Abstract
Background
There has been a relative lack of epidemiological data on generalised anxiety disorder (GAD) in Southeast Asia. A previous study reported a lifetime prevalence of 1.5% and highlighted low preference for seeking professional help and consultation by persons suspected to be suffering from mental health problems. The present study is part of a National Mental Health survey of adults conducted from February 2003–March 2004 specifically assessing anxiety and depression in Singapore. In this paper we report on prevalence, co-morbidity and risk factors associated with GAD.
Methods
We interviewed 2,847 households from an ethnically stratified random sample of adults aged 20–59 years who were Singapore citizens or permanent residents. The General Health Questionnaire and Schedule for Clinical Assessment of Neuropsychiatry were administered, which generated Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) diagnoses of GAD. We assessed socio-demographic correlates, life events, medical and other psychiatric co-morbidities related to GAD.
Results
Lifetime prevalence of GAD was 3.3%, current prevalence is 3.0%. Female to male ratio is 3.6:1. GAD was significantly associated (p<0.001) with the presence of other psychiatric co-morbidities, including major depressive disorder, dysthymia, panic disorder, agoraphobia and social phobia. Prevalence increased in older individuals, with the odds of association greatest in subjects with three or more co-morbid medical conditions [adjusted odds ratio (OR) 3.66]. Those who had experienced one or more threatening life events showed increased odds of association with GAD. Chinese ethnicity, the divorced and persons from both the upper and the lowest socio-economic status had highest odds of association with GAD.
Conclusions
We challenge established notions that GAD tends to be a disorder of the socially disadvantaged. Life events are important as precipitating factors in GAD, and uniquely different types of events appear to affect both extremes of social classes. High co-morbidity associations with current GAD are grounds for concern. This may suggest failure to seek treatment, hence giving rise to an increase in severity of the primary condition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Generalised anxiety disorder (GAD) is a common lifetime condition associated with considerable disability [1, 2] and co-morbidity [3, 4]. In community samples, point prevalence of between 1.5 and 3% [2], 1-year prevalence of 3–5% [5] and lifetime prevalence of 4–7% [6] have been described. GAD runs a chronic course [6], characterised by periods of relapse and remission [7, 8], with evidence to suggest that persons with GAD are also at higher risk of poor physical health [9, 10]. While it has been well documented in Western psychiatric literature that GAD is more commonly diagnosed in females and among those with lower socio-economic status, the previously married, homemakers, the unemployed and retirees [2, 11, 12], there has been a relative lack of epidemiological data from countries in Southeast Asia.
In Singapore, an earlier population study [13] found a 1.5% prevalence of GAD. Moreover, there seemed to be a low preference for seeking professional help and consultation by persons suspected to be suffering from mental health problems [14].
This paper assesses the prevalence, co-morbidity, socio-demographic correlates and other risk factors associated with persons diagnosed with GAD.
Singapore is an island inhabited by a multi-ethnic, multi-cultural population of about four million persons. The main ethnic groups are the Chinese (77%), the Malays (14%) and the Indians (8%), with Eurasians and people of other descent comprising the remaining 1%. The Chinese and Indians were immigrants from China and the Indian subcontinent, respectively, around the nineteenth century. The Malays were historically the earliest inhabitants, originating from Yunnan province in southern China. In view of the relatively high cost of “landed” property such as bungalows, semi-detached houses or terrace houses compared to government built flats or private apartments, those living in such “landed” properties usually belong to the upper socio-economic group.
Method
Study design and subjects
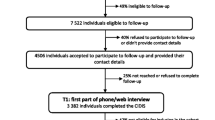
We analysed data collected from the National Mental Health Survey (Adults) of Singapore [NMHS(A)], a population-based survey of a national representative sample of adults aged 20–59 years, conducted from 15 February 2003 to 30 March 2004.
The sampling list for the study was obtained from household addresses randomly generated for the Ministry of Health National Health Survey of 2001. The random sample list was generated by the Department of Statistics using pure probability sampling from a national sampling frame based on population census of persons residing in coded districts throughout the country. The NMHS(A) used an ethnically stratified random sample of households to identify eligible adults aged 20–59 years who were Singapore citizens or permanent residents. The ethnic stratification ensured that about one third equal proportions of Chinese, Malay and Indian subjects were represented in the survey sample.
The survey was conducted in two phases. In the first enumeration phase, letters were sent to the selected households informing householders of the survey before field interviewers visited them, explained the purpose of the survey, enumerated all household members, and recorded enumeration information from each member on name, position in household, age, sex, ethnicity and citizenship/permanent resident status. Family members who were admitted into nursing homes/institutions were also identified.
The eligibility of each member of the household was determined by the following criteria: aged between 20 and 59, citizens or permanent residents of Singapore, and not incapacitated or mentally unfit to answer the interview questions for reasons such as severe stroke aphasia or dementia, cachexia, coma etc. Foreign domestic workers and subtenants (i.e. tenants who sublet their dwellings to other tenants) did not qualify for the interview. One eligible person per household was randomly selected from the household enumeration list for invited participation in the study.
Subjects gave written informed consent. The survey was approved by the Institute of Mental Health (IMH) ethics committee. Subjects who refused participation were replaced by another member of the family or persons living next door to the initially intended household.
In the second phase of the survey, selected subjects were informed by letter before a multi-ethnic team of trained field interviewers visited them at home and administered the survey questionnaires. The interviews were conducted in the language or dialect with which the subjects were most conversant: English, Mandarin or other Chinese dialects, and Malay. Indian subjects were interviewed in either English or Malay, as they were mostly conversant in either language.
Survey instruments
General health questionnaire (12 items)
Participating householders were screened for mental disorders using the 12-item General Health Questionnaire (GHQ-12) [15]. The questionnaire is rated on a 4-point response scale, and symptoms were scored as absent or present using a bimodal method (“not at all” = 0, “same as usual” = 0, “more than usual” = 1 and “much more than usual” = 1). The GHQ-12 has been translated into 11 languages and has demonstrated stable discriminating power cross-culturally [16]. The validity of this instrument has been demonstrated in previous studies in Singapore [17, 18].
All subjects with GHQ scores of at least 2 were further interviewed using the Schedule for Clinical Assessment in Neuropsychiatry (SCAN) [19] to derive the diagnosis of GAD. With this optimum cut-off determined from receiver operating characteristic analyses, the GHQ-12 scale gave a sensitivity of 92.1% and specificity of 48.1 for depression/anxiety, while positive predictive value of subjects with GHQ of at least 2 was 31%. In addition, random one-in-ten subjects with GHQ-12 scores below 2 were further interviewed using the SCAN. This was intended to address the remote possibility of false-negative results from low scorers on the GHQ-12.
Schedule for clinical assessment in neuropsychiatry
The aim of a set of instruments, SCAN, is to assess, measure and classify the psychopathology and behaviour associated with the major psychiatric syndromes in adulthood. It has its origins in the Present State Examination (PSE) [20]. SCAN version 2.1 comprises four components: the tenth edition of the PSE (PSE 10), which is its core content; the Glossary of Differential Definitions; the Item Group Checklist (IGC), for detailed definitions of symptoms; and the Clinical History Schedule (CHS), consisting of items on clinical history that rate the presence or absence of disorders. The PSE 10 has two parts. Part one covers somatoform, dissociative, anxiety, depressive and bipolar disorders, and problems associated with basic bodily functions and use of alcohol and other substance use. Part two covers psychotic and cognitive disorders and observed abnormalities of speech, affect and behaviour. SCAN is intended for use by clinicians with an adequate knowledge of psychopathology who have taken a course at a World Health Organization (WHO)-designated training centre. Case diagnoses are generated in accordance with International Statistical Classification of Disease, 10th Revision (ICD-10) [21] and Diagnostic and Statistical Manual of Mental Disorders, Revised Third Edition (DSM-III-R) or Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) [22] criteria. In this study the diagnoses were based on DSM-IV criteria. SCAN has been found to be generally acceptable, appropriate and reliable across cultures and settings [23] when administered by trained lay interviewers in community surveys [24, 25].
Our interviewers were trained in the use of the SCAN by a senior psychiatrist who had received training from a WHO training centre. Each interviewer received a total of 6 h of training, conducted over several weeks, which included didactic teaching, discussion and practice interviews with out-patients from the IMH with clinical diagnoses of anxiety and depressive disorders and who agreed to take part in the sessions. The multi-ethnic interviewers were experienced psychiatric nurses from the IMH. The inter-rater reliability of the SCAN results conducted by the interviewers and the trainer was good to excellent, with kappa values ranging from 0.63 for major depressive episodes to 0.78 for GAD. The interviewers were supervised every week, and survey data were proofread by the research coordinator and supervising psychiatrists. In addition, at random intervals, the research coordinator accompanied field workers to ensure that interviews were conducted in accordance with the study protocol, and that diagnoses were accurately made.
Data on socio-demographic variables included gender, age, ethnicity, marital status, education, employment status, income, housing type (as a surrogate of socio-economic status), religion and living arrangement. We took a detailed medical history to enquire about the presence of 16 specific and other chronic medical conditions, medications and whether there was a family history of mental illness.
List of threatening experiences questionnaire
Subjects who were interviewed with SCAN (N=895) were also asked whether they had experienced any life events in the previous 6 months from a List of Threatening Experiences Questionnaire (LTEQ) [26]. The LTEQ lists 12 items of life events, and the total number of reported threatening experiences was computed for each subject.
Statistical analyses
Crude population prevalence estimates of GAD, extrapolated from the sample estimates, were obtained using weighted estimation procedures, given the ethnically stratified disproportionate sampling employed. The proportions of GAD cases among subjects with a GHQ score less than 2 in the total sample were estimated from the random subsample estimates and included in the overall population estimates.
The analyses of risk factors associated with GAD were performed by comparing subjects with a SCAN diagnosis of recent GAD (N=76) (i.e. those with symptoms of GAD in the last 1 month) and those without (N=2,771). Crude and adjusted odds ratio (OR) [point estimates and their 95% confidence intervals (CIs)] were calculated in univariate and multivariable logistic regression analyses. Weighted analyses were performed for logistic regression, with all explanatory variables entered in full saturated models. Two final models are presented, one based on the full sample (N=2,847), omitting the LTE-Q variable (Model 1), and another based on the subsample (N=895) of subjects with available data on LTE-Q (Model 2). For clarity and simplicity, only the ORs of significant explanatory variables are shown for these models.
Data were analysed using Statistical Package for the Social Sciences (SPSS) version 12 and the Confidence Interval Analysis (CIA).
Results
There were 2,847 persons who agreed to be interviewed from a total of 3,875 randomly selected eligible persons, a response rate of 75.2%. The crude lifetime prevalence of GAD was 3.3% (95% CI 2.4–4.2); point prevalence of recent GAD (i.e. symptoms in the 1 month prior to interview) was 3.0% (95% CI 2.1–3.9). The overall female to male ratio was 3.6:1 (Table 1). Recent GAD was significantly associated (p<0.001) with the presence of other recent psychiatric co-morbidities, including major depressive disorders, dysthymia, panic disorder, agoraphobia and social phobia (please refer to Table 2).
The results of the frequencies of potential risk factors and their associations with GAD are shown in Tables 3 and 4. As expected, female gender was a strong determinant of GAD, as shown in both univariate and multivariate ORs (3.5 and 3.7, p<0.001), independently of other factors. Older age was significantly associated with lifetime in crude estimates of associations but was not found to be an independent explanatory factor after adjustment for confounding variables.
Ethnicity was significantly and strongly associated with GAD, independently of other factors in multivariate analyses. Significantly higher odds of association with GAD was observed for Chinese ethnicity (adjusted OR 2.4 in Model 1 and OR 4.7 in Model 2), but not Indian ethnicity, when compared to Malay ethnicity which had the lowest prevalence.
Socio-economic status was consistently demonstrated by surrogate indices of income, housing type and employment to be associated with GAD in univariate analyses. Compared to middle-income or intermediate socio-economic groups which appeared to have the lowest rate of GAD, those in the lowest and highest income and socio-economic groups appeared to show greatest odds of association with GAD. In multivariate analyses that adjusted for the influence of other factors, only the highest socio-economic group who lived in a landed housing type was shown to have significantly highest odds of association with GAD (OR 9.17). Being divorced was strongly associated with GAD in both univariate (OR 10.2, p<0.001) and multivariate analyses (OR 9.3, p<0.001).
Higher odds of association were found between GAD and having a religion (OR 4.21), particularly Buddhism and Christianity.
Table 5 demonstrates the presence of certain medical conditions, for example coronary artery disease and chronic obstructive pulmonary disease (COPD), to be significantly associated with GAD, with the odds of association greatest in subjects with three or more co-morbid medical conditions (adjusted OR 3.66).
The association of life events with GAD was analysed in a subsample of subjects (N=895) (Model 2). Persons who reported life events in the previous 6 months were more likely to be diagnosed with GAD (p<0.001), with greater odds of association observed in those with one and two or more events (OR 2.39 and 2.87).
Discussion
The associations between GAD and certain at-risk socio-demographic factors have been well described in literature. Our findings are in accordance with these risk factors with some exceptions. The prevalence of our GAD sufferers seemed to rise with age, a finding shared with other researchers [2].The association with age could have been mediated by other biological, social and health-related correlates of GAD.
Our female to male ratio of 3.6:1 is more than the usual 2:1 in most studies. Several explanations are proposed. Firstly, there can indeed be a higher female preponderance of GAD in Singapore than elsewhere. Secondly, males with GAD were more likely to refuse participation in the study. Thirdly, as the aim of the study was primarily at assessing prevalence of anxiety and depressive disorders, we did not assess the prevalence of co-morbid alcohol or substance abuse disorders. Had we measured primarily the prevalence of substance abuse disorders, we would also have captured symptoms of GAD in males. Hence, these factors might have been responsible for spuriously elevating the female to male ratio. In contrast to the association of age with GAD, the strong association of female gender with GAD, independent of other social and health-related factors, suggests that gender-related factors that were not measured in this study might have been relevant.
While we were able to confirm an expected strong association of GAD with divorce and separation, we found no association with widowed status. This can be attributed to favourable levels of social and financial support accorded the bereaved, or that bereavement might be associated more with depressive disorders than with GAD.
In this study population, we found that socio-economic status, as measured by both income levels and type of housing, were both consistently associated with GAD in an interesting way. We observed consistently a U-shaped relationship between socio-economic status and GAD. Subjects in both socio-economic extremes, the poorest and the wealthiest, had higher rates of GAD, whereas subjects in the intermediate group were least likely to report GAD. This has been rarely described in psychiatric literature.
Persons in the highest and lowest socio-economic groups also had significantly more experience of threatening life events (Table 6). In particular, poorer subjects reported significantly more serious illness to self, being unemployed, being dismissed from a job, and problems with the law than other subjects. The wealthiest reported significantly more adverse experiences with relationships and a threat of loss of loved ones (illnesses to close relatives, serious relationship problems with close friends or relatives and bereavement), and both groups reported significantly more financial crises.
Exposure to threat of loss and danger events have been associated especially with GAD [27–29]. As the LTEQ asked for life events during the 6 months prior to interview, and because GAD, by definition, requires 6 months duration of symptoms, we need to consider whether life events precipitated the onset of GAD or whether GAD could have also resulted in certain life events, e.g. being dismissed from a job. However, certain types of life events, e.g. serious injury or sickness in family, would most likely precede the onset of GAD. We observed that certain medical conditions, including coronary artery disease, asthma, COPD and arthritis, were significantly associated with elevated odds of GAD. Such associations have been well described [30–33] In our present survey, the self-reporting of medical conditions can be subject to reporting bias. To avoid this we asked subjects to allow inspection of their medications. On the other hand, studies have shown that self-reported information were accurate for certain medical disorders such as diabetes and hypertension [34].
We confirmed strong co-morbidity between GAD and other psychiatric disorders, with some 85% of recently diagnosed GAD sufferers and some 93% persons with lifetime GAD having a co-morbid psychiatric condition. The possible explanation for such high co-morbidity associations is the reluctance to seek psychiatric help, which might result in a worsening of the primary condition.
The relationship between race, religion and mental illness in a multi-ethnic, multi-religious society is a complex one. In Singapore, religious affiliation is deemed to be highly related to ethnicity. Malays almost exclusively embrace the Muslim faith; most Indians embrace Hinduism, with lesser numbers Islam and Christianity, whereas Chinese are diversely devoted to Buddhism, Taoism or Christianity. The distinction between Taoism and Buddhism is often unclear, as the Chinese historically practise a syncretic mix of Buddhism and Taoism. The association between anxiety disorder and religion is not surprising, given that distressed individuals are more likely to seek spiritual help and embrace certain religious faiths.
Conclusion
Although GAD prevalence in Singapore, a Southeast Asian country, may appear to be similar in prevalence, co-morbidity and socio-demographic correlates from those reported elsewhere, there are distinct exceptions which we have highlighted. The upper socio-economic groups and the Chinese are more likely to be identified with GAD. This poses a challenge to established notions that GAD tends to be a disorder of the socially disadvantaged. Threatening life events are particularly associated with GAD. Physical conditions might precipitate GAD or vice versa. The association between certain physical conditions and GAD is still poorly understood and merits further study. Our survey has implications for service provision and emphasises the necessity of detecting and treating GAD, especially in patients with certain medical conditions. Traditionally, services have tended to cater to the underprivileged. It would be wise to address the mental health needs of the upper social classes as well.
References
Wittchen H-U, Carter RM, Pfister H et al (2000) Disabilities and quality of life in pure and comorbid generalised anxiety disorder and major depression in a national survey. Int Clin Psychopharmacol 15:319–328
Wittchen HU, Zhao S, Kessler RC, Eaton WW (1994) DSM-III-R generalised anxiety disorder in the National Comorbidity Survey. Arch Gen Psychiatry 51(5):355–364
Goisman RM, Goldenberg I, Vasile RG, Keller MB (1995) Comorbidity of anxiety disorders in a multi centre study. Compr Psychiatry 36:303–311
Noyes R Jr (2001) Comorbidity in generalised anxiety disorder. Psychiatr Clin North Am 24:41–55
Kessler RC, Dupont RL, Berglund P et al (1999) Impairments of twelve-month independent and comorbid generalised anxiety disorder and major depression in two national surveys. Am J Psychiatry 156:1915–1923
Blazer DG, Hughes D, George LK et al (1991) Generalised anxiety disorder. In: Robins LN, Regier DA (eds) Psychiatric disorders in America. The Free Press, New York, 180–203
Kessler RC, Wittchen H-U (2002) Patterns and correlates of generalised anxiety disorder in community samples. J Clin Psychiatry 63(Suppl 8):4–10
Keller MB (2002) The long-term clinical course of generalised anxiety disorder. J Clin Psychiatry 63(Suppl 8):6–11
Anderson DJ, Noyes R Jr, Crowe RR (1984) A comparison of panic disorder and generalised anxiety disorder. Am J Psychiatry 141:572–575
Barlow DH, Blanchard EB, Vermilyea JA et al (1986) Generalised anxiety and generalised anxiety disorder: description and reconceptualization. Am J Psychiatry 143:40–44
Coryell W, Noyes RJ, House J (1986) Mortality among outpatients with anxiety disorders. Am J Psychiatry 143:508–510
Kessler RC et al (2002) Generalized anxiety disorder in primary care: prevalence, recognition, and management. J Clin Psychiatry 63(Suppl 8):24–34
Fones CSL, Kua EH, Ng TP, Ko SM (1998) Studying the mental health of a nation: a preliminary report on a population survey in Singapore. Singapore Med J 39(6):251–255
Ng TP, Fones CSL, Kua EH (2003) Preference, need and utilisation of mental health services, Singapore National Mental Health Survey. Aust N Z J Psychiatry 37:613–619
Goldberg D, Williams P (1988) A user's guide to the General Health Questionnaire. NFER-Nelson, Berkshire, UK
Luo N, Fones CS, Thumboo J, Li SC (2004). Factors influencing health-related quality of life of Asians with anxiety disorders in Singapore. Qual Life Res 13(2):557–565
Boey KW (1999) Distressed and stress resistant nurses. Issues Ment Health Nurs 20(1):33–54
Üstün TB, Sartorius N (1995) Mental illness in general health care: an international study. Wiley, Chichester
World Health Organization (1994) Schedules for clinical assessment in neuropsychiatry (SCAN). American Psychiatric Research, Washington, DC
Wing JK (1960) The measurement of behaviour in chronic schizophrenia. Acta Psychiatr Neurol 35:245–254
World Health Organization (1992) International Classification of Diseases and Related Health Problems, 10th revision. World Health Organization, Geneva
American Psychiatric Association (1994) Diagnostic and Statistical Manual of Mental Disorders, 4th edn (DSM-IV). American Psychiatric Association, Washington, DC
Janca A et al (1994) New versions of world health organisation instruments for the assessment of mental disorders. Acta Psychiatr Scand 90:73–83
Rijnders CA, van den Berg JF, Hodiamont PP, Nienhuis FJ, Furer JW, Mulder J, Giel R (2000) Psychometric properties of the schedules for clinical assessment in neuropsychiatry (SCAN- 2.1). Soc Psychiatry Psychiatr Epidemiol 35(8):348–352
Brugha TS, Nienhuis F, Bagchi D, Smith J, Meltzer H (1999) The survey form of SCAN: the feasibility of using experienced lay survey interviewers to administer a semi-structured systematic clinical assessment of psychotic and non-psychotic disorders. Psychol Med 29(3):703–711
Brugha TS, Cragg D (1990) The list of threatening experiences: the reliability and validity of a brief life events questionnaire. Acta Psychiatr Scand 82(1):77–81
Kendler KS, Hettema JM, Butera F, Gardner CO, Prescott CA (2003) Life event dimensions of loss, humiliation, entrapment, and danger in the prediction of onsets of major depression and generalized anxiety. Arch Gen Psychiatry 60(8):789–796
Finlay-Jones R, Brown GW (1981) Types of stressful life event and the onset of anxiety and depressive disorders. Psychol Med 11(4):803–815
Blazer D, Hughes D, George LK (1987) Stressful life events and the onset of a generalised anxiety syndrome. Am J Psychiatry 144 (9):1178–1183
Goldberg RJ, Posner DA (1993) Anxiety in the medically ill. In: Stoudemire A, Fogel BS (eds) Psychiatric care of the medically ill patient. Oxford University Press, New York, pp 155–206
Harter MC, Conway KP, Merikangas KR (2003) Associations between anxiety disorders & physical illness. Eur Arch Psychiatry Neurosci 253:313–320
Katon W (1996) Panic disorder: relationship to high medical utilisation, unexplained physical symptoms, and medical costs. J Clin Psychiatry 57(Suppl 10):11–17
Karajgi B, Rifkin A, Doddi S, Kolli R (1990) The prevalence of anxiety disorders in patients with chronic obstructive pulmonary disease. Am J Psychiatry 147:200–201
Goldman N, Lin IF, Weinstein M, Lin YH (2003) Evaluating the quality of self-reports of hypertension and diabetes. J Clin Epidemiol 56:148–154
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lim, L., Ng, T.P., Chua, H.C. et al. Generalised anxiety disorder in Singapore: prevalence, co-morbidity and risk factors in a multi-ethnic population. Soc Psychiat Epidemiol 40, 972–979 (2005). https://doi.org/10.1007/s00127-005-0978-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-005-0978-y