Abstract
Background
Data based on general population studies of exposure-to-risk factors is not adequate to describe the mental health of children living in the most extreme “high-risk” environments.
Methods
Data were collected in a longitudinal prospective study of two cohorts of 9 and 13 year-old socially at-risk children. Cluster analysis was used to classify youths based on the reports about potential areas of risk. The psychopathological structure of empirical clusters was compared through cross-sectional and longitudinal epidemiological indexes and through multiple regression and multivariate analysis of variance.
Results
Cluster analysis provided eight binary high-low risk classifications. Exposure to risk was highly prevalent. In preadolescence, broken family, parenting style and contextual profiles were the highest risk factors for psychopathology. In adolescence, they were psychological variables, verbal comprehension, pre-peri-postnatal history, physical health and family characteristics. Cumulative risk followed a linear trend for psychopathology and functional impairment. The child’s perception of low marital discord and good school achievement were protective factors.
Conclusions
Extreme socially at-risk populations have specific profiles of risk that can be identified through a person-centered approach and may be amenable to selective preventive interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The median prevalence of psychopathology in children and adolescents is around 12% [8]. Treatment interventions for reducing the high prevalence of mental disorders in populations exceed the budgets of most developed countries. A main concern of developmental epidemiology is the detection of risk factors that can be addressed in preventive interventions to reduce the incidence of the disorders [9]. Information taken from risk research is useful to decide target groups, what factors must be altered, and the time and choice of adequate evidence-based preventive interventions. Effective preventive programs use a research-based risk factor framework that involves families, peers, schools and communities as partners to target multiple outcomes [37].
Risk factors tend to co-occur and to interact. For this reason, research into risk factors needs to consider multiple domains of risk. Essex et al. [17] have suggested that externalizing and internalizing disorders share similar risk factors. They point out the cases of socioeconomic risk, history of psychopathology, marital and family conflict, and other authors have added parent–child relationships to the list [49], as well as temperament [36]. Prenatal factors [1, 48], deviant peer groups [13], parental monitoring and discipline [49] and verbal comprehension [30] have mostly been related to externalizing disorders, whereas life events were related to internalizing disorders [34, 51]. These factors also have important influences on prognosis [22]. However, not all the children exposed to risk factors develop later problems, since the relationship between exposure to risk and psychopathology could be moderated by the presence of protective factors. Parenting, child’s language skills, normal family functioning and monitoring of the child, or child’s competence act as protective factors in child psychopathology [5, 35]. Knowledge of protective factors can help to identify groups for selective preventive interventions and to develop preventive strategies.
Different studies have reported that the effect of risk factors is cumulative and the greater the number of risk factors, the greater the risk, regardless of which single particular risk factors are present or absent. This approach provides a comprehensive analysis of the global adversity experienced by a child and has implications for identifying candidates for intervention. Two models of how risk factors operate have been proposed: (a) a linear model in which risk increases steadily and would imply that every risk factor must be considered for prevention [3, 42] and (b) a threshold model in which the occurrence of an outcome of a certain number of risk factors increases in a quadratic shape and would indicate that preventative intervention should be administered to those children exceeding a certain number of risk factors [26, 32, 40].
Social and economic disadvantages place children at higher than average likelihood of developing mental disorders [7]. It is necessary to study the most disadvantaged nuclei of the populations, as they constitute a target group that is susceptible of receiving selective preventive interventions. Moreover, this would make it possible to determine the number of children in this segment of the population affected by at-risk situations, what these situations are, and how they affect the mental health and daily functioning of the population. The effective planning of services requires knowledge of where the preventive efforts should be focused. The overall aim of this work was to examine profiles of risk factors in a socially at-risk population of children followed over 3 years and the influence of the identified groups and their accumulative impact on subsequent adjustment. The specific objectives were: (a) to explore the existence of risk profiles taking into account the individual, familial and contextual characteristics of the children; (b) to provide epidemiological indexes of the exposure to risk and to evaluate its association with psychopathology at different ages; (c) to examine protective factors; and (d) to analyze the nature of the cumulative risk of clusters on psychopathology. A “person-centered approach” begins with the grouping of individuals according to their responses/scores for different features, and focuses attention on the intra-individual structure of variables [10]. The primary advantage of these analyses is the conceptualization of the subjects; they are conceived as a whole, and not as the addition of isolated features. These analytic procedures have rarely been used in the research of child and adolescent psychopathology in deprived social groups in Europe.
Methods
Participants
Data were taken from a longitudinal study carried out to obtain mental health epidemiological indexes for a full high-risk population of children and adolescents located on the periphery of Barcelona [21]. The concentration of low socio-economic levels, social problems, immigration and disadvantages in this municipality is very similar to the suburbs surrounding the industrial belts of other large cities in Spain.
Two cohorts of all children born in 1989 and in 1993 registered in the Badía del Vallès census in 2001 were assessed over 3 years (2002, 2003, 2004) at 1-year intervals. In 2002, these children were 13 and 9 years old, respectively. Ages 9 and 13 were chosen as developmental points indicating pre- and post-puberty.
The census for children born in 1989 contained 147 subjects. Of these, 79 (53.7%) agreed to participate in the study. The list of children born in 1993 included a total of 121 subjects. Of these, 72 children (59.5%) joined the study. Fifty-six percent of participating children were male, 98% Caucasian and 85% were of mean-low or low socioeconomic status [29]. More data on the demographic characteristics and participation is available in [21, 25].
Measures
The current version of the Diagnostic Interview for Children and Adolescents, the MAGIC [39], was used to assess psychopathology following DSM-IV [2]. The interview has been adapted and validated for the Spanish population [18]. Diagnoses from the last year were generated by combining the information from parents and children at a symptom level. The number of externalizing (disruptive behavior disorders and substances) and internalizing symptoms (depression and anxiety) was calculated by summing up the number of positive symptoms in these areas.
The schedule for risk factors (SRF) [47] is a structured interview based on the Service Utilization and Risk Factors interview [24], but modified for administration with the aid of a portable computer. The interview is conceived as a compendium of potential areas of risk of psychopathology for children aged 8–18 that include some previously developed independent instruments. Inter-interviewer reliability and concurrent validity of this modified version are acceptable [20, 28]. The following sections reported by parents and children were used: school and other activities, family environment (Family APGAR [23]), parental monitoring scale [24], discipline (Parental Discipline Practices Scales [24]), marital discord (Child’s Perception of Interparental Conflict Scale [27]); Dyadic Adjustment Scale [45], friends and relationships with siblings. Children were asked about uncontrollable life events (based on Life Events Checklist [31]), self-esteem and social skills. Self-esteem and social skills were included as independent variables because different theoretical models have reported that self-system processes mediate the relationship between adversity and psychological adjustment [38, 43]. Parents reported on socio-demographic information, pregnancy, delivery, early development, temperament and family history (based on Family Psychiatric History Screen for Epidemiologic Studies [33]). Parents and children’s reports were combined by selecting the highest risk level reported by the dyad. Binary variables were coded as 1 indicating the relevant risk was present.
The age-standardized scores of the Peabody Picture Vocabulary Test [16] were used to evaluate verbal comprehension.
The global children’s assessment scale (CGAS) [19, 44] was used to assess the functional-impairment level produced by the psychopathology. A CGAS lower than 70 was considered to be of clinical significance.
Procedure
After obtaining informed written consent from parents and oral consent from children, trained interviewers conducted interviews with parents and their children separately and simultaneously. All the measures described previously were recorded in each assessment.
Statistical analysis
Analyses were conducted through SPSS 14. Risk factor profiles were explored through Two-Step Cluster Analyses. This procedure identifies natural groups from a data set based on a nearness criterion, using a hierarchical agglomerative clustering procedure in which individual cases are successively combined to form clusters whose centers are far apart. The distance measure selected in this study was likelihood, which is computed using the normal density for continuous variables and the multinomial probability mass function for categorical variables. Due to the large number of previous independent variables and the limited sample size, separate cluster analyses were conducted for the different sections of the SRF interview grouped by its content life-time (including time 0 assessment). Two cluster solutions were specified a priori. The internal validity of the clusters was investigated by comparing the cluster-profiles based on independent variables from the first assessment with new cluster assignments based on the variables recorded during the subsequent assessment (second year of the study). The accuracy (stability over time) of the cross-classification was tested through “hit rates” calculated independently for each cluster and based on the cross-tabulation of the results obtained in each assessment. Hit rates were equal to the ratio between the number of individuals falling within the same cluster by the two time-methods (i.e. the “coincidences” in both classifications) divided by the cluster sample size from the comparative classification (in this study, groups obtained in the first assessment). In 2 × 2 tables, hit rates reveal the “sensitivity” and “specificity” of the clustering. Hit rates above 75% indicate high agreement, between 50 and 75% moderate agreement and below 50% fair to poor agreement [15].
The prevalence of psychopathology was calculated for the different ages and clusters. Differences due to the risk factor profile were assessed with Pearson’s chi-square procedures (selecting exact methods with small samples). Means for total internalizing and externalizing symptoms were also obtained and compared with Fisher’s t test. The population attributable fraction (AFp) expresses the maximum proportion of outcome in the population that would be eliminated if a risk factor was eliminated [46]. This index was estimated for general indicators of psychopathology (any diagnosis and impairment) when the difference in the prevalence between the high and low cluster was significant.
The predictive value of clusters with regard to psychopathology was assessed during the study with logistic and multiple linear regressions. In these analyses, the risk profiles (independent variables) at time 0 were entered simultaneously into models and subjects’ psychological state at times 1 or 2 (functional impairment and total number of disorders and symptoms) was the criteria (outcome variables). Global predictive value was assessed with adjusted and Nagelkerke’s R 2 coefficients. For the study of protection from any DSM-IV diagnosis in follow-ups 1 and 2 (dependent variable), we used the cluster of life-events as independent variables in the first assessment (follow-up 0) as a measure of adversity against which we could check whether risk trajectories were modified. Moderator variables included individual variables related with the degree of parental monitoring, self-esteem, marital discord (CPIC), number of temperamental difficulties, number of physical diseases, school achievement and deviant peers (use of substances). When the interaction terms achieved P ≤ 0.010 values, OR coefficients indicating the association between the inclusion in the high-risk life-events cluster and the presence of any diagnosis were obtained for each level of binary moderator variables and for percentiles 25, 50 and 75 for quantitative ones.
The number of accumulated risk clusters was obtained by adding up the high-risk profiles in which the children were included. The association between this accumulated risk measure and psychopathology was analyzed through analyses of variance and linear regression models (for quantitative psychopathological measures) and through chi-square tests and logistic regressions (for categorical outcomes). Polynomial contrasts revealed linear and quadratic trends.
Results
Composition of clusters
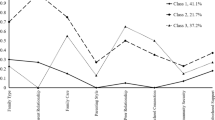
Cluster analyses provided eight binary classifications. Each cluster constitutes a specific risk-profile at the beginning of preadolescence and adolescence. Table 1 contains the composition of these profiles, the number of subjects included, and the mean values of independent variables selected for the grouping. No significant differences due to age were found in the cluster contents. Each cluster was labeled “high-risk” versus “low-risk” level depending on the agreement of its content with previous theory. The exception was the demographic cluster which grouped two at-risk groups: broken families and major economic disadvantage (keeping in mind that the whole population is at-socio-economic risk). The stability of clusters over time ranged between moderate and high. Differences between sexes were only observed for parenting style cluster: more boys than girls were associated with the high-risk cluster (P = 0.03). The high-risk cluster with the lowest percentage of subjects was verbal comprehension (22%) while the highest percentage of subjects was associated with physical health (63.2%).
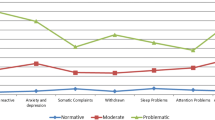
Prevalence and AFps
One hundred percent of the preadolescents and 90% of the adolescents belonged to some high-risk group. Table 2 contains prevalence and means stratified by cluster and age. The high-risk cluster based on demographic features (economic disadvantage) was highly prevalent in disruptive disorders (age 9), while the demographic characteristics of broken families were significantly more prevalent in depressive disorders and functional impairment (age 13). Low self-esteem and poor social skills occurred frequently in any diagnosis (10, 13), disruptive disorders (10, 14, 15), depressive disorders (13) and the functional impairment cluster (9, 13). High-risk profile of pre-peri-postnatal history was frequent in any diagnosis, disruptive and functional impairment at ages 13 and 14. An unhealthy physical profile was common in any diagnosis (age 13) and functional impairment (11). High-risk family characteristics were mostly present in disruptive psychopathology (age 13). The life events cluster occurred frequently in any diagnosis (age 14) and depressive disorders and functional impairment (age 13). Harsh discipline and lack of control was prevalent in disruptive disorders (ages 9, 11, 13) whereas parental monitoring and low discipline was frequent in anxiety disorders at age 9. Finally, the high-risk context cluster was common in any diagnosis (age 15), disruptive disorders (all ages except 9) and functional impairment (ages 9, and all adolescents).
AFps indicate that the maximum proportion of any diagnoses in the population that would be eliminated if risk factors were eliminated ranged between 12.3 and 81.6%. These proportions would arise in the case of functional impairment between 20.6 and 86.3%.
Association between clusters and psychopathology and functional impairment
Table 3 shows the results of multiple regressions which highlight the predictive value of clusters in psychopathology. Data indicated that the parenting style high-risk profile was predictive of a higher number of externalizing symptoms (ages 10, 11) and any diagnosis (15) but a lower number of internalizing symptoms (age 11). A contextual high-risk profile increased the number of total symptoms, functional impairment (11) and the number of externalizing symptoms (11, 14). The existence of a previous high-risk psychological profile increased “any DSM-IV diagnosis” (10, 14, 15), functional impairment (14, 15), the number of total disorders and symptoms, and externalizing symptoms (14). Good verbal comprehension predicted better functioning (14, 15), lower externalizing and total symptoms (14), and less risk of any diagnosis (15). Pre-peri and postnatal high-risk profiles were related to a subsequent higher number of externalizing and total symptoms (14). The poor physical health and family characteristics profile predicted “any DSM-IV diagnosis” (14).
Whole clusters explained between 24 and 55.8% of the variance of any DSM-IV diagnosis. The totality of clusters also explained a high percentage of externalizing and total symptoms (63.2 and 56% at age 14; 30.9 and 29.3% at age 15).
It could be argued that the high number of statistical comparisons could result in an increase in false positives. Table 3 contains 27 significant results out of a total of 216 comparisons. The probability of obtaining at least 27 statistically significant associations at α = 0.05 level from 216 comparisons by chance was equal to 0.0007 [4, 41]. This small value suggests that chance alone is not the reason for the results obtained in Table 3.
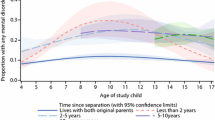
Protective factors
Given the high level of risk exposure it was interesting to find out what protected healthy children from psychopathology. Considering each cohort separately, no interaction was significant and both cohorts were skipped in this analysis. Low perception of marital conflict (interaction P = 0.044, OR = 0.83, 95% CI: 0.26–2.59) and good school achievement (interaction P = 0.084, OR = 1.02, 95% CI: 0.39–2.63) were protective factors of any DSM-IV diagnosis in relation to life-events (Fig. 1).
Cumulative risk
The cumulative risk of belonging to different clusters of risk at age 9 was predictive of a higher functional impairment (age 10) and a higher number of externalizing and total symptoms (ages 10, 11) (Table 4). Similarly, cumulative risk at age 13 was predictive of all the outcome variables at age 14 and of any diagnosis, higher functional impairment, higher number of total and externalizing symptoms at age 15. Analysis of variance to evaluate the nature of the relations (linear vs. quadratic) between the number of clusters of risk and outcomes at every age supported a significant linear trend of risk for functional impairment (ages 9, 10, 13, 14, 15), total disorders (ages 13, 14, 15), externalizing and total symptoms (all ages), internalizing symptoms (ages 9, 13, 14), and any diagnosis (ages 13, 14, 15).
The number of clusters of risk was linearly associated with having any diagnosis at ages 13 (P = 0.001), 14 (P = 0.002) and 15 (P = 0.001).
Discussion
Different homogeneous subgroups of at risk children with a distinct predisposition for later psychopathology and functioning were identified. High-risk groups were characterized by broken families or major economic difficulties, poor self-esteem and social skills, mother’s use of substances during pregnancy and high number of problems during pregnancy, early developmental difficulties, poor physical health, bad marital relationships and a history of psychopathology/abuse in caretakers, high number of life-events, low parental monitoring and harsh discipline, peers’ substance use and difficulties at school. The most prevalent high-risk clusters across all the disorders were the psychological, demographics, life-events, pre-peri-postnatal history and context clusters. In preadolescence, demographics (broken family), parenting style and contextual profiles were the highest risk factors for psychopathology. In adolescence, the highest risk factor profiles were psychological variables, verbal comprehension, pre-peri-postnatal history, physical health and family characteristics. Cumulative risk followed a linear trend in terms of psychopathology and functional impairment. Low marital discord and good school achievement were protective factors in terms of life-events.
Relative to previous research which was based mostly on a variable-level approach assessing associations between variables, the objective of this study was to identify naturally occurring groups of youths in a socially deprived population, and to examine repercussions for later adaptation. The independent variables selected as input to the cluster analyses represent a broad spectrum of background risk variables for subjects. Additionally, their specific configuration led to different profiles based on the individual characteristics of children–adolescents, their families and their context, and proved useful in predicting children’s psychopathological symptoms. Psychopathology measures, with which resultant profiles were related, reflect the most frequent mental-health indicators considered for determining the need (or not) of receiving professional help and planning interventions. The sum of all the clusters was highly explicative of psychopathology (highest R 2 63 and 56%).
Key areas of preventive intervention and key critical periods when exposure is most harmful were evidenced. There were developmental differences between preadolescents and adolescents with regard to the effect of the risk profiles. Specifically, age 13 is a key year associated with the highest prevalence of high-risk clusters and at age 14 the effect of the risk is most significant. Also, the effect of cumulative risk was more marked in adolescence than in preadolescence. Adolescence in general and age 14 in particular, is the most sensitive period to the accumulation of risk. Early adolescence is a critical period in which high-risk youths are more vulnerable to different influences [14]. The implications of the linear trend of risk for prevention are twofold: (1) the number of risk factors should be reduced, and (2) “every” risk factor should be taken into account. Preventive effective intervention must be multi-systemic [50] and should incorporate interventions directed towards the child, the parents, the school, and the community. Wide-ranging social and educational strategies to eliminate the high concentration of adversity and diminish the incidence of disorders must co-occur. Pregnancy follow-ups and early development focus including parental training, improvement of school difficulties, marital functioning and parent’s mental health, intervention on peer substance use, and enhancement of cognitive abilities of youth should be fundamental components for intervention in populations such as this in order to diminish the risk of externalizing disorders, functional impairment and psychopathology in general. By targeting generic risk factors, vulnerabilities to different disorders will be prevented. AFp considers the prevalence of the risk factor and the strength of its association with the outcome in determining the target population for preventive intervention and, by doing this, helps to optimize the balance between the benefits and the costs of the preventive program [12]. If AFps are taken into account to hierarchically arrange the intervention, the maximum proportion of any diagnosis (81.6%) and functional impairment in the population (between 66.1 and 86.3%) would be eliminated assuming a preventive intervention was directed at eliminating the risks of context. Adolescents with school difficulties and friends using substances would be the target population. AFp would also recommend a focus on physical health in preadolescents (AFp 80.5%) and intervening early in life, from pregnancy to age 6, to prevent between 38.3 and 62.8% of difficulties adapting later in adolescence. Further, preventive interventions can be oriented towards promoting protective factors. Considering life-events to be a measure of adversity, we found that the trajectories to a DSM-IV diagnosis for this population were modified in the case of families with low marital discord and children with good school achievement. Accordingly, preventive efforts could also be focused on promoting good relations in families and competence at school. The importance of both competence in resiliency and marital discord as detrimental factors for a child’s mental health have been extensively highlighted in the literature [11, 35]. Future research must indicate the efficiency of cluster groups as targets for preventive interventions.
Some of the unique contributions of this research include the use of a non-Anglo-Saxon disadvantaged population, the analysis of risk factors using a person-centered approach including multiple domains of risk longitudinally reported by multiple informants, and the reporting of the effect of the cumulative risk of the clusters. Data based on general population studies of exposure-to-risk factors is not adequate to describe the mental health of children living in the most extreme “high-risk” environments [6]. These children represent a segment of the population where the concentration of adverse living circumstances creates specific risks and needs that must be addressed by administrators. The fact that the population had a small number of subjects is the main limitation of this study. This had implications on (a) the number of independent variables included in each analysis and the need to group into sets and (b) the number of final clusters for each set, which was at the most two (otherwise the subsequent analytic procedures would not carry enough statistical weight). Sample size could well account for some inconsistencies across ages in the association between risk factors and diagnoses. Finally, because of the small number of cases, the absence of relationships between risk clusters and disorders must not be interpreted as being a real lack of association; it may simply be an effect of the lack of statistical weight.
Conclusion
Literature on the prevalence of risk factors in deprived populations is scarce. Exposure to risk was extremely high in this population: all the preadolescents and 90% of the adolescents pertained to a risk-cluster, which indicates that extreme high-risk populations need specific preventive measures. Risk is cumulative and follows a linear trend: the higher the number of high-risk clusters, the higher the psychopathology and impairment.
These results have implications for preventive programs. Multicomponent comprehensive preventive programs should reduce the number of risk factors taking into account “every” risk present. Profiles of high-risk clusters can be used as target groups for prevention. To eliminate risks of context, the targeting of adolescents with school difficulties and substance using friends should be a priority. It would then be important to take care of the physical health of preadolescents and intervene early in life (from pregnancy to age 6).
Abbreviations
- AFp:
-
Population attributable fraction
References
Allen NB, Lewinsohn PM, Seeley JR (1998) Prenatal and perinatal influences on risk for psychopathology in childhood and adolescence. Dev Psychopathol 10:513–529
American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders-IV. Author, Washington
Appleyard K, Egeland B, van Dulmen MHM, Sroufe A (2005) When more is not better: the role of cumulative risk in child behavior outcomes. J Child Psychol Psychiatry 46:235–245
Brozec J, Tiede K (1952) Reliable and questionable significance in a series of statistical tests. Psychol Bull 49:339–341
Burchinal M, Roberts JE, Zeisel SA, Hennon EA, Hooper SR (2006) Social risk and protective child, parenting, and child care factors in early elementary school years. Parenting-Sci Pract 6:79–113
Canty-Mitchell J, Austin JK, Jaffee K, Qi RA, Swigonski N (2004) Behavioral and mental health problems in low-income children with special health care needs. Arch Psychiatr Nurs 18:79–87
Costello EJ, Compton SN, Keeler G, Angold A (2003) Relationship between poverty and psychopathology. JAMA 290:2023–2029
Costello EJ, Egger HL, Angold A (2005) 10-year research update review: the epidemiology of child and adolescent psychiatric disorders: I. Methods and public health burden. J Am Acad Child Adolesc Psychiatry 44:972–986
Costello EJ, Foley D, Angold A (2006) 10-year research update review: the epidemiology of child and adolescent psychiatric disorders: II. Developmental epidemiology. J Am Acad Child Adolesc Psychiatry 45:8–25
Crockett LJ, Moilanen KL, Raffaelli M, Randall BA (2006) Psychological profiles and adolescent adjustment: a person-centered approach. Dev Psychopathol 18:195–214
Cummings EM, Davies PT (2002) Effects of marital conflict on children: Recent advances and emerging themes in process-oriented research. J Child Psychol Psychiatry 43:31–64
Davis CH, MacKinnon DP, Schultz A, Sandler I (2003) Cumulative risk and population attributable fraction in prevention. J Clin Child Adolesc Psychol 32:228–235
Dishion TJ (2000) Cross-setting consistency in early adolescent psychopathology: deviant friendships and problem behavior sequelae. J Pers 68:1109–1126
Dishion TJ, Poulin F, Medici Skaggs B (1999) The ecology of premature adolescent autonomy: biological and social influences. In: Kerns KA, Contreras JM, Neal-Baret M (eds) Explaining associations between family and peer relationships. Praeger, Westport
DiStefano C, Kamphaus RW, Horne AM, Winsor A (2003) Behavioral adjustment in the. U.S. Elementary school: cross-validation of a person-oriented typology of risk. J Psychoeduc Assess 21:338–357
Dunn LM (1984) Vocabulario en imágenes Peabody. Adaptación española. Mepsa, Madrid
Essex MJ, Kraemer HC, Armstrong JM, Boyce T, Goldsmith HH, Klein MH, Woodward H, Kupfer DJ (2006) Exploring risk factors for the emergence of children’s mental health problems. Arch Gen Psychiatry 63:1246–1256
Ezpeleta L, de la Osa N, Júdez J, Doménech JM, Navarro JB, Losilla JM (1997) Diagnostic agreement between clinician and the diagnostic interview for children and adolescents—DICA-R in a Spanish outpatient sample. J Child Psychol Psychiatry 38:431–440
Ezpeleta L, Granero R, de la Osa N (1999) Evaluación del deterioro en niños y adolescentes a través de la children’s global assessment scale (CGAS). Rev Psiquiatr Infanto-Juv 1:18–26
Ezpeleta L, Granero R, de la Osa N, Guillamon N (2000) Predictors of functional impairment in children and adolescents. J Child Psychol Psychiatry 41:793–801
Ezpeleta L, Guillamón N, Granero R, de la Osa N, Doménech JM, Moya I (2007) Prevalence of mental disorders in children and adolescents from a Spanish slum. Soc Sci Med 64:842–849
Ford T, Collishaw S, Meltzer H, Goodman R (2007) A prospective study of childhood psychopathology: independent predictors of change over three years. Soc Psychiatry Psychiatr Epidemiol 42:953–961
Good MD, Smilkstein G, Good BJ, Shaffer T, Arons T (1979) The family APGAR indices: a study of construct validity. J Fam Pract 8:577–582
Goodman S, Hoven C, Narrow W, Cohen P, Fielding B, Alegria M, Leaf PJ, Kandel D, Horwitz SM, Bravo M, Moore R, Dulcan MK (1998) Measurement of risk for mental disorders and competence in a psychiatric epidemiologic community survey: the national institute of mental health methods for the epidemiology of child and adolescent mental disorders (MECA). Soc Psychiatry Psychiatr Epidemiol 33: 162–173
Granero R, Ezpeleta L, Doménech JM (2007) Features associated with non-participation and abandonment in mental health epidemiological designs of socially-at-risk children and adolescents. Soc Psychiatry Psychiatr Epidemiol 42:251–258
Greenberg MT, Speltz ML, DeKlyen M, Jones K (2001) Correlates of clinic referral for early conduct problems: variable- and person-oriented approaches. Dev Psychopathol 13:255–276
Grynch J, Seid M, Finchman F (1992) Assessing marital conflict from the child’s perspective: the child’s perception of interparental conflict scale. Child Dev 63:558–572
Guillamon N (1999) Fiabilidad entre entrevistadores del Protocolo de Factores de Riesgo-Versión niños. Unpublished manuscript Universitat Autònoma de Barcelona
Hollingshead AB (1975) Four factor index of social status. Unpublished manuscript, Yale University, Department of Sociology, New Haven, CT
Hooper SR, Roberts JE, Zeisel SA, Poe M (2003) Core language predictors of behavioral functioning in early elementary school children: concurrent and longitudinal findings. Behav Disord 29:10–24
Johnson JH, McCutcheon SM (1980) Assessing life stress in older children and adolescents: preliminary findings with the life events checklist. In: Saranson I, Spielberger CD (eds) Stress and anxiety. Hemisphere, Washington, pp 111–125
Jones DJ, Forehand R, Brody G, Armistead L (2002) Psychosocial adjustment of African American children in single-mother families: a test of three risk models. J Marriage Fam 64:105–115
Lish JD, Weissman MM, Adams PB, Hoven CW, Bird HR (1995) Family psychiatric screening instrument for epidemiological studies: pilot testing and validation. Psychiatry Res 57:169–180
Luby JL, Belden AC, Spitznagel E (2006) Risk factors for preschool depression: the mediating role of early stressful life events. J Child Psychol Psychiatry 47:1292–1298
Masten AS, Obradovic J (2006) Competence and resilience in development. Ann N Y Acad Sci 1094:13–27
Muris P, Ollendick TH (2005) The role of temperament in the etiology of child psychopathology. Clin Child Fam Psychol Rev 8:271–289
Nation M, Crusto C, Wandersman A, Kumpfer KL, Seybolt D, Morrisey-Kane E, Davino K (2003) What works in prevention: principles of effective prevention programs. Am Psychol 58:449–456
Prelow HM, Weaver SR, Swenson RR (2005) Competence, self-esteem, and coping efficacy as mediators of ecological risk and depressive symptoms in urban African American and European American youth. J Adolesc 35:507–517
Reich W (2000) Diagnostic interview for children and adolescents (DICA). J Am Acad Child Adolesc Psychiatry 39:59–66
Rutter M, Cox A, Tupling C, Berger M, Yule W (1975) Attainment and adjustment in 2 geographical areas.1. Prevalence of psychiatric-disorders. Br J Psychiatry 126:493–509
Sakoda JM, Cohen BH, Beall G (1954) Test of significance for a series of statistical tests. Psychol Bull 51:172–175
Sameroff AJ, Bartko WT, Baldwin A, Baldwin C, Seifer R (1998) Family and social influences on the development of child competence. In: Lewis M, Feiring C (eds) Families, risk, and competence. Lawrence Erlbaum Associates, Mahwah, pp 161–186
Sandler I (2001) Quality and ecology of adversity as common mechanisms of risk and resilience. Am J Community Psychol 29:19–61
Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, Aluwahlia S (1983) A children’s global assessment scale (CGAS). Arch Gen Psychiatry 40:1228–1231
Spanier GB (1976) Measuring dyadic adjustment: A new scale for assessing the quality of marriage and similar dyads. J Marriage Fam 38:15–28
Tu S (2003) Developmental epidemiology: a review of three key measures of effect. J Clin Child Adolesc Psychol 32:187–192
Unitat d’Epidemiologia i de Diagnòstic en Psicopatologia del Desenvolupament (1997) Protocolo de Factores de Riesgo. Versión para padres. Universitat Autònoma de Barcelona, Departament de Psicologia Clínica i de la Salut, Barcelona
Wakschlag LS, Leventhal BL, Pine DS, Pickett KE, Carter AS (2006) Elucidating early mechanisms of developmental psychopathology: the case of prenatal smoking and disruptive behavior. Child Dev 77:893–906
Wamboldt MZ, Wamboldt FS (2000) Role of the family in the onset and outcome of childhood disorders: selected research findings. J Am Acad Child Adolesc Psychiatry 39: 1212–1219
Weissberg RP, Kumpfer KL, Seligman MEP (2003) Prevention that works for children and youth—an introduction. Am Psychol 58:425–432
Williamson DE, Birmaher B, Dahl RE, Ryan ND (2005) Stressful life events in anxious and depressed children. J Child Adolesc Psychopharmacol 15:571–580
Acknowledgments
This study was supported by grants BS02002-3850 and SEJ2005-01786 of the Ministry of Science and Technology, Spain. We wish to thank the City Council and Educational and Health Centers of Badía del Vallés for their support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ezpeleta, L., Granero, R., de la Osa, N. et al. Risk factor clustering for psychopathology in socially at-risk Spanish children. Soc Psychiat Epidemiol 43, 559–568 (2008). https://doi.org/10.1007/s00127-008-0312-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-008-0312-6