Abstract
Background
International variation in compulsory admissions to psychiatric care has mainly been studied in terms of civil commitment rates. The objectives of this study were to compare and analyse the levels of perceived coercion at admission to psychiatric in-patient care among the Nordic countries and between centres within these countries, in relation to legal prerequisites and clinical practice.
Method
From one to four centres each in Denmark, Iceland, Norway, Finland and Sweden, a total of 426 legally committed and 494 formally voluntarily admitted patients were interviewed within 5 days from admission.
Results
The proportion of committed patients reporting high levels of perceived coercion varied among countries (from 49% in Norway to 100% in Iceland), and in Sweden, only, among centres (from 29 to 90%). No clear variations in this respect were found among voluntary patients. A wide concept of coercion in the Civil Commitment Act and no legal possibility of detention of voluntary patients were associated to low levels of perceived coercion at admission among committed patients.
Conclusion
For committed patients, differences in national legal prerequisites among countries were reflected in differences in perceived coercion. The results from Sweden also indicate that local care traditions may account for variation among centres within countries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Compulsory admissions to psychiatric hospitals differ substantially among and within countries [1–8], when the patient’s formal legal status is used as a measure for coercion. However, over the last 10–15 years several studies have shown that the formal legal status of the patient often differs from the patient’s perceptions of being coerced [9–17], and it has been argued that perceived coercion constitutes a more valid measure for coercion [18]. Accordingly, there is a growing literature on perceived coercion but little discussion about the interpretation of perceived coercion score levels and differences between local and international settings.
Variations in civil commitment rates are usually discussed in terms of differences in the coercive powers of various mental health acts [6–8]. As a part of the Nordic study on the use of coercion in the mental health care system [19], performed in all the five Nordic countries (Denmark, Finland, Iceland, Norway and Sweden), Nilstun and Syse [20] have analysed the Nordic mental health acts. They distinguish between a narrow and a wide concept of coercion, defined as follows. “According to the narrow concept, an intervention is coercive if, and only if, two conditions are satisfied: (1) the patient has no option (he or she will be hospitalised), and (2) the patient refuses hospitalisation or is incompetent to express an opinion (absence of protest is not enough)... According to the wide concept of coercion, an intervention is coercive if, and only if, the patient has no option (he or she will be hospitalised). This wide concept of coercion does not require that the patient refuses or is incompetent” [20]. In their analysis of the criteria for civil commitment in the Nordic mental health acts, Nilstun and Syse conclude that a narrow concept of coercion is used in the Danish, Icelandic and Swedish acts, but not in the Finnish and Norwegian. All Nordic mental health acts as authorized involuntary detention of voluntarily admitted patients, except in Norway where this is not permitted.
It is not known, however, whether levels of perceived coercion among psychiatric in-patients are related to the legal prerequisites for civil commitment. Knowledge about the patients’ own experiences of coercion and factors associated to such experiences are important for the development of the psychiatric clinical practice. The objectives of this article are to compare levels of perceived coercion, among committed and voluntary patients, at admission to psychiatric in-patient care across the five Nordic countries, and across centres within countries, and to analyse differences in perceived coercion in terms of legal prerequisites and differences in clinical practice.
The study is a part of the Nordic study on the use of coercion in the mental health care system. The Nordic study as a whole has been described by Høyer et al. [19], and more detailed descriptions of the Danish, Finnish, Norwegian and Swedish national studies are presented in previous articles [17, 21–24].
Methods
Settings and inclusion of participants
Twelve psychiatric hospitals (one in Denmark, three in Finland, one in Iceland, three in Norway and four in Sweden) participated in the study. The data collection was done in 1996–1997 in Denmark, 1996 in Finland, 1996–1997 in Iceland, 1997–1998 in Norway and 1997–1999 in Sweden. In Norway and Iceland, all consecutively admitted patients aged 18–60 were included, regardless of their legal admission status. In the other countries, all consecutively committed patients, and samples of voluntarily admitted patients, all aged 18–60, were included. The voluntary patients were either selected by including the next voluntarily admitted patient following each commitment (Denmark and Finland), or by selecting every nth consecutive patient admitted voluntarily (Sweden). Thus, two groups of patients were studied: legally involuntarily admitted patients (committed patients) and legally voluntarily admitted patients (voluntary patients). Due to the sampling methods in Denmark, Finland and Sweden, the proportion between committed and voluntary patients in our total sample does not reflect population-based admission rates of the two groups. Excluded in all countries were patients unable to communicate in the national language or unable to communicate due to clinical conditions, patients with a primary diagnosis of substance abuse, forensic patients and readmitted patients already are interviewed once.
Assessments
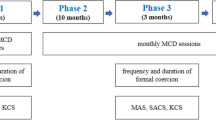
The participants were interviewed within 5 days of admission, using the Nordic Admission Interview, NorAI [19]. The interview starts with six questions concerning the admission, followed by a summary questions where the patient is asked to state if he or she came involuntarily or voluntarily to the hospital. The NorAI also includes a 10-step anchored visual analogue self-report scale on perceived coercion at admission, the Coercion Ladder (CL). The lowest step on the scale, 1, means “minimum use of coercion (I came totally on my own will and initiative),” and 10 means “maximum use of coercion” at admission.
In all countries except Finland the interview also included the MacArthur Perceived Coercion Scale, MPCS [25]. The scale consists of five true or false items: “I felt free to do what I wanted about coming to the hospital”; “I chose to come into the hospital”; “It was my idea to come into the hospital”; “I had a lot of control over whether I went into the hospital”; and “I had more influence than anyone else on whether I came into the hospital.” In the present Nordic study, the items were rephrased into questions [26], with yes or no response alternatives. An affirmative answer scored zero and a negative answer scored 1, giving a maximum possible score of 5.
The participants were assessed by the Global Assessment of Functioning Scale, GAF [27] and the Brief Psychiatric Rating Scale, BPRS [28]. The interviewers were psychiatrists, and in Sweden also clinical psychologists, all trained in doing the interviews of the study. They were personally not involved in the treatment of the interviewed patients. The patients’ legal status at admission and diagnoses according to ICD-10 were collected from the case records of the patients. Prior to its instigation, the study was approved by research ethics committees in each country.
Data analysis
As the distribution on the CL had a U-shaped tendency with a small middle group, the scores were dichotomised into low (1–4) and high (5–10). According to previous studies [29, 30], scores 0–2 on the MPCS were classified as “low perceived coercion” and scores 3–5 were classified as “high perceived coercion”. The χ2-test was used to test for differences in proportions. Differences in age, and GAF and BPRS scores were tested with Student’s t-test or one-way analysis of variance (ANOVA). To test for differences in CL and MPCS scores, the Kruskal-Wallis test was used. Logistic regression analyses were performed with the dichotomised CL as dependent variable, and country, or centre within a country, respectively, and patient characteristic variables as independents. P-values < 0.05 were considered significant.
Results
Participants
Of patients asked to participate, between 75% (Sweden) and 89% (Norway) accepted. A total number of 920 patients were included in the study, whereof 426 (46%) were committed. Characteristics of the study participants are presented in Table 1.
Committed patients
The committed patients’ statements about whether they came involuntarily to the hospital varied significantly among countries (Table 2), and we found significant differences in levels of perceived coercion at admission between countries (Table 3).
There were no differences between committed patients scoring high and low on the CL with regard to sex, age, diagnostic group, BPRS scores or if the patient was admitted for the first time or not. However, committed patients are scoring low on the CL had higher GAF scores than patients scoring high; mean (SD) 36.9(11.3) vs. 33.6(10.8) (t = 2.8, df = 391, P = 0.006).
We found no differences in perceived coercion scores between the participating centres within countries, with the exception of Sweden. One of the centres in Sweden, with few cases, differed significantly from the other three centres (Tables 2, 3).
In a logistic regression analysis with the dichotomised CL as dependent variable and country as independent variable, living in Norway was a significant predictor for low perceived coercion. When adding patient characteristic variables into the model as independents, country was still a significant explanatory variable. In analyses for Finland, Norway and Sweden separately, with local centre as independent variable, the models were not significant in Finland and Norway. In Sweden, local centre was a significant explanatory variable for CL (Table 4).
Voluntary patients
There were significant differences between countries in the proportion of voluntary patients stating that they came involuntarily to the hospital (Table 2), but no differences in CL and MPCS scores, either between countries or centres (Table 3). There were no differences among the voluntary patients between patients scoring high and low on the CL, with regard to sex, age, diagnostic group, BPRS scores or if the patient was first time admitted or not. Patients scoring high on the CL had lower GAF than patients scoring low; mean (SD) 35.8(12.0) vs. 39.3(10.7) (t = 2.7, df = 467, P = 0.008).
When doing the same logistic regression analyses as for committed patients, living in Sweden was found to be a significant predictor for low perceived coercion (P = 0.036), when the patient characteristic variables were included in the model (Table 4).
Discussion
Variations in perceived coercion between countries
We found significant differences between the Nordic countries in levels of perceived coercion at admission among committed patients. The lowest level was found in Norway, where less than half of the committed patients scored high on the CL. When using subjective self-report scales, different “set points” might be expected depending on local culture, even if the Nordic countries in a worldwide context may be regarded as culturally quite similar. Variation between countries was not due to differences in patient’s characteristics. Low level of functioning according to GAF was associated with high levels of perceived coercion, but there were no differences between countries in mean GAF scores among committed patients, and country was a significant predictor for CL scores even after controlling for GAF.
The differences found in perceived coercion scores between the Nordic countries can more likely be explained by differences in the mental health legislation of the participating countries. In countries where a wide concept of coercion in the Civil Commitment Act is applied, more patients will be formally committed, even if they are willing to be hospitalised, and these patients will likely report less perceived coercion at admission. Our results partly support this explanation. The two countries applying a wide concept of coercion, Finland and Norway, had the lowest proportions of committed patients reporting that they came involuntarily to the hospital, and the lowest proportions of high-perceived coercion scores. However, only Norway differed markedly from the other countries. The Norwegian mental health act does not permit involuntary detention of voluntary patients, which is likely to be important in this context. Clinicians knowing they cannot retain voluntarily admitted patients and who want to prevent the patients from deteriorating, leaving the hospital too early and not getting necessary treatment, will be inclined to admit more patients on a formally involuntary basis from the beginning, regardless if the patients accept admission or not. Such strategic use of civil commitment combined with a wide concept of coercion will cause differences in reported perceived coercion among committed patients.
If this holds true, it should have been expected that differences were found also among the voluntary patients. In countries with a wide concept of coercion more patients would score lower on perceived coercion compared to patients in countries applying a narrow concept. We were not able to confirm this as there were small differences between countries, but with a tendency of lower perceived coercion in Sweden. So even if we found evidence in support of the “wide coercion concept” hypothesis for the committed patients, the lack of confirmation for voluntary patients indicates that explanations of differences in perceived coercion between countries are more complicated, and need to be further studied.
Variations in perceived coercion within countries
Among three countries with more than one participating centre, there was a significant difference between centres in levels of perceived coercion at admission among committed patients in Sweden, only. At the Swedish centre with the lowest proportion of committed patients reporting that they came involuntarily to the hospital, and also the lowest proportion scoring high on the CL, involuntary psychiatric care has been performed for a long time without locking the wards where the patients are treated [22, 31], a clearly different approach than in the other three centres and in most psychiatric departments in Sweden. This finding indicates that local care traditions may have an impact on coercion as perceived by patients.
Levels of perceived coercion
The results cannot be used to make judgements whether the levels of perceived coercion among committed and voluntary patients are appropriate. If we had chosen other cut–off points, the results might have been different. However, if repeated measures of perceived coercion are applied, scores could be more useful. By emphasizing changes in perceived coercion over time (both for the same patients at different times as for new groups of patients admitted to the same hospital) clinicians can get valuable feedback that might be helpful in order to improve clinical practice.
Some other studies also have provided MPCS scores for committed and voluntary patients separately, and it is interesting to note the similarities in mean MPCS scores found in our study compared with studies from England, the United States, and New Zealand [9, 11, 29, 32]. Except for voluntary patients in the study of Hoge et al. [29], where the mean MPCS score was lower (0.6 vs. 1.7), the scores are almost identical (Table 5). Our results also confirm the bimodal distribution of perceived coercion scores found by others [9, 11, 25].
Formal legal status and perceived coercion
In the present study, we found poor correspondence between the patients’ formal legal status and perceived coercion scores. Neither did the patients own opinion on whether they came voluntarily to the hospital correspond well with their formal legal status at admission. The discrepancy was particularly pronounced for the committed patients. These results confirm previous findings [9, 10, 13, 15, 17, 33, 34] and should remind us to be cautious and not rely on the formal legal status as a valid measure for coercion in scientific studies.
Conclusion
Among committed patients, the levels of perceived coercion varied significantly across the Nordic countries. A wide concept of coercion in the Civil Commitment Act and no legal possibility of detention of voluntary patients were associated with low levels of perceived coercion at admission among committed patients. The results from Sweden also indicate that local care traditions may account for variation between centres within countries. The levels of perceived coercion found in the present study were comparable to studies from other parts of the world. Furthermore, the study confirmed the poor correspondence between perceived coercion and the patients’ formal legal status previously found by others.
References
Bjørngaard JH, Heggestad T (2001) Kan ulik pasientsammensetning forklare forskjeller i tvangsinleggelser? (Can case-mix explain differences in involuntary admissions? In Norwegian, Abstract in English). Tidsskr Nor Laegeforen 121:3369–3374
Engberg M (1991) Involuntary commitment in Greenland, the Faroe Islands and Denmark. Acta Psychiatr Scand 84:353–356
Hansson L, Muus S, Saarento O, Vinding HR, Göstas G, Sandlund M, Zandrén T, Öiesvold T (1999) The Nordic comparative study on sectorized psychiatry: rates of compulsory care and use of compulsory admissions during a 1-year follow-up. Soc Psych Psych Epid 34:99–104
Kjellin L (1997) Compulsory psychiatric care in Sweden 1979–1993 Prevalence of committed patients, discharge rates and area variation. Soc Psych Psych Epid 32:90–96
Kokkonen P (1993) Coercion and legal protection in psychiatric care in Finland. Med Law 12:113–124
Riecher-Rössler A, Rössler W (1993) Compulsory admission of psychiatric patients—an international comparison. Acta Psychiat Scand 87:231–236
Salize HJ, Dressing H (2004) Epidemiology of involuntary placement of mentally ill people across the European Union. Br J Psychiat 184:163–168
Zinkler M, Priebe S (2002) Detention of the mentally ill in Europe—a review. Acta Psychiat Scand 106:3–8
Bindman J, Reid Y, Szmukler G, Tiller J, Thornicroft G, Leese M (2005) Perceived coercion at admission to psychiatric hospital and engagement with follow-up. Soc Psych Psych Epid 40:160–166
Engberg M (1994) Frihedsberøvelse i psykiatrien og aspekter ved den nye psykiatrilovs funktion (Deprivation of liberty and aspects of the functioning of the new mental health act. In Danish. Summary in English) Universitetshospital Aarhus
Hiday VA, Swartz MS, Swanson J, Wagner HR (1997) Patient perceptions of coercion in mental hospital admission. Int J Law Psychiat 20:227–241
Kaltiala-Heino R (1995) Involuntary psychiatric hospitalization. Tampere Acta Universitatis Tamperensis
Kjellin L, Westrin CG (1998) Involuntary admissions and coercive measures in psychiatric care Registered and reported. Int J Law Psychiat 21:31–42
Lidz CW, Hoge SK, Gardner W, Bennett NS, Monahan J, Mulvey EP, Roth LH (1995) Perceived coercion in mental hospital admission. Pressures and process. Arch Gen Psychiat 52:1034–1039
Monahan J, Hoge SK, Lidz C, Roth LH, Bennet N, Gardner W, Mulvey E (1995) Coercion and commitment: understanding involuntary mental hospital admission. Int J Law Psychiat 18:249–263
Rogers A (1993) Coercion and “voluntary” admission: an examination of psychiatric patients views. Beh Sci Law 11:259–267
Tuohimäki C, Kaltiala-Heino R, Korkeila J, Protshenko J, Tuori T, Lehtinen V (2001) Psychiatric inpatients’ views on self-determination. Int J Law Psychiat 24:61–69
Lidz CW, Mulvey EP, Hoge SK, Kirsch BL, Monahan J, Bennett NS, Eisenberg M, Gardner W, Roth LH (1997) The validity of mental patients’ accounts of coercion-related behaviors in the hospital admission process. Law Hum Behav 21:361–376
Høyer G, Kjellin L, Engberg M, Kaltiala-Heino R, Nilstun T, Sigurjónsdóttir M, Syse A (2002) Paternalism and autonomy: a presentation of a Nordic study on the use of coercion in the mental health care system. Int J Law Psychiat 25:93–108
Nilstun T, Syse A (2000) The right to accept and the right to refuse. Acta Psychiat Scand Suppl. 399:31–34
Iversen KI, Høyer G, Sexton H, Grønli OK (2002) Perceived coercion among patients admitted to acute wards in Norway. Nord J Psychiat 56:433–439
Kjellin L, Andersson K, Bartholdsson E, Candefjord IL, Holmström H, Jacobsson L, Sandlund M, Wallsten T, Östman M (2004) Coercion in psychiatric care—patients’ and relatives’ experiences from four Swedish psychiatric services. Nord J Psychiat 58:153–159
Poulsen HD (1999) Perceived coercion among committed, detained, and voluntary patients. Int J Law Psychiat 22:167–175
Poulsen HD, Engberg M (2001) Validation of psychiatric patients’ statements on coercive measures. Acta Psychiat Scand 103:60–65
Gardner W, Hoge SK, Bennett N, Roth LH, Lidz CW, Monahan J, Mulvey EP (1993) Two scales for measuring patients’ perceptions for coercion during mental hospital admission. Behav Sci Law 11:307–321
Seigel K, Wallsten T, Torsteinsdottir G, Lindström E (1997) Perception of coercion: a pilot study using the Swedish version of the Admission Experience Scale. Nord J Psychiat 51:49–54
American Psychiatric Association (1987) Diagnostic and Statistical Manual of Mental Disorders, 3rd edn. revised, DSM-III-R. Washington, APA
Overall JE, Gorham DE (1962) The brief psychiatric rating scale. Psychol Rep 10:799–812
Hoge SK, Lidz CW, Eisenberg M, Gardner W, Monahan J, Mulvey E, Roth L, Bennett N (1997) Perceptions of coercion in the admission of voluntary and involuntary psychiatric patients. Int J Law Psychiat 20:167–181
Rain SD, Williams VF, Robbins PC, Monahan J, Steadman HJ, Vesselinov R (2003) Perceived coercion at hospital admission and adherence to mental health treatment after discharge. Psychiat Serv 54:103–105
Holmström H, Larsson MJ, Toft R, Jentzsch G (1988) Psykiatrisk tvångsvård utan lås: illusion eller verklighet? (Compulsory psychiatric care without locked wards: illusion or reality? In Swedish). Lakartidningen 85:1512–1516
McKenna BG, Simpson AI, Laidlaw TM (1999) Patient perception of coercion on admission to acute psychiatric services. The New Zealand experience. Int J Law Psychiat 22: 143–153
Edelsohn GA, Hiday VA (1990) Civil commitment: a range of patient attitudes. Bull Am Acad Psych Law 18:65–77
Kaltiala-Heino R, Laippala P, Salokangas RK (1997) Impact of coercion on treatment outcome. Int J Law Psychiat 20:311–322
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kjellin, L., Høyer, G., Engberg, M. et al. Differences in perceived coercion at admission to psychiatric hospitals in the Nordic countries. Soc Psychiat Epidemiol 41, 241–247 (2006). https://doi.org/10.1007/s00127-005-0024-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-005-0024-0