Abstract
Purpose
To review emerging techniques in cardiac magnetic resonance imaging (CMR) and their clinical applications with a special emphasis on new technologies, recent trials, and updated guidelines.
Technological innovations
The utility of CMR has expanded with the development of new MR sequences, postprocessing techniques, and artificial intelligence-based technologies, which have substantially increased the spectrum, quality, and reliability of information that can be obtained by CMR.
Established and emerging indications
The CMR modality has become an irreplaceable tool for diagnosis, treatment guidance and follow-up of patients with ischemic heart disease, myocarditis, and cardiomyopathies. Its role has been further strengthened by recent trials and guidelines. Quantitative mapping techniques are increasingly used for tissue characterization and detection of diffuse myocardial changes including myocardial storage diseases.
Practical recommendations
With state-of-the-art CMR sequences, postprocessing techniques and understanding of their interpretation, CMR makes invaluable contributions to provide state-of-the-art diagnostics and care for cardiac patients in a multidisciplinary team.
Zusammenfassung
Ziel
Überblick über neuere Techniken der kardialen Magnetresonanztomographie (MRT) und ihre klinischen Anwendungen mit besonderem Schwerpunkt auf neuen Technologien, jüngsten Studien und aktualisierten Richtlinien.
Technologische Innovationen
Der Nutzen der kardialen MRT wurde durch die Entwicklung neuer MR-Sequenzen, Nachbearbeitungstechniken und Technologien auf der Basis künstlicher Intelligenz erweitert. Mit dem technischen Fortschritt haben sich das Spektrum, die Qualität und die Zuverlässigkeit von Informationen, die die kardiale MRT liefert, erheblich verbessert.
Etablierte und aufkommende Indikationen
Die kardiale MRT hat sich zu einem unersetzlichen Instrument für Diagnostik, Behandlungsentscheidungen und Nachsorge bei Patienten mit ischämischer Herzerkrankung, Myokarditis und Kardiomyopathien entwickelt. Ihre Rolle wurde durch jüngste Studien und Leitlinien weiter gestärkt. Quantitative Kartierungstechniken werden zunehmend zur Gewebecharakterisierung und zum Nachweis diffuser Myokardveränderungen einschließlich myokardialer Speicherkrankheiten eingesetzt.
Praktische Empfehlungen
Mit modernsten MR-Sequenzen, Nachbearbeitungstechniken und Verständnis ihrer Interpretation leistet die kardiale MRT einen unschätzbaren Beitrag zur zeitgemäßen Diagnostik und Versorgung von Herzpatienten in einem multidisziplinären Team.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
In recent years, cardiac magnetic resonance imaging (CMR) has become ever more important in the diagnosis and risk stratification of patients with cardiac disease. The CMR modality is the established gold standard for the noninvasive volumetric and functional assessment of the ventricles, the assessment of myocardial viability, and tissue characterization. Established diagnostic approaches have been complemented by new techniques such as T1, T2 mapping and strain imaging. Recent large clinical trials have helped to further refine the role of CMR in the current guidelines for a variety of cardiac diseases. With innovative strategies and artificial intelligence in CMR, novel pathways have emerged for data evaluation, reducing gaps and weaknesses found in conventional approaches.
Emerging techniques in CMR
T1 mapping
T1 mapping is a quantitative technique by which the T1 relaxation times of each pixel of myocardium can be measured and a map of T1 values created. These maps play an important role for patients with diffuse or subtle changes in the myocardium that cannot be detected by visual inspection of gray-scale images [7, 35]. Even isotropic sequences are currently being developed, which will enable three-dimensional (3D) mapping [27].
Pre-contrast T1 mapping can detect early amyloid involvement, before overt changes in late gadolinium enhancement (LGE) sequences, and an example is shown in Fig. 1 [1]. Diffuse cardiac fibrosis and elevated T1 values are also seen in patients with low-flow low-gradient aortic stenosis and dilated cardiomyopathy [23, 30]. Conversely, accumulation of glycosphingolipids in Fabry’s disease causes a characteristic decrease in T1 values [28].
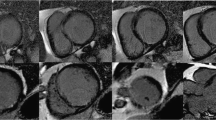
Cardiac magnetic resonance imaging (MRI) in a 54-year-old man admitted after an event of ventricular fibrillation and successful cardiopulmonary resuscitation. Coronary artery disease was excluded by cardiac catheterization. Echocardiography showed reduced ejection fraction. Cardiac MRI was performed 5 days after the event. T2 mapping (a), late gadolinium enhancement in short-axis (b) and vertical long-axis view (d), and fat-suppressed T2-weighted short-axis images (c) are shown. Findings include subepicardial late gadolinium enhancement in the anterior (dotted arrow in b) and inferior wall (dotted arrow in d) with corresponding edema, which is more readily appreciated on T2 mapping (white arrows in a) than on conventional fat-suppressed T2-weighted imaging (dashed arrows in c). These findings are consistent with acute myocarditis
If T1 mapping is performed before and after contrast agent administration, it makes it possible to calculate and map the distribution of the myocardial extracellular volume fraction [35]. Extracellular volume (ECV) and cardiac fibrosis measurements have been shown to predict clinical outcomes in a variety of cardiac diseases; however, more studies with larger sample sizes may be required to definitely establish ECV as an independent predictive factor for adverse prognosis [15, 37]. The lack of standardization and reference values in regional populations may restrict the use of T1 mapping, and the establishment of in-house standard values is necessary. Nevertheless, T1 mapping is being adopted widely in routine CMR examinations.
T2 mapping
T2 mapping, similar to T1 maps, creates parametric images or maps representing T2 relaxation times of the myocardium, thereby providing a potentially more objective representation of inflammation and edema than gray-scale T2 images [20]. There is increasing evidence that T2 mapping can detect acute inflammation extending beyond areas identified on routine T2 sequences [8]. The current clinical indication for T2 mapping includes acute myocarditis, sarcoidosis, inflammation associated with myocardial infarction, toxicity due to chemotherapeutic drugs, and cardiac transplant rejection [5, 12].
T2* mapping
Cardiac failure is a common cause of death in patients with thalassemia and iron overload. Conventional imaging techniques have a limited role in early detection, as cardiac involvement is apparent only after the onset of ventricular dysfunction, which is late in the course of the disease. T2* values allow for the detection and quantification of iron deposition in early stages as well as for monitoring treatment response and efficacy of the chelation. Cardiac iron deposition in these patients is a predictor for adverse prognosis and early detection permits early institution of chelation along with other treatment strategies [38]. More recently, T2* mapping has been used to detect intramyocardial hemorrhage as an adverse prognostic marker in acute infarction [4].
Strain imaging
Strain imaging by CMR is a promising technique for cardiac evaluation beyond routine functional analysis. It provides information on myocardial deformation, helping in the detection of preclinical left ventricular dysfunction before overt regional wall motion abnormality and reduction in ejection fraction. Strain analysis can be performed either by acquiring specific targeted sequences (CMR tagging) or by applying post-processing techniques on standard cine SSFP sequences such as feature tracking. CMR tagging is validated and currently accepted as a standard for strain imaging [32]. Left ventricular strain after vasodilator stress has been shown to be an independent predictor for adverse cardiac events in a recently concluded prospective study [29]. Similar studies have shown the value of strain analysis for other cardiac chambers in specific clinical situations such as prediction of adverse cardiac events with right atrial strain in patients with pulmonary arterial hypertension [19]. There are ongoing studies on the reference values and the comparison between different techniques of strain analysis.
Update on diagnostic criteria for myocarditis
Patients with myocarditis present with symptoms ranging from transient chest pain to life-threatening ventricular arrhythmias. Often, CMR is used as part of the diagnosis with initial imaging criteria (known as the “Lake Louise Criteria”) described in 2009. According to these original criteria, the diagnosis is made if at least two of three criteria are present: namely, myocardial edema, hyperemia, and necrosis/scarring as seen on T2-weighted, early gadolinium and late gadolinium enhancement sequences [9]. However, qualitative analysis may miss the presence of edema in patients with diffuse homogeneous or subtle involvement and early gadolinium enhancement has been notoriously difficult to interpret and reproduce. Consequently, the Lake Louise Criteria were revised in 2018, including the more robust quantitative evaluation by parametric T1 and T2 mapping [8]. The new criteria are classified into main and supportive criteria of which the main criteria are:
-
1.
Regional or global increase in native T2 times or T2 signal intensity
-
2.
T1-based markers for nonischemic myocardial damage with regional or global increase in T1 times or ECV or a nonischemic pattern of LGE
The presence of one of each of the main criteria significantly increases the specificity for acute myocarditis, while the presence of just one of the two criteria still supports the diagnosis in an appropriate clinical context. Supporting criteria include signs of pericarditis such as pericardial effusion or abnormal signal in T2, T1, or LGE, and systolic wall motion abnormality [8]. An example of acute myocarditis is demonstrated in Fig. 2.
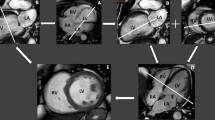
Cardiac magnetic resonance imaging (MRI) in an 88-year-old male patient with a 3-month history of progressive heart failure with dyspnea (NYHA class III). Echocardiography had shown diffuse left ventricular (LV) hypertrophy and reduced systolic and diastolic function. Cardiac MRI was performed for suspected cardiac storage disease. Late gadolinium enhancement image (a), cine image (b), and T1 mapping (c) in short-axis orientation as well as quantitative results of T1 mapping in the form of a polar map divided by AHA segments (d) are shown. Findings include marked hypertrophy of the LV myocardium with an end-diastolic septal thickness of 18 mm (a–c), diffuse late gadolinium enhancement (a), and substantially increased T1 relaxation times of 1150–1250 ms (approximately 6 standard deviations above the local reference value in healthy individuals, 1027 ± 29 ms). These findings are typical for cardiac amyloidosis
Update on cardiac sarcoidosis
Considering the low yield and potential risks of endomyocardial biopsy, imaging plays an increasing role in the diagnosis and prognostic assessment of cardiac sarcoidosis. Magnetic resonance imaging can be used to evaluate cardiac function and areas of fibrosis and F‑fluorodeoxyglucose positron emission tomography (FDG-PET) to visualize disease activity and monitor treatment response. The combination of MRI and PET allows for the differentiation between patients with and without active disease. If abnormal findings are discovered on both PET and MRI studies, this is a strong predictor for major adverse cardiac events [6, 33].
Update on MRI safety of cardiac implants
With increasing life expectancy and a growing number of patients with cardiac implantable devices, objective imaging evaluation becomes essential for follow-up. Conventionally, CMR has been contraindicated for these patients due to reports of serious complications and device heating. While implants, such as stents or prosthetic valves, are mostly MRI-safe or at least conditional, implants such as pacemakers and implantable cardioverter defibrillators (ICDs) are more complex and require a dedicated team trained to perform CMR on these patients [14]. Nevertheless, cardiac implants are no longer considered an absolute contraindication for MRI. The current generation of pacemakers have suitable technical specifications, thereby allowing for a safe CMR examination, even in patients who are pacemaker-dependent. Independent of whether the pacemakers are MRI-conditional or MRI-safe, prior presentation in cardiology is necessary for reprogramming into an MRI mode. Under certain circumstances, MRI examinations can also be performed on patients with older models, as studies have shown. For this purpose, dedicated protocols and safety measures are necessary [34].
Owing to the close spatial proximity of the pacemakers to the heart, the image quality may suffer due to artifacts, especially in sequences like phase-sensitive inversion recovery (PSIR) and steady-state free precession (SSFP) that are used for LGE and functional evaluation; however, the images are mostly of diagnostic quality [16]. The sequences may be modified for improvement of image quality, for example, by the use of wideband IR sequences for LGE evaluation will allow a more accurate assessment [13]. Therefore, the use of CMR in these patients should be reserved for clear clinical indications and information that cannot be obtained by other imaging techniques. During the scan, close hemodynamic monitoring of the patient is required by trained personnel.
Major recent trials on CMR
In recent years, several clinical trials have been published that further strengthen and refine the role of CMR in management algorithms, especially regarding coronary heart disease. A brief summary of important recent trials is given here.
CE-MARC and CE-MARC 2
The CE-MARC trial, published in 2012, was a prospective study that recruited 752 patients with suspected angina and at least one cardiovascular risk factor to undergo stress adenosine CMR, single-photon emission computed tomography (SPECT), and coronary angiography. It was found that CMR was superior to SPECT for the detection of significant coronary artery disease with invasive coronary angiography as the reference standard [10]. The CE-MARC 2 trial was a randomized clinical trial that investigated whether CMR-guided care was superior to routine care and could avoid unnecessary angiographies. Symptomatic patients (n = 1202) were randomized into three groups—routine care according to the British NICE guidelines, CMR-guided care, and myocardial perfusion scintigraphy-guided care. While major adverse cardiovascular events were similar in all three groups, fewer patients in the CMR- and scintigraphy-guided groups received “unnecessary” coronary angiographies (7.5% in the CMR group and 7.1% in the scintigraphy group vs. 28.8% in NICE guidelines group; [11]).
STRATEGY
This prospective observational registry, published in 2016, compared outcomes between patients with prior history of coronary revascularization and recurrent chest pain who were examined with CT coronary angiography versus stress-CMR. A total of 600 patients were included and followed up for a mean period of 2 years. Patients in the stress CMR group underwent fewer subsequent noninvasive tests and invasive procedures (including angiographies and revascularization procedures) and experienced fewer major adverse cardiac events [26]. This study suggests that stress-CMR should be favored over coronary computed tomography angiography (CTA) as the initial noninvasive test in patients with prior revascularization and recurrent symptoms. Figure 3 shows an example of stress-induced ischemia after a previous myocardial infarction.
Cardiac magnetic resonance imaging (MRI) in a 39-year-old man with a history of myocardial infarction 4 months previously (with percutaneous coronary intervention of the posterolateral branch of the right coronary artery) presenting with recurrent chest pain. Late gadolinium enhancement (a), adenosine stress perfusion (b), cine (c) and rest perfusion (d) images are shown, all in short-axis orientation. Findings include a small near-transmural scar in the basal inferolateral left ventricular wall (white arrow in a) and a stress-induced perfusion defect in the basal inferior wall extending beyond the area of scarring. The perfusion defect is reversible at rest (d). Findings are consistent with stress-induced ischemia adjacent to the scar and prompted repeat cardiac catheterization
MR-INFORM
This multicenter trial compared the clinical effectiveness of CMR with stress perfusion and invasive fractional flow reserve (FFR) in guiding revascularization in patients with stable angina and two or more cardiovascular risk factors or a positive exercise treadmill test. Patients (n = 918) were randomly assigned into two groups: In the MRI-guided group, revascularization was recommended if stress-CMR demonstrated relevant myocardial ischemia (≥6% of myocardium), in the FFR group revascularization was recommended for lesions with an FFR of ≤0.8. The primary outcome measures were major adverse cardiac events or target vessel revascularization. The trial demonstrated that an MRI-guided strategy was associated with a lower incidence of coronary revascularization than an FFR-guided strategy with no difference in major adverse cardiac events at the 1‑year follow-up [22]. Based on the results of the MR-INFORM trial, CMR with stress perfusion should be considered non-inferior to invasive FFR measurements for making decisions on coronary revascularization.
Updated guidelines
The European Society of Cardiology (ESC) guidelines for the diagnosis and management of chronic coronary syndromes had an important update in 2019, which has received much attention in the cardiology and cardiovascular imaging community [17]. Overall, the updated guidelines have substantially strengthened the role of noninvasive imaging in the diagnosis of coronary artery disease (CAD). The ESC has now issued a strong class I recommendation that noninvasive functional imaging or coronary CTA should be used as the initial test for diagnosing chronic CAD disease in most patients. Invasive angiography as the initial test is only considered appropriate for patients with a high pretest likelihood and severe symptoms refractory to medical therapy or a high event risk. In this context, it is important to mention that the pretest probabilities for obstructive CAD have been revised and are substantially lower in the revised 2019 ESC guidelines compared with the previous version.
The choice between coronary CTA and functional imaging testing for ischemia (stress CMR or nuclear perfusion imaging) should be based on the clinical likelihood of CAD, patient characteristics and preference, availability, and local expertise. A lower pretest likelihood of CAD favors coronary CTA over functional imaging tests, while functional imaging may be preferable for patients in the higher range of pretest probabilities.
Importantly, functional testing for ischemia (with stress CMR or nuclear perfusion imaging) is now also recommended as the next appropriate step, if coronary CTA shows CAD of uncertain functional significance or is non-diagnostic [17].
In order to further standardize cardiovascular MRI examinations, the Society for Cardiovascular Magnetic Resonance has recently (in 2020) issued updated recommendations for the acquisition, postprocessing, and reporting of cardiovascular MRI examinations [18, 31].
Applications of artificial intelligence in CMR
Artificial intelligence (AI) is quickly changing the practice of imaging, and CMR has been on the forefront of this development. Multiple AI-based algorithms are in the pipeline and many have received FDA approval, ranging from decision-making, image acquisition, reconstruction, postprocessing, and risk stratification technologies [25, 36]. Although the benefit of AI in improving patient outcomes remains to be shown, the incorporation of machine learning-based algorithms can substantially facilitate and accelerate repetitive tasks in radiological practice. Several challenges for the development and validation of accurate and clinically useful AI algorithms need to be kept in mind, including the availability of representative high-quality annotated data as a reference standard, possible biases (which might be difficult to detect due to the “black box” nature of neural networks), and the reproducibility of results. Ethical and legal aspects as well as data protection are issues, which need to be considered when such algorithms are integrated into routine radiological workflow.
Postprocessing
Artificial intelligence algorithms have simplified the process of volumetric and functional analysis of cardiac chamber and put an end to cumbersome circle drawing, also reducing interobserver variability. Several studies have shown the reproducibility of automated segmentation with results comparable or superior to human evaluation in less time [2, 3, 39]. Algorithms for automated segmentation are currently FDA licensed and are commercially available [36]. In addition to the ventricular functional assessment, regions of myocardial fibrosis and scarring can be segmented and quantified automatically by using various algorithms [21].
Diagnosis
Various models have been able to show the advantages of applying AI in diagnostics with CMR. A fully automatic deep learning algorithm has shown the ability to detect myocardial scars using non-contrast-enhanced cine images [40]. Such algorithms might reduce scan acquisition times and be beneficial for patients with contraindications for gadolinium-based contrast administration, in whom myocardial scar estimation (postcontrast LGE) might not otherwise be possible. However, these initial results need confirmation in larger studies with a more robust design.
Prognosis
With limitations in individual risk assessment in the current approaches, AI may improve risk stratification. For instance, AI may predict the response to cardiac resynchronization therapy based on a combination of image data and clinical information in patients with heart failure [24].
Practical conclusion
-
Cardiac magnetic resonance imaging (MRI) is increasingly used for the diagnosis and management of cardiac pathologies
-
This widespread use has led to a demand for physicians with expertise in the performance and interpretation of cardiac MRI is increasing.
-
Knowledge of new technologies, current guidelines, and major trials is essential to provide state-of-the-art care for cardiac patients as part of a multidisciplinary team.
References
Baggiano A, Boldrini M, Martinez-Naharro A, Kotecha T, Petrie A, Rezk T, Gritti M, Quarta C, Knight DS, Wechalekar AD, Lachmann HJ, Perlini S, Pontone G, Moon JC, Kellman P, Gillmore JD, Hawkins PN, Fontana M (2020) Noncontrast magnetic resonance for the diagnosis of cardiac amyloidosis. JACC Cardiovasc Imaging 13(1 Pt 1):69–80. https://doi.org/10.1016/j.jcmg.2019.03.026
Bai W, Sinclair M, Tarroni G, Oktay O, Rajchl M, Vaillant G, Lee AM, Aung N, Lukaschuk E, Sanghvi MM, Zemrak F, Fung K, Paiva JM, Carapella V, Kim YJ, Suzuki H, Kainz B, Matthews PM, Petersen SE, Piechnik SK, Neubauer S, Glocker B, Rueckert D (2018) Automated cardiovascular magnetic resonance image analysis with fully convolutional networks. J Cardiovasc Magn Reson 20(1):65. https://doi.org/10.1186/s12968-018-0471-x
Bhuva A, Bai W, Lau C, Davies R, Ye Y, Bulluck H, McAlindon E, Culotta V, Swoboda P, Captur G, Treibel T, Augusto J, Knott K, Seraphim A, Cole G, Petersen S, Edwards N, Greenwood J, Bucciarelli-Ducci C, Hughes A, Rueckert D, Moon J, Manisty C (2019) A multicenter, scan-rescan, human and machine learning CMR study to test generalizability and precision in imaging biomarker analysis. Circ Cardiovasc Imaging 12(10):e9214. https://doi.org/10.1161/CIRCIMAGING.119.009214
Carrick D, Haig C, Ahmed N, McEntegart M, Petrie MC, Eteiba H, Hood S, Watkins S, Lindsay MM, Davie A, Mahrous A, Mordi I, Rauhalammi S, Sattar N, Welsh P, Radjenovic A, Ford I, Oldroyd KG, Berry C (2016) Myocardial hemorrhage after acute reperfused ST-segment-elevation myocardial infarction: relation to microvascular obstruction and prognostic significance. Circ Cardiovasc Imaging 9(1):e4148. https://doi.org/10.1161/CIRCIMAGING.115.004148
Chaikriangkrai K, Abbasi MA, Sarnari R, Dolan R, Lee D, Anderson AS, Ghafourian K, Khan SS, Vorovich EE, Rich JD, Wilcox JE, Blaisdell JA, Yancy CW, Carr J, Markl M (2020) Prognostic value of myocardial extracellular volume fraction and T2-mapping in heart transplant patients. JACC Cardiovasc Imaging. https://doi.org/10.1016/j.jcmg.2020.01.014
Chang S, Lee WW, Chun EJ (2019) Recent Update of Advanced Imaging for Diagnosis of Cardiac Sarcoidosis: Based on the Findings of Cardiac Magnetic Resonance Imaging and Positron Emission Tomography. Investig Magn Reson Imaging 23(2):100. https://doi.org/10.13104/imri.2019.23.2.100
Demirkiran A, Everaars H, Amier RP, Beijnink C, Bom MJ, Götte MJW, van Loon RB, Selder JL, van Rossum AC, Nijveldt R (2019) Cardiovascular magnetic resonance techniques for tissue characterization after acute myocardial injury. Eur Heart J Cardiovasc Imaging 20(7):723–734. https://doi.org/10.1093/ehjci/jez094
Ferreira VM, Schulz-Menger J, Holmvang G, Kramer CM, Carbone I, Sechtem U, Kindermann I, Gutberlet M, Cooper LT, Liu P, Friedrich MG (2018) Cardiovascular magnetic resonance in nonischemic myocardial inflammation: expert recommendations. J Am Coll Cardiol 72(24):3158–3176. https://doi.org/10.1016/j.jacc.2018.09.072
Friedrich MG, Sechtem U, Schulz-Menger J, Holmvang G, Alakija P, Cooper LT, White JA, Abdel-Aty H, Gutberlet M, Prasad S, Aletras A, Laissy J‑P, Paterson I, Filipchuk NG, Kumar A, Pauschinger M, Liu P (2009) Cardiovascular magnetic resonance in myocarditis: a JACC white paper. J Am Coll Cardiol 53(17):1475–1487. https://doi.org/10.1016/j.jacc.2009.02.007
Greenwood JP, Maredia N, Younger JF, Brown JM, Nixon J, Everett CC, Bijsterveld P, Ridgway JP, Radjenovic A, Dickinson CJ, Ball SG, Plein S (2012) Cardiovascular magnetic resonance and single-photon emission computed tomography for diagnosis of coronary heart disease (CE-MARC): a prospective trial. Lancet 379(9814):453–460. https://doi.org/10.1016/S0140-6736(11)61335-4
Greenwood JP, Ripley DP, Berry C, McCann GP, Plein S, Bucciarelli-Ducci C, Dall’Armellina E, Prasad A, Bijsterveld P, Foley JR, Mangion K, Sculpher M, Walker S, Everett CC, Cairns DA, Sharples LD, Brown JM (2016) Effect of care guided by cardiovascular magnetic resonance, myocardial perfusion scintigraphy, or NICE guidelines on subsequent unnecessary angiography rates: the CE-MARC 2 randomized clinical trial. JAMA 316(10):1051–1060. https://doi.org/10.1001/jama.2016.12680
Haslbauer JD, Lindner S, Valbuena-Lopez S, Zainal H, Zhou H, D’Angelo T, Pathan F, Arendt CA, Bug G, Serve H, Vogl TJ, Zeiher AM, Carr-White G, Nagel E, Puntmann VO (2019) CMR imaging biosignature of cardiac involvement due to cancer-related treatment by T1 and T2 mapping. Int J Cardiol 275:179–186. https://doi.org/10.1016/j.ijcard.2018.10.023
E‑SH I, Runge M, Stojanovska J, Agarwal P, Ghadimi-Mahani M, Attili A, Chenevert T, den Harder C, Bogun F (2018) Optimized cardiac magnetic resonance imaging inversion recovery sequence for metal artifact reduction and accurate myocardial scar assessment in patients with cardiac implantable electronic devices. World J Radiol 10(9):100–107. https://doi.org/10.4329/wjr.v10.i9.100
Indik JH, Gimbel JR, Abe H, Alkmim-Teixeira R, Birgersdotter-Green U, Clarke GD, Dickfeld T‑ML, Froelich JW, Grant J, Hayes DL, Heidbuchel H, Idriss SF, Kanal E, Lampert R, Machado CE, Mandrola JM, Nazarian S, Patton KK, Rozner MA, Russo RJ, Shen W‑K, Shinbane JS, Teo WS, Uribe W, Verma A, Wilkoff BL, Woodard PK (2017) 2017 HRS expert consensus statement on magnetic resonance imaging and radiation exposure in patients with cardiovascular implantable electronic devices. Heart Rhythm 14(7):e97–e153. https://doi.org/10.1016/j.hrthm.2017.04.025
Jellis CL, Kwon DH (2014) Myocardial T1 mapping: modalities and clinical applications. Cardiovasc Diagn Ther 4(2):126–137. https://doi.org/10.3978/j.issn.2223-3652.2013.09.03
Klein-Wiele O, Garmer M, Busch M, Mateiescu S, Urbien R, Barbone G, Kara K, Schulte-Hermes M, Metz F, Hailer B, Grönemeyer D (2017) Cardiovascular magnetic resonance in patients with magnetic resonance conditional pacemaker systems at 1.5 T: influence of pacemaker related artifacts on image quality including first pass perfusion, aortic and mitral valve assessment, flow measurement, short tau inversion recovery and T1-weighted imaging. Int J Cardiovasc Imaging 33(3):383–394. https://doi.org/10.1007/s10554-016-1012-z
Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C, Prescott E, Storey RF, Deaton C, Cuisset T, Agewall S, Dickstein K, Edvardsen T, Escaned J, Gersh BJ, Svitil P, Gilard M, Hasdai D, Hatala R, Mahfoud F, Masip J, Muneretto C, Valgimigli M, Achenbach S, Bax JJ (2020) 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J 41(3):407–477. https://doi.org/10.1093/eurheartj/ehz425
Kramer CM, Barkhausen J, Bucciarelli-Ducci C, Flamm SD, Kim RJ, Nagel E (2020) Standardized cardiovascular magnetic resonance imaging (CMR) protocols: 2020 update. J Cardiovasc Magn Reson 22(1):17. https://doi.org/10.1186/s12968-020-00607-1
Leng S, Dong Y, Wu Y, Zhao X, Ruan W, Zhang G, Allen JC, Koh AS, Tan R‑S, Yip JW, Le Tan J, Chen Y, Zhong L (2019) Impaired cardiovascular magnetic resonance-derived rapid semiautomated right atrial longitudinal strain is associated with decompensated hemodynamics in pulmonary arterial hypertension. Circ Cardiovasc Imaging 12(5):e8582. https://doi.org/10.1161/CIRCIMAGING.118.008582
Lota AS, Gatehouse PD, Mohiaddin RH (2017) T2 mapping and T2* imaging in heart failure. Heart Fail Rev 22(4):431–440. https://doi.org/10.1007/s10741-017-9616-5
Moccia S, Banali R, Martini C, Muscogiuri G, Pontone G, Pepi M, Caiani EG (2019) Development and testing of a deep learning-based strategy for scar segmentation on CMR-LGE images. Magma 32(2):187–195. https://doi.org/10.1007/s10334-018-0718-4
Nagel E, Greenwood JP, McCann GP, Bettencourt N, Shah AM, Hussain ST, Perera D, Plein S, Bucciarelli-Ducci C, Paul M, Westwood MA, Marber M, Richter W‑S, Puntmann VO, Schwenke C, Schulz-Menger J, Das R, Wong J, Hausenloy DJ, Steen H, Berry C (2019) Magnetic resonance perfusion or fractional flow reserve in coronary disease. N Engl J Med 380(25):2418–2428. https://doi.org/10.1056/NEJMoa1716734
Nakamori S, Dohi K, Ishida M, Goto Y, Imanaka-Yoshida K, Omori T, Goto I, Kumagai N, Fujimoto N, Ichikawa Y, Kitagawa K, Yamada N, Sakuma H, Ito M (2018) Native T1 mapping and extracellular volume mapping for the assessment of diffuse myocardial fibrosis in dilated cardiomyopathy. JACC Cardiovasc Imaging 11(1):48–59. https://doi.org/10.1016/j.jcmg.2017.04.006
Peressutti D, Sinclair M, Bai W, Jackson T, Ruijsink J, Nordsletten D, Asner L, Hadjicharalambous M, Rinaldi CA, Rueckert D, King AP (2017) A framework for combining a motion atlas with non-motion information to learn clinically useful biomarkers: application to cardiac resynchronisation therapy response prediction. Med Image Anal 35:669–684. https://doi.org/10.1016/j.media.2016.10.002
Petersen SE, Abdulkareem M, Leiner T (2019) Artificial intelligence will transform cardiac imaging-opportunities and challenges. Front Cardiovasc Med 6:133. https://doi.org/10.3389/fcvm.2019.00133
Pontone G, Andreini D, Guaricci AI, Rota C, Guglielmo M, Mushtaq S, Baggiano A, Beltrama V, Fusini L, Solbiati A, Segurini C, Conte E, Gripari P, Annoni A, Formenti A, Petulla M, Lombardi F, Muscogiuri G, Bartorelli AL, Pepi M (2016) The STRATEGY study (stress cardiac magnetic resonance versus computed tomography coronary angiography for the management of symptomatic revascularized patients): resources and outcomes impact. Circ Cardiovasc Imaging. https://doi.org/10.1161/CIRCIMAGING.116.005171
Qi H, Jaubert O, Bustin A, Cruz G, Chen H, Botnar R, Prieto C (2019) Free-running 3D whole heart myocardial T1 mapping with isotropic spatial resolution. Magn Reson Med 82(4):1331–1342. https://doi.org/10.1002/mrm.27811
Roller FC, Fuest S, Meyer M, Harth S, Gündüz D, Bauer P, Schneider C, Rolfs A, Krombach GA, Tanislav C (2019) Natives T1-Mapping zur Beurteilung einer kardialen Beteiligung bei Morbus Fabry. Fortschr Röntgenstr 191(10):932–939. https://doi.org/10.1055/a-0836-2723
Romano S, Romer B, Evans K, Trybula M, Shenoy C, Kwong RY, Farzaneh-Far A (2020) Prognostic implications of blunted feature-tracking global longitudinal strain during vasodilator cardiovascular magnetic resonance stress imaging. JACC Cardiovasc Imaging 13(1):58–65. https://doi.org/10.1016/j.jcmg.2019.03.002
Rosa VEE, Ribeiro HB, Sampaio RO, Morais TC, Rosa MEE, Pires LJT, Vieira MLC, Mathias W, Rochitte CE, de Santis ASAL, Fernandes JRC, Accorsi TAD, Pomerantzeff PMA, Rodés-Cabau J, Pibarot P, Tarasoutchi F (2019) Myocardial fibrosis in classical low-flow, low-gradient aortic stenosis. Circ Cardiovasc Imaging 12(5):e8353. https://doi.org/10.1161/CIRCIMAGING.118.008353
Schulz-Menger J, Bluemke DA, Bremerich J, Flamm SD, Fogel MA, Friedrich MG, Kim RJ, von Knobelsdorff-Brenkenhoff F, Kramer CM, Pennell DJ, Plein S, Nagel E (2020) Standardized image interpretation and post-processing in cardiovascular magnetic resonance—2020 update: Society for cardiovascular magnetic resonance (SCMR): board of trustees task force on standardized post-processing. J Cardiovasc Magn Reson 22(1):19. https://doi.org/10.1186/s12968-020-00610-6
Seetharam K, Lerakis S (2019) Cardiac magnetic resonance imaging: the future is bright. F1000Research. https://doi.org/10.12688/f1000research.19721.1
Sharma A, Okada DR, Yacoub H, Chrispin J, Bokhari S (2020) Diagnosis of cardiac sarcoidosis: an era of paradigm shift. Ann Nucl Med 34(2):87–93. https://doi.org/10.1007/s12149-019-01431-z
Sommer T, Bauer W, Fischbach K, Kolb C, Luechinger R, Wiegand U, Lotz J, Eitel I, Gutberlet M, Thiele H, Schild HH, Kelm M, Quick HH, Schulz-Menger J, Barkhausen J, Bänsch D (2017) MR-Untersuchungen bei Patienten mit Herzschrittmachern und implantierbaren Kardioverter-Defibrillatoren. Fortschr Röntgenstr 189(3):204–217. https://doi.org/10.1055/s-0043-102029
Taylor AJ, Salerno M, Dharmakumar R, Jerosch-Herold M (2016) T1 mapping: basic techniques and clinical application. JACC Cardiovasc Imaging 9(1):67–81. https://doi.org/10.1016/j.jcmg.2015.11.005
Topol EJ (2019) High-performance medicine: the convergence of human and artificial intelligence. Nat Med 25(1):44–56. https://doi.org/10.1038/s41591-018-0300-7
Treibel TA, Fridman Y, Bering P, Sayeed A, Maanja M, Frojdh F, Niklasson L, Olausson E, Wong TC, Kellman P, Miller CA, Moon JC, Ugander M, Schelbert EB (2020) Extracellular volume associates with outcomes more strongly than native or post-contrast myocardial T1. JACC Cardiovasc Imaging 13(1 Pt 1):44–54. https://doi.org/10.1016/j.jcmg.2019.03.017
Triadyaksa P, Oudkerk M, Sijens PE (2019) Cardiac T2 * mapping: techniques and clinical applications. J Magn Reson Imaging. https://doi.org/10.1002/jmri.27023
Winther HB, Hundt C, Schmidt B, Czerner C, Bauersachs J, Wacker F, Vogel-Claussen J (2018) ν‑net: deep learning for generalized biventricular mass and function parameters using multicenter cardiac MRI data. JACC Cardiovasc Imaging 11(7):1036–1038. https://doi.org/10.1016/j.jcmg.2017.11.013
Zhang N, Yang G, Gao Z, Xu C, Zhang Y, Shi R, Keegan J, Xu L, Zhang H, Fan Z, Firmin D (2019) Deep learning for diagnosis of chronic myocardial infarction on Nonenhanced cardiac cine MRI. Radiology 291(3):606–617. https://doi.org/10.1148/radiol.2019182304
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. Busse, R. Rajagopal, S. Yücel, E. Beller, A. Öner, F. Streckenbach, D. Cantré, H. Ince, M.-A. Weber and F.G. Meinel declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies performed were in accordance with the ethical standards indicated in each case.
The supplement containing this article is not sponsored by industry.
Rights and permissions
About this article
Cite this article
Busse, A., Rajagopal, R., Yücel, S. et al. Cardiac MRI—Update 2020. Radiologe 60 (Suppl 1), 33–40 (2020). https://doi.org/10.1007/s00117-020-00687-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00117-020-00687-1