Abstract
Background
Parental and child psychiatric disorders have been found to be associated, and this association can be mediated by other psychosocial variables, including parenting attitudes and strategies. As most previous studies included clinical samples, the purpose of this study was to establish the relationship between parental psychopathology and parenting strategies with child psychiatric disorders in a national survey population.
Methods
The sample included 10,438 children of 5–15 years and their parents, from representative UK households. Families were assessed on child psychiatric diagnosis, parental psychopathology, family functioning, and socioeconomic status. Parenting strategies included using rewards, physical and non-physical punishments towards their child.
Findings
Parental psychopathology scores (OR 3.99, 95% CI 3.13–5.09) and non-physical punishment (OR 1.50, 95% CI 1.27–1.76) were associated with child psychiatric disorders. This association was particularly prominent among children with conduct disorders: parental psychopathology scores (OR 3.13, 95% CI 2.28–4.30) and non-physical punishment (OR 3.19, 95% CI 2.55–3.97). Absence of child psychopathology was associated with a combination of rewarding and non-punitive parenting strategies.
Conclusions
Although parents in the general population may be using less physical strategies than in the past, non-physical punishment is strongly related to mental health problems in children. Enhancement of positive parenting through universal and targeted interventions is an important preventive strategy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The association between parental and child psychiatric disorders is well established [18, 25]. The psychological and social development of children of mentally ill parents is at high-risk of a range of emotional, behavioural, cognitive and social difficulties [15, 31]. Furthermore, children of mentally ill parents are more likely to lack adequate support, care provision and access to services [7, 19, 21].
This relationship between parental and child psychopathology has been found to be confounded by family discord [26] and socioeconomic adversity [4]. Less is known on the relationship between adult psychopathology and parenting attitudes or strategies, and how these impact on children’s mental health [2]. Some studies established a mediating role of negative parenting attitudes [12], which themselves were predicted by previous life events and adversities [13, 24]. In a sample of mentally ill mothers, permissive parenting style was related to higher symptoms of adolescent depression and anxiety, while a positive and directive parenting style was related to fewer symptoms of depression [22]. Parents’ perceptions of reasons involved included problems with diagnosis and treatment, stigma, interpersonal difficulties, social supports, strain of parenthood and custody issues [1, 23]. Children’s own perceptions and attributions of parents’ symptoms, behaviours and illness are also contributing variables [28], as well as their coping strategies in processing and responding to adult symptoms of mental illness [14].
Several previous studies were confined to clinical samples and were based on information from adults [20, 21]. An analysis of the 1970 British national cohort accounted for these methodological constraints, and found that maternal authoritarian attitudes predicted conduct problems in children, independently of socio-economic status and maternal psychopathology [30]. In a retrospective descriptive survey, adults who reported having been slapped or spanked as children in Canada had a significantly higher prevalence of psychiatric disorders than those who had not [16].
Previous research thus indicates the importance of studying the impact of parenting on children’s mental health. As child-rearing attitudes can reflect societal changes, it is important that new information reflects such current family and parent characteristics. Therefore, the rationale for this study was to investigate the association between parental psychopathology, parenting strategies and child mental health in a representative UK sample of families. An advantage over previous cohorts was the use of detailed diagnostic measures collected from different informants, including young people themselves, and the selections of different age groups from childhood to adolescence. The purpose of this study was to establish the relationship of parental psychopathology and parenting strategies with child psychiatric disorders in a national survey population.
Method
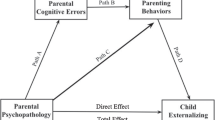
It was hypothesised that parental psychopathology would be associated with the main types of child psychiatric disorders, and that this association would be significantly mediated by punitive parenting strategies.
Sample
The main aspects of the study design are summarised here, with a more detailed account of the survey methodology available from Meltzer et al. [17]. As most children in Great Britain are entitled to benefits, i.e., financial contributions/support from the state (unless placed with a foster family or in a residential unit), the GB Child Benefit Register centralised computerised records which were used as the sampling frame of all children between 5 and 15 years living in England, Wales and Scotland. Of the 8,265 postal sectors of the country, 475 sectors were selected at random, with a probability proportional to the size of the sector. A letter was sent to the parents/carers of 14,250 children, or 30 children in each of the 475 postal sectors. There were 931 (6.5%) refusals, and 790 (5.5%) families were excluded from the study, mainly those who had moved and could not be traced (629 or 4.4%), as well as children in care or outside the age range. Of the 12,529 eligible children, information from interviews was collected on 10,438 (83%) children. The study received research ethics approval, and all procedures were in accordance with ethical standards.
Measures
The Development and Well-Being Assessment (DAWBA) [11] was used to establish psychiatric diagnoses based on both DSM-IV and ICD-10 diagnostic criteria for research. The assessment was administered by trained interviewers to parents. The comparable DAWBA adolescent interviews were only administered to the 11–15 year olds. Questions on common psychiatric symptoms and their impact were followed by open-ended questions and supplementary prompts. A teacher questionnaire on common psychiatric symptoms and their impact was also administered, and data from all informants were combined to produce computer-generated diagnoses. All interview data were subsequently reviewed by experienced clinicians who confirmed or overturned the computer-generated diagnoses. The main types of disorders are reported in this paper, i.e., conduct, emotional and hyperkinetic disorders.
The General Health Questionnaire (GHQ) [10] was used to assess common mental health problems (depression, anxiety, somatic problems or social dysfunction) among parents. Mothers were available for the interviews in over 95% of the subjects. The GHQ is a standardised and widely used 12-item self-report instrument, with established cut-off scores indicating psychiatric morbidity.
Parenting strategies: In order to examine how parents reward their children for good behaviours and punish them for negative behaviours, parents were asked to rate the frequency with which they use three types of rewards and six types of punishments (non-physical and physical). Parents reported whether they ‘never’, ‘seldom’, ‘sometimes’ or ‘frequently’ used each one. These were grouped in two categories, ‘never/seldom using this strategy’ and ‘sometimes/frequently using this strategy’. Rewards strategies included, giving encouragement or praise; giving treats such as extra pocket money, staying up late or a special outing; and giving the child favourite objects (such as toys or sweets). Punishment regimes (non-physical) included, sending child to his/her room; grounding or keeping him/her in; and shouting or yelling at him/her. And physical punishments were, smacking him/her; hitting him/her with a strap or something else; shaking him/her. Variables were analysed both as individual items and total rewards or punishments scores.
The General Functioning Scale of the McMasters Family Assessment Device (FAD) [8] was completed by parents. This assesses the level of the family discord and includes 12 items, scored on a 1–4 scale, with a total score 0–48, with family functioning being classified as ‘healthy’ or ‘unhealthy’.
Socio-demographic data was collected from parents.
Statistical analysis
Exploratory analysis: relationship between parenting items and child psychiatric disorders
The association between individual risk factors (as established by previous research) and each of the main categories of child psychiatric disorders (dependent variable) was investigated by univariate logistic regression analyses. Those variables that were significantly associated with a diagnostic category were entered in a multivariate model, with parenting items as covariates.
Primary analysis: relationship between rewarding or punitive categories and child psychiatric disorders
Parenting items were then grouped in three categories, reward, physical punishment and non-physical punishment. Each category was dichotomised into ‘high’ if a parent used two out of the three strategies in this category, and ‘low’ if they used one strategy, i.e., ‘high/low reward, high/low physical punishment and high/low non-physical punishment’. The multivariate models were repeated, with parenting categories as the covariates.
Secondary analysis: relationship between combined parenting categories and child psychiatric disorders
As parents may concurrently use reward and punishment (physical/non-physical), eight parenting ‘types’ were established for all possible combinations of the parenting categories (combination of high/low severity and rewarding/physically punitive/non-physically punitive categories), and were entered in multivariate models.
Results
The prevalence for any psychiatric disorder was 9.5% [22]. Prevalence rates of the main disorders were, conduct disorders 5.3%, emotional disorders 4.3% and hyperkinetic disorders 1.4%.
Primary analysis: relationship between rewarding or punitive categories and child psychiatric disorders
Parental psychiatric morbidity (GHQ scores within the clinical range 9–12) was associated with most types of disorder (separate univariate logistic regression models), i.e., any psychiatric disorder odds ratio (OR) 5.55, 95% CI 4.46–6.92, P=0.001; conduct disorder OR 5.17, 95% CI 3.91–6.85, P=0.001; and emotional disorder OR 6.35, 95% CI 4.80–8.39, P=0.001. Hyperkinetic disorder was predicted by lower GHQ scores (6–8): OR 3.03, 95% CI 1.88–4.90, P=0.001. As a number of socio-demographic variables (child’s gender, child’s age, family income, family type and family functioning score) were also independently associated with child psychiatric disorders in series of univariate logistic regression analyses, these variables were included in the next stage of multivariate logistic regression as potential confounding factors (the results of univariate tests are not reported in detail).
A series of multivariate analyses were subsequently conducted, with parental psychiatric (GHQ) ratings as the independent variable, and parenting strategies (treated as individual items), family functioning (FAD) type and socio-demographic variables as the covariates. A ‘best’ multivariate model was established for each child diagnostic category (according to R-squared score and level of significance).
The best multivariate model for any psychiatric disorder (Table 1) included the variables of parental psychiatric morbidity (GHQ), grounding the child (depriving of favourite outings or habits), sending the child to his/her room, age 11–15 years, male gender of child, low family income, family type of lone or cohabiting parent and unhealthy family functioning (model significant P<0.001; Nagelkerle R-squared score 0.132).
The same variables, with the addition of shouting and smacking, were significantly associated with conduct disorder (Table 2—model significant P<0.001; Nagelkerle R-squared score 0.178).
Hyperkinetic disorder was associated with parental GHQ scores 6–8 (OR 2.51, 95% CI 1.53–4.11, P=0.001), sending child to their room (OR 2.01, 95% CI 1.42–2.84, P=0.001), male gender (OR 5.22, 95% CI 3.27–8.34, P=0.001) and unhealthy family functioning (OR 2.00, 95% CI 1.38–2.89, P=0.001). The model was significant at P<0.001; Nagelkerke R-squared 0.092.
Emotional disorder was associated with parental GHQ scores 6–8 (OR 3.08, 95% CI 2.28–4.15, P=0.001) and scores 9–12 (OR 5.05, 95% CI 3.74–6.83, P=0.001), grounding child (OR 1.30, 95% CI 1.05–1.60, P=0.015), 11–15 years age (OR 1.59, 95% CI 1.29–1.95, P=0.001), low weekly family income (<£199) (OR 1.96, 95% CI 1.46–2.95, P=0.001) and unhealthy family functioning (OR 1.45, 95% CI 1.15–1.83, P=0.001). The model was significant at P<0.001; Nagelkerke R-squared 0.091.
Primary analysis: relationship between rewarding or punitive categories and child psychiatric disorders
High use of non-physical punishment was significantly associated with all disorders, particularly conduct disorders. The best models for any psychiatric diagnosis (high non-physical punishment OR 1.50, 95% CI 1.27–1.76, P=0.001; R square 0.132) and conduct disorder (high non-physical punishment OR 3.18, 95% CI 2.55–3.97, P=0.001; R square 0.171) are presented in Tables 3 and 4.
The variables associated with hyperkinetic disorder, were: parental GHQ score 6–8, OR 2.49, 95% CI 1.52–4.09, P=0.001; high non-physical punishment OR 2.16, 95% CI 1.50–3.11, P=0.001; male gender OR 5.11, 95% CI 3.19–8.16, P=0.001, unhealthy type of family functioning OR 1.89, 95% CI 1.30–2.75, P=0.001 (model P<0.001; Nagelkerke R square 0.091).
The variables associated with emotional disorder, were: parental GHQ score 6–8, OR 3.09, 95% CI 2.29–4.17, P=0.001; parental GHQ score 9–12 OR 5.08, 95% CI 3.75–6.86, P=0.001; high non-physical punishment OR 1.36, 95% CI 1.11–1.67, P=0.003; age 11–15 years OR 1.65, 95% CI 1.33–2.01; P=0.001; low income OR 1.99, 95% CI 1.48–2.68, P=0.001; and unhealthy type of family functioning OR 1.44, 95% CI 1.14–1.81, P=0.002 (model P<0.001; Nagelkerke R square 0.091).
Secondary analysis: relationship between combined parenting categories and child psychiatric disorders
In this tentative analysis, the concurrent use of rewards and punishments was associated with the presence of psychiatric disorders: high reward/high non-physical punishment/low physical punishment (OR 2.00, 95% CI 1.40–2.87, P<0.001); high reward/high non-physical punishment/high physical punishment (OR 4.42, 95% CI 1.77–11.04, P=0.001). Interestingly, absence of any psychiatric disorder was significantly associated with the combination of high reward/low non-physical/low physical punishment (OR 4.73, 95% CI 2.02–11.12, P=0.001).
DISCUSSION
This general population study established an association between parental psychopathology and use of punitive parenting strategies with child psychiatric disorders, particularly conduct disorders. This relationship was previously established in studies with high-risk families, such as those with mentally ill parents [12]. The emerging evidence indicates that the three variables are inter-related, and that the underlying mechanisms are more complex than a linear relationship between parental and child disorders, with other confounding psychosocial and child- related factors also involved [9, 16].
The study has a number of limitations, mainly the lack of observational parenting instruments (which may have detected higher rates of physical punishment strategies) and adult psychiatric diagnostic interviews. Another limitation was the failure to establish severity of psychopathology and parenting strategies in both parents, but attempts to obtain data directly from fathers in large community samples such as ours are liable to fail, with low response rates and an unrepresentative sample of fathers. Large-scale epidemiological studies of this kind inevitably cannot use detailed measurements and are constrained by their cross-sectional design; however, they can test hypotheses at a population level generated by previous smaller-scale research in a statistically more powerful way. A longitudinal design would have enabled the investigation of the predictive value of the key variables, including the potential reverse or contributing effect of child behaviour on parent-related outcomes. For example, it maybe that some parents who find it difficult to deal with children’s behaviours develop more anxiety and depressive symptoms, consequently use more punitive strategies, not being able to break this escalating family pattern. Such associations should therefore be interpreted with caution [20]. Future research could investigate the impact of parenting types in more detail, as well as the relationship between attachment and later parenting types among high-risk parents such as those with mental health problems [6].
The findings highlight societal changes in parenting attitudes towards punishment, with the predominant use of non-physical strategies. However, the impact of non-physical punishment is not necessarily lesser. The reverse finding is particularly important in considering implications for prevention and treatment. The combination of using rewarding strategies, without either physical or non-physical punishment, was found to be strongly associated with the absence of mental health problems in children.
Although beyond the direct remit of this study, there are implications for different levels of parent education, support and specialist intervention [29]. These should aim to enhance positive parenting such as the use of rewarding strategies, and reduce punitive and rejecting attitudes towards children. Programmes could respectively target all parents, families at risk, and parents with established mental illness, preferably on a service continuum, depending on families’ level of need. Such a comprehensive parenting programme has been described and evaluated in Australia, which encompasses prevention, secondary and tertiary treatment, with families moving flexibly between different programme components, as appropriate [27]. Parents with mental illness may require more intensive and specialist interventions [5]. There is also a requirement for closer links between child and adult mental health services [3, 19].
In conclusion, negative parenting attitudes, involving physical and non-physical punishment, were associated with both parental and child mental health problems, and were mediated by other family and socioeconomic factors, in a national survey population. Parenting styles combining the use of rewards and the lack of punishment were strongly associated with absence of child psychiatric disorders. The findings have implications for a range of health and welfare agencies and professionals planning universal and targeted preventive programmes, as well as secondary interventions for children, young people and their families.
References
Ackerson B (2003) Coping with the dual demands of severe mental illness and parenting: the parents’ perspective. Fam Soc 84:109–118
Berg-Nielsen T, Vikan A, Dahl A (2002) Parenting related to child and parental psychopathology: a descriptive review of the literature. Clin Child Psychol Psychiatr 7:529–552
Brunette M, Dean W (2002) Community mental health care for women with severe mental illness who are parents. Community Mental Health J 38:153–165
Canino G, Bird H, Rubio-Stipec M, Bravo M, Alegria M (1990) Children of parents with psychiatric disorders in the community. J Am Acad Child Adol Psychiatr 29:398–406
Craig E (2004) Parenting programmes for women with mental illness who have young children. Austr New Zeal J Psychiatr 38:923–928
Cunningham J, Harris G, Vostanis P, Oeybode F, Blissett J (2004) Children of mothers with mental illness: attachment, emotional and behavioural problems. Early Child Dev Care 174:639–650
Cunningham J, Oyebode F, Vostanis P (2000) Children of mothers admitted to psychiatric hospital: care arrangements and mothers’ perceptions. Child Psychol Psychiatr Rev 5:114–119
Epstein N, Baldwin L, Bishop D (1983) The McMaster Family Assessment Device. J Mar Fam Therapy 9:171–180
Ford T, Goodman R, Meltzer H (2004) The relative importance of child, family, school and neighbourhood correlates of childhood psychiatric disorder. Soc Psychiatry Psychiatr Epidemiol 39:487–496
Goldberg D, Williams P (1988) User’s guide to the general health questionnaire. NFER-Nelson, Windsor
Goodman R, Ford T, Richards H, Gatward R, Meltzer H (2000) The development and well-being assessment: description and initial validation of an integrated assessment of child and adolescent psychopathology. J Child Psychol Psychiatr 41:645–655
Johnson J, Cohen P, Kasen S, Smailes E, Brook J (2001) Association of maladaptive parental behaviour with psychiatric disorder among parents and their offspring. Arch Gen Psychiatr 58:453–460
Kettinger L, Nair P, Schuler M (2000) Exposure to environmental risk factors and parenting attitudes among substance-abusing women. Am J Drug Alcohol Abuse 26:1–11
Langrock A, Compas B, Keller G, Merchant M, Copeland M (2002) Coping with the stress of parental depression: parents’ reports of children’s coping, emotional, and behavioural problems. J Clin Child Adol Psychol 31:312–324
Leverton T (2003) Parental psychiatric illness: the implications for children. Curr Opin Psychiatr 16:395–402
MacMillan H, Boyle M, Wong M, Duku E, Fleming J, Walsh C (1999) Slapping and spanking in childhood and its association with lifetime prevalence of psychiatric disorders in a general population sample. Can Med Assoc J 16:805–809
Meltzer H, Gatward R, Goodman R, Ford T (2000) Mental health of children and adolescents in Great Britain. Office for National Statistics, London
Mordoch E, Hall W (2002) Children living with a parent who has a mental illness: a critical analysis of the literature and research implications. Archiv Psychiatric Nursing 16:208–216
Mowbray C, Lewandowski L, Bybee D, Oyserman D (2004) Children of mothers diagnosed with serious mental illness: patterns and predictors of service use. Mental Health Serv Res 6:167–183
Najman J, Williams G, Nikles J, Spence S, Bor W, O’Callaghan M, Le Broque R, Andersen M (2000) Mothers’ mental illness and child behaviour problems: cause-effect association or observation bias? J Am Acad Child Adol Psychiatr 39:592–602
Ostman M, Hansson L (2002) Children in families with a severely mentally ill member. Soc Psychiatry Psychiat Epidemiol 37:243–248
Oyserman D, Bybee D, Mowbray C (2002) Influences of maternal mental illness on psychological outcomes for adolescent children. J Adolescence 25:587–602
Oyserman D, Bybee D, Mowbray C, Kahng S (2004) Parenting self-constructs of mothers with a serious mental illness: efficacy, burden, and personal growth. J Appl Soc Psychol 34:2502–2523
Oyserman D, Mowbray C, Meares PA, Firminger K (2000) Parenting among mothers with a serious mental illness. Am J Orthopsychiatr 70:296–315
Ramchandani P, Stein A (2003) The impact of parental psychiatric disorder on children: avoiding stigma, improving care. BMJ 327:242–243
Rutter M, Quinton D (1984) Parental psychiatric disorder: effects on children. Psychol Med 14:853–880
Sanders M, Markie-Dadds C, Bor W, Tully L (2000) The Triple P-Positive Parent Programme: a comparison of enhanced, standard, and self-directed behavioural family intervention for parents of children with early onset conduct problems. J Consult Clin Psychol 4:624–640
Scherer D, Melloh T, Buyck D, Anderson C, Foster A (1996) Relation between children’s perceptions of maternal mental illness and children’s psychological adjustment. J Clin Psychol 25:156–169
Scott S (1998) Intensive interventions to improve parenting. Arch Dis Childhood 79:90–93
Thompson A, Hollis C, Richards D (2003) Authoritarian parenting attitudes as a risk for conduct problems: results from a British national cohort study. Eur Child Adol Psychiatr 12:84–91
Wang A, Goldschmidt V (1994) Interviews of psychiatric inpatients about their family situation and young children. Acta Psychiatr Scand 90:459–465
Acknowledgements
We are grateful to all the children, parents and teachers who took part in this study. This was funded by the British Department of Health and was carried out by the Office for National Statistics.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vostanis, P., Graves, A., Meltzer, H. et al. Relationship between parental psychopathology, parenting strategies and child mental health. Soc Psychiat Epidemiol 41, 509–514 (2006). https://doi.org/10.1007/s00127-006-0061-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-006-0061-3