Abstract
Aims/hypothesis
Low phosphate and high calcium concentrations have been linked to altered glucose tolerance and reduced insulin sensitivity in non-diabetic individuals. The aim of this study was to examine the relationships of calcium and phosphate levels and the calcium–phosphate product with the development of type 2 diabetes.
Methods
Participants were 863 African-Americans, Hispanics and non-Hispanic whites in the Insulin Resistance Atherosclerosis Study who were free of diabetes at baseline. The mean follow-up period was 5.2 years. The insulin sensitivity index (SI) and acute insulin response (AIR) were directly measured using the frequently sampled IVGTT.
Results
Calcium concentration (OR per 1 SD unit increase, 1.26 [95% CI 1.04, 1.53]) and calcium–phosphate product (OR 1.29 [95% CI 1.04, 1.59]) were associated with incident diabetes after adjustment for demographic variables, family history of diabetes, and 2 h glucose. The relationship between phosphate concentration and progression to diabetes was close to statistical significance (OR 1.21 [95% CI 0.98, 1.49]). Calcium concentration (OR 1.37 [95% CI 1.09, 1.72]) and calcium–phosphate product (OR 1.39 [95% CI 1.09, 1.77]) remained associated with incident diabetes after additional adjustment for BMI, plasma glucose, SI, AIR, C-reactive protein, estimated GFR, diuretic drugs and total calcium intake.
Conclusions/interpretation
Elevated serum calcium and calcium–phosphate product are associated with increased risk of developing type 2 diabetes independently of measured glucose, insulin secretion and insulin resistance. Future studies need to analyse the role of calcium–phosphate homeostasis in the pathophysiology of diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Increased serum calcium concentration predicts all-cause and cardiovascular disease (CVD) mortality [1–4]. Primary hyperparathyroidism, a condition characterised by high calcium levels, has been associated with increased CVD risk [5], prevalent diabetes and impaired glucose tolerance [6, 7]. Parathyroid resection tends to restore normocalcaemia and improves left ventricular hypertrophy and glucose tolerance [8, 9]. In addition, elevated calcium concentration is related to a number of metabolic abnormalities in cross-sectional studies, including impaired glucose tolerance [10], decreased insulin sensitivity and insulin secretion in individuals with fasting glucose <7.0 mmol/l [11], and decreased insulin sensitivity measured by the clamp technique in elderly men with normal glucose tolerance and renal function [12]. Recent results from the Tromsø Study indicate that serum calcium concentration predicts the incidence of diabetes [4]. Although the authors adjusted for age, sex, BMI, smoking, blood pressure and cholesterol, there was no information on glucose concentration or insulin resistance.
Serum calcium and phosphate levels are under tight hormonal control [13]. The calcium–phosphate product is used as a risk measure for ectopic calcification in chronic kidney disease [14]. Both increased phosphate concentration and calcium–phosphate product predict CVD events and mortality in individuals with end-stage renal disease [15]. Some reports also describe similar associations in persons with normal or mildly decreased renal function: elevated calcium–phosphate product with the severity of aortic stenosis in patients with normal renal function [16]; increased phosphate concentration with CVD events in individuals with normal renal function [17, 18] and mortality in men with hypertension and type 2 diabetes [2]. In contrast, low phosphate concentration is associated with altered glucose tolerance and reduced insulin sensitivity in non-diabetic individuals [19] and in patients with hyperparathyroidism [20]. Phosphate supplementation improves glucose tolerance in hypophosphataemic patients with impaired glucose tolerance [21]. However, whether phosphate concentration and calcium–phosphate product predict the incidence of diabetes has not been tested.
We hypothesised that the development of diabetes may be preceded by elevated calcium and decreased phosphate levels. Therefore, we assessed the risk of developing diabetes associated with serum calcium and phosphate levels and calcium–phosphate product in non-diabetic participants in the Insulin Resistance Atherosclerosis Study (IRAS). We also examined whether these relationships were explained by risk factors for diabetes including BMI, glucose tolerance, insulin sensitivity and insulin secretion. In the IRAS, insulin sensitivity and first-phase insulin secretion were directly measured by the frequently sampled IVGTT.
Methods
Study sample
The IRAS is a multicentre epidemiological study of the relationships between insulin resistance, CVD and its known risk factors in different ethnic groups and varying states of glucose tolerance. The design and methods of this study have been described in detail in previous publications [22]. Briefly, the study was conducted at four clinical centres. At centres in Oakland and Los Angeles, California, non-Hispanic whites and African-Americans were recruited from Kaiser Permanente, a non-profit health maintenance organisation. Centres in San Antonio, Texas and San Luis Valley, Colorado recruited Hispanics from two ongoing population-based studies (the San Antonio Heart Study and the San Luis Valley Diabetes Study). A total of 1,625 individuals participated in the baseline IRAS examination (56% women; age range 40–69 years), which occurred between October 1992 and April 1994. After an average of 5.2 years (range 4.5–6.6 years), follow-up examinations were conducted using the baseline protocol (the response rate was 81%). The IRAS protocol was approved by local institutional review committees, and all participants provided written informed consent.
Participants were eligible for analysis if they were non-diabetic at the baseline examination (n = 1,065). We excluded 22 participants who died during the follow-up period. We also excluded 153 participants for failure to return to the follow-up visit, and 27 for lack of information on calcium levels. Therefore, the present report includes information on 863 participants (348 non-Hispanic whites, 217 African-Americans and 298 Hispanics). These participants were similar to those who were excluded in terms of demographics and baseline characteristics, including adiposity, insulin sensitivity index (SI), acute insulin response (AIR), estimated GFR (eGFR) and levels of plasma glucose and serum calcium and phosphate (p > 0.22 for comparisons).
Clinical measurements and procedures
The IRAS protocol required two visits, 1 week apart, of approximately 4 h each. Protocols were identical at the baseline and 5-year follow-up examinations. Individuals were asked before each visit to fast for 12 h, to abstain from heavy exercise and alcohol for 24 h, and to refrain from smoking the morning of the examination. Data on age, sex, race/ethnicity, diet, family history of diabetes, and medication were gathered by trained personnel. Duplicate measures of anthropometry were made following a standardised protocol, and averages were used in the analysis.
During the first baseline and follow-up visits, a 75 g OGTT was administered to assess glucose tolerance status. During the second baseline visit, insulin sensitivity and insulin secretion were determined using the frequently sampled IVGTT [22]. Some modifications were made to the original frequently sampled IVGTT. An injection of regular insulin rather than tolbutamide was used to ensure adequate plasma insulin levels for the accurate computation of insulin sensitivity across a broad range of glucose tolerance. Glucose in the form of 50% solution (0.3 g/kg) and regular human insulin (0.03 U/kg) were injected through an intravenous line at 0 and 20 min, respectively. Blood was collected at −5, 2, 4, 8, 19, 22, 30, 40, 50, 70, 100 and 180 min for measurement of plasma glucose and insulin. Insulin sensitivity expressed as SI was computed using mathematical modelling methods (MINMOD version 3.0 [1994]; Los Angeles, CA, USA; courtesy of Richard Bergman, Department of Physiology and Biophysics, University of Southern California Medical School, Los Angeles, CA, USA). AIR was calculated as the mean of 2 and 4 min insulin concentrations after glucose administration.
Plasma glucose concentration was determined by the glucose oxidase method on an automated autoanalyser (Yellow Springs Equipment, Yellow Springs, OH, USA). Plasma insulin concentration was measured by the dextran–charcoal RIA (CV 19%) [23]. This assay had a high cross-reactivity with proinsulin. C-reactive protein concentration was measured by an in-house ultrasensitive competitive immunoassay (antibodies and antigens from Calbiochem, La Jolla, CA, USA) (CV 8.9%) [24]. Serum calcium concentration (normal range 2.05–2.58 mmol/l) was determined by the cresolphthalein complexone method (CV 3%) [25], phosphate concentration (inorganic phosphorus contained in the inorganic phosphates; normal range 0.78–1.49 mmol/l) by the phosphomolybdate reduction method (CV 4.5%) [26], creatinine concentration by a modified kinetic Jaffe reaction (CV 1.9%), and albumin concentration by the bromocresol purple dye-binding method (CV 4%) at the central IRAS laboratory with a Paramax PLA instrument (Baxter, Deerfield, IL, USA). Quality-control procedures included blind duplicate blood measurements (10% sample) [22].
Diabetes was defined as fasting glucose ≥7.0 mmol/l and/or 2 h glucose ≥11.1 mmol/l, and impaired glucose tolerance as 2 h glucose ≥7.8–11.0 mmol/l. Individuals who reported current treatment with glucose-lowering medications were considered to have diabetes. Calcium concentration was corrected for the level of albumin: albumin-corrected calcium (mmol/l) = calcium (mmol/l) + 0.2 × (40 − albumin [g/l]) [27]. Calcium–phosphate product (mmol2/l2) was calculated as albumin-corrected calcium × phosphate concentrations. We used the Modification of Diet in Renal Disease equation to estimate eGFR [28]. None of the participants had an eGFR <30 ml/min per 1.73 m2. We gathered information on dietary calcium intake with a validated food frequency questionnaire [29]. Total dietary calcium indicates dietary calcium plus calcium supplements.
Statistical analysis
Analysis was carried out using the SAS (version 9.2; SAS Institute, Cary, NC, USA) and R project statistical software packages (version 2.9.2; The R Foundation for Statistical Computing, Vienna, Austria). We assessed baseline differences in anthropometric and metabolic variables by incident diabetic status using one-way analysis of covariance (for continuous variables) and logistic regression analysis (for dichotomous variables). Pearson’s correlation coefficients were used to examine the strength of the relationship of calcium and phosphate concentrations and calcium–phosphate product to relevant metabolic variables and total calcium intake. To take into account the effect of potential confounders, we used multiple logistic regression analysis to determine the risk of developing diabetes associated with calcium and phosphate concentrations and calcium–phosphate product. In separate models, appropriate interaction terms were introduced to assess the effect of sex, race/ethnicity, family history of diabetes, and glucose tolerance status on the relationship between calcium concentration (phosphate concentration or calcium–phosphate product) and incident diabetes. A separate logistic regression model was fitted to model incident diabetes with a restricted cubic polynomial spline for serum calcium concentration to estimate the varying effects of calcium concentration over its full range [30]. We also generated additional models with phosphate concentration or calcium–phosphate product as the independent variable. We used loge-transformed values of AIR and C-reactive protein in all analyses to minimise the influence of extreme observations. We also used the loge transformation of (SI + 1) given that some participants had SI = 0. We considered a p value <0.05 to be significant.
Results
Mean (range) calcium and phosphate concentrations were 2.25 (1.52–3.02) and 1.02 (0.13–1.55) mmol/l, respectively. Progression to diabetes was associated with the following baseline characteristics: older age, decreased SI and AIR, and increased BMI and levels of plasma glucose, C-reactive protein, calcium and calcium–phosphate product (Table 1). Individuals who developed diabetes did not differ from those who remained non-diabetic with regard to baseline total calcium intake, albumin and phosphate levels, and eGFR.
There was a moderate relationship between serum calcium and phosphate concentrations (r = 0.33). Calcium and phosphate levels and calcium–phosphate product were negatively related to eGFR (Table 2). However, few correlation coefficients relating calcium and phosphate levels and calcium–phosphate product to total calcium intake, plasma glucose levels, SI and AIR were statistically significant: albumin-corrected calcium concentration with SI (very weak and negative); and albumin-corrected calcium concentration and calcium–phosphate product with C-reactive protein (very weak and positive).
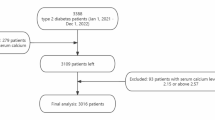
Figure 1 presents the relationship between 5-year incidence of diabetes and calcium concentration (phosphate concentration, calcium–phosphate product or calcium intake) modelled by a smooth function. The relationship was not linear (Wald test, p = 0.040) but statistically significant for calcium concentration (Wald χ 2, p = 0.020), linear and significant for albumin-adjusted calcium concentration (p = 0.268 and 0.046, respectively) and calcium–phosphate product (p = 0.409 and 0.016, respectively), close to significance for phosphate concentration (p = 0.077), and not significant for total calcium intake (p = 0.769).
Probability of developing type 2 diabetes during the 5 year follow-up period. The relation of (a) calcium (p = 0.020) and (b) albumin-adjusted calcium (p = 0.046) concentrations to 5 year incidence of diabetes was significant, whereas the relation of (c) phosphate concentration was marginally significant (p = 0.077). A significant relationship was also demonstrated for (d) calcium–phosphate product (p = 0.016), but not for (e) total calcium intake (0.769). The relationship between calcium concentration and incident diabetes was not linear (Wald test for linearity, p = 0.040), but all the other relationships did not fail the test for linearity (p > 0.26). The dotted lines represent 95% CIs
Individuals with calcium concentration ≥2.38 mmol/l (9.5 mg/dl) were at increased risk of developing diabetes (Table 3). After adjustment for age, sex, race/ethnicity and clinic, the OR was 79% higher in individuals with calcium concentration ≥2.38 mmol/l than in those with calcium concentration <2.38 mmol/l (OR 1.79 [95% CI 1.13, 2.85]). The OR remained statistically significant despite adjustment for BMI, family history of diabetes, fasting and 2 h glucose concentrations, SI, AIR, eGFR and diuretic drugs (OR 2.05 [95% CI 1.16, 3.60]). Similarly, individuals with phosphate concentration ≥1.20 mmol/l (3.7 mg/dl) were at increased risk of developing diabetes (Table 4). The demographically adjusted OR of developing diabetes was 72% higher in individuals with phosphate concentration ≥1.20 mmol/l than in those with phosphate concentration <1.20 mmol/l (OR 1.72 [95% CI 1.03, 2.87]). The OR also remained unchanged in the full model (OR 1.87 [95% CI 0.97, 3.60]).
We further examined the risk of developing diabetes using serum calcium and phosphate levels and calcium–phosphate product as continuous variables (Table 5). Serum calcium and albumin-adjusted calcium levels and calcium–phosphate product were associated with incident diabetes independently of the effect of demographics, clinic, family history of diabetes, plasma glucose levels, BMI, SI, AIR, eGFR, diuretic drugs, C-reactive protein and total calcium intake. Serum phosphate concentration was also associated with incident diabetes in the full model.
In separate models, we examined the effect of sex, race/ethnicity, family history of diabetes and glucose tolerance on the relationship between calcium concentration (phosphate concentration or calcium–phosphate product) and incident diabetes (electronic supplementary material [ESM] Fig. 1). None of these interaction terms was statistically significant (all p > 0.37), indicating consistent relationships across categories of sex, race/ethnicity, family history of diabetes and glucose tolerance.
Discussion
This study has several novel findings. First, serum calcium and phosphate concentrations are not associated with insulin sensitivity and insulin secretion in non-diabetic individuals. Second, calcium concentration has a non-linear relationship with incident diabetes. Individuals with calcium levels ≥2.38 mmol/l (9.5 mg/dl) are at increased risk of developing the disease. Third, this relationship is independent of the effect of measured glucose, insulin secretion and insulin resistance. Finally, the risk of diabetes associated with calcium–phosphate product is comparable with the risk associated with calcium concentration.
Causal inferences cannot be drawn from our results. The association between calcium concentration and incident diabetes has already been reported by a much larger study, the Tromsø Study [4]. Calcium has an important role in a wide range of biological functions including insulin secretion [31]. Insulin secretion is a calcium-dependent process requiring the influx of calcium to the beta cell [32, 33]. Calcium is involved in the regulation of insulin secretion under physiological conditions: (1) extracellular calcium is needed for glucose to increase insulin secretion; (2) glucose must be metabolised by beta cells in order to induce an increase in intracellular calcium; and (3) this increase in intracellular calcium initiates exocytosis of insulin granules [31]. Vitamin D and calcium regulate transcription of calcium transporter genes [33]. In addition, glucose intolerance and insulin resistance are accompanied by an increase in intracellular calcium [34]. Therefore, it is possible that persistent alterations of calcium concentration could affect the insulin secretory response.
In cross-sectional studies, calcium concentration correlated with fasting glucose concentration in a Swedish community [35], and with fasting glucose concentration and homeostasis model assessment of insulin resistance and secretion in non-diabetic individuals from Newfoundland, Canada [11]. Elevated calcium concentration was associated with decreased insulin sensitivity measured by the euglycaemic clamp in elderly men with normal glucose tolerance and normal renal function [12]. Increased calcium concentration was associated with the metabolic syndrome in the general population [36] and increased fasting insulin and late insulin secretory response in middle-aged men [37]. However, there are somewhat mixed results in the literature. In the study by Wareham et al [10], impaired glucose tolerance was related to elevated calcium concentration, even after the effect of age, obesity or vitamin D concentration had been accounted for. However, calcium concentration did not have a significant relationship with surrogate measures of either insulin resistance (fasting insulin concentration) or insulin secretion (30 min insulin increment) [10]. There are also inconsistent reports with regard to the relationship between calcium concentration and the prevalence of type 2 diabetes [38, 39].
In the IRAS, serum calcium concentration is not related to insulin sensitivity and early insulin response (only albumin-corrected calcium concentration has a very weak relationship with insulin sensitivity in cross-sectional analyses [r = −0.08, p < 0.05]). Insulin sensitivity, insulin secretion or plasma glucose levels do not explain the relationship between calcium concentration and progression to diabetes. These results are novel in view of those of the Tromsø Study, in which the described relationship between calcium concentration and incident diabetes is independent of common CVD risk factors including adiposity [4]. Future studies may need to examine mechanisms other than insulin sensitivity and insulin secretion. For example, intracellular calcium has an important role in beta cell apoptosis [40, 41]. Increases in intracellular calcium occur with the development of endoplasmic reticulum stress and dysfunction of both mitochondria and gene transcription, all of which have been implicated in apoptosis [42].
Phosphate concentration has been inversely related to fasting insulin, fasting glucose and late insulin response in the general population [37]. In non-diabetic individuals, low serum phosphate levels have been shown to be associated with high 2 h glucose levels and reduced insulin sensitivity at baseline and high 2 h glucose levels after a lifestyle intervention [19]. Alterations in glucose metabolism and insulin sensitivity have also been described in individuals with chronic hypophosphataemia [20]. However, our results indicate that phosphate concentration has no relationship with measures of insulin sensitivity, insulin secretion and plasma glucose in apparently healthy individuals. The relationship between phosphate concentration and incident diabetes is near significance in demographically adjusted analysis. After adjustment for glucose tolerance and measures of insulin sensitivity and secretion, high rather than low phosphate concentration is associated with future development of diabetes.
Elevated serum phosphate concentration and calcium–phosphate product have been described in an experimental model of insulin resistance [43]. As previously described in middle-aged men participating in a health examination survey [44], the relationship between calcium and phosphate levels is direct and moderate. In IRAS participants, all of whom had normal or mildly decreased renal function [45], the calcium–phosphate product is not associated with plasma glucose levels and measures of insulin sensitivity and insulin secretion. The relationship of calcium–phosphate product (i.e. OR) to incidence of diabetes is not very different from that of calcium concentration. There is also a relation between phosphate concentration and CVD [17, 18]. Thus, we cannot dismiss a potential association between phosphate concentration and development of diabetes. Follow-up ORs for phosphate concentration are similar to those for calcium concentration (Table 5), even though the former fails to reach statistical significance in some analyses. This could be due to a type 2 error.
Our study has several strengths. Calcium concentration (uncorrected and corrected values) is associated with incident diabetes with no significant interaction effects of sex, race/ethnicity and glucose tolerance status. The IRAS has a well characterised sample population and validated measures of both insulin sensitivity and insulin secretion. Our study also has limitations. First, it lacks information on dietary vitamin D and serum levels of vitamin D and parathyroid hormone. Low vitamin D concentration has been associated with increased risk of diabetes [46], but also with low ionised calcium [47]. The absence of data on vitamin D and parathyroid hormone limits our ability to assess the relation of calcium and phosphate levels to both incident diabetes and eGFR. However, the Tromsø Study has already described a relationship between calcium concentration and incident diabetes [4]. Small elevations of both calcium and phosphate levels have also been linked to mild worsening of renal function [48–50]. Second, our study lacks data on ionised calcium, which is the physiologically active form [26]. Total calcium concentration in serum continues to be measured in the clinical setting, and corrected calcium for the level of albumin is commonly used. However, this presupposes that the binding of calcium to albumin is constant and ignores other relevant ligands [26]. Thus, future studies need to examine whether ionised calcium is associated with incident diabetes. Finally, sample size and the number of individuals developing diabetes are moderate. Statistical power of correlation coefficients is high, but power of logistic regression models is moderate for weak predictors of incident diabetes, such as calcium and phosphate levels. Therefore our results on risk prediction need to be interpreted with caution. Nevertheless, we have found that the relationship between calcium concentration and incident diabetes is comparable to that of the Tromsø Study, a study with higher statistical power (25,055 individuals and 705 new cases of diabetes) [4]. Our study is also novel because it suggests that the relationship is independent of important determinants of diabetes such as glucose tolerance, insulin resistance and insulin secretion.
In conclusion, serum calcium concentration and calcium–phosphate product are associated with the development of type 2 diabetes. These associations are independent of the effect of adiposity, glucose tolerance, insulin sensitivity, insulin secretion and subclinical inflammation. In the IRAS population, high rather than low phosphate concentration is associated with progression to diabetes. Future studies need to examine whether calcium–phosphate homeostasis plays a role in the development of diabetes independent of measured glucose, insulin secretion and insulin resistance.
Abbreviations
- AIR:
-
Acute insulin response
- CVD:
-
Cardiovascular disease
- eGFR:
-
Estimated GFR
- IRAS:
-
Insulin Resistance Atherosclerosis Study
- SI :
-
Insulin sensitivity index
References
Leiffsson BG, Ahren B (1996) Serum calcium and survival in a large health screening program. J Clin Endocrinol Metab 81:2149–2153
Håglin L, Törnkvist B, Bäckman L (2007) Prediction of all-cause mortality in a patient population with hypertension and type 2 DM by using traditional risk factors and serum-phosphate, -calcium and -magnesium. Acta Diabetol 44:138–143
Walsh JP, Divitini ML, Knuiman MW (2013) Plasma calcium as a predictor of cardiovascular disease in a community-based cohort. Clin Endocrinol (Oxf) 78:852–857
Jorde R, Schirmer H, Njølstad I et al (2013) Serum calcium and the calcium-sensing receptor polymorphism rs17251221 in relation to coronary heart disease, type 2 diabetes, cancer and mortality: the Tromsø Study. Eur J Epidemiol 28:569–578
Andersson P, Rydberg E, Willenheimer R (2004) Primary hyperparathyroidism and heart disease: a review. Eur Heart J 25:1776–1787
Procopio M, Magro G, Cesario F et al (2002) The oral glucose tolerance test reveals a high frequency of both impaired glucose tolerance and undiagnosed type 2 diabetes mellitus in primary hyperparathyroidism. Diabet Med 19:958–961
Taylor WH, Khaleeli AA (2001) Coincident diabetes mellitus and primary hyperparathyroidism. Diabetes Metab Res Rev 17:175–180
Stefenelli T, Mayr H, Bergler-Klein J, Globits S, Woloszczuk W, Niederle B (1993) Primary hyperparathyroidism: incidence of cardiac abnormalities and partial reversibility after successful parathyroidectomy. Am J Med 95:197–202
Richards ML, Thompson NW (1999) Diabetes mellitus with hyperparathyroidism: another indication for parathyroidectomy? Surgery 126:1160–1166
Wareham NJ, Byrne CD, Carr C, Day NE, Boucher BJ, Hales CN (1997) Glucose intolerance is associated with altered calcium homeostasis: a possible link between increased serum calcium concentration and cardiovascular disease mortality. Metabolism 46:1171–1177
Sun G, Vasdev S, Martin GR et al (2005) Altered calcium homeostasis is correlated with abnormalities of fasting serum glucose, insulin resistance, and beta-cell function in the Newfoundland population. Diabetes 54:3336–3339
Hagström E, Hellman P, Lundgren E, Lind L, Arnlöv J (2007) Serum calcium is independently associated with insulin sensitivity measured with euglycaemic-hyperinsulinaemic clamp in a community-based cohort. Diabetologia 50:317–324
DeLuca HF (1975) The kidney as an endocrine organ involved in the function of vitamin D. Am J Med 58:39–47
National Kidney Foundation (2003) K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis 42:S77–S84
Block GA, Port FK (2000) Re‐evaluation of risks associated with hyperphosphatemia and hyperparathyroidism in dialysis patients: recommendation for a change in management. Am J Kidney Dis 35:1226–1237
Mills WR, Einstadter D, Finkelhor RS (2004) Relation of calcium-phosphorus product to the severity of aortic stenosis in patients with normal renal function. Am J Cardiol 94:1196–1198
Dhingra R, Sullivan LM, Fox CS et al (2007) Relations of serum phosphorus and calcium levels to the incidence of cardiovascular disease in the community. Arch Intern Med 167:879–885
Tonelli M, Sacks F, Pfeffer M et al (2005) Relation between serum phosphate level and cardiovascular event rate in people with coronary disease. Circulation 112:2627–2633
Haap M, Heller E, Thamer C, Tschritter O, Stefan N, Fritsche A (2006) Association of serum phosphate levels with glucose tolerance, insulin sensitivity and insulin secretion in non-diabetic subjects. Eur J Clin Nutr 60:734–739
DeFronzo RA, Lang R (1980) Hypophosphatemia and glucose intolerance: evidence for tissue insensitivity to insulin. N Engl J Med 303:1259–1263
Wittmann I, Nagy J (1997) Effectiveness of phosphate supplementation in glucose intolerant, hypophosphatemic patients. Miner Electrolyte Metab 23:62–63
Wagenknecht LE, Mayer EJ, Rewers M et al (1995) The Insulin Resistance Atherosclerosis Study: design, objectives and recruitment results. Ann Epidemiol 5:464–472
Herbert V, Lau K, Gottlieb C, Bleicher S (1965) Coated charcoal immunoassay of insulin. J Clin Endocrinol Metab 25:1375–1384
Macy EM, Hayes TE, Tracy RP (1997) Variability in the measurement of C-reactive protein in healthy subjects: implications for reference intervals and epidemiological applications. Clin Chem 43:52–58
Lott JA, Manning NR, Kyler MK (1989) Proficiency testing in a medical-needs context. Clin Chem 35:347–354
Guynn RW, Veloso D, Veech RL (1972) Enzymic determination of inorganic phosphate in the presence of creatine phosphate. Anal Biochem 45:277–285
Payne RB, Little AJ, Williams RB, Milner JR (1973) Interpretation of serum calcium in patients with abnormal serum proteins. BMJ 4:643–646
Levey AS, Coresh J, Balk E et al (2003) National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med 139:137–147
Ma B, Lawson AB, Liese AD, Bell RA, Mayer-Davis EJ (2006) Dairy, magnesium, and calcium intake in relation to insulin sensitivity: approaches to modeling a dose-dependent association. Am J Epidemiol 164:449–458
Harrell FE (2001) Regression modeling strategies. Springer, New York
Henquin JC (2000) Triggering and amplifying pathways of regulation of insulin secretion by glucose. Diabetes 49:1751–1760
Pittas AG, Lau J, Hu FB, Dawson-Hughes B (2007) The role of vitamin D and calcium in type 2 diabetes. A systematic review and meta-analysis. J Clin Endocrinol Metab 92:2017–2029
Ko SH, Lee GS, Vo TT (2009) Dietary calcium and 1,25-dihydroxyvitamin D3 regulate transcription of calcium transporter genes in calbindin-D9k knockout mice. J Reprod Dev 55:137–142
Resnick LM (1991) Calcium metabolism in hypertension and allied metabolic disorders. Diabetes Care 14:505–520
Lind L, Jakobsson S, Lithell H, Wengle B, Ljunghall S (1988) Relation of serum calcium concentration to metabolic risk factors for cardiovascular disease. BMJ 297:960–963
Saltevo J, Niskanen L, Kautiainen H et al (2011) Serum calcium level is associated with metabolic syndrome in the general population: FIN-D2D study. Eur J Endocrinol 165:429–434
Lind L, Skarfors E, Berglund L, Lithell H, Ljunghall S (1997) Serum calcium: a new, independent, prospective risk factor for myocardial infarction in middle-aged men followed for 18 years. J Clin Epidemiol 50:967–973
Levy J, Stern Z, Gutman A et al (1986) Plasma calcium and phosphate levels in an adult non-insulin-dependent diabetic population. Calcif Tissue Int 39:316–318
Heath H, Lambert PW, Service FJ et al (1979) Calcium homeostasis in diabetes mellitus. J Clin Endocrinol Metab 49:462–466
Chandra J, Zhivotovsky B, Zaitsev S, Juntti-Berggren L, Berggren PO, Orrenius S (2001) Role of apoptosis in pancreatic beta-cell death in diabetes. Diabetes 50(Suppl 1):S44–S447
Wang L, Bhattacharjee A, Zuo Z et al (1999) A low voltage-activated Ca2+ current mediates cytokine-induced pancreatic beta-cell death. Endocrinology 140:1200–1204
Ramadan JW, Steiner SR, O'Neill CM, Nunemaker CS (2011) The central role of calcium in the effects of cytokines on beta-cell function: implications for type 1 and type 2 diabetes. Cell Calcium 50:481–490
Zhou YB, Zhang J, Cai Y et al (2012) Insulin resistance induces medial artery calcification in fructose-fed rats. Exp Biol Med (Maywood) 237:50–57
Ljunghall S, Hedstrand H, Hellsing K, Wibell L (1977) Calcium, phosphate and albumin in serum. A population study with special reference to renal stone formers and the prevalence of hyperparathyroidism in middle-aged men. Acta Med Scand 201:23–30
Lorenzo C, Nath SD, Hanley AJ, Abboud HE, Haffner SM (2008) The relation of low glomerular filtration rate to metabolic disorders in individuals without diabetes and with normoalbuminuria. Clin J Am Soc Nephrol 3:783–789
Scragg R (2008) Vitamin D and type 2 diabetes. Are we ready for a prevention trial? Diabetes 57:2565–2566
Steingrimsdottir L, Gunnarsson O, Indridason OS, Franzson L, Sigurdsson G (2005) Relationship between serum parathyroid hormone levels, vitamin D sufficiency, and calcium intake. JAMA 294:2336–2341
Craver L, Marco MP, Martínez I et al (2007) Mineral metabolism parameters throughout chronic kidney disease stages 1–5: achievement of K/DOQI target ranges. Nephrol Dial Transplant 22:1171–1176
Hsu CY, Chertow GM (2002) Elevations of serum phosphorus and potassium in mild to moderate chronic renal insufficiency. Nephrol Dial Transplant 17:1419–1425
Levin A, Bakris GL, Molitch M et al (2006) Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: results of the study to evaluate early kidney disease. Kidney Int 71:31–38
Funding
This study was supported by National Heart, Lung, and Blood Institute grants HL-47887, HL-47889, HL-47890, HL-47892 and HL-47902, and the General Clinical Research Centers Program (NCRR GCRC, M01 RR431 and M01 RR01346).
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
CL contributed to the conception and design of the study, analysis and interpretation of data and drafting the article. AJH and MJR contributed to the analysis and interpretation of data and revised the manuscript critically for important intellectual content. SMH contributed to the acquisition of data, conception and design of the study, analysis and interpretation of data and drafting the article. All authors gave final approval of the version to be published. CL is responsible for the integrity of the work as a whole.
Author information
Authors and Affiliations
Corresponding author
Additional information
Steven M. Haffner is a retired Professor of Medicine, University of Texas Health Science Center.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Fig. 1
(PDF 266 kb)
Rights and permissions
About this article
Cite this article
Lorenzo, C., Hanley, A.J., Rewers, M.J. et al. Calcium and phosphate concentrations and future development of type 2 diabetes: the Insulin Resistance Atherosclerosis Study. Diabetologia 57, 1366–1374 (2014). https://doi.org/10.1007/s00125-014-3241-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-014-3241-9