Abstract
Background
Deliberate self-harm has become more prevalent among adolescents.
Aims
To investigate the prevalence and the associated background factors of self-cutting and other self-harming behaviour.
Methods
The study sample included 4,205 adolescents aged 13–18 years. Background factors, social relationships, alcohol and substance abuse, self-harm and self-cutting were assessed by a structured questionnaire including the Youth Self Report and Beck Depression Inventory.
Results
The life-time prevalence of self-cutting was 11.5% and of other self-harm 10.2%, while the prevalence of current self-cutting was 1.8%. Self-cutting was associated with female gender and a very wide range of adverse psychosocial background variables. Parents living together were an independent protective factor. By contrast, there was no gender difference in the risk of other self-harm. Independent risk factors were depressive mood, somatic complaints, drug abuse, poor school performance and poor family relationships. No protective factors were found for other self-harm.
Conclusions
During adolescence, self-cutting and other self-harm are common. Adolescents who have self-cutting or harm themselves have wide-ranging problems in their lives. The specific characteristics of these phenomena need further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, deliberate self-harm has clearly become more prevalent among adolescents [8, 15, 23]. It has been shown to be associated with different psychiatric disorders such as depression, bipolar disorder and borderline personality disorder [7, 9–11, 19, 25]. Self-mutilation as a form of self-harm is also common in non-clinical samples of adolescents [20].
In England [17] and in Australia [4] the prevalence of deliberate self-harm was 6–7% among adolescents and the main methods were self-cutting and overdosing with medication.
A recent meta-analysis revealed that 13% of adolescents have engaged in deliberate self-harm at some point, while suicidal thoughts have been reported by 20–30% of adolescents and approximately 10% of adolescents have attempted suicide, 6% during the preceding 12 months [5]. The meta-analysis included 128 population-based studies (including 518,188 study subjects) of self-reported suicidal phenomena among adolescents. Nevertheless, the authors concluded that methodological factors, for example study population and terminology used, may influence the results.
Thus, although Evans et al. [5] included an exhaustive number of studies and study subjects in their meta-analysis, there is still a need for studies that use terminology carefully and consistently, where adolescents are asked to describe self-harm with the use of consistently-defined terminology (i.e. self-cutting; other kinds of self-harm), and which have clear time frames and include a sufficient number of study subjects. In this study we investigated self-harming behaviours, distinguishing self-cutting from other forms of self-harming behaviours in a relatively large, regionally comprehensive sample of 13- to 18-year-old Finnish adolescents. Our first aim was to determine the prevalence of self-cutting and other kinds of self-harm. We used the definition proposed by Favazza [6], according to which self-mutilation is a deliberate act to destroy one’s own body tissue without a conscious intent to die. This definition includes self-cutting with any instruments but not tattooing and body piercing. Our second aim was to determine whether there were any differences in factors associated with self-cutting and other self-harm, namely differences in sociodemographic variables, substance use/abuse, depressive symptoms and somatic complaints, family and social relationships and in academic performance.
Method
Participants
The participants were cohorts of 13- to 18-year-old adolescents who were attending school in Kuopio, a city in Eastern Finland with approximately 90,000 inhabitants. Permission was obtained in advance from the headmasters of the schools in which the study was performed. The ethical committee of Kuopio University Hospital and the University of Kuopio granted permission for the study.
The study focused on comprehensive, secondary, and secondary modern schools. Two special schools were excluded from the study by recommendation of their headmasters, as the questionnaires were considered too complicated for their disabled students. Prior to participating in the study, a written informed consent was requested from the adolescents and from the parents of those aged less than 15 years.
The research data were collected by structured self-rating questionnaires that the participants completed during class periods at school. Half of upper secondary schools (n = 8), two of ten secondary schools and one of three secondary modern schools wanted to administer the study by themselves. These students represented 33% of the study subjects and the response rate among them was 76.8% (χ 2 = 99,99, df = 1, P < 0.001 as compared to the other schools). In these cases the researcher informed the teachers about the study and gave them instructions on how to perform it. In the other schools a researcher administered the test (67% of study subjects; response rate 61.5%). The feasibility of the questionnaires was tested in a pilot study performed in one class (n = 27). The questionnaires included questions of a very personal nature that were possibly even distressing to some of the participants. For this reason they were accompanied by a letter that included the offer of contacting a psychiatric facility. Thus, the study may have served for some of the youths as a channel for early treatment. Nevertheless, the number of adolescents who contacted health services after the study is not known, because we recommended contact with a low-level walk-in clinic offering psychiatric services for adolescents as a part of primary health care.
At the time of the study there were 7,087 (3,554 boys and 3,533 girls) 13- to 18-year-old adolescents studying in Kuopio. The parents of 666 adolescents refused to allow their children (less than 15 years of age) to participate, which left an eligible sample of 6,421 adolescents and a response rate of 65.5% (n = 4,214). Nine questionnaires were excluded due to missing data. The final sample (n = 4,205) included 486 boys and 557 girls in the age group under 15 years of age with response rates of 69.3 and 78.8%, respectively (P < 0.01). Among those aged 15 years or more there were 1,467 male and 1,695 female respondents with response rates 58.2 and 68.0%, respectively (P < 0.001). In both age groups girls responded significantly more often than boys.
In this paper we compared the participants with no history of self-cutting with those who reported currently cutting themselves and those having a history of self-cutting. Moreover, we compared those participants who reported no other self-harming behaviour with those having a history of other self-harming behaviour.
Measures
Competence, adaptive functioning a problems
The background factors, academic performance, social relationships and somatic complaints of the adolescents were determined by questions included in a standardized self-rated questionnaire, the youth self-report for ages 11–18 years (YSR) [1]. The background variables were: gender, age, parents’ marital status (living together/not living together). Social relationships were asked about with the questions: How many friends do you have? (none, 1, 2–3, 4 or more); How many times a week do you do things with any friends outside of your regular school hours? (less than 1, 1 or 2, 3 or more); Compared to others of your age, how well do you get along with your brother(s) and sister(s) (I have no brothers or sisters), with other kids, and with your parents (1 = worse; 2 = average; 3 = better)? School performance was examined with the question: How is your performance in academic subjects: reading, your mother language (all Finnish), history or social studies, arithmetic and mathematics, biology, chemistry, physics and sports (1 = failing; 2 = below average; 3 = average; 4 = above average)?
Somatic symptoms and aggressive behaviour were inquired using several items with the question: “How well do these items describe you now or within the past 6 months?” Items for somatic symptoms were headaches, nausea, feeling sick, rashes or other skin problems, stomach aches, aches or pains (not stomach or headaches) and vomiting. The presence of aggressive behaviour was screened with two items: “attacks others” and “breaks things”. All these items had the following alternative responses: 1 = not true, 2 = sometimes true, 3 = very often true. Sometimes true and very often true were recoded to indicate the presence of somatic symptoms or aggressive behaviour.
Self-cutting and self-harm
The questionnaire about self-cutting was based on the qualitative study of Rissanen [18], in which Finnish adolescents provided written descriptions in their own words of their self-cutting (n = 70). The questions used were: Have you ever cut yourself (1 = yes; 2 = never)? Do you currently cut yourself (1 = yes; 2 = no)? When have you last cut yourself? A person can consistently harm him/herself, for example, by taking an overdose of medicine or other drugs. Self-cutting is one way to harm oneself. Now we are asking you, have you ever engaged in any kind of self-harming behaviour other than self-cutting (1 = yes; 2 = never)?
Alcohol and substance use/abuse
The use of alcohol and other drugs was mapped in this study with questions that had earlier been used in studies on school-aged people [15]. The questions were related to: smoking (1 = never; 2 = yes, occasionally; 3 = yes, daily); the abuse of legal drugs to get intoxicated with or without alcohol (1 = never; 2 = yes, monthly; 3 = yes, weekly; 4 = yes, more often; 5 = yes, but not so often); sniffing (glue, gas) (1 = never; 2 = yes, monthly; 3 = yes, weekly; 4 = yes, more often; 5 = yes, but not so often); use of cannabis, use of intravenous drugs (1 = never; 2 = yes); driving under the influence of alcohol (1 = never; 2 = yes) and alcohol use: “How often have you consumed an alcoholic beverage on average during the past 6 months?” (0 = not at all; 1 = once a month or less; 2 = 2–4 times/month; 3 = 2–3 times/week; 4 = 4 times a week or more).
Depression
Depressive symptoms were examined by using the 21-item beck depression inventory (BDI) [3]. The BDI includes four-step questions and the total score of the scale can vary between 0 and 63. Scores were analyzed as a continuous variable.
Statistics
The data were analyzed using SPSS analytical software (version 14.0). The differences between the groups of self-cutting or self-harming participants and others were evaluated with the Pearson χ 2 test for categorical variables, and with the Mann–Whitney U test for continuous variables. In addition, univariate and multivariate odds ratios with 95% confidence intervals were calculated. Missing values were imputed with estimated values that were calculated using linear regression. In general, a P-value of <0.05 was considered statistically significant in the analyses.
Results
Prevalence of self-cutting and other self-harm
The study sample included 1,953 boys and 2,252 girls aged 13–18 years with no statistically significant difference in age distribution between them (χ 2 = 1.73, df = 5, P = 0.89). Girls had higher BDI scores than boys (mean 5.4, SD 6.4 vs. 2.3, SD 3.7, Mann–Whitney U test, P < 0.001).
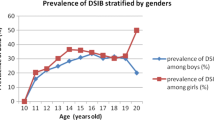
In the sample, the life-time prevalence of self-cutting was 11.5% (95% CI 10.8–12.3), the frequency of current self-cutting 1.8% (95% CI 1.5–2.1) and the life-time prevalence of other self-harm 10.2% (95% CI 9.5–10.9). Both the life-time prevalence (16.5% vs. 6.6%, χ 2 = 170.86, df = 1, P < 0.0005) and frequency of current self-cutting (2.7% vs. 0.9%, χ 2 = 31.44, df = 1, P < 0.0005) were significantly higher among girls than boys. Nevertheless, there was no gender difference in the prevalence of other self-harm (10.1% vs. 10.2%, respectively). Other self-harm was more common among both those who had a history of self-cutting (15.8% vs. 9.4%, χ 2 = 32.07, df = 1, P < 0.0005) and those who reported current self-cutting (25.4% vs. 9.9%, χ 2 = 32.63, df = 1, P < 0.0005) than among the others.
When examined by age, the risk of having a history of self-cutting was higher among girls than among boys in all age-groups. Moreover, the risk of current self-cutting was also higher among girls, except those participants who were 14 or 18 years old, among whom no gender difference was found. The risk of lifetime history of other self-harm was mostly the same in boys as in girls. The only statistically significant differences were found among those who were 16 (girls < boys) or 18 years old (girls > boys; Table 1).
Background factors
Frequent alcohol consumption, legal drug abuse, sniffing and cannabis use were all associated with an increased risk of past and current self-cutting and other self-harm. Daily smoking weakly associated with an increased risk of a history of self-cutting and the use of other illegal drugs with a history of self-cutting and other self-harm (Table 2).
There were only minor differences in psychosocial and behavioural risk factors for a history of and current self-cutting. The highest risk associated with having no friends. Parents living together was a protective factor. These two factors did not associate with the risk of other self-harm (Table 3).
Multivariate analyses
Finally, we conducted several multivariate logistic regression analyses to identify the factors that were independently associated with self-cutting and other self-harm. Because some variables correlated strongly with each other the following new variables were recoded: poor family relationships (yes/no), social isolation (yes/no), legal/illegal drug use/abuse (yes/no), poor school performance (yes/no), somatic symptoms (yes/no) and aggressive behaviour (yes/no). A history of self-cutting associated with all adverse background variables used in this study. Moreover, female gender was also a risk factor. Parents living together was an independent protective factor. In contrast, there was no gender difference in the risk of other self-harm. Independent risk factors were depressive mood, somatic complaints, drug abuse, poor school performance and poor family relationships. No protective factor was for other self-harm (Table 4).
Discussion
This study among Finnish adolescents aged 13–18 years revealed that the life-time prevalence of self-cutting was 11.4 % and the life-time prevalence of other self-harm was 10%. The figures are quite high compared to results from England and Australia (6–7%), but are in accordance with the results of an earlier meta-analysis [5]. However, it should be noted that our results are not entirely comparable with the figures presented by Evans and co-workers, because they also included other kinds of self-harming behaviour. The frequency of current self-cutting among 13- to 18-year-old Finnish adolescents was 1.9%, being most prevalent among 13- to 16-year-old girls (3.0–4.5%). A history of self-cutting was also most common among 16-year-old girls (21.1%).
The prevalence of current self-cutting among girls was quite similar to that in the studies of Rodman et al. [19] and De Leo and Heller [4], who reported the prevalence of self-cutting during the preceding year to be 3.6% among 15- to 16-year-old adolescents.
As this is the first Finnish study on adolescent self-cutting, no conclusion can be drawn about temporal changes. Interestingly, Internet pages for adolescents about self-cutting are currently also available in Finland. These pages have been created as a means of support, but they can also have stimulating effects on those adolescents who are susceptible to this type of behaviour. This hypothesis has been indirectly supported by the study of Taiminen et al. [22], which demonstrated that this behaviour was contagious among inpatient adolescents. Furthermore, international comparisons between the results of other studies is challenging, because different definitions have been used to describe self-harm, self-mutilation and self-cutting [5, 16, 21].
According to our final multivariate analysis, female gender was a risk factor for self-cutting. Moreover, self-cutting associated with a very wide range of adverse psychosocial variables such as poor social relationships, aggressive behaviour and depressive and somatic symptoms. Other studies have shown that depressive symptoms are more common among girls than boys [12]. Recent statistics reflect that deaths from suicides among 10- to 19-year-old girls in Nordic countries have followed an increasing trend (In Finland 1.9/100,000 in 1995 and 4.7/100,000 in 2005; 13). It has been suggested that girls express through self-injurious behaviour their inability to achieve psychological homeostasis in more adaptive ways. Self-cutting is used as a self-therapeutic method for tension relief [24].
The risk of other self-harming behaviour associated with the presence of substance abuse. The relationship between substance abuse and self-harm can be two-fold. Firstly, substance abuse can itself be an act of self-harming behaviour. This statement is supported by many studies showing that substance abuse is associated with other problems in an adolescent’s life, such as poor social skills, poor school achievements, psychosomatic symptoms and a negative self-image [2, 15]. Secondly, a drug-induced state may trigger self-harming behaviour, because it impairs pain perception and judgment, lowers impulse control and may stimulate, for example, aggressive and depressive fantasies.
Our study demonstrated that self-cutting and other self-harm are overlapping phenomena, but there are also differences. Both are associated with smoking, frequent use of alcohol, the abuse of legal and illegal drugs and a poor school performance, especially in mathematics. The frequency of abuse of legal drugs was two-fold higher (20%) among those adolescents who reported current self-cutting compared to those who had a history of self-harm (9.0%). Nevertheless, both these figures are significantly higher than those found in the general adolescent population in Finland (4%) [13].
Study strengths and limitations
The major strength of this study is the clear differentiation between self-cutting and other self-harm in the questionnaire completed by the adolescents, which increases the validity of our findings and makes it possible to draw conclusions about the phenomenon of self-cutting. The study population was large and representative of Finnish adolescents and the response rate was over 65%. The results can be generalized within Finland, but generalization to other countries must be done with caution because of cultural differences. One limitation of the sample is that it did not include those adolescents who were absent from school. They are likely to be at increased risk of self-harming behaviour and so the prevalence figures could be even higher.
In terms of the limitations, the use of additional informants could have yielded more information, but we assume that the inclusion of several questions concerning self-cutting in the questionnaire presented to the adolescents in their classrooms and the advice given by the researcher increase the validity of the adolescents’ responses. Adolescents less than 15 years of age needed written consent from parents prior to participating in this study, which could have led to an underestimation of self-cutting and other self-harm in this age group. Parents who have no worries about their children may more readily give consent in this kind of study.
Clinical implications
Our results demonstrate that self-cutting and other self-harming behaviour are quite common among adolescents. Both are associated with other wide-ranging problems in the adolescents’ lives, but despite their common features these phenomena also differ from each other. Our study suggests that girls who have depressive and somatic symptoms, live with separated/divorced parents and have poor family relationships are at risk of self-cutting. Other self-harming behaviour is associated with illegally used drugs, poor family relationships and poor school performance. Both groups need support and perhaps also some therapeutic interventions for healthy development. It is known that both groups of adolescents are problematic to approach. Thus, more studies concerning the separate characteristics of self-cutting and self-harm are needed to develop appropriate preventive and therapeutic interventions. Adolescents’ own opinions and wishes about the support and help they need should be investigated. Teachers, school nurses and general practitioners should be conscious that even non-dangerous and superficial self-cutting may be a part of complex psychosocial problems that may severely threaten healthy psychic maturation during the important years of adolescent development.
References
Achenbach TM, Rescorla LA (2001) Manual for the ASEBA school-age forms & profiles. University of Vermount, Research Center for Children, Youth & Families, Burlington, VT
Arata CM, Stafford J, Tims MS (2003) High school drinking and its consequences. Adolescence 38:567–579
Beck A, Steer RA, Garbin MC (1988). Psychometric properties of the beck depression inventory: twenty-five years evolution. Clin Psychol Rev 8:77–100
De Leo D, Heller TS (2004) Who are the kids who self-harm? An Australian self-report school survey. MJA 181:140–144
Evans E, Hawton K, Rodman K, Deeks J (2005) The prevalence of suicidal phenomena in adolescents: a systematic review of population-based studies. Suicide Life Threat Behav 35:239–250
Favazza A (1989) Why patients mutilate themselves. Hosp Community Psychiatry 40:137–144
Favazza AR (1996) Bodies under siege. self-mutilation and body modifications in culture and psychiatry, 2nd edn. The John Hopkins University Press, Baltimore
Fortune SA, Hawton K (2005) Deliberate harm in children and adolescents: a research update. Curr Opin Psychiatry 18:401–406
Ghaziuddin M, Tsai L, Naylor M, Ghaziuddin N (1992) Mood disorders in a group of self-cutting adolescents. Acta Paedopsychiatr 55:103–105
Haavisto A, Sourander A, Multimäki P, Parkkola K, Santalahti P, Helenius H, Nikolakaros G, Moilanen I, Kumpulainen K, Piha J, Aronen E, Puura K, Linna SL, Almqvist F (2005) Factors associated with ideation and acts of deliberate self-harm among 18-year-old boys. Soc Psychiatr Epidemiol 40:912–921
Haw C, Hawton K, Houston K, Townsend E (2001) Psychiatric and personality disorders in deliberate self-harm patients. Br J Psychiatry 178:48–54
Hawton K, Rodham K, Evans E, Weatherall R (2002) Deliberate self harm in adolescents: self report survey in school in England. BMJ 325:1207–1211
Hibell B, Andersson B, Bjarnasson T, Ahlstrom S, Balakireva O, Morgan M (2004) The ESPAD report 2003: alcohol and other drug use among students in 35 European countries, Swedish Council for information on alcohol and other drugs, CAN; Council of Europe, co-operation group to combat drug abuse and illicit trafficking in drugs (Pompidou group)
Klonsky ED, Oltmanns TF, Turkheimer E (2003) Deliberate self-harm in nonclinical population: prevalence and psychological correlates. Am J Psychiatry 160:1501–1508
Laukkanen E, Shemeikka S, Viinamäki H, Pölkki P, Lehtonen J (2001) Heavy drinking is associated with more severe psychosocial dysfunction among girls than boys in Finland. J Adolesc Health 28:270–277
McAllister M (2003) Multiple meanings of self-harm. A critical review. Int J Ment Health Nurs 12:177–185
Nordisk Medicinal Statistisk Komité (2007) Health Statistics in the Nordic Countries Schults information, Kopenhagen
Rissanen ML (2003) Nuoren itsensä viiltäminen ja polttaminen—mitä nuoret itse siitä kertovat (self-cutting and burning among adolescents—what adolescents tell by themselves). Scolarly thesis. University of Kuopio, Department of Nursing Science, Kuopio
Rodham K, Hawton K, Evans E (2005) Deliberate self-harm in adolescents: the importance of gender. Psychiatr Times 22:36–40
Ross S, Health N (2002) A study of the frequency of self-mutilation in a community sample of adolescents. J Youth Adolesc 31:61–77
Skegg K (2005) Self-harm. Lancet 366:1471–1483
Taiminen T, Kallio-Soukainen K, Nokso-Koivisto H, Kaljonen A, Kelenius H (1998) Contagion of deliberate self-harm among adolescent inpatients. J Am Acad Child Adolesc Psychiatry 37:211–217
Tick NT, Van der Ende J, Verhulst FC (2008) Ten-year trends in self-reported emotional and behavioural problems of Dutch adolescents. Soc Psychiatry Psychiatr Epidemiol Published online: 9 February
Zila LM, Kiselica MS (2001) Understanding and counseling self-mutilation in female adolescents and young adults. J Couns Dev 79:46–52
Zlotnick C, Mattia JI, Zimmerman M (1999) Clinical correlates of self-mutilation in a sample of general psychiatric patients. J Nerv Ment Dis 187:296–301
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Laukkanen, E., Rissanen, ML., Honkalampi, K. et al. The prevalence of self-cutting and other self-harm among 13- to 18-year-old Finnish adolescents. Soc Psychiat Epidemiol 44, 23–28 (2009). https://doi.org/10.1007/s00127-008-0398-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-008-0398-x