Abstract
Objective
Research on status inconsistency (SI) and its impact on mental health has been dormant for many years. This study tested the association between SI and emotional distress, anxiety and mood disorders.
Methods
Data were gathered from the Israel-based component of the World Mental Health Survey (n = 4,859). SI was defined by the combination of high education (13+ years) with low income (1st decile). Mood and anxiety disorders were diagnosed with the composite international diagnostic instrument (CIDI), and emotional distress was measured with the 12-item general health questionnaire (GHQ-12).
Results
Multivariate analysis showed increased risk for mood or anxiety disorders among SI subjects (n = 231), odds ratio (OR) = 1.75, 95% confidence interval (95% CI) 1.13–2.63. The estimate was slightly attenuated when marital status was added to the model (OR = 1.55, 95% CI 1.0–2.39). SI subjects showed higher GHQ-12 scores.
Conclusion
SI, which can disrupt an individual’s sense of coherence, is associated, although not causally, with increased 12 month prevalence rates for mood or anxiety disorders and with higher psychological distress.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Individuals strive to achieve coherence in their lives. Its disruption might lead to stress and, ultimately, to challenges to the individuals’ health [2]. Status inconsistency (SI) is an example of such a disruption, resulting from the discrepant positions that individuals hold in different domains of the social structure. This anomaly constitutes a departure from accepted patterns in society, whereby individuals obtain rewards commensurate with their education [23].
As early as 1954, Lenski [15] argued that persons with SI may be affected by psychological stress. Years later, Dressler [4] empirically showed that SI generated symptoms of emotional distress and physical illness. Although not a fully dormant research subject, status inconsistency was a subject seldom investigated in recent years [except for: 5, 6, 21, 22]. Recently, it reemerged in a report on an increased risk for cardiovascular disease among subjects with SI [19]. Conceivably, the many methodological critiques leveled at studies of SI, including the operational definitions that were applied, the control over status variables, and the indicators of status that were included [3, 8, 9, 24], seemed to have discouraged research on the subject.
In contrast to the studies on the impact of SI on physical health, its impact on mental health has remained largely unexplored. This has been the case even in Israel, where psychiatric epidemiology has thrived [7]. The single study conducted locally dates four decades ago when Abramson [1] reported the effect of SI on emotional health. That survey, conducted in a Jerusalem neighborhood settled by old (19%) and new immigrants (81%), measured the effect of the discrepancy between educational level and occupation. The dependant variable was the Cornell Medical Index, a 195-item questionnaire that measures emotional distress. Among the new immigrants Abramson found that distress was associated with a discrepancy between educational and occupational status [1]. Curiously, although in recent years Israel has received large numbers of immigrants who are at risk for SI, research in this area had not been resumed.
SI raises the question whether going to school pays off financially. Almost invariably, people think that this should be the case. Indeed, there is a general expectation in open market societies for economic success based on educational attainment. Israel is no exception to this view. The objective of this study was to assess the associations between SI, defined here as the discrepancy between high education and low income, and emotional distress, anxiety and mood disorders. We hypothesized that such a type of SI generates psychopathology. To test this hypothesis we used data collected in the Israel national health survey (INHS), the Israeli component of the World Mental Health Survey.
Methods and procedures
The INHS [16] study design has been described previously [14]. The sample of non-institutionalized de jure residents aged 21 and over was extracted from the Population Register. It was designed to reflect the distribution of selected gender-age groups in the general population (Arab–Israelis; post-1990 immigrants from the former USSR.; and other Jewish-Israelis, both local and foreign born). The sample was weighted back to the total population to compensate for unequal selection probabilities resulting from disproportionate stratification, clustering effects and non-response. Those weights were adjusted to conform to known population totals taken from reliable central bureau of statistics (CBS) sources. Face-to-face interviews at the respondents’ homes were conducted from May 2003 to April 2004, in Arabic, Hebrew or Russian. The interviews were administered using laptop computer-assisted personal interview (CAPI) methods by professional survey interviewers trained and supervised by the CBS. A letter explaining the purpose of the survey and the respondent’s rights was sent prior to the first contact. Upon making in-person contact with the sampled respondent, the interviewer reiterated the purpose of the survey and obtained verbal informed consent. Interviews took on average 60 min. There were no replacements. A Human Subjects Committee approved the study. The overall response rate was 73% (88% among Arab-Israelis and 71% among Jewish–Israelis), totaling 4,859 completed interviews. Of these, 2,849 (59%) respondents reported they have been employed for the 30 days prior to the interview, thus meeting the inclusion criterion of personal income.
Study variables
Status inconsistency
SI was defined in terms of the discrepancy between years of education and personal income. Subjects with 13 or more years of academic or technical education, and a personal monthly income of 3,000 NIS (US$ 625) or less were defined as being in a SI position. Education was chosen since it opens the path to economical opportunities. This is particularly the case in Israel with regard to the achievement of an academic level of education. The relative high number of respondents meeting this level of education (56%) indicated that the group targeted for inquiry was not of marginal representation in society. The income level was chosen based on CBS’s criteria in the years 2003–2004, when the field operation took place, that an income of 2,958 NIS or less represented the lowest (1st) decile of the income distribution [21]. The comparison group included all the respondents with personal income.
Orthodox Jewish–Israelis were not included in the analysis since they represent a unique group within the higher educational cluster. Although they achieve many years of education, their cycle of religious studies rarely provides skills that enable gainful employment.
Socio-demographic information
A questionnaire on socio-demographic variables (e.g., age, gender, country of origin, immigration, ethnic-national group, marital and employment status, education, income) was administered to all respondents.
Diagnostic assessment
The Composite International Diagnostic Instrument (CIDI), a fully-structured diagnostic instrument which assesses lifetime and recent prevalence of selected psychiatric disorders according to both the ICD-10 and the DSM-IV classification systems, was utilized in the INHS [14, 16]. We assessed the following disorders: 1. anxiety disorders, including panic disorder, generalized anxiety disorder (GAD), agoraphobia without panic disorder, and post-traumatic stress disorder (PTSD); and 2. mood disorders, including major depressive disorder, dysthymia, bipolar I and II disorders. For each disorder, a screening questionnaire was administered. All participants answering positively to a specific screening item were asked the relevant diagnostic questions. Prevalence estimates of mental disorders were determined by whether respondents’ symptoms met the diagnostic criteria for DSM-IV disorder during the 12-months period prior to the interview. Organic exclusion criteria were taken into account in determining DSM-IV diagnoses. A combined measure of any mood or anxiety disorder (AMAD) in the past 12 months was defined when at least one disorder was present.
Retrospective age-of-onset replies were obtained using the direct question: “How old were you the first time you had the symptoms?” Respondents who failed to remember when the symptoms begun were given anchor points, such age they started school, before their teens or later. Analysis of the association between childhood abuse and age of onset of the disorder was restricted to subjects whose age of onset was equal or later than that of abuse.
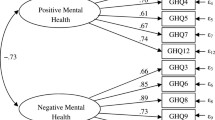
The interview schedule also included the 12-item general health questionnaire (GHQ-12). This scale screens for psychiatric disorder and is a measure of emotional distress. Scores range between 12 and 48, where higher scores indicate increased distress. The GHQ-12 had previously been used in Israel [20]. The internal consistency of the instrument, as measured by Cronbach’s α, was 0.88 for the entire sample.
Analysis
Frequency distributions of the demographic data of SI subjects and the comparison group were calculated. The associations between SI and demographic data were analyzed using χ 2 tests. Twelve month prevalence rates were estimated for AMAD and mean scores for GHQ-12. The age of (first) onset of AMAD was identified to establish the temporal relationship between those disorders and SI. Logistic regression analysis [11] was used to assess the association between SI and potential confounder variables and AMAD. Odds ratios (ORs) and 95% confidence intervals (CIs) were computed. Following the identification of significant variables of the unadjusted models, a stepwise logistic regression model was applied. A t test for independent samples compared GHQ-12 scores between the SI group and its counterpart. In case of unequal variances, the Satterthwaite method was used, allowing for the calculation of an approximate t test to be calculated. Interactions between SI and demographic variables were tested using two-way ANOVA models. As SI in this study was based on a combination of low income and high education we wanted to control for the possible effects of the personal income or education. Therefore, we have further analyzed these factors as follows: SI subjects were compared with subjects of the comparison group with: 1. a similar income levels (monthly income less than 3,000 NIS); or 2. a similar education level (13 years of schooling and above). Association tests were performed using χ 2 (AMAD) and t tests (GHQ). All statistical analyses were performed using SAS 9.1.3 (SAS Inc.).
Results
Socio-demographic characteristics and respective comparison group are shown in Table 1.
Socio-demographic information
Two hundred and thirty one subjects were identified in a SI position (8.5%), and 2,498 (91.5%) in the comparison group. The group of SI subjects included greater proportion of women; younger and older subjects; unmarried; and immigrants than the counterpart. By design, SI subjects had higher education than their counterparts.
Psychiatric morbidity
Higher prevalence rate of AMAD (12.1%) was observed in the SI than in the comparison group (7.4%). This was supported by an unadjusted logistic regression model which indicated a significant association between SI and AMAD (Table 2). Additional models showed significant associations between gender, age, and marital status and AMAD (Table 2). A stepwise logistic regression analysis for the prediction of AMAD indicated the significant effects of marital status and AMAD, while gender and age were not included in the model (Table 3). However, when an additional model which forced the adjustment according to gender and age was performed, the association between SI and AMAD was attenuated (OR = 1.45, 95% CI 0.93–2.25) and failed to reach significance (P = 0.1).
The associations of marital status with SI and AMAD were further analyzed. The greater proportion of singles and divorced/widowers (taken together as unmarried) among the SI subjects, as well as the higher proportion of AMAD among the unmarried (12.0%) compared to married subjects (5.9%), suggested that greater proportion of AMAD would be observed among unmarried SI subjects but not among the married. Indeed, the proportion of AMAD among unmarried SI subjects (17.1%) tended to be higher than in unmarried subjects with no-SI (11.2%) (χ 2 = 3.46, df = 1, P = 0.06), while a negligent difference was observed among married subjects (SI 6.5%; comparison 5.8%).
The SI group showed higher GHQ-12 scores (20.0 ± 5.9) (mean ± SD) than the comparison group (17.6 ± 4.9), (t = 5.94, df = 258, P < 0.001). The effects of SI on GHQ-12 scores were further analyzed using two-way ANOVA models where gender, age, immigration status, population group, and marital status were added to SI. A significant interaction with SI was observed with age group (F = 3.36, df = 2, 2688, P = 0.03). This effect was due to an increase in GHQ-12 scores with age among SI subjects (21–34, 19.2; 35–64, 20.6; 65+, 21.5), while a slight decrease in the comparison group (21–34, 17.6; 35–64, 17.6; 65+, 17.1). No significant interactions were found with other demographic variables (all P values were >0.1).
The data were further analyzed to control for the simple effects of income and education: 1. Subjects with similar income to SI subjects (n = 240) were identified in the comparison group. The prevalence rate of AMAD in the SI group (12.1%) was higher than in the latter group (7.1%) (χ 2 = 3.46, df = 1, P = 0.06). In addition, SI subjects showed higher GHQ-12 scores (20.0 ± 5.9) than subjects with similar income (16.8 ± 4.8) (t = 5.03, df = 439, P < 0.001). 2. Subjects with similar education level (n = 1,285) were identified in the comparison group. As above, SI group showed higher prevalence rate of AMAD (12.1% vs. 5.6%) (χ 2 = 13.50, df = 1, P < 0.001), and higher GHQ-12 scores (20.0 ± 5.9 vs. 17.0 ± 4.4) (t = 7.30, df = 276, P < 0.001) compared to their counterparts with similar education level.
Discussion
This study explored the association between SI and emotional distress, anxiety and mood disorders, and the temporal relationship with the latter two. Individuals in a SI position had both higher 12-month prevalence rate of AMAD and higher distress scores than their counterparts. The association between SI and AMAD was slightly attenuated when marital status was included in the adjusted model. Higher proportion of both SI and AMAD were noted among unmarried compared to married subjects. Indeed, an interaction between SI and marital status was observed with regard to AMAD. This marital effect could result from both economical and emotional factors. Conceivably, among married subjects the negative effect of low personal income of SI subjects may be buffered by the spouse’s income. In contrast, unmarried subject have to negotiate the challenges posed by low income on their own. This interpretation is supported by the higher percentage of women among SI subjects, 67%, compared to 42% in the comparison group. Also, the fact that lower risk of AMAD was seen among married subjects could be attributed to the better support network of these subjects compared to subjects who are alone. This explanation suggests that although subjects with SI are at risk for emotional distress, this effect could be down-regulated by the support from a significant other.
The effect of SI on the level of symptoms during the last 30 days (GHQ-12) parallels some of the pattern seen regarding AMAD. First, SI subjects showed greater distress than the comparison group. Second, married subjects showed lower level of symptoms compared to unmarried subjects (results not presented). However, this pattern was not supported by an interaction between SI and marital status. Thus, with regard to emotional distress, the effect of SI was confounded by age only.
Although not reported here, we analyzed the role of unemployment on subjects with 13 or more years of education. Interestingly, while among the unemployed subjects the levels of AMAD were higher than in the comparison group, there was no difference between SI individuals and their counterparts in the likelihood for AMAD. Moreover, SI subjects showed lower distress scores compared to the control group. Conceivably, this group of SI subjects may have opted out of the work market and thus rely on other sources of income. Also, SI subjects could have intentionally chosen not to work and thus forestall the frustration and hardships caused by unemployment.
This study did not confirm our hypothesis that psychiatric morbidity could be imputed to the effects of SI. Support for this social causation interpretation would have been established if the age in which both completed education and a compatible income retribution were achieved (in Israel, around 30 years) had been followed by the (first) onset of the disorder. For most SI subjects (80%) the onset of the mood or anxiety disorder (positive AMAD) was before the age of 30. Therefore, these data do not support the assumption that AMAD resulted from SI.
There are two important limitations in this study. First, a selection bias may have been present due to non-response. A recent analysis of the causes for non-participation [17] showed that subjects with low income cooperated less in their epidemiological study compared to subjects with high income. In addition, they found greater, but non-significant, tendency to refuse among respondents diagnosed with mood disorders compared to healthy subjects. Thus, it could be argued that the effect of non-response would have rather increased the observed association between SI and AMAD. Second, the definition of SI we used was based on the respondents’ report on their income and education, where the reliability of the former variable is always suspected. The INHS was conducted by a governmental institution, thus the interviewer could have been regarded as a possible direct or indirect representative of the tax authorities. If that was the case, the reliability of the item could have been compromised. However, it is highly doubtful that an individual in a higher educational bracket would have lowered the reported income to the lowest decile. We thus believe that the strengths of this study outweigh its possible limitations.
To conclude, the findings of the current inquiry agree with previous reports that ascertained an association between SI and mental health [1, 4, 10, 12, 13, 18]. However, it failed to prove that this association results from the stressful effect of SI through the disruption of the subjective sense of coherence [2]. With regard to intervention, this study did build a strong “case for action”: to reduce the impact of psychopathology in a population group that in spite of the ability to reach higher education is close to poverty level.
References
Abramson JH (1966) Emotional disorder, status inconsistency and migration. Milbank Mem Fund Q 44:23–47
Antonovsky A (1984) The sense of coherence as a determinant of health. In: Matarazzo JD (eds) Behavioral health: a handbook of health enhancement and disease prevention. Wiley, New York, pp 114–129
Blalock HM (1966) The identification problem and theory building: the case of status inconsistency. Am Sociol Rev 31:52–61
Dressler WW (1988) Social consistency and psychological distress. J Health Soc Behav 29:79–91
Dressler WW, Evans P, Gray DJ (1992) Status incongruence and serum cholesterol in an English general practice. Soc Sci Med 34:757–762
Faresjö T, Svärdsudd K, Tibblin G (1997) The concept of status incongruence revisited: a 22-year follow-up of mortality for middle-aged men. Scand J Soc Med 25:28–32
Gross R (2007) Psychiatric epidemiology in Israel, 2007: reflections on the Israel national health survey. Isr J Psychiatry Relat Sci 44:152–157
Hartman M (1974) On the definition of status inconsistency. Am J Sociol 80:706–721
Hope K (1975) Models of status inconsistency and social mobility effects. Am Sociol Rev 40:322–343
Hornung CA (1977) Social status, status inconsistency and psychological stress. Am Sociol Rev 42:623–638
Hosmer DW, Lemeshow S (1989) Applied logistic regression. Wiley, New York
Jackson EF (1962) Status consistency and symptoms of stress. Am Sociol Rev 27:469–480
Kasl SV, Cobb S (1971) Physical and mental health correlates of status incongruence. Soc Psychiatry Psychiatr Epidemiol 6:1–10
Kessler RC, Ustun TB (2004) The world mental health (WMH) survey initiative version of the world health organization (WHO) composite international diagnostic interview (CIDI). Int J Methods Psychiatr Res 13:93–121
Lenski GE (1954) Status crystallization: a non-vertical dimension of social status. Am Sociol Rev 19:405–413
Levinson D, Paltiel A, Nir M, Makovki T (2007) The Israel national health survey: issues and methods. Isr J Psychiatry Relat Sci 144:85–93
Lundberg I, Thakker KD, Hällström T, Forsell Y (2005) Determinants of non-participation, and the effects of non-participation on potential cause-effect relationships, in the part study on mental disorders. Soc Psychiatry Psychiatr Epidemiol 40:475–483
Meile RL, Haese PN (1969) Social status, status incongruence and symptoms of stress. J Health Soc Behav 10:237–244
Peter R, Gässler H, Geyer S (2007) Socioeconomic status, status inconsistency and risk of ischaemic heart disease: a prospective study among members of a statutory health insurance company. J Epidemiol Community Health 61:605–611
Shemesh AA, Levav I, Blumstein T, Nobikov I (2004) A community study on emotional distress among the elderly in Israel. Isr J Psychiatry Relat Sci 41:174–183
Statistical abstract of Israel (2005) Table 5.27. Central Bureau of Statistics, Jerusalem
Siegrist J, Peter R, Junge A, Cremer P, Seidel D (1990) Low status control, high effort at work and ischemic heart disease: prospective evidence from blue-collar men. Soc Sci Med 31:1127–1134
Stehr N (1968) Status consistency: the theoretical concept and its empirical referent. Pac Sociol Rev 11:95–99
Whitt HP (1983) Status inconsistency: a body of negative evidence or a statistical artifact? Soc Forces 62:201–233
Acknowldgments
The national health survey was funded by the Ministry of Health with additional support from the Israel National Institute for Health Policy and Health Services Research and the National Insurance Institute of Israel. The views and opinions expressed in this article are those of the authors and they neither represent the views of the sponsoring organizations nor of the Government. The Israel Health Survey was carried out in conjunction with the World Health Organization/World Mental Health (WMH) Survey Initiative. We thank the staff of the WMH Data Collection and Data Analysis Coordination Centers for assistance with instrumentation, fieldwork and consultation on data analysis. These activities were supported by the National Institute of Mental Health (R01 MH070884), the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, the U.S. Public Health Service (R13-MH066849, R01-MH069864, and R01 DA016558), the Fogarty International Center (FIRCA R03-TW006481), the Pan American Health Organization/World Health Organization, Eli Lilly and Co., Ortho-McNeil Pharmaceutical, Inc., GlaxoSmithKline, and Bristol-Myers Squibb. A complete list of WMH publications can be found at http://www.hcp.med.harvard.edu/wmh/.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gal, G., Kaplan, G., Gross, R. et al. Status inconsistency and common mental disorders in the Israel-based world mental health survey. Soc Psychiat Epidemiol 43, 999–1003 (2008). https://doi.org/10.1007/s00127-008-0393-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-008-0393-2