Abstract
Interferon alpha and its surrogates, including IP-10 and SIGLEC1, paralleled changes of disease activity in systemic lupus erythematosus (SLE). However, the whole blood interferon signature (WBIFNS)—the current standard for type I IFN assessment in SLE—does not correlate with SLE disease activity in individual patients over time. The underlying causes for this apparent contradiction have not been convincingly demonstrated. Using a multicenter dataset of gene expression data from leukocyte subsets in SLE, we identify distinctive subset-specific contributions to the WBIFNS. In a subsequent analysis, the effects of type I interferon on cellular blood composition in patients with SLE and hepatitis B were also studied over time. We found that type I interferon mediates significant alterations in whole blood composition, including a neutropenia and relative lymphocytosis. Given different effects of type 1 interferon on different leukocyte subsets, these shifts confound measurement of a type 1 interferon signature in whole blood. To minimize and overcome these limitations of the WBIFNS, we suggest to measure IFN-induced transcripts or proteins in a specific leukocyte subset to improve clinical impact of interferon biomarkers.
Key messages
-
Myeloid cells contribute more to the WBIFNS in SLE than their lymphocytic counterpart.
-
Very similar leukocyte subsets reveal distinctive IFN signatures.
-
IFN alpha mixes up composition of blood and leads to a preferential neutropenia, yielding relative lymphocytosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since 2003, type I interferon (IFN) signatures, defined by the simultaneous measurement of different interferon-induced transcripts (IFITs) in whole blood or PBMCs, either by PCR or microarray technologies, were used to detect IFN activity in systemic lupus erythematosus (SLE) [1–11]. Various studies have demonstrated that an indirect assessment of IFN-α by detecting downstream response molecules at the transcriptional level is more sensitive and robust than quantifying IFN-α levels directly in serum or plasma samples (with recent available technologies) [1, 12–14]. Although the term “type I IFN signature” is commonly used, a conventional definition of that signature does not yet exist. Neither the selection of IFN-induced transcripts nor materials or techniques are standardized (see Table 1).
IFN-α and IFN signatures were the first new promising biomarkers for measuring disease activity [3, 4, 15] and monitoring therapeutic effects aiming to shut down an activated IFN system in SLE [8–10, 16, 17], but later, conflicting data arose as to whether IFN is also longitudinally correlated with lupus activity.
In 2009, two independent studies did not find any correlation of the whole blood IFN signature (WBIFNS) with the SLE activity over time [5, 6]. Landolt-Marticorena et al. described a lack of association between the IFN signature and longitudinal changes in systemic lupus erythematosus disease activity index (SLEDAI) comparing two consecutive visits of 27 SLE patients, including two patients with a ΔSLEDAI ≥ 6, 11 with a ΔSLEDAI ≤ 6, and 14 with no change in SLEDAI [5]. Petri et al. confirmed these results with an improved study design by analyzing 15 patients with two paired visits that differed by a SLEDAI ≥ 4 and a further 40 visits of 11 additional SLE patients who were followed over three to five visits [6].
In contrast to these data, all of the other reports that did not determine IFN activity via the IFN signature concordantly found a correlation of IFN-α with lupus activity over time [18–21]. In the very earliest report of Hooks et al. in 1979 about elevated levels of IFN-α, as measured by its antiviral bioactivity in the sera of nine longitudinally monitored SLE patients, a strong correlation with disease activity over time was observed [18]. Two decades later, the group of Lars Ronnblöm reported that IFN-α levels increase during flares (defined as an increase in SLEDAI ≥ 4) when analyzing the serial samples of 30 SLE patients who were prospectively followed over 16 months [19]. Recently, two large studies independently demonstrated that IP-10, a chemokine that is mainly produced by monocytes upon stimulation with IFN-α, was correlated longitudinally with lupus activity [20, 21].
The reasons for the unexpected missing correlation of the IFN signature assessed in whole blood have not yet been discussed in more detail, although a differential expression of IFITs in leukocyte subsets and IFN-mediated changes in the cellular composition of whole blood or PBMCs might be attributable. With a more integrated view, Waddell et al. impressively demonstrated different transcriptional responses of leukocyte subsets upon stimulation with IFN-γ using blood from healthy donors [22]. In 2005, Kirou et al. reported that their IFN score as calculated for lupus PBMCs was significantly and independently associated with percentages of monocytes and further found that IFIT1 was eightfold more strongly induced in the CD14+ fraction than in the CD14− fraction of PBMCs in healthy donors [3]. The adhesion molecule SIGLEC1 (CD169) is one of the constituents of the IFN signature that has been described in some studies [10, 16, 23]. It is the most highly upregulated gene encoding for a surface protein in blood cells upon IFN-α stimulation [16] but is exclusively expressed in monocytes and dendritic cells [24]. Comparing the transcriptomes of leukocyte subsets from SLE patients and yellow-fever-immunized healthy controls, we could further demonstrate that cell-specific IFN signatures are differently modulated in both entities [25]. Our other studies reported similar suggestions but did not focus on this problem [26–28].
Substantial changes in absolute numbers of leukocytes are often observed in SLE—influenced by various factors like disease activity, infections, autoantibodies, and drugs [29]. Moreover, from the therapeutic use of IFN-α in hepatitis C patients, it has long been known that absolute numbers of neutrophils, lymphocytes, and thrombocytes decrease—with severe cytopenia as a therapy-limiting factor [30, 31]. In both entities, changes in leukocyte frequencies have not been addressed so far.
In this report, we demonstrate that IFN-α induces cell-type-specific IFN signatures and disarranges the cellular composition of the whole blood compartment over time. Based on these findings, we propose a strategy using cell-type-specific IFN signatures as biomarkers for the successful longitudinal monitoring of SLE patients. Moreover, these results explain why WBIFNS has failed so far in the longitudinal monitoring of SLE activity.
Material and methods
A synopsis reflecting the study design, existing substudies, included patient cohorts, and investigated leukocyte subsets is given in Table 2.
Study participants
All SLE patients fulfilled at least 4 of the 11 American College of Rheumatology (ACR) criteria for SLE [32]. Disease activity was measured using the SLEDAI or the British Isles Lupus Assessment Group (BILAG) 2004 index. Active disease was defined as a SLEDAI score ≥8 or as at least one BILAG A or two BILAG B scores. All patients with hepatitis C had a chronic and untreated infection. Viral loads and genotypes were determined by PCR. Detailed patient characteristics were previously described [25–27, 30]. Healthy donors had no signs of infections and no history of rheumatic diseases.
Definitions of IFN signatures
Studies were selected that measured IFN signatures in whole blood or PBMCs as a biomarker for disease activity or pharmacodynamics in SLE. In these studies as summarized in Table 2, different combinations of 24 genes were used as IFN signature. Because of the use of different microarray platforms, some of these IFITs could not be assessed in all analyses.
Cell-specific expression of IFN-inducible transcripts
Detailed separation strategies, procedures, materials, and purification of cell subsets (always ≥95%) are specific for recruiting sites: Cambridge, Dallas, and Berlin [25–28].
Signal log ratios (SLR) for HG-U133 arrays were calculated by the GCOS software (Affymetrix) as described elsewhere (http://mmjggl.caltech.edu/microarray/data_analysis_fundamentals_manual.pdf).
Hierarchical cluster analyses were performed by Genesis software (version 1.7.6) using Euclidean distance and average linkage clustering.
Cross-sectional differences in blood cell counts
Absolute counts and percentages of neutrophils, lymphocytes, and monocytes from local laboratory blood counts from 79 patients with SLE were compared in a cross-sectional design to those of 20 healthy controls and 42 patients with untreated chronic hepatitis C virus infection.
Longitudinal effects of IFN-α on blood cell counts
Changes of absolute counts and percentages of neutrophils, lymphocytes, and monocytes were longitudinally compared to changes of disease and IFN activity in 26 SLE patients (with a total of 77 visits). For the measurement of IFN activity, sialic acid-binding actin Ig-like lectin 1 (SIGLEC1) was determined by flow cytometry as described previously [14]. Additionally, 16 hepatitis C patients received a single IFN sensitivity testing dose of 9 megaunits (MU) IFN-α2a (n = 10) or 10 MU IFN-α2b (n = 6). After 1 week without therapy, 180 μg pegylated IFN-α2a (n = 10) or 1.5 μg/kg body weight pegylated IFN-α2b (n = 6) was administered weekly for a total of three times. Blood counts drawn at day 0 (before IFN sensitivity testing dose) and at day 21 (after the last administration of pegylated IFN-α) were evaluated.
Statistical analysis
Statistical analysis was performed with GraphPad Prism 5.0 (GraphPad, La Jolla, CA, USA) and IBM SPSS Statistics V.19.0. The significance of mean differences between related and parametric variables was determined by paired t test or one-way repeated-measure ANOVA followed by Tukey’s post hoc test as appropriate. To compare the composition of peripheral blood leukocytes in patients with SLE to healthy controls and to patients with hepatitis C, the nonparametric Kruskal-Wallis test followed by Dunn’s post hoc test was used. For analysis of correlation between the BILAG-2004 index and the expression of SIGLEC1 on monocytes with absolute counts and percentages of different leukocyte subsets, a Pearson correlation was performed. p values less than 0.05 were considered statistically significant.
Results
Quantitative characterization of cell-type-specific interferon signatures
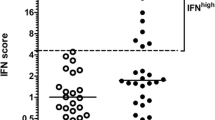
To investigate the individual contribution of different leukocyte subsets to the WBIFNS, we determined the magnitude of the IFN-induced signatures in neutrophils, monocytes, CD4+ T helper cells, CD8+ cytotoxic T cells, and CD19+ B cells from 10 SLE patients with active disease by summing up the SLR from 20 IFITs (see Table 1) (Fig. 1). Based on these transcripts, the IFN signatures in neutrophils (mean = 23.03) and monocytes (mean = 18.82) were significantly higher than those of the lymphocyte subtypes (mean CD4+ = 2.35; mean CD8+ = −1.04; mean CD19+ = 0.35). No statistically significant difference could be detected between neutrophils and monocytes or between the lymphocyte subtypes.
Neutrophils and monocytes reveal significantly higher IFN signatures than T and B cells. The magnitude of IFN signatures was calculated using the sum of signal log ratios from 20 IFN-induced genes and compared in neutrophils, monocytes, T helper cells, and cytotoxic T cells and B cells from 10 patients with active SLE. Statistical significance was determined using a one-way repeated-measure ANOVA (F value) followed by Tukey’s post hoc test (**p < 0.01, ns = not significant). Horizontal bars denote the mean. Neutrophils revealed a significantly higher IFN signature than T helper cells and cytotoxic T cells and B cells (all p < 0.001). Additionally, monocytes had a significantly higher IFN signature than T helper cells (p < 0.01) and cytotoxic T cells (p < 0.001) and B cells (p < 0.01). No statistically significant difference could be detected between neutrophils and monocytes or between the lymphocyte subtypes
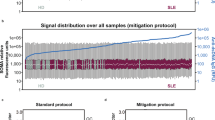
To confirm this finding, an independent transcriptome dataset was analyzed in the same way but was based on 23 IFITs (see Table 2). The magnitude of the IFN signatures was compared in monocytes, CD4+ T helper cells, and CD19+ B cells from six SLE patients with active disease (SLEDAI ≥ 8) and five SLE patients with less active disease (SLEDAI ≤ 7) (Fig. 2a). Six patients, including five patients with active disease (SLEDAI ≥ 8) and one patient with SLEDAI = 7, had prominent IFN signatures in all three cell lines. The other five patients with low IFN signatures had less active disease (SLEDAI ≤ 7). IFN-signature-positive patients were further examined separately from the IFN-signature-negative patients: monocytes (mean = 95.21) revealed again a significant higher IFN signature than did T helper cells (mean = 80.13) and B cells (mean = 77.76).
Monocytes, T helper cells, and B cells reveal substantial differences in the quantity of their IFN signatures. a The magnitude of IFN signatures was calculated using the sum of signal log ratios from 23 IFN-induced genes and compared in monocytes, T helper cells, and B cells from six SLE patients with active and five SLE patients with less active disease (left graph). Six SLE patients showed prominent IFN signatures in all three leukocyte subsets and were analyzed separately (right graph). Statistical significance was determined using a one-way repeated-measure ANOVA (F value) followed by Tukey’s post hoc test (***p < 0.001, ns = not significant). Horizontal bars denote the mean. In IFN-signature-positive patients, monocytes had a significantly higher IFN signature than T helper cells and B cells. b Expression levels from 21 IFITs as calculated using the signal log ratio were examined individually in monocytes (green), T helper cells (blue), and B cells (magenta). The three graphs above show the means of gene expression levels from the six IFN-signature-positive SLE patients in monocytes and both lymphocyte subtypes. The lower graphs compare the means of gene expression levels between all three cell lines in an overlay. Statistical significance was determined using a one-way repeated-measure ANOVA followed by Tukey’s post hoc test (*p < 0.05, **p < 0.01, and ***p < 0.001). Expression differences depend on the selected interferon-induced transcripts. c SLE monocytes separate from SLE lymphocytes based on their IFN signature in principal component (PC) analysis using Genesis software. Distributions of monocytes (green), T helper cells (blue), and B cells (magenta) are visualized in two two-dimensional plots (second view: same data rotated around the y-axis by 90° to the right) in PC analysis. PC1, PC2, and PC3 explained a variation of 32.76, 21.31, and 14.81%, respectively. Separation of T and B cells is less clear
Next, transcriptome data from the six IFN-signature-positive patients were used to study the individual expression levels from 21 IFITs (Fig. 2b). Because LTK and CD63 were expressed at very low levels in all of the investigated samples, these two IFITs were not considered here. This analysis showed that cell-type-specific quantitative differences in gene expression of selected IFITs were ascertained. Thus, the expression of EIF2AK2, HERC5, IFI44L, IFIT1, PLSCR1, and RTP4 did not differ significantly between the three leukocyte subtypes. In contrast, there was a significantly elevated expression of IFI27, LY6E, OAS2, OAS3, OASL, RSAD2, SIGLEC1, and USP18 in monocytes compared to both lymphocyte subtypes. IFI44, ISG15, and SPATS2L were expressed significantly higher in B cells than in monocytes. T cells also revealed a significantly elevated expression of OAS1 compared to both monocytes and B cells. Besides OAS1, T and B cells differ significantly in the expression of IFI6, IFI44, IFIT3, MX1, OASL, and USP18.
In SLE, leukocyte subtypes can be classified according to their specific IFN signatures
To validate the observation that leukocyte subsets present unique IFN responses, the gene expression levels in monocytes, T helper cells, and B cells from six IFN-signature-positive SLE patients (see Fig. 2a) and six healthy donors were visualized as a heat map by hierarchical clustering. As shown in supplementary Fig. 1, all of the SLE samples were clearly separated from healthy donors, but most importantly, even the different cell types were grouped as separate clusters according to their cell-specific IFN responses. The same holds true when using principal component analysis (see Fig. 2c). Leukocyte subtypes from normal donors allowed no cell-type-specific clustering.
We next examined whether closely related leukocyte subtypes that share many similarities in phenotype and function can be distinguished based on their IFN signatures. First, the IFN signatures—defined by 24 IFITs (see Table 2)—in plasma cells and plasma cell progenitors (plasmablasts) from four active SLE patients and four healthy donors were investigated by a hierarchical cluster analysis (Fig. 3a). As a result, the cluster dendrogram for plasma cells and plasmablasts clearly showed separated cell-specific branches in SLE.
IFN signatures distinguish closely related plasma cells from plasmablasts and inflammatory from resident monocytes. a Hierarchical clustering of IFN signatures in plasma cells and plasmablasts from four patients with active SLE and four normal donors (ND). b Hierarchical clustering of IFN signatures in inflammatory (inf) and resident (res) monocytes from four patients with active SLE and four and three normal donors (ND), respectively. The interferon signature was defined by 24 interferon-induced genes. For some of these genes, several probe sets were used. Gene expression levels were calculated using signal log ratios. The expression values are represented by color changes. Red indicates relatively upregulated and green relatively downregulated transcripts
The same holds true for transcriptome data from another four active SLE patients when comparing the IFN signatures of CD14++CD16+ inflammatory and CD14+/−CD16+ resident monocytes, the two major subpopulations of monocytes that are found in human peripheral blood (Fig. 3b). For monocytes from SLE patients, a perfect classification of subsets was obtained. Thus, the hierarchical cluster analyses clearly indicate that IFN signatures are modulated in a cell-specific manner.
Composition of peripheral blood leukocytes in SLE is highly different from that of healthy controls and untreated patients with hepatitis C
Considering the existence of cell-type-specific type I IFN signatures as shown before, it can be assumed that differences in the composition of peripheral blood leukocytes will bias the transcriptomic analyses of whole blood in SLE. Therefore, we compared the absolute counts and frequencies of leukocyte subsets from 79 SLE patients to 20 age- and sex-matched healthy donors and to 42 untreated hepatitis C patients (Fig. 4). Factors potentially influencing blood compartment in SLE like lupus activity and medication were not further addressed in this cross-sectional analysis.
Composition of peripheral blood leukocytes in SLE is highly different from that of healthy controls and untreated patients with hepatitis C. a Absolute counts and b percentages of neutrophils, lymphocytes, and monocytes compared in patients with SLE (n = 79), normal donors (ND; n = 20), and untreated patients with hepatitis C (HepC; n = 42). Statistical significance was determined using Kruskal-Wallis test followed by Dunn’s post hoc test (*p < 0.05, **p < 0.01, and ***p < 0.001). Horizontal bars denote the median. Dotted lines show the normal reference ranges
Although the absolute counts of neutrophils in SLE patients and healthy donors did not show a significant difference, their percentages were significantly increased in SLE patients. The number and percentage of lymphocytes were significantly reduced in SLE patients when compared to healthy controls, indicating that lymphocytopenia is a common feature in lupus pathology. In contrast, the distribution of monocytes did not significantly differ between SLE patients and healthy controls.
Remarkably, the absolute counts and frequencies of leukocyte subsets in untreated patients with hepatitis C were very similar to those observed in healthy donors. Only monocyte counts and percentages were significantly higher in hepatitis C patients. Thus, the comparison of patients with SLE and hepatitis C revealed the same results as did the comparison of SLE patients and healthy controls concerning changes in leukocyte percentages in SLE.
SLE disease activity and interferon alpha change leukocyte composition over time
To elucidate the influences of disease activity and IFN-α on the composition of peripheral blood leukocytes over time, longitudinal data from 26 SLE patients, including 77 visits, were investigated. Changes in BILAG-2004 and SIGLEC1, as surrogate markers for IFN activity, were compared with changes in the absolute counts and frequencies of neutrophils, lymphocytes, and monocytes (Table 3).
There was a negative correlation between both disease activity and SIGLEC1 and absolute counts of neutrophils, but no statistically significant relationship was observed with the counts of other leukocyte subsets. Interestingly, disease activity correlated inversely with the percentage of neutrophils and positively with those of lymphocytes and monocytes. SIGLEC1 correlated similarly to BILAG-2004 with the percentage of neutrophils and lymphocytes. No correlation could be detected between SIGLEC1 and the percentage of monocytes.
To further discriminate the effects of IFN-α on blood composition from that of SLE disease activity, the leukocyte counts and percentages of 16 hepatitis C patients were compared before and after three administrations of subcutaneous pegylated IFN-α (once weekly 180 μg of Peg-IFN-α2a or 1.5 μg/kg of Peg-IFN-α2b) (Fig. 5).
Interferon alpha treatment strongly affects the composition of peripheral blood leukocytes. Absolute counts and percentages of neutrophils, lymphocytes, and monocytes in patients with hepatitis C were compared before (day (d) 0) and after (day (d) 21) three administrations of subcutaneous pegylated interferon alpha (once weekly 180 μg Peg-IFN-α2a or 1.5 μg/kg Peg-IFN-α2b). Statistical significance was determined using the paired t test (*p < 0.05, **p < 0.01, and ***p < 0.001). Horizontal bars denote the mean
After treatment with IFN-α, counts of neutrophils, lymphocytes, and monocytes were significantly suppressed. However, absolute counts of neutrophils and monocytes decreased by 54.2 and 32.1%, respectively, while lymphocyte numbers only decreased by 15.5%. These differences in the reduction of cell numbers strongly affected the percentages of leukocytes: within 21 days of IFN administration, the leukocyte frequencies (neutrophils:lymphocytes:monocytes) changed from approximately 60:30:10 to approximately 45:45:10.
Discussion
In the present study, we described critical parameters leading to a significant bias in the evaluation of type I IFN signatures in whole blood or PBMCs as biomarkers of lupus activity. We illuminate that the measurement of an IFN signature in mixed cell populations is associated with several problems that are caused by quantitative and qualitative differences in IFN responses and changes in the composition of peripheral blood leukocytes as influenced by disease activity and IFN-α themselves. Cell-specific analyses of transcriptomes or proteomes will overcome these problems and, therefore, should become standards in monitoring disease activity in SLE and other interferonopathies in the future.
When we first compared the amplitude of IFN signatures in leukocyte subsets of SLE patients, we found that neutrophils and monocytes—as representatives of innate immunity—contribute by a significantly stronger response to the WBIFNS than do B and T cells. Moreover, it must be noted that we did not consider the mRNA expression of reticulocytes and thrombocytes that may also contribute to the WBIFNS [33], as described for thrombocytes of SLE patients [34]. To our knowledge, IFN responses have not been investigated so far in immature erythrocyte precursor cells.
Based on the most frequently used IFITs (see Table 1) and as illustrated by hierarchical clustering and principal component analysis, we could clearly demonstrate that leukocyte subsets were characterized by cell-type-specific IFN signatures. These data agree with the cell-distinct gene responses upon IFN-γ in healthy controls shown by Waddell et al. [35]. Remarkably, a classification of different—even closely related—cell types, such as plasmablasts and plasma cells, was possible according to their particular IFN signatures, using only approximately 1% of 2100 IFN-α-related genes [36].
Comparing the relative frequencies of leukocytes in SLE patients and healthy controls, dramatic differences were observed. Thus, the comparability of whole blood samples from SLE and healthy donors for -omic studies seems per se to be questionable. The same holds true for analyzing PBMCs in SLE because of a significantly decreased percentage of CD4+ T cells [26] and the contamination with low-density neutrophils that cannot be separated by density-gradient centrifugation [2, 37]. These facts query many -omic studies done so far.
Disruptive factors destabilizing the blood composition in SLE include lupus activity, viral and bacterial infections, cell-destroying autoantibodies, and medication (e.g., glucocorticoids or cyclophosphamide) [29]. In addition, IFN-α can affect the absolute counts of leukocytes [19, 30, 31], but changes in frequencies have not yet been investigated in detail. Here, we correlated the disease activity and the expression of SIGLEC1 to changes in the cellular blood composition of 26 SLE patients over time and found that both seemed to be coregulated and were related to a significant reduction of absolute neutrophil counts. Thus, in active SLE patients, dramatic shifts in leukocyte frequencies can be observed: the percentage of neutrophils decreased, while that of lymphocytes relatively increased.
To more clearly elaborate the blood effects of IFN-α, we next examined the blood of patients with hepatitis C before and after therapy with pegylated IFN-α. Again, a prominent decrease in neutrophils was observed—very similar to that during a SLE flare or an acute viral infection. By consequence, the ratio of neutrophils to lymphocytes changed in favor of the latter. Thus, it is expectable that type I IFN inhibitors also affect cellular blood composition in IFN-positive SLE patients.
With a global perspective, it appears that neutrophils and monocytes are more sensitive to IFN-α: both subsets reveal higher IFN signatures than B or T cells and, during IFN-α therapy, their absolute numbers decrease much more strongly than do those of lymphocytes. The higher sensitivity of myeloid cells can be explained by a higher density of IFN receptor expression. Tochizawa et al. studied expression of IFNAR2, one of the two subunits of type I IFN receptor, in a leukocyte-specific manner by flow cytometry and observed a significant higher IFNAR2 expression on neutrophils, monocytes, and NK cells in healthy individuals; even more pronounced after blood stimulation with recombinant IFN-α [38]. Alternatively, the IFN-α-induced suppression of neutrophil colony-stimulating factor (G-CSF) or an induction of FAS expression could be responsible for the decrease in neutrophil and monocyte counts [19, 39].
In light of the presented cell-specific and IFN-α-induced considerations, it becomes obvious why the WBIFNS failed in reflecting changes of disease activity over time in SLE [5, 6]. Because neutrophils showed a stronger IFN response than did lymphocytes, the WBIFNS during a SLE flare is strongly biased by neutropenia accompanied by a relative lymphocytosis. In principle, these observations are applicable to other IFN-mediated rheumatic diseases, such as Sjögren’s syndrome [40], immune thrombocytopenia [41], genetic interferonopathies [42, 43], and viral infections [44, 45].
In conclusion, we show suggestive data that the highest diagnostic power of IFN signatures as biomarkers for monitoring SLE disease activity is achieved when their assessment is performed in a cell-specific manner. This assessment can be performed at the transcriptional manner but is dependent on an enrichment of the target cell population, or analyses must be performed by appropriate mRNA-based flow cytometric procedures. It must be determined whether bioinformatic tools, such as the deconvolution [46] of WBIFNS, will allow a reliable readout of cell-specific signatures. The last method—despite its unproven status—would enable the reanalysis of WBIFNS assessed in clinical trials to rechallenge the relationship of IFN signatures with the disease activity and pharmacodynamic action of IFN-α inhibitors. Alternatively, transcriptional signatures must be translated at the protein level, enabling flow cytometric measurements at the single-cell level, as shown for SIGLEC1 [14, 24, 27] and CD64 [47, 48], or for being independent from cell-based assays by the detection of mediators that are released in serum, such as IP-10 [14, 20, 21], or the IFN gene reporter assay [49]. However, as previously shown [14], the highest sensitivity is rather ensured by monitoring cell-associated biomarkers, which are not influenced by dilution or adsorption effects in the bloodstream. To reevaluate the diagnostic power of interferon signatures in SLE and other interferon-driven diseases, the implementation of appropriate biomarker/biosignature assays in clinical studies is urgently needed.
References
Baechler EC, Batliwalla FM, Karypis G, Gaffney PM, Ortmann WA, Espe KJ, Shark KB, Grande WJ, Hughes KM, Kapur V et al (2003) Interferon-inducible gene expression signature in peripheral blood cells of patients with severe lupus. Proc Natl Acad Sci U S A 100:2610–2615
Bennett L, Palucka AK, Arce E, Cantrell V, Borvak J, Banchereau J, Pascual V (2003) Interferon and granulopoiesis signatures in systemic lupus erythematosus blood. J Exp Med 197:711–723
Kirou KA, Lee C, George S, Louca K, Peterson MG, Crow MK (2005) Activation of the interferon-alpha pathway identifies a subgroup of systemic lupus erythematosus patients with distinct serologic features and active disease. Arthritis Rheum 52:1491–1503
Feng X, Wu H, Grossman JM, Hanvivadhanakul P, FitzGerald JD, Park GS, Dong X, Chen W, Kim MH, Weng HH et al (2006) Association of increased interferon-inducible gene expression with disease activity and lupus nephritis in patients with systemic lupus erythematosus. Arthritis Rheum 54:2951–2962
Landolt-Marticorena C, Bonventi G, Lubovich A, Ferguson C, Unnithan T, Su J, Gladman DD, Urowitz M, Fortin PR, Wither J (2009) Lack of association between the interferon-alpha signature and longitudinal changes in disease activity in systemic lupus erythematosus. Ann Rheum Dis 68:1440–1446
Petri M, Singh S, Tesfasyone H, Dedrick R, Fry K, Lal P, Williams G, Bauer J, Gregersen P, Behrens T et al (2009) Longitudinal expression of type I interferon responsive genes in systemic lupus erythematosus. Lupus 18:980–989
Yao Y, Higgs BW, Richman L, White B, Jallal B (2010) Use of type I interferon-inducible mRNAs as pharmacodynamic markers and potential diagnostic markers in trials with sifalimumab, an anti-IFNalpha antibody, in systemic lupus erythematosus. Arthritis Res Ther 12(Suppl 1):S6
McBride JM, Jiang J, Abbas AR, Morimoto A, Li J, Maciuca R, Townsend M, Wallace DJ, Kennedy WP, Drappa J (2012) Safety and pharmacodynamics of rontalizumab in patients with systemic lupus erythematosus: results of a phase I, placebo-controlled, double-blind, dose-escalation study. Arthritis Rheum 64:3666–3676
Petri M, Wallace DJ, Spindler A, Chindalore V, Kalunian K, Mysler E, Neuwelt CM, Robbie G, White WI, Higgs BW et al (2013) Sifalimumab, a human anti-interferon-a monoclonal antibody, in systemic lupus erythematosus: a phase 1 randomized controlled, dose-escalation study. Arthritis Rheum. doi:10.1002/art.37824
Lauwerys BR, Hachulla E, Spertini F, Lazaro E, Jorgensen C, Mariette X, Haelterman E, Grouard-Vogel G, Fanget B, Dhellin O et al (2013) Down-regulation of interferon signature in systemic lupus erythematosus patients by active immunization with interferon alpha-kinoid. Arthritis Rheum 65:447–456
Kalunian KC, Merrill JT, Maciuca R, McBride JM, Townsend MJ, Wei X, Davis JC Jr, Kennedy WP (2016) A phase II study of the efficacy and safety of rontalizumab (rhuMAb interferon-alpha) in patients with systemic lupus erythematosus (ROSE). Ann Rheum Dis 75:196–202
Preble OT, Rothko K, Klippel JH, Friedman RM, Johnston MI (1983) Interferon-induced 2′-5′ adenylate synthetase in vivo and interferon production in vitro by lymphocytes from systemic lupus erythematosus patients with and without circulating interferon. J Exp Med 157:2140–2146
von Wussow P, Jakschies D, Hochkeppel H, Horisberger M, Hartung K, Deicher H (1989) MX homologous protein in mononuclear cells from patients with systemic lupus erythematosus. Arthritis Rheum 32:914–918
Rose T, Grutzkau A, Hirseland H, Huscher D, Dahnrich C, Dzionek A, Ozimkowski T, Schlumberger W, Enghard P, Radbruch A et al (2013) IFNalpha and its response proteins, IP-10 and SIGLEC-1, are biomarkers of disease activity in systemic lupus erythematosus. Ann Rheum Dis 72:1639–1645
Hooks JJ, Jordan GW, Cupps T, Moutsopoulos HM, Fauci AS, Notkins AL (1982) Multiple interferons in the circulation of patients with systemic lupus erythematosus and vasculitis. Arthritis Rheum 25:396–400
Yao Y, Higgs BW, Morehouse C, de Los RM, Trigona W, Brohawn P, White W, Zhang J, White B, Coyle AJ et al (2009) Development of potential pharmacodynamic and diagnostic markers for anti-IFN-alpha monoclonal antibody trials in systemic lupus erythematosus. Hum Genomics Proteomics 1:374312
Morimoto AM, Flesher DT, Yang J, Wolslegel K, Wang X, Brady A, Abbas AR, Quarmby V, Wakshull E, Richardson B et al (2011) Association of endogenous anti-interferon-alpha autoantibodies with decreased interferon-pathway and disease activity in patients with systemic lupus erythematosus. Arthritis Rheum 63:2407–2415
Hooks JJ, Moutsopoulos HM, Geis SA, Stahl NI, Decker JL, Notkins AL (1979) Immune interferon in the circulation of patients with autoimmune disease. N Engl J Med 301:5–8
Bengtsson AA, Sturfelt G, Truedsson L, Blomberg J, Alm G, Vallin H, Ronnblom L (2000) Activation of type I interferon system in systemic lupus erythematosus correlates with disease activity but not with antiretroviral antibodies. Lupus 9:664–671
Kong KO, Tan AW, Thong BY, Lian TY, Cheng YK, Teh CL, Koh ET, Chng HH, Law WG, Lau TC et al (2009) Enhanced expression of interferon-inducible protein-10 correlates with disease activity and clinical manifestations in systemic lupus erythematosus. Clin Exp Immunol 156:134–140
Bauer JW, Petri M, Batliwalla FM, Koeuth T, Wilson J, Slattery C, Panoskaltsis-Mortari A, Gregersen PK, Behrens TW, Baechler EC (2009) Interferon-regulated chemokines as biomarkers of systemic lupus erythematosus disease activity: a validation study. Arthritis Rheum 60:3098–3107
Waddell SJ, Popper SJ, Rubins KH, Griffiths MJ, Brown PO, Levin M, Relman DA (2010) Dissecting interferon-induced transcriptional programs in human peripheral blood cells. PLoS One 5:e9753
Merrill JT, Wallace DJ, Petri M, Kirou KA, Yao Y, White WI, Robbie G, Levin R, Berney SM, Chindalore V et al (2011) Safety profile and clinical activity of sifalimumab, a fully human anti-interferon alpha monoclonal antibody, in systemic lupus erythematosus: a phase I, multicentre, double-blind randomised study. Ann Rheum Dis 70:1905–1913
Biesen R, Demir C, Barkhudarova F, Grun JR, Steinbrich-Zollner M, Backhaus M, Haupl T, Rudwaleit M, Riemekasten G, Radbruch A et al (2008) Sialic acid-binding Ig-like lectin 1 expression in inflammatory and resident monocytes is a potential biomarker for monitoring disease activity and success of therapy in systemic lupus erythematosus. Arthritis Rheum 58:1136–1145
Kyogoku C, Smiljanovic B, Grun JR, Biesen R, Schulte-Wrede U, Haupl T, Hiepe F, Alexander T, Radbruch A, Grutzkau A (2013) Cell-specific type I IFN signatures in autoimmunity and viral infection: what makes the difference? PLoS One 8:e83776
Lyons PA, McKinney EF, Rayner TF, Hatton A, Woffendin HB, Koukoulaki M, Freeman TC, Jayne DR, Chaudhry AN, Smith KG (2010) Novel expression signatures identified by transcriptional analysis of separated leucocyte subsets in systemic lupus erythematosus and vasculitis. Ann Rheum Dis 69:1208–1213
Becker AM, Dao KH, Han BK, Kornu R, Lakhanpal S, Mobley AB, Li QZ, Lian Y, Wu T, Reimold AM et al (2013) SLE peripheral blood B cell, T cell and myeloid cell transcriptomes display unique profiles and each subset contributes to the interferon signature. PLoS One 8:e67003
Yoshida T, Mei H, Dorner T, Hiepe F, Radbruch A, Fillatreau S, Hoyer BF (2010) Memory B and memory plasma cells. Immunol Rev 237:117–139
Hepburn AL, Narat S, Mason JC (2010) The management of peripheral blood cytopenias in systemic lupus erythematosus. Rheumatology (Oxford) 49:2243–2254
Peck-Radosavljevic M, Wichlas M, Homoncik-Kraml M, Kreil A, Hofer H, Jessner W, Gangl A, Ferenci P (2002) Rapid suppression of hematopoiesis by standard or pegylated interferon-alpha. Gastroenterology 123:141–151
Soza A, Everhart JE, Ghany MG, Doo E, Heller T, Promrat K, Park Y, Liang TJ, Hoofnagle JH (2002) Neutropenia during combination therapy of interferon alfa and ribavirin for chronic hepatitis C. Hepatology 36:1273–1279
Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield NF, Schaller JG, Talal N, Winchester RJ (1982) The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 25:1271–1277
Kabanova S, Kleinbongard P, Volkmer J, Andree B, Kelm M, Jax TW (2009) Gene expression analysis of human red blood cells. Int J Med Sci 6:156–159
Lood C, Amisten S, Gullstrand B, Jonsen A, Allhorn M, Truedsson L, Sturfelt G, Erlinge D, Bengtsson AA (2010) Platelet transcriptional profile and protein expression in patients with systemic lupus erythematosus: up-regulation of the type I interferon system is strongly associated with vascular disease. Blood 116:1951–1957
Courtney PA, Crockard AD, Williamson K, Irvine AE, Kennedy RJ, Bell AL (1999) Increased apoptotic peripheral blood neutrophils in systemic lupus erythematosus: relations with disease activity, antibodies to double stranded DNA, and neutropenia. Ann Rheum Dis 58:309–314
Samarajiwa SA, Forster S, Auchettl K, Hertzog PJ (2009) INTERFEROME: the database of interferon regulated genes. Nucleic Acids Res 37:D852–D857
Hacbarth E, Kajdacsy-Balla A (1986) Low density neutrophils in patients with systemic lupus erythematosus, rheumatoid arthritis, and acute rheumatic fever. Arthritis Rheum 29:1334–1342
Tochizawa S, Akamatsu S, Sugiyama Y, Muraguchi M, Ohmoto Y, Ono Y, Ishikawa H, Tanigami A, Sumida T, Mori T (2004) A flow cytometric method for determination of the interferon receptor IFNAR2 subunit in peripheral blood leukocyte subsets. J Pharmacol Toxicol Methods 50:59–66
Shoshan Y, Shapira I, Toubi E, Frolkis I, Yaron M, Mevorach D (2001) Accelerated Fas-mediated apoptosis of monocytes and maturing macrophages from patients with systemic lupus erythematosus: relevance to in vitro impairment of interaction with iC3b-opsonized apoptotic cells. J Immunol 167:5963–5969
Maria NI, Brkic Z, Waris M, van Helden-Meeuwsen CG, Heezen K, van de Merwe JP, van Daele PL, Dalm VA, Drexhage HA, Versnel MA (2014) MxA as a clinically applicable biomarker for identifying systemic interferon type I in primary Sjogren’s syndrome. Ann Rheum Dis 73:1052–1059
Sehgal K, Guo X, Koduru S, Shah A, Lin A, Yan X, Dhodapkar KM (2013) Plasmacytoid dendritic cells, interferon signaling, and FcgammaR contribute to pathogenesis and therapeutic response in childhood immune thrombocytopenia. Sci Transl Med 5:193ra189
Crow YJ (2011) Type I interferonopathies: a novel set of inborn errors of immunity. Ann N Y Acad Sci 1238:91–98
Crow YJ, Casanova JL (2014) STING-associated vasculopathy with onset in infancy—a new interferonopathy. N Engl J Med 371:568–571
Ramilo O, Allman W, Chung W, Mejias A, Ardura M, Glaser C, Wittkowski KM, Piqueras B, Banchereau J, Palucka AK et al (2007) Gene expression patterns in blood leukocytes discriminate patients with acute infections. Blood 109:2066–2077
Zaas AK, Chen M, Varkey J, Veldman T, Hero AO 3rd, Lucas J, Huang Y, Turner R, Gilbert A, Lambkin-Williams R et al (2009) Gene expression signatures diagnose influenza and other symptomatic respiratory viral infections in humans. Cell Host Microbe 6:207–217
Abbas AR, Wolslegel K, Seshasayee D, Modrusan Z, Clark HF (2009) Deconvolution of blood microarray data identifies cellular activation patterns in systemic lupus erythematosus. PLoS One 4:e6098
Li Y, Lee PY, Kellner ES, Paulus M, Switanek J, Xu Y, Zhuang H, Sobel ES, Segal MS, Satoh M et al (2010) Monocyte surface expression of Fcgamma receptor RI (CD64), a biomarker reflecting type-I interferon levels in systemic lupus erythematosus. Arthritis Res Ther 12:R90
Kikuchi-Taura A, Yura A, Tsuji S, Ohshima S, Kitatoube A, Shimizu T, Nii T, Katayama M, Teshigawara S, Yoshimura M et al (2015) Monocyte CD64 expression as a novel biomarker for the disease activity of systemic lupus erythematosus. Lupus. doi:10.1177/0961203315579093
Hua J, Kirou K, Lee C, Crow MK (2006) Functional assay of type I interferon in systemic lupus erythematosus plasma and association with anti-RNA binding protein autoantibodies. Arthritis Rheum 54:1906–1916
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The work was supported by the Sixth Framework Programme (project AutoCure; LSHB-CT-2006-018861), the German Research Foundation (grant number SFB650 TP12), the IMI JU-funded project BeTheCure (contract number 115142-29), and the Zukunftsfond Berlin (contract number 101399339). PAL and SMF were funded by project grants from the Medical Research Council (G0400929) and the Wellcome Trust (094227/Z/10/Z). SMF was supported by a Wellcome Trust Translational Medicine and Therapeutics PhD Studentship. Cambridge Institute for Medical Research is in receipt of a Wellcome Trust Strategic Award (079895). LSD was supported by an Alliance for Lupus Research (ALR) Award #257549 and National Institutes of Health grants AR067625 (PI, Satterthwaite) and AI122720 (PI, Satterthwaite).
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
.
ESM 1
(PDF 238 kb)
Rights and permissions
About this article
Cite this article
Strauß, R., Rose, T., Flint, S.M. et al. Type I interferon as a biomarker in autoimmunity and viral infection: a leukocyte subset-specific analysis unveils hidden diagnostic options. J Mol Med 95, 753–765 (2017). https://doi.org/10.1007/s00109-017-1515-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-017-1515-7