Abstract
Background
Promotion of physical activity (PA) is at the top of the public health agenda. However, there are few longitudinal studies investigating the relationship between PA and children’s mental health. Therefore, we aimed to investigate the association between self-reported physical activity (PA) and emotional problems 1-year later in a cohort of schoolchildren.
Methods
A total of 1,446 children aged 11–14 years from 39 schools in the North West of England completed a self-report questionnaire in class. Each child reported the total number of sessions of sporting activities (lasting more than 20 min) in which they participated during the previous week, including activities both in school and out of school. This total was averaged for the week in order to determine whether the child was physically active at recommended levels (1 h per day). Childhood emotional problems were measured using the Strengths and Difficulties Questionnaire (SDQ) (self-report) at baseline and 1-year later. Data on potential confounders were also collected by self-report questionnaire at baseline.
Results
In unadjusted analyses, children who, on average, participated in at least 1 h of sporting activity on a daily basis had fewer emotional problems at 1-year follow-up. This attenuated substantially after adjustment for gender (girls were less active but more likely to report emotional problems than boys). After adjustment for additional confounders including emotional problems at baseline, children who met recommended levels for PA had, on average, a score on the emotional problems sub-scale that was 0.29 units lower (−0.29 (95%CI: −0.61, 0.022)) at 1 year follow-up compared to children who did not undertake recommended levels of PA. Children who were physical activity also had higher scores on the hyperactivity sub-scale of the SDQ 1 year later, but there was no evidence to support an association between PA and other behavioural problems.
Conclusions
Children who met recommended levels for PA had fewer emotional problems 1-year later, although the magnitude of this difference was reduced after adjustment for confounders, particularly gender. Future longitudinal studies need to record both PA and emotional problems at more frequent intervals in order to enable us to determine the effect of maintaining a physically active lifestyle on adolescent mental health outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Promotion of physical activity (PA) is at the top of the public health agenda and current recommendations state that children should accumulate (at least) 1 h of moderate intensity activity every day [3, 6, 38]. However, there is little evidence for health benefits of the recommended levels of PA in children and adolescents [32, 40], particularly in terms of mental health [40]. Amongst children, most of the evidence on PA and mental health is based on cross-sectional studies [1, 9, 13, 18, 21, 28–30, 37, 41]. These support an association between more frequent PA and lower levels of depression, emotional problems or psychological distress amongst adolescents [9, 18, 21, 28–30, 37, 41], although some cannot rule out the possibility of no association [13] and one study found that adjustment for confounders substantially attenuated the effect [1]. In many cases, the correlation between PA and depressive symptoms is modest (r = −0.14 to −0.18) [21, 28–30]. Few studies adjusted for confounders, with those that did mostly limiting this to age, gender and socio-economic background [1, 13, 37]. Other important confounders that should be taken into account include adiposity and parental mental health. Three studies report gender differences [10, 24, 31]. Two studies found an association between self- reported PA and depressive symptoms in boys, but not girls [10, 24]; whereas another study found an association amongst girls but not boys [31]. However, none of these studies formally tested an interaction between gender and PA.
Of particular importance, the cross-sectional design of most studies to date limits the conclusions that can be drawn about the temporal nature of the association and there is little published longitudinal evidence to determine this. Lewinsohn et al. [20] examined predictors of depression amongst US high school students (mean age 16 years) over a 1-year interval and found that frequency of PA was not associated with incident depression. Similarly, in a representative sample of UK adolescents, Clark et al. [5] found that exercising for more than twice a week for an hour was not associated with the likelihood of depressive symptoms after 2 years follow-up. In contrast, Motl et al. [25], using latent growth modelling, found that changes in the frequency of PA outside school were inversely associated with changes in depressive symptoms in US students (mean age 13 years) over a 2-year period, although concurrent measurement of depression and PA precludes inference of the direction of causality. More recently, Sagatun et al. [33] found a reduction in emotional problems and peer problems amongst more physically active boys, but no differences in mental health outcomes by levels of physical activity for girls. However, no formal test of interaction on the effect of physical activity by gender was conducted. A recent systematic review examined the evidence for PA reducing or preventing common mental health disorders (specifically, anxiety and depression) amongst children and adolescents [19] and concluded that, whilst there was some evidence for a beneficial effect, there was little robust evidence given the substantial heterogeneity in the populations studied and interventions [19].
Given the paucity of evidence, we therefore aimed to determine whether there was an association between self-reported physical activity and emotional problems 1-year later in a longitudinal study of schoolchildren.
Methods
Description of cohort
Data for this analysis were collected as part of a study of low back pain amongst schoolchildren. Full details are described elsewhere [16, 43]. In brief, 39 schools were randomly selected from all secondary schools in Cheshire and North Derbyshire, UK between November 1999 and July 2000. The schools were from both urban and rural communities and were mixed socio-demographically, including both state funded and independent (fee-paying) schools. Children aged 11–14 years were eligible to take part in the study and each school was asked to select between one and three classes. Parent and child consent was obtained before study participation and permission to approach schools in the study area was obtained from the appropriate regional directors of education.
At baseline, from a total population of approximately 36,000 children, 1,496 children were invited to take part in the study, of whom 1,446 participated (97%). These children completed a self-report questionnaire during class, with a further questionnaire completed 1 year later (November 2000 to July 2001). They were then followed up a second time approximately 4 to 4.5 years after baseline (November 2003 to October 2004) [8].
Childhood behavioural problems
Childhood behavioural problems were measured using the Strengths and Difficulties Questionnaire (SDQ) [11] at baseline and 1-year follow-up. The validity and reliability of the SDQ have been established and reported previously [12]. The SDQ comprises five 5-item subscales covering emotional problems, conduct problems, hyperactivity, peer problems and prosocial behaviour. Each item is rated not true (zero), somewhat true (1) or certainly true (2), giving sub-scale scores from zero to 10. A score for total difficulties (range: 0–40) can be derived from the sum of scores for the first four sub-scales. Higher scores denote more problems except on the prosocial sub-scale, which is reverse scored. A priori, we focussed on the emotional problems sub-scale score.
Measurement of physical activity
Participation in sporting activities (in school and outside of school) was recorded, as part of the baseline questionnaire, using a grid that listed 16 sporting activities (including football, tennis, and swimming). Children were asked to indicate the number of times that they took part in such activities, that lasted for more than 20 min, during the previous week.
The total number of sessions of sporting activity in the previous week was calculated for each child. No data were available on participation in sports on a daily basis. Therefore in order to determine whether children met recommended levels of PA (at least 1 h per day [3, 6, 38]), the total was divided by seven to obtain the average number of sessions of sporting activity per day. Those children who, on average, participated in at least three sessions of sporting activity per day (3 × 20 mins) were regarded as meeting recommended levels of PA. Children were divided into those who did or did not meet recommended daily activity levels for further analyses.
Measurement of confounders
Data on age and gender were available from the baseline self-report questionnaire. Socio-economic deprivation was measured using the Townsend score [39] for the child’s home address. Measurements of each child’s weight and height recorded at the time of the baseline survey were used to calculate the child’s body mass index (BMI) [weight (in kg)/height2 (in m)].
Statistical analysis
All analyses were conducted in Stata Version 9.2 [36].
A random effects linear regression model was used to examine the relationship between baseline PA (defined as whether the child met recommended levels for PA) and emotional problems at follow-up allowing for any clustering by school. Coefficients and their 95% confidence intervals (95% CI) are reported. Univariable models were adjusted for potential confounders: firstly, gender, then baseline emotional problems, followed by age, socio-economic deprivation, and BMI.
Further analyses examined the association between participation in sporting activity and scores on the other sub-scales of the SDQ and total difficulties. In addition, separate analyses were conducted to examine the effect of participating in sporting activity in school and outside of school. For each child, the number of sessions of sporting activity (lasting more than 20 min) taking place in-school or out-of-school was calculated. The association between in-school and out-of-school sports (in units of 20 mins per day) and behavioural problems (for all sub-scales of the SDQ and total difficulties) was examined.
Missing data
Sensitivity analyses were conducted to examine the effect of missing data on the results obtained. Missing data were imputed using the method of multiple imputations by chained equation (MICE) [42] in Stata (ice procedure: 16 March 2007 Version 1.4.0). The imputation model included all potential confounders, school status (state or fee-paying school), sporting activity (number of sessions per week) together with all SDQ sub-scale scores at baseline. When SDQ sub-scale scores were imputed, the imputation model included sub-scale scores available at all time points (baseline, 1-year and 4-year follow-up, as appropriate), together with scores on the other SDQ sub-scales at the same time point. We generated 25 datasets and undertook 10 switching procedures. Analyses were repeated including imputed data and compared with the results of the complete-case analyses.
Results
Description of the cohort
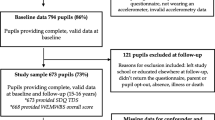
At baseline, just over half the cohort (53.9%; n = 780) were girls, and the mean age was 12.9 years (SD 0.8). Twenty percent of children attended fee-paying schools.
Of the 1,424 children with data on both participation in sporting activity (in-school and out-of-school activities) and emotional problems at baseline, 1,218 (86%) had data on emotional problems at 1-year follow-up. In total, 1,135 children (80%) had complete data including information on confounders.
Participation in sporting activities at baseline
At baseline, on average, children participated in a total of 9 sessions of sporting activities (each lasting more than 20 min) in the previous week (Table 1). Boys were more active than girls (Kruskal–Wallis test: P < 0.001) and older children were less active (Kruskal–Wallis test: P = 0.001). Only 193 children (13.4%) met recommended levels for PA (1 h per day). This figure was substantially higher for boys (n = 142; 21.3%) compared to girls (n = 51; 6.5%) (Chi-squared test: P < 0.001).
Behavioural problems at baseline and 1-year follow-up
The mean scores on the five sub-scales of the SDQ and for total difficulties at both baseline and 1-year follow-up are presented in Table 2. Girls had more emotional problems than boys (t test: P < 0.001). Boys were more likely to have conduct problems and to score lower on prosocial behaviour (t test: P < 0.001). Overall, girls scored higher on total difficulties (t test: baseline P = 0.03; follow-up P < 0.001). There were no other consistent differences by gender.
Sporting activity at baseline and emotional problems at 1-year follow-up
Our a priori focus was in examining the association between PA at baseline and emotional problems at 1-year follow-up. In unadjusted analyses, children who, on average, participated in at least 1 h of sporting activity on a daily basis had fewer emotional problems at 1-year follow-up (Table 3). This effect attenuated substantially after adjustment for both gender and score on the emotional problems sub-scale at baseline. Additional adjustment for other potential confounders (age, deprivation and BMI) had little effect. In the fully adjusted model, children who met recommended levels for PA had, on average, a score on the emotional symptoms sub-scale that was 0.29 units lower at 1-year follow-up compared to children who did not undertake recommended levels of PA. When this difference is related to the mean baseline emotional symptom score, it equates to a 9% reduction in symptoms (coefficient divided by mean baseline symptom score). However, the confidence interval surrounding the estimate just spanned the null (coefficient = −0.29 (95% CI: −0.61, 0.022)). There was no evidence of an interaction by gender (test for interaction, P = 0.79). There was no evidence of an effect of school (data not shown).
Sporting activity at baseline and other behavioural problems at 1-year follow-up
After adjustment for confounders, those children who met recommended levels for PA had higher scores on the hyperactivity sub-scale at 1-year follow-up (Table 3). The increase of 0.39 units on the SDQ hyperactivity sub-scale equates to a 9% increase in average symptoms compared to baseline. There was little evidence to support an association between recommended levels of PA at baseline and scores on the other sub-scales of the SDQ or for total difficulties (Table 3). Again, there was no evidence for an interaction by gender (P values for test for interaction: 0.12–0.81).
When the analyses were repeated using physical activity as a continuous variable (sessions of sporting activity), results were consistent. There was no evidence of any non-linear effects (data not shown).
Sporting activities in- and out- of school and behavioural problems at 1-year follow-up
The association between sporting activities and later behavioural problems may differ according to whether the activity takes place in school or outside of school. Given the small percentage of children who, overall, met recommended levels for daily PA, it was only feasible to examine the association based on the number of sessions of sporting activity either in school or out of school (Table 4). At baseline, on average, children undertook 0.6 sessions (lasting more than 20 min) of sporting activity per day in school (range: 0–5.2) and 0.9 sessions per day out of school (range: 0–6.6).
In Table 4, the coefficients represent the mean (adjusted) change in symptom score at 1-year follow-up for every session of sports participation (lasting at least 20 min). A negative coefficient therefore represents a reduction in problems at follow-up. There was some evidence that participation in out-of-school sporting activities was associated with a larger reduction in emotional problems at 1-year follow-up (regression coefficient = −0.14) compared to participation in in-school sports (regression coefficient = −0.065) (Table 4). However, the confidence intervals surrounding these estimates overlapped considerably. There was little difference between the regression coefficients for in school and out of school sports participation for the other four SDQ sub-scales.
Missing data
Of the 1,424 children with data on emotional problems and participation in sporting activities at baseline, 206 were missing outcome data at 1-year follow-up. Imputing missing data using MICE suggested that those imputed were more likely to have higher scores at follow-up. Sensitivity analyses including imputed data were consistent with the results of the complete-case analyses suggesting that missing data had not biased the results (Table 5).
Discussion
Children who undertake PA at recommended levels (1 h per day) had fewer emotional problems 1-year later, although this effect attenuated markedly after adjustment for gender and baseline symptoms. Whilst the effect was small, it represented a 9% reduction in average symptoms compared to baseline, which may be important from a population perspective. We could not exclude the possibility of no association, or, given the lack of data on parental mental health, residual confounding.
Children who were physically active were also more likely to have higher scores on the hyperactivity sub-scale of the SDQ 1-year later; this finding providing some validation of our measure of physical activity. There was no evidence to support an association between PA and other behavioural problems.
The main strength of this study is the longitudinal design that eliminates the possibility of recall bias and that exposure measurement preceded outcome assessment. Although not a national sample, SDQ scores in this cohort were broadly similar to data representative of the British population (http://www.sdqinfo.com/bba3.pdf) [23], although this North West based cohort had slightly more problems.
Children were asked to report their participation in sporting activities as part of the baseline questionnaire. Ideally, measurement of PA should incorporate information on the frequency, duration and intensity of such activity [17], and should include general daily activities (such as walking to and from school, or playing outdoors). There are concerns about the ability of children to accurately recall PA [14]. However, this particularly relates to younger children who are frequently active in short bursts [2] and are less likely to engage in structured activities. Using a list of activities to prompt the child may aid their recall [14], although we acknowledge that some children may have participated in sports other than those listed and hence we may be under-estimating their levels of activity. Similarly, we did not incorporate time walking to and/or from school, or non-sporting activities. Nonetheless, others have also reported low levels of PA using objective measurements based on accelerometry (average of 20 min of moderate-vigorous PA (MVPA) per day in the ALSPAC birth cohort at age 12, with 75% of the cohort undertaking 30 mins or less of MVPA per day) [27]. In order to estimate their daily level of PA, we had to take an average of the child’s weekly sports participation. Hence, we had a relatively crude measure of PA. Whilst this has enabled us to examine the association between PA and behavioural problems from a public health perspective, it is likely that this will have led to a misclassification, which may have attenuated any effect. However, we did find a significant association between the number of sessions of sporting activity in the previous week and the number of days in which the children reported participating in physical activity outside their home (Kruskal–Wallis P < 0.001), which provides some evidence for the validity of our measure of PA. An objective measure of PA would provide more accurate estimates.
We adjusted for a number of potential confounders. Boys were more active than girls and adjustment for gender substantially attenuated the observed activity-behaviour association. Adjustment for baseline symptoms also further attenuated the effect. We cannot rule out the possibility of residual confounding (e.g., by parental mental health or family socio-economic position), although adjustment for other potential confounders (including area-level deprivation) had little effect. Moreover, it is plausible that if PA is associated with behavioural problems, then scores on the SDQ at baseline will lie on a causal pathway between PA at an earlier age and later behavioural problems, and as such, adjustment for baseline symptoms may represent an over-adjustment.
The proportion of children who met recommended levels was low (13%). This will have reduced the precision of our effect estimates. In addition, emotional problems are less common in younger adolescents, which means that we may have under-estimated the effect. Moreover, any benefit of PA may be greater amongst those who maintain a physically active lifestyle and thus examining the association over a shorter interval or in datasets with repeated measurements of PA may be useful.
Nonetheless, as highlighted earlier, there is little existing longitudinal data. In a US study of 1,500 high school students, the relationship between a wide range of psychosocial variables and current, past and incident depression was examined [20]. This study found that frequency of exercise was not significantly associated with incident depression over the 14-month follow-up period. However, a detailed description of the single-item question used to ascertain exercise frequency was lacking and no data were presented to permit examination of the effect size that was excluded. A more recent study of a representative sample of UK adolescents also found no association between exercising habits at baseline and depressive symptoms after 2-years follow-up [5]. However, the definition of exercise in that study, as in ours, was relatively crude in that it described those children who exercised “more or less than twice a week for an hour”. Assuming two hours exercise per week, this equates to 17 min per day, considerably less than the recommended levels.
One previous longitudinal study, using a latent growth modelling approach, found that changes in physical activity were associated with a reduction in depressive symptoms over a 2-year period [25]. However, the authors acknowledged that the direction of causality could not be inferred because of the concurrent measurement of PA and depressive symptoms. In common with the findings from our study, they also remarked that the magnitude of the change was small, with a one SD change in PA associated with a 0.25 SD decrease in depressive symptoms [25]. Others have found an association between physical activity and emotional problems amongst boys [33] but not girls, but we found little evidence for a differential effect when testing formally for an interaction by gender.
Whilst at present, there is only weak evidence to support an association between PA and emotional problems amongst children, in part this reflects the dearth of longitudinal studies with very good quality data in this area. Furthermore, little is understood about the mechanisms that may underlie an association between PA and mental health, although the existing evidence points towards a link with the pathophysiology of depression. This is in agreement with our finding that the association between PA and mental health was specific to emotional problems rather than other childhood behavioural problems (conduct problems, peer problems or prosocial behaviour). In animal studies, exercise has been shown to increase levels of brain-derived neurotrophic factor [44], cell proliferation [4] and 5-hydroxytryptamine release [22]. Reductions in cortisol may also be implicated [26]. Other studies have suggested a mediating role for psychosocial factors such as body image [15] and self-esteem [7, 35], and mechanisms operating via social support may also be relevant [34].
Any benefits derived from leading a physically active lifestyle could depend on the context in which this PA is accumulated. In England, it is recommended that children aged 11–14 years (key stage 3) should receive 90 min of physical education each week (http://www.teachernet.gov.uk/teachingandlearning/subjects/pe/curriculum). Extramural activities are therefore essential to meeting recommended daily levels of PA. Voluntary participation in sporting activities outside of school could increase social networks, which in turn could provide the child with better social support, which may protect against the development of emotional problems. Exploratory analyses examining the association between sporting activities undertaken in school and those out-of-school sessions in our study provided some evidence of a larger effect from participation in out-of-school sports. However, no firm conclusions could be drawn given the overlapping confidence intervals surrounding effect estimates. Nonetheless, this warrants further investigation.
Conclusions
Children who met recommended levels for PA had fewer emotional problems 1-year later. Future longitudinal studies need to record both PA and emotional problems at frequent intervals (every 3 or 4 months) in order to enable us to examine the effect of maintaining a physically active lifestyle on adolescent mental health outcomes. In addition, such studies need to focus on examining potential mediators of this relationship.
References
Allison KR, Adlaf EM, Irving HM, Hatch JL, Smith TF, Dwyer JJ, Goodman J (2005) Relationship of vigorous physical activity to psychologic distress among adolescents. J Adolesc Health 37:164–166
Bailey RC, Olson J, Pepper SL, Porszasz J, Barstow TJ, Cooper DM (1995) The level and tempo of children’s physical activities: an observational study. Med Sci Sports Exerc 27:1033–1041
Biddle SJH, Cavill N, Sallis J (1998) Policy framework for young people and health-enhancing physical activity. In: Biddle SJH, Sallis J, Cavill N (eds) Young and active? Young people and health-enhancing physical activity: Evidence and implications. Health Education Authority, London, pp 3–16
Bjornebekk A, Mathe A, Brene S (2005) The antidepressant effect of running is associated with increased hippocampal cell proliferation. Int J Neuropsychopharmacol 8:357–368
Clark C, Haines MM, Head J, Klineberg E, Arephin M, Viner R, Taylor SJ, Booy R, Bhui K, Stansfeld SA (2007) Psychological symptoms and physical health and health behaviours in adolescents: a prospective 2-year study in East London. Addiction 102:126–135
Department of Health (2004) At least five a week. Evidence on the impact of physical activity and its relationship to health. Department of Health, London
Dishman RK, Hales DP, Pfeiffer KA, Felton GA, Saunders R, Ward DS, Dowda M, Pate RR (2006) Physical self-concept and self-esteem mediate cross-sectional relations of physical activity and sport participation with depression symptoms among adolescent girls. Health Psychol 25:396–407
El-Metwally A, Halder S, Thompson D, Macfarlane GJ, Jones GT (2007) Predictors of abdominal pain in schoolchildren: a 4-year population-based prospective study. Arch Dis Child 92:1094–1098
Field T, Diego M, Sanders CE (2001) Exercise is positively related to adolescents’ relationships and academics. Adolescence 36:105–110
Fulkerson JA, Sherwood NE, Perry CL, Neumark-Sztainer D, Story M (2004) Depressive symptoms and adolescent eating and health behaviors: a multifaceted view in a population-based sample. Prev Med 38:865–875
Goodman R (1997) The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry 38:581–586
Goodman R (2001) Psychometric properties of the Strengths and Difficulties Questionnaire. J Am Acad Child Adolesc Psychiatry 40:1337–1345
Haarasilta LM, Marttunen MJ, Kaprio JA, Aro HM (2004) Correlates of depression in a representative nationwide sample of adolescents (15–19 years) and young adults (20–24 years). Eur J Public Health 14:280–285
Harro M, Riddoch C (2000) Physical activity. In: Armstrong N, van Mechelen W (eds). Paediatric Exercise Science and Medicine. Oxford University Press, Oxford, pp 77–84
Hausenblas HA, Fallon EA (2006) Exercise and body image: a meta-analysis. Psychol Health 21:33–47
Jones GT, Watson KD, Silman AJ, Symmons DPM, Macfarlane GJ (2003) Predictors of low back pain in British schoolchildren: a population-based prospective cohort study. Pediatrics 111:822–828
Kesaniemi YK, Danforth E Jr, Jensen MD, Kopelman PG, Lefebvre P, Reeder BA (2001) Dose-response issues concerning physical activity and health: an evidence-based symposium. Med Sci Sports Exerc 33:S351–S358
Kirkcaldy BD, Shephard RJ, Siefen RG (2002) The relationship between physical activity and self-image and problem behaviour among adolescents. Soc Psychiatry Psychiatr Epidemiol 37:544–550
Larun L, Nordheim LV, Ekeland E, Hagen KB, Heian F (2006) Exercise in prevention and treatment of anxiety and depression among children and young people. Cochrane Database of Systematic Reviews Issue 3 Art. No: CD004691, doi:10.1002/14651858.CD004691.pub2
Lewinsohn PM, Roberts RE, Seeley JR, Rohde P, Gotlib IH, Hops H (1994) Adolescent psychopathology II: Psychosocial risk factors for depression. J Abnorm Psychol 103:302–315
McDermott RJ, Hawkins WE, Marty PJ, Littlefield EA, Murray S, Williams TK (1990) Health behavior correlates of depression in a sample of high school students. J Sch Health 60:414–417
Meeusen R, Thorre K, Chaouloff F, Sarre S, De Meirleir K, Ebinger G, Michotte Y (1996) Effects of trytophan and/or acute running on extracellular 5-HT and 5-HIAA levels in the hippocampus of food-deprived rats. Brain Res 740:245–252
Meltzer H, Gatward R, Goodman R, Ford T (2000) Mental health of children and adolescents in Great Britain. The Stationery Office, London
Milligan RA, Burke V, Beilin LJ, Richards J, Dunbar D, Spencer M, Balde E, Gracey MP (1997) Health-related behaviours and psycho-social characteristics of 18-year-old Australians. Soc Sci Med 45:1549–1562
Motl RW, Birnbaum AS, Kubik MY, Dishman RK (2004) Naturally occurring changes in physical activity are inversely related to depressive symptoms during early adolescence. Psychosom Med 66:336–342
Nabkasorn C, Miyai N, Sootmongkol A, Junprasert S, Yamamoto H, Arita M, Miyashita K (2005) Effects of physical exercise on depression, neuroendocrine stress hormones and physiological fitness in adolescent females with depressive symptoms. Eur J Public Health 159:1–6 doi:10.1093/eurpub/cki
Ness AR, Leary SD, Mattocks C, Blair SN, Reilly JJ, Wells J, Ingle S, Tilling K, Davey Smith G, Riddoch C (2007) Objectively measured physical activity and fat mass in a large cohort of children. PLoS Med 4:e97 doi:10.1371/journal.pmed.0040097
Norris R, Carroll D, Cochrane R (1992) The effects of physical activity and exercise training on psychological stress and well-being in an adolescent population. J Psychosom Res 36:55–65
Page RM, Tucker LA (1994) Psychosocial discomfort and exercise frequency: an epidemiological study of adolescents. Adolescence 29:183–191
Pastor Y, Balaguer I, Pons D, Garcia-Merita M (2003) Testing direct and indirect effects of sports participation on perceived health in Spanish adolescents between 15 and 18 years of age. J Adolesc 26:717–730
Perera B, Torabi MR, Jayawardana G, Pallethanna N (2006) Depressive symptoms among adolescents in Sri Lanka: prevalence and behavioral correlates. J Adolesc Health 39:144–146
Riddoch C (1998) Relationships between physical activity and physical health in young people. In: Biddle SJH, Sallis J, Cavill N (eds) Young and active? Young people and health-enhancing physical activity: evidence and Implications. Health Education Authority, London, pp 17–48
Sagatun A, Sogaard AJ, Bjertness E, Selmer R, Heyerdahl S (2007) The association between weekly hours of physical activity and mental health: A three-year follow-up study of 15–16 year old students in the city of Oslo, Norway. BMC Public Health 7, doi:10.1186/1471-2458-7-155
Seefeldt V, Malina RM, Clark MA (2002) Factors affecting levels of physical activity in adults. Sports Med 32:143–168
Spence JC, McGannon KR, Poon P (2005) The effect of exercise on global self-esteem: a quantitative review. J Sport Exerc Psychol 27:311–334
StataCorp (2007) Stata Statistical Software: Release 9.2. Stata Corporation, College Station
Steptoe A, Butler N (1996) Sports participation and emotional wellbeing in adolescents. Lancet 347:1789–1792
Strong WB, Malina RM, Blimkie CJ, Daniels SR, Dishman RK, Gutin B, Hergenroeder AC, Must A, Nixon PA, Pivarnik JM, Rowland T, Trost S, Trudeau F (2005) Evidence based physical activity for school-age youth. J Pediatr 146:732–737
Townsend P, Phillimore P, Beattie A (1988) Health and deprivation: inequality in the North. Crook Helm, London, UK
Twisk JW (2001) Physical activity guidelines for children and adolescents: a critical review. Sports Med 31:617–627
Ussher MH, Owen CG, Cook DG, Whincup PH (2007) The relationship between physical activity, sedentary behaviour and psychological wellbeing among adolescents. Soc Psychiatry Psychiatr Epidemiol 42:851–856
van Buuren S, Boshuizen HC, Knook DL (1999) Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med 18:681–694
Watson KD, Papageorgiou AC, Jones GT, Taylor S, Symmons DPM, Silman AJ, Macfarlane GJ (2002) Low back pain in schoolchildren: occurrence and characteristics. Pain 97:87–92
Zheng H, Liu Y, Li W, Yang B, Chen D, Wang X, Jiang Z, Wang H, Wang Z, Cornelisson G, Halberg F (2006) Beneficial effects of exercise and its molecular mechanisms on depression in rats. Behav Brain Res 168:47–55
Acknowledgements
We acknowledge the contributions of Kath Watson, who was responsible for co-ordinating the baseline survey; the team of fieldworkers (Stewart Taylor, Ann Papageorgiou, Priscilla Appelbe, Elizabeth Nahit and Isabelle Hunt), who conducted the school visits; and Professors Alan Silman and Deborah Symmons who assisted in supervising study conduct. Finally, we are indebted to the school staff and children who participated in the study. The study of low back pain amongst schoolchildren was funded by the Colt Foundation, Medical Research Council and the Arthritis Research Campaign.Declaration of interest None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wiles, N.J., Jones, G.T., Haase, A.M. et al. Physical activity and emotional problems amongst adolescents. Soc Psychiat Epidemiol 43, 765–772 (2008). https://doi.org/10.1007/s00127-008-0362-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-008-0362-9