buhrich N, Butler T (2001) Mortality among homeless people with schizophrenia in Sydney, Australia. A 10-year follow-up. Acta Psychiatr Scand 103:105–110
Brown S (1997) Excess mortality of schizophrenia. Br J Psychiatry 171:502–508
Brown S, Birtwistle J, Roe L, Thompson C (1999) The unhealthy lifestyle of people with schizophrenia. Psychol Med 29:697–701
Brown S, Inskip H, Barraclough B (2000) Causes of the excess mortality of schizophrenia. Br J Psychiatry 177:212–217
Cohen ME, Dembling B, Schorling JB (2002) The association between schizophrenia and cancer: a population-based mortality study. Schizophr Res 57:139–146
Connolly M, Kelly C (2005) Lifestyle and physical health in schizophrenia. Advan Psychiatr Treat 11:125–132
D’Avanzo B, La Vecchia C, Negri E (2003) Mortality in long-stay patients from psychiatric hospital in Italy: results from the Qualyop project. Soc Psychiatry Psychiatr Epidemiol 38:385–389
De Hert M, van Winkel R, van Eyck D, Hanssens L, Wampers M, Scheen A, Peuskens J (2006) Prevalence of diabetes, metabolic syndrome and metabolic abnormalities in schizophrenia over the course of the illness: a cross-sectional study. Clin Pract Epidemiol Ment Health 2:14
Dickerson FB, McNary SW, Brown CH, Kreyenbuhl J, Goldberg RW, Dixon LB (2003) Somatic healthcare utilization among adults with serious mental illness who are receiving community psychiatric services. Med Care 4:560–570
Dixon L, Postrado L, Delahanty J, Fischer P, Lehman A (1999) The association of medical comorbidity in schizophrenia with poor physical and mental health. J Nerv Ment Dis 187:496–502
Druss BG, Bradford DW, Rosenheck RA, Radford MJ, Krumholz HM (2000) Mental disorders and use of cardiovascular procedures after myocardial infarction. JAMA 283:506–511
Finnish Statistics on Medicines (2007) National Agency for Medicines and Social Insurance Institution. Helsinki
Fors BM, Isacson D, Bingefors K, Widerlöv B (2007) Mortality among persons with schizophrenia in Sweden: An epidemiological study. Nord J Psychiatry 61:253–259
Grinshpoon A, Barchana M, Ponizovsky A, Lipshitz I, Nahon D, Tal O, Weizman A, Levav I (2005) Cancer in schizophrenia: is the risk higher or lower? Schizophr Res 73:333–341
Harris E, Barraclough B (1998) Excess mortality of mental disorder. Br J Psychiatry 173:11–53
Halbreich U, Shen J, Panaro V (1996) Are chronic psychiatric patients at increased risk for developing breast cancer? Am J Psychiatry 153:559–560
Heilä H, Haukka J, Suvisaari J, Lönnqvist J (2005) Mortality among patients with schizophrenia and reduced psychiatric hospital care. Psychol Med 35:725–732
Jeste DV, Gladsjo JA, Lindamer LA, Lacro JP (1996) Medical comorbidity in schizophrenia. Schizophr Bull 22:413–430
Joukamaa M, Heliövaara M, Knekt P, Aromaa A, Raitasalo R, Lehtinen V (2001) Mental disorders and cause-specific mortality. Br J Psychiatry 179:498–502
Joukamaa M, Heliövaara M, Knekt P, Aromaa A, Raitasalo R, Lehtinen V (2006) Schizophrenia, neuroleptic medication and mortality. Br J Psychiatry 188:122–127
Kaltiala-Heino RK, Laippala P, Joukamaa M (2001) Has the attempt to reduce psychiatric inpatient treatment been successful in Finland? Eur Psychiatry 16:215–221
Keskimäki I, Aro S (1991) Accuracy of data on diagnoses, procedures and accidents in the Finnish Hospital Discharge Register. Int J Health Sci 2:15–21
Korkeila J, Salminen JK, Hiekkanen H, Salokangas RKR (2007) Use of antidepressants and suicide rate in Finland: an ecological study. J Clin Psychiatry 68:505–511
Koro CE, Fedder DO, ĹItalien GJ, Weiss SS, Magder LS, Kreyenbuhl J, Revicki DA, Buchanan RW (2002) Assessment of independent effect of olanzapine and risperidone on risk of diabetes among patients with schizophrenia: population-based nested case-control study. BMJ 325:243–247
Lawrence D, Jablensky AV, Holman CDJ, Pinder TJ (2000) Mortality in Western Australian psychiatric patients. Soc Psychiatry Psychiatr Epidemiol 35:341–347
Lawrence D, Holman C, Jablensky A, Hobbs MST (2003) Death rate from ischemic heart disease in western Australian psychiatric patients 1980–1998. Br J Psychiatry 182:31–36
Lichtermann D, Ekelund J, Pukkala E, Tanskanen A, Lönnqvist J (2001) Incidence of cancer among persons with schizophrenia and their relatives. Arch Gen Psychiatry 58:573–578
Middelboe T, Mackeprang T, Hansson L, Werdelin G, Karlsson H, Bjarnason O, Bengtsson-Tops A, DyBBro J, Nilsson LL, Sandlund M, Sörgaard KW (2001) The Nordic study on schizophrenic patients living in the community. Subjective needs and perceived help. Eur Psychiatry 16:207–215
Moilanen K, Veijola J, Läksy K, Mäkikyrö T, Miettunen J, Kantojärvi L, Kokkonen P, Karvonen J, Herva A, Joukamaa M, Järvelin M-R, Moring J, Jones P, Isohanni M (2003) Reasons for the diagnostic discordance between clinicians and researches in schizophrenia in the Northern Finland 1966 Birth Cohort. Soc Psychiatry Psychiatr Epidemiol 38:305–310
Mortensen PB, Juel K (1993) Mortality and causes of death in first admitted schizophrenic patients. Br J Psychiatry 163:183–189
Mortensen PB (1994) The occurrence of cancer in first admitted schizophrenic patients. Schizophr Res 12:185–194
Muir-Cochrane E (2006) Medical comorbidity risk factors and barriers to care for people with schizophrenia. J Psychiatr Ment Health Nurs 13:447–452
Munk-Jørgensen P, Mors O, Mortensen PB, Ewald H (2000) The schizophrenic patient in the somatic hospital. Acta Psychiat Scand 102:96–99
National Research and Development Centre for Welfare and Health (2005) STAKES/Tilastotiedote. www.stakes.fi/FI/tilastot/aiheittain/Mielenterveys/indew.htm
Nordentoft M, Laursen TM, Agerbo E, Qin P, Hoyer EH, Mortensen PB (2004) Change in suicide rates for patients with schizophrenia in Denmark, 1981–97: nested case-control study. BMJ 329:261
Osborn DPJ, Nazareth I, King MB (2007) Physical activity, dietary habits and Coronary Heart Disease risk factor knowledge amongst people with severe mental illness. Soc Psychiatry Psychiatr Epidemiol 42:787–793
Öhberg A, Lönnqvist J (1997) Suicide trends in Finland 1980–1995. Psychiatr Fenn 28:11–23
Ösby U, Correia N, Brandt L, Ekbom A, Sparen P (2000a) Mortality and causes of death in schizophrenia in Stockholm County, Sweden. Schizophr Res 45:21–28
Ösby U, Correia N, Brandt L, Ekbom A, Sparen P (2000b) Time trends in schizophrenia mortality in Stockholm County. BMJ 321:19–26
Palmer BA, Pankratz VS, Bostwick M (2005) The lifetime risk of suicide in schizophrenia. A re-examination. Arch Gen Psychiatry 62:247–253
Pirkola S, Sohlman B (2007) Reductions in postdischarge suicide after deinstitutionalization and decentralization: A Nationwide Register Study in Finland. Psychiatr Serv 58:221–226
Pompili M, Amador XF, Girardi P, Harkavy-Friedman J, Harrow M, Kaplan K, Krausz M, Lester D, Meltzer HY, Modestin J, Montross LP, Mortensen PB, Munk-Jørgensen P, Nielsen J, Nordentoft M, Saarinen PI, Zisook S, Wilson ST, Tatarelli R (2007) Suicide risk in schizophrenia: learning from the past to change the future. Ann Gen Psychiatry 6:10
Radomsky ED, Haas GL, Mann JJ, Sweeney JA (1999) Suicidal behaviour in patients with schizophrenia and other psychotic orders. Am J Psychiatry 156:1590–1595
Reist C, Mintz J, Albers L, Jamal MM, Szabo S, Ozdemir V (2007) Second-generation antipsychotic exposure and metabolic-related disorders in patients with schizophrenia: An observational pharmacoepidemiologial study from 1988 to 2002. J Clin Psychopharmacol 27:46–51
Robinson DG, Worner MG, Napolitano B, Patel RC, Sevy SM, Gunduz-Bruce H, Soto-Perello JM, Mendelowitz A, Khadivi A, Miller R, MacCormack J, Lorell BS, Lesser ML, Schooler NR (2006) Randomized comparison of olanzapine versus risperidone for the treatment of first-episode schizophrenia: 4-month outcomes. Am J Psychiatry 163:2096–2102
Roick C, Fritz-Wieacker A, Matschinger H, Heider D, Schindler J, Riedel-Heller S, Angermeyer MC (2007) Health habits of patients with schizophrenia. Soc Psychiatry Psychiatr Epidemiol 42:268–276
Rossau CD, Mortensen PB (1997) Risk factors for suicide in patients with schizophrenia: nested case-control study. Br J Psychiatry 171:355–359
Ryan MC, Flanagan S, Kinsella U, Keeling F, Thakore JH (2004) The effects of atypical antipsychotics on visceral fat distribution in first episode, drug-naïve patients with schizophrenia. Life Sci 74:1999–2008
Räsänen S, Hakko H, Viilo K, Meyer-Rochow VB, Moring J (2003) Excess mortality among long-stay psychiatric patients in Northern Finland. Soc Psychiatry Psychiatr Epidemiol 38:297–304
Saha S, Chant D, McGrath J (2007) Is the differential mortality gap worsening over time? A systematic review of mortality in schizophrenia. Arch Gen Psychiatry 64:1123–1131
Salo M, Kallinen M (2007) Yhteisasumisesta yhteiskuntaan? Mielenterveyskuntoutujien asumispalveluiden tila ja tulevaisuus. Mielenterveydenkeskusliitto, Pori
Salokangas RKR, Stengård E (1990) Gender and short-term outcome in schizophrenia. Schizophr Res 3:333–345
Salokangas RKR, Stengård E, Räkköläinen V, Alanen YO, Kaljonen A (1991) Uusien skitsofreniapotilaiden hoito ja ennuste (USP-projekti) V:Viiden vuoden ennuste (English Summary: Treatment and prognosis of new schizophrenia patients).Reports of Psychiatria Fennica No 95, Helsinki
Salokangas RKR, Honkonen T, Stengård E, Koivisto A-M (2001) Skitsofreniapotilaiden neuroleptilääkehoito ja sen muutokset sairaansijojen vähetessä. SLL 25–26:2755–2762
Salokangas RKR, Honkonen T, Stengård E, Koivisto A-M (2002) Mortality in chronic schizophrenia during decreasing number of psychiatric beds in Finland. Schizophr Res 54:265–275
Salokangas RKR (2004) Psychiatric specialist care in Finland-achievements and challenges. J Ment Health 13:47–54
Salokangas RKR (2007) Medical problems in schizophrenia patients living in the community (alternative facilities). Curr Opin Psychiatry 20:402–405
Suvisaari J, Perälä J, Saarni SI, Härkänen T, Pirkola S, Joukamaa M, Koskinen S, Lönnqvist J, Reunanen A (2007) Type 2 diabetes among persons with schizophrenia and other psychotic disorders in a general population survey. Eur Arch Psychiatry Clin Neurosci (Online) Nov 7
Tiihonen J, Wahlbeck K, Lönnqvist J, Klaukka T, Ioannidis PA, Volavka J, Haukka J (2006) Effectiveness of antipsychotic treatments in nationwide cohort of patients in community care after first hospitalisation due to schizophrenia and schizoaffective disorder: observational follow-up study. BMJ 333:224–227
Wahlbeck K, Manderbacka K, Vuorenkoski L, Kuusio H, Luoma M, Widström E (2007) Equality in access to healthcare – focus on migrants, old people and people with mental disorders. HealthQUEST country report for Finland. STAKES reports, Helsinki
World Health Organization (1967) The ICD-8 classification of mental and behavioural disorders. World Health Organization, Geneva
World Health Organization (1992) The ICD-10 classification of mental and behavioural disorders. World Health Organization, Geneva
Young JK, Foster DA (2000) Cardiovascular procedures in patients with mental disorders. JAMA 284(letter), 3198
Acknowledgments
This study was made possible by funding from the Academy of Finland (project number 207481).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rantanen, H., Koivisto, AM., Salokangas, R.K.R. et al. Five-year mortality of Finnish schizophrenia patients in the era of deinstitutionalization. Soc Psychiat Epidemiol 44, 135–142 (2009). https://doi.org/10.1007/s00127-008-0414-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-008-0414-1