Abstract
ZSTK474 [2-(2-difluoromethylbenzimidazol-1-yl)-4,6-dimorpholino-1,3,5-triazine] is a novel phosphatidylinositol 3-kinase (PI3K) inhibitor that exhibits potent antitumor effects. Recent studies have shown that ZSTK474 is also with anti-inflammatory properties in collagen-induced arthritis. However, the effects of ZSTK474 on dendritic cells and inflammatory Th17 cell-mediated autoimmune central nervous system inflammation are not understood. In this study, we demonstrated that ZSTK474 suppressed human CD14+ monocyte-derived dendritic cell differentiation, maturation, and endocytosis, and further inhibited the stimulatory function of mature dendritic cell on allogeneic T cell proliferation. In addition, ZSTK474 inhibited the expression of dendritic cell-derived Th1 and Th17 cells polarizing cytokines interferon-γ/interleukin (IL)-12 and IL-6/IL-23. Furthermore, our results indicated that the in vivo administration of ZSTK474, which targets the dendritic cell and inflammatory Th1 and Th17 cell, led to a reduction of clinical score, central nervous system inflammation, and demyelination of mouse experimental autoimmune encephalomyelitis. Therefore, ZSTK474 significantly suppressed the human CD14+ monocyte-derived dendritic cell functions and ameliorated mouse experimental autoimmune encephalomyelitis. We further found that ZSTK474 inhibited the phosphorylation of PI3K downstream signaling Akt and glycogen synthase kinase 3 beta in the dendritic cell. These data suggested that ZSTK474 exerted potent anti-inflammatory and immunosuppressive properties via PI3K signaling and may serve as a potential therapeutic drug for multiple sclerosis and other autoimmune inflammatory diseases.
Key Messages
• ZSTK474 inhibits dendritic cell (DC) differentiation and maturation.
• ZSTK474 inhibits DC-derived Th1 and Th17-polarizing cytokines.
• ZSTK474 ameliorates EAE and suppresses DCs, Th1, and Th17 cells in EAE.
• ZSTK474 reduces CNS inflammation and demyelination of EAE mice.
• ZSTK474 could be a potential therapeutic drug for multiple sclerosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In a variety of cell types, the phosphoinositide 3-kinase (PI3K)/Akt signal transduction pathway is essential for most key cellular responses [1]. The most studied class I PI3Ks are a family of dual-specificity lipid and protein kinases which include class IA (consisting of PI3Kα, PI3Kβ, and PI3Kδ isoforms) and class IB (consisting of PI3Kγ alone) proteins. The expressions of PI3Kα and PI3Kβ are ubiquitous; however, PI3Kδ and PI3Kγ, which were restricted to hematopoietic cells [1], are key enzymes in leukocyte signaling and are promising targets for intervention in the signaling pathways involved in inflammatory and autoimmune diseases [2].
Wortmannin and LY294002 are potent inhibitors of PI3K that have been extensively used for studying PI3K signal pathways, but they also inhibit other related enzymes [3, 4]. LY294002 causes severe dermal toxicity [5], and wortmannin and its analog has shown hepatic toxicity when administered in mice [6]. ZSTK474 [2-(2-difluoromethylbenzimidazol-1-yl)-4,6-dimorpholino-1,3,5-triazine] is a novel PI3K inhibitor that demonstrates promising antitumor effects without observable toxicity [7–11], which has been tested as an anticancer drug in phase I clinical trials [trial number: UMIN000008807]. A recent study demonstrated that ZSTK474 also exhibited anti-inflammatory properties and protected mice from collagen-induced arthritis [12], an autoimmune inflammatory disease. However, the effect of ZSTK474 on autoimmune multiple sclerosis (MS) and its animal model of experimental autoimmune encephalomyelitis (EAE) is unclear. EAE is an autoimmune disorder of the central nervous system (CNS) that serves as an animal model for the human MS disease [13].
A number of immunomodulatory drugs, including β-interferon (Avonex, Betaseron, and Rebif), glatiramer acetate (Copaxone), mitoxantrone (Novantrone), natalizumab (Tysabri), and fingolimod (Gilenya), have been introduced as a treatment for MS. There are several drug undergoing phase II and III trials. However, current drugs have proved unsatisfactory because of their toxicity in a number of patients [14]. Therefore, the improvement of MS therapy through the development of new drugs is necessary.
Dendritic cells (DCs) play a critical role in directing adaptive immune responses. At different stages of differentiation, DCs undergo changes in surface markers, migratory patterns, and cytokine production. These differences determine the differentiation of naïve T lymphocytes into the various mature effector cells, such as Th1, Th2, and Th17 cells. The initial T cell activation is dependent on T cell receptor triggering and costimulatory signaling through CD28 and CD80/CD86 which are expressed on the surface of antigen-presenting cells (APCs), such as DCs. The activation of toll-like receptors (TLR) on DCs leads to the maturation and induction of the cytokines that regulate adaptive immunity against pathogens. In addition, PI3K is activated by TLR signaling in innate immune cells in which it appears to regulate inflammatory cytokine production [15, 16]. However, the precise role of PI3K in DC activation and cytokine production is not fully understood.
The pathogenesis of many autoimmune diseases is dependent on the activation of CD4+ T cells [17–19]. Therefore, most current therapies for autoimmune disorders are target T cells. Recently, the contribution of dendritic cells (DCs) to autoimmune diseases has been examined more extensively. In this study, we are focused on inhibiting DCs to decrease the autoreactive T cell response. Therefore, we investigated whether ZSTK474 affects DC differentiation and activation by monitoring the DC cytokine production and the mature DC (mDC) allostimulatory activity on T cell proliferation and on production of T helper cells polarizing cytokines and further to ameliorate EAE. In conclusion, ZSTK474 significantly decreased PI3K and glycogen synthase kinase 3 beta (GSK3β) phosphorylation in DCs, which is critical for maintaining DCs in a tolerogenic state, by reducing the levels of various proinflammatory factors such as IFN-γ, IL-12, IL-6, and IL-23. This led to a reduction in the EAE clinical score and in CNS inflammation and demyelination. This study also provided further insights into the biological functions and clinical applications of ZSTK474 and demonstrated the need for further investigation of ZSTK474 as a potential therapeutic drug for MS and other autoimmune inflammatory diseases.
Materials and methods
Additional experimental procedures are described in the Supporting materials.
Induction and treatment of EAE
For the EAE induction, the C57BL/6 mice (aged 6–8 weeks) were immunized (s.c.) with 150 μg of myelin oligodendrocyte glycoprotein (MOG residues 35–55). The peptide sequence was Met-Glu-Val-Gly-Trp-Tyr-Arg-Ser-Pro-Phe-Ser-Arg-Val-Val-His-Leu-Tyr-Arg-Asn-Gly-Lys, and the purity was >95 % (CL. Bio-Scientific Co., LTD., Xi’an, China). The immunization was performed by mixing the MOG35–55 peptide with complete Freund’s adjuvant containing 5 mg/ml of heat-killed H37Ra, a Mycobacterium tuberculosis strain (Difco Laboratories). Pertussis toxin (400 ng) (List Biological Laboratories) in PBS and 50 mM NaCl was administered i.p. on the day of immunization and again after 24 h. For the treatment of EAE, the dose/route/frequency of administration drug was determined through pre-experiments. We found that low-dose (25 mg/kg/day) ZSTK474 was not enough to ameliorate the severity of EAE, but high-dose (100 mg/kg/day) ZSTK474 were toxic to mice. ZSTK474 (25 and 50 mg/kg/day) or DMSO (vehicle control) (Sigma-Aldrich) was administered p.o. daily starting on day 7 postimmunization. The mice were weighed and examined daily for disease symptoms, which were assessed using the following standard score system: 0, no obvious changes in motor functions; 1.0, limp tail; 2.0, limp tail and wobbly gait; 3.0, bilateral hind limb paralysis; 4.0, complete hind limb and partial fore limb paralysis; and 5.0, death [20].
DC response in EAE mice
The single cell suspension was isolated from the spleens of PBS- or ZSTK474-treated EAE mice by mashing and passing the tissue through a cell strainer as we have described previously [21, 22]. For the surface staining, the splenocytes from the ZSTK474-treated or control mice were staining. The expressions of CD11c, CD80, CD86, and MHC-II were analyzed by staining the cells (0.5–1 × 106) with fluorescein isothiocyanate (FITC)-conjugated specific mAbs or isotype controls (Sungene, Tianjin, China) diluted in PBS containing 1 % BSA in accordance with the manufacturer’s protocol.
Histopathology
The spinal cords from mice transcardially perfused with 4 % paraformaldehyde were dissected and were postfixed overnight. The paraffin-embedded 5–10 μm spinal cord sections were stained with hematoxylin-eosin (H&E) for the routine histological analysis of the inflammatory infiltration and with Luxol fast blue (Alfa Aesar, Ward Hill, USA) for the evaluation of the demyelination.
Intracellular cytokine staining
The single cell suspension was isolated from the spleens of PBS- or ZSTK474-treated EAE mice by mashing and passing the tissue through a cell strainer. For the in vitro study, the splenocytes isolated from the EAE mice were cultured (in triplicate) in complete RPMI 1640 medium (containing 100 mM sodium pyruvate, 200 mM l-glutamine, 100 mg/ml kanamycin, and 10 % fetal bovine serum) at a density of 5 × 105 per well in 96-well plates in the presence of the MOG peptide (20 μg/ml). Next, the cells were restimulated with 1 μg/ml brefeldin A (Sigma, St. Louis, USA), 600 ng/ml PMA (phorbol 12-myristate 13-acetate, Enzo Life Sciences, Farmingdale, USA), and 1 μg/ml ionomycin (Enzo Life Sciences) for 5 h and were collected and washed with PBS. To stain the cell surface markers, the APC-conjugated rat antimouse CD4 antibody (eBioscience, San Diego, USA) was used. Next, the cells were fixed, permeabilized, and stained for the intracellular cytokines using PE-conjugated rat antimouse IL-17 or FITC-conjugated rat antimouse IFN-γ (eBioscience). The nonspecific staining was monitored using the isotype antibody controls. The cells were analyzed by FACS Calibur, and the acquired data were analyzed using the FlowJo software and WinMDI 2.9 software.
Statistical analysis
The experiments were performed in triplicate on three separate occasions. One-way analysis of variance (ANOVA), where applicable, was performed to determine whether an overall statistically significant change existed before the Student’s t test was used to analyze the difference between any two groups. p < 0.05 was considered statistically significant. In addition, the standard deviations from the mean, expressed as the SD values or as equivalent error bars, were calculated.
Results
ZSTK474 inhibits differentiation and endocytosis of human monocyte-derived DCs
To determine the effects of ZSTK474 on the differentiation of the monocyte-derived DCs, the purified CD14+ monocytes were allowed to differentiate into immature DCs (iDCs) in the presence of various concentrations of ZSTK474 (0.008, 0.04, and 0.2 μM), granulocyte macrophage-colony stimulating factor (GM-CSF), and IL-4. After 5 days of culture, the changes in the expression level of the costimulatory molecules CD80 and CD86, CD83, and HLA-DR were assessed using flow cytometry. Compared with the day-5-untreated iDCs, a significant dose-dependent reduction in CD80, CD86, and CD83 expressions and HLA-DR expression only at the highest concentration was observed in the ZSTK474-treated cells, demonstrated by the mean fluorescence intensity (MFI) histograms (Fig. 1a) and the percentage of the untreated control MFI levels (Fig. 1b). The results indicted that ZSTK474 inhibited the differentiation of the human CD14+ monocytes into DCs in a dose-dependent manner. We also demonstrated that the inhibited effects are not caused by the toxicity of ZSTK474 (Fig. 1c). There were no significant changes in the percentages of apoptosis and dead cells by treatment with ZSTK474.
ZSTK474 inhibits differentiation and endocytosis of monocyte-derived DCs. The cell surface markers CD80, CD83, CD86, and HLA-DR were examined on day 5 by FACS analysis. a Histograms of cell surface marker expression from one of three independent experiments. The numbers represent the MFI of the stained cells. The filled and dotted lines respectively represent the positive staining and isotype control. b Relative levels of cell markers compared with the ZSTK474 untreated controls (100 %) from three independent experiments with means ± s.d. NS > 0.05, *p < 0.05, **p < 0.01 determined by Student’s t test. The MFI level in each ZSTK474 treatment was compared to the controls, generating the percentage value relative to the controls. c The percentage of apoptosis and dead iDC treated by ZSTL474. d The FITC-dextran uptake by iDCs was evaluated by flow cytometry after 30 min of incubation with FITC-dextran at 37 °C. a 4 °C negative control; b, c, and d 0.2, 0.04, and 0.008 μM ZSTK474-treated iDCs incubated with FITC-dextran at 37 °C for 30 min; e 37 °C positive control. The peak shifting denotes the significant changes. The data are representative of three independent experiments using different blood donors
To further investigate whether ZSTK474 affected the antigen uptake capacity of the iDCs, we examined the endocytosis function of iDCs by estimating the uptake of FITC-dextran. As shown in Fig. 1d, compared with the control, the FITC-dextran uptake decreased gradually in the ZSTK474-treated iDCs in a dose-dependent manner. The maximum inhibition of the FITC-dextran uptake in the iDCs was observed following the treatment with 0.2 μM ZSTK474, which was similar to the negative control (iDCs at 4 °C). The data suggested that ZSTK474 impaired the endocytosis function of the iDCs.
ZSTK474 suppressed maturation of iDCs and mDC-induced allogeneic T cell proliferation
mDCs functionally present antigens to T cells and initiate immune responses. Therefore, it was critical to determine the effect of ZSTK474 on the phenotypic maturation of the DCs. The iDCs, with or without the ZSTK474 treatment, were activated by the addition of 1 μg/mL lipopolysaccharide (LPS) for 2 days, and the expression of the mDC surface markers CD83, CD80, CD86, and HLA-DR was determined using flow cytometry. As shown in Fig. 2a, the control mDCs demonstrated a significant increase in CD80, CD83, CD86, and HLA-DR expressions following LPS activation. However, the mDCs treated with ZSTK474 (0.008, 0.04, and 0.2 μM) demonstrated a gradual reduction in the expression levels of CD80, CD83, CD86, and HLA-DR compared with the LPS control mDCs (Fig. 2a, b). The results indicated that ZSTK474 inhibited the LPS-induced DC maturation. We also demonstrated that the inhibitory effects are not caused by the toxicity of ZSTK474 (Fig. 2c). There were no significant changes in the percentages of apoptosis and dead cells by treated with ZSTK474.
ZSTK474 suppresses maturation of iDCs and mDC-induced allogeneic T cell proliferation. a Histograms of the cell surface marker staining from one of three independent experiments. The numbers indicate the MFI of the stained cells. b Relative levels of the markers compared to the ZSTK474 untreated controls (100 %) from three independent experiments with means ± s.d. *p < 0.05, **p < 0.01 determined by Student’s t test. The MFI level in each ZSTK474 treatment was compared to that of the controls, generating the percentage value relative to the controls. c The percentage of apoptosis and dead mDC treated by ZSTL474. d CFSE-labeled CD4+ T cell to respond in vitro to DC pulsed with different concentrations of ZSTK474, data shown being after 3 days of culture. The flow cytometry analysis was performed to detect the allogeneic T cell proliferation. The y-axis represents the proliferation index (PI). PI was calculated by ModFit software, which was the sum of the cells in all generations divided by the calculated number of original parent cells. The data are representative of three independent experiments using different blood donors. The values represent the means ± s.d. NS > 0.05, *p < 0.05, **p < 0.01 determined by Student’s t test
To investigate whether ZSTK474 impaired the mDC-mediated allogeneic T cell activation and proliferation, the allogeneic T cell proliferation stimulated by mDCs treated with or without ZSTK474 was assessed using MLR. As shown in Fig. 2d, the mDCs without the ZSTK474 treatment demonstrated the highest allogeneic T cell proliferation activity, which was represented by proliferation index (PI). However, the mDCs treated with ZSTK474 demonstrated significantly lower dose-dependent levels of allogeneic T cell proliferation. And the significance marks denote mDCs with ZSTKL474 treatment showed significant lower levels of allogeneic T cell proliferation in a concentration-dependent manner (p < 0.01, DC:T cell = 1:10; p < 0.05, DC:T cell = 1:20). These suggest that ZSTK474 could impair one of the most important biologic functions of mDCs and consequently suppress immune responses.
ZSTK474 blocks the DC-derived Th1- and Th17-polarizing cytokines in concentration-dependent
DC-derived cytokines are required for polarization of the adaptive immune response. Therefore, we investigated the potential role of ZSTK474 in the expression of T helper cell-polarizing cytokines. The DCs were pretreated with different ZSTK474 (0.04 and 0.2 μM) for 1 h, were stimulated with LPS, and the steady-state levels of the cytokine mRNAs were analyzed using quantitative PCR. As shown in Fig. 3a, the ZSTK474 substantially inhibited the production of the inflammatory cytokine tumor necrosis factor-α (TNF-α), Th1 cytokine interferon-γ (IFN-γ), Th1 cell-polarizing cytokine IL-12p35, Th17 cell-polarizing cytokine IL-6, and IL-12/23p40 at the peak of expression (4 h after LPS stimulation). However, IL-23p19 did not change significantly. We deduced that ZSTK474 may have not influenced this subunit and just influenced the IL12/23p40 to change IL-23 expression. Furthermore, we analyzed the IFN-γ, TNF-α, and IL-6 proteins in the culture supernatants by cytometric bead array (cat.560484, BD Biosciences, California, USA). The result is consistent with the observation of mRNA (Fig. 3b). The data suggest that ZSTK474 suppressed the DC-mediated Th1 and Th17 cell polarization and may be useful for the treatment of Th1 cell- and Th17 cell-mediated autoimmune inflammatory diseases.
ZSTK474 blocks expression of Th1- and Th17-polarizing cytokines by DCs. The iDCs on day 5 of culture were pretreated for 1 h with 0.04 and 0.2 μM ZSTK474 and were stimulated with 1 μg/mL LPS. a The DCs were collected at 4 h after LPS stimulation and were quantified using quantitative PCR. The gene expression was normalized based on the GAPDH content. b The cell supernatant were quantified using CBA kit to detect the protein level. The values represent the means ± s.d. NS > 0.05, *p < 0.05, **p < 0.01 determined by Student’s t test
Overall, the in vitro studies demonstrated that ZSTK474 significantly inhibited the human CD14+ monocyte-derived DC differentiation and maturation, the antigen uptake ability of the iDCs, and the antigen-presenting ability of the mDCs. Specifically, ZSTK474 suppressed the expression of costimulatory molecules, inflammatory cytokines, and Th1- and Th17-polarizingg cytokines in the DCs. The results suggested that ZSTK474 exhibits anti-inflammatory and immunosuppressive properties.
ZSTK474 ameliorates the clinical severity of EAE in mice
To investigate the functional anti-inflammatory and immunosuppressive roles of ZSTK474 in vivo, the Th1 and Th17 cell-mediated autoimmune inflammatory disease EAE was induced in the C57BL/6 mice using the MOG35–55 peptide. The ZSTK474 was administered intragastrically daily, and the mice were sacrificed on day 26 postimmunization. Compared with the PBS-treated mice, the onset of clinical symptoms in the ZSTK474-treated mice was delayed by approximately 6 days (Fig. 4a, b). The disease severity, assessed by the maximal (2.67 ± 0.61 vs. 1.67 ± 0.52, p < 0.05) and cumulative clinical scores (35.59 ± 11.7 vs. 9.3 ± 2.81, p < 0.01), was significantly lower in the ZSTK474-treated mice (Fig. 4c, d). The data suggested that ZSTK474 significantly ameliorates the clinical outcome of EAE.
ZSTK474 ameliorates the clinical severity of EAE in mice. EAE was induced in female C57BL/6 mice using MOG35–55, and the treatment with ZSTK474 was performed as described in the “Materials and methods” section, n = 12 mice per group. a, b The mean clinical score is the mean of the daily clinical scores observed from days 1 to 26 post-immunization by 25 mg and 50 mg ZSTK474 treatment. c The mean cumulative score is the mean of the sum of the daily clinical scores observed between days 1 and 26. d The mean maximum clinical score was calculated from the maximum clinical score of individual animals between days 1 and 26. The values represent the mean ± SD. *p < 0.05 and **p < 0.01 (Mann-Whitney U test, nonparametric data). The data are representative of three experiments exhibiting similar results
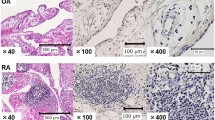
ZSTK474 limits the CNS inflammation and demyelination
To characterize the disease progression at the level of the CNS injury, we performed a histological analysis of the lumbar spinal cords on day 15 postimmunization. At the peak of the acute phase of the disease, the H&E staining demonstrated that the lumbar spinal cords from the ZSTK474-treated mice exhibited smaller numbers of inflammatory cells in the white matter (Fig. 5a). The sections stained with Luxol fast blue revealed that the PBS-treated mice exhibited large areas of demyelination; however, the demyelination was markedly attenuated in the ZSTK474-treated mice (Fig. 5b). In summary, ZSTK474 inhibited the CNS inflammation and demyelination in EAE, suggesting that ZSTK474 improved the pathological events of the EAE.
Histopathological analysis of spinal cord sections from representative PBS and ZSTK474-treated EAE mice. Serial sections of spinal cord were obtained on day 17 after immunization. a Hematoxylin and eosin (H&E)-stained section shows the infiltration of inflammatory cells in the white matter. The arrows indicate the inflammatory cells. b Luxol fast blue staining shows the areas of intact myelin (blue) and demyelination (pink). The arrows indicate the demyelination in the spinal cord, which includes sites associated with the infiltration of inflammatory cells. The arrows indicate positive immunostaining. c, d Quantification of spinal cord infiltrates in the a and b. Three animals from each group were sacrificed, and 10 sections of the spinal cord of each animal were analyzed. **p < 0.01 determined by Student’s t test
ZSTK474 suppresses T helper cell differentiation in vivo
Because the inflammatory Th1 and Th17 cells mediated the autoimmune CNS inflammation and demyelination, we investigated further the impact of ZSTK474 on the development of pathogenic Th1 and Th17 cell subsets in vivo. In the ex vivo experiments, we examined the Th1 and Th17 cell subsets in the splenocytes and CNS through the intracellular staining of the IFN-γ and IL-17 cytokines. The data demonstrate that the percentage of IFN-γ- and IL-17-producing CD4+ lymphocyte cells was lower in the ZSTK474-treated mice compared with the PBS-treated mice. The results demonstrated that the ZSTK474 suppression of EAE was concomitant with the decrease in the IFN-γ-producing Th1 cells and the IL-17-producing Th17 cells. Data are presented as a representative plot (Fig. 6a, b) and summary graph (Fig. 6c, d).
ZSTK474 restricts MOG-specific T cell responses ex vivo. a, c. Flow cytometry analysis of activation markers (IFN-γ and IL-17) on gated CD4+ cell isolated from the spleens and CNS of control and ZSTK474-treated EAE mice (n = 3 mice per group), assessed on the indicated 15 days after the induction of EAE. Data are presented as a representative plot (a, b) and summary graph (c, d). For the flow cytometry Th1 and Th17 profile analyses, the cells were stimulated for 5 h with phorbol-12-myristate-13-acetate/ionomycin (PMA/I) and brefeldin (BFA), then were stained for CD4, IFN-γ, and IL-17. Data are from three independent experiments (mean and s.d., c, d). **p < 0.01 determined by Student’s t test
ZSTK474 suppresses DCs in vivo in EAE mice
We addressed, in addition to the characteristic effects of ZSTK474 on T cells, whether the regulatory properties of ZSTK474 on the MOG-reactive T cell responses were attributable at least in part to the ability of the protein to alter the function of DCs. The splenocytes were obtained from the ZSTK474-treated or control EAE mice and were analyzed ex vivo for the expression of CD83, CD86, and MHC-II. As shown in Fig. 7, the surface expression of CD80, CD86, and MHC-II was decreased significantly in the CD11c+ cell populations from the ZSTK474-treated EAE mice compared with the control mice. Data are presented as a representative line (A) and summary graph (B) and absolute number of CD11c+ cell (C). The data indicated that the ZSTK474 not only suppressed the DC maturation, but also decreased the absolute number of DCs in the EAE mice in vivo.
ZSTK474 suppresses CD11c+ APCs in vivo in EAE mice. a The splenocytes from ZSTK474-treated or control mice (n = 3 mice per group) were stained for CD83, CD86, and MHC-II (solid line) or isotype control (dashed line) after MOG stimulation and were examined by flow cytometry in the gate of CD11c+ cell population. Relative levels of the surface markers (b) and the absolute number of CD11C+ (c) compared with the control and ZSTK474 treated from three independent experiments with means ± s.d.; *p < 0.05 determined by Student’s t test
Inhibition of PI3K downstream signaling in mDCs by ZSTK474
The effect of various concentrations of ZSTK474 on the inhibition of Akt phosphorylation, a major target of PI3K, and the inhibition of other downstream signaling components was examined in the mDCs using immunoblotting. The DCs treatment with 0.04, 0.2 μM of ZSTK474 significantly decreased the level of phosphorylated Akt (Ser-473) and slightly reduced phosphorylated GSK-3β (Ser-9) within 30 min with 1 μg/ml LPS. However, the nonphosphorylated Akt and GSK-3β were not changed (Fig. 8).
Discussion
Although molecular mechanisms have been described for the antitumor activities of ZSTK474, its potential effect on inflammatory and immune-mediated diseases such as MS and EAE remain unclear. In this study, we demonstrated that ZSTK474 exhibits anti-inflammatory properties and therapeutic potential for autoimmune inflammatory. Our results demonstrate that ZSTK474 can suppress human CD14+ monocyte-derived DC differentiation and activation by decreasing the expression levels of several key DC surface markers, thereby inhibiting endocytosis in the cells and inhibiting the activation of mDCs and allogeneic T cell proliferation. Based on these studies, we further investigated the effect of ZSTK474 in vivo. Our results demonstrate ZSTK474 can decrease the absolute number of DC, delay and ameliorate EAE onset. These suggest that ZSTK474 could provide a therapeutic intervention for immune inflammatory diseases through DC.
The IC50 values of ZSTK474 for inhibits PI3K α, β, δ, and γ were determined as 7, 72, 6, and 38 nM, respectively [10]. In our study, the highest dose of ZSTK474 we used for treated DC were 0.2 μM, it is higher enough to inhibit the all four subtype of PI3K. At 10 μM, a higher concentration than its GI50, ZSTK474 did not induce apoptosis in A549 cells. Therefore, it appears that induction of apoptosis by ZSTK474 is weak [7]. In our experiments, we use lower concentration of ZSTK474 and observed no significant toxicity to DCs.
DC and T cell interactions play important roles in the balance between the immune response and tolerance. The maturation status of the DCs determines whether they prime or tolerate T cells. The early antigen-dependent T cell arrest in DCs appears to be a shared feature of tolerance and priming associated with activation and proliferation [23]. Upon antigen exposure, the migration of antigen-carrying DCs to the secondary lymphoid organs is a prerequisite for the activation of naïve T cells. Thus, the DC migration represents a critical step in the triggering of an optimal immune response. Previous studies have demonstrated that PI3Kγ plays a nonredundant role in DC trafficking and T-cell activation [24]. DCs from PI3Kγ−/− mice exhibit a reduced ability to respond to chemokines in vitro and ex vivo and to travel to the draining lymph node under inflammatory conditions [24]. Sarah Haylock-Jacobs demonstrated that T cell activation and function during EAE was markedly reduced, and fewer T cells were observed in the CNS in p110δ-inactivated mice [25]. Furthermore, they found that PI3Kδ activity is required for efficient Th17 differentiation and function both in vitro and in vivo and protects CD4+ T cells from undergoing apoptosis during an autoimmune response [25]. PI3Kγ deficiency delays the onset of experimental autoimmune encephalomyelitis and ameliorates the clinical outcome [26]. Thus, the inhibitory effects of ZSTK474 on DC absolute number and maturation demonstrated in our study may play an important role in the inhibition of T-cell priming. This functional deficiency is likely to contribute to the delayed onset of EAE following ZSTK474 treatment in mice. Collectively, our findings and the findings reported by Del Prete [24] and Luciana Berod [26] strongly suggest that the lack of PI3K delays T-cell priming, thus prolonging the induction phase and consequently, the clinical onset of the disease. We also found that ZSTK474-induced inhibition of the differentiation of Th1 and Th17 cells was associated with a downregulation of the production of Th1- and Th17-polarizing cytokines such as IL-12, IFN-γ, IL-6, and IL-23 in DCs. PI3Kδ has been implicated in the development of Th1 and Th2 cells in vitro [27, 28].
Our results indicated that ZSTK474 might prevent development of EAE through p-Akt and p-GSK-3β signaling collectively. We also found that the p-GSK3β level was reduced in DCs. Our conclusion was further supported by the finding that the level of p-GSK3β was highly upregulated during Th17 polarization, which is particularly notable considering that p-GSK3β levels are generally very stable in numerous cell types and conditions [29].
The role of T cells in the pathogenesis of EAE and MS makes them an attractive target for therapeutic intervention. IFN-γ and glatiramer acetate, which are two most commonly drugs to treat MS, can increase Treg cells and IL-10 and thereby suppress proinflammatory T cell cytokines, although they probably also act on other cell types. Another drug, natalizumab, have higher efficacy than the IFN-β and glatiramer acetate. However, the pivotal trials were not examined in second-line therapy, and some questions are yet unanswered [30]. Other therapies in clinical trials include fingolimod and alemtuzumab. Fingolimod prevents lymphocyte recruitment from lymph nodes to sites of inflammation. Alemtuzumab kills T cells and other target cells [31]. Although these drugs have demonstrated suppression of inflammatory disease in clinical trials, many second-line therapies for MS are accompanied by the risk of life-threatening complications [32]. Efforts are now focused upon targeting Th17 cells and associated cytokines, including anti-IL-17 antibodies and antibodies or antagonists to cytokines that drive Th17 cells, such as IL-6 and IL-23 [33]. Thus, while the IL-17/IL-23 axis is clearly an important drug target for the treatment of MS, its potential as a front-line therapy awaits further clinical evaluation [34]. Maybe ZSTK474 is a potential therapeutic drug for multiple sclerosis and other autoimmune inflammatory diseases through anti-IL-17/IL-23.
In summary, we demonstrated that ZSTK474, a novel PI3K inhibitor, significantly decreased Akt and slightly reduced GSK-3β signaling phosphorylation in DCs. These conditions are critical for maintaining DCs in their tolerogenic state via a reduction in the expression of proinflammatory factors such as IFN-γ, IL-12, IL-6, and IL-23. ZSTK474 treatment of DCs inhibited their production of Th1- and Th17-polarizing cytokines and maybe indirectly influencing Th cell differentiation. In vivo, ZSTK474 treatment decreased the absolute number of DC, inhibited DC mature and Th cell differentiation, which further led to a reduction in the EAE clinical score and in CNS inflammation and demyelination. Therefore, these data suggest that ZSTK474 inhibition can be exploited as a therapeutic strategy to control pathological conditions, such as autoimmune diseases.
Abbreviations
- PI3K:
-
Phosphatidylinositol 3-kinase
- DC:
-
Dendritic cell
- CNS:
-
Central nervous system
- EAE:
-
Experimental autoimmune encephalomyelitis
- MS:
-
Multiple sclerosis
- GSK3β:
-
Glycogen synthase kinase 3 beta
- mTOR:
-
Mammalian target of rapamycin
- APC:
-
Antigen-presenting cell
- TLR:
-
Toll-like receptor
- PKB:
-
Protein kinase B
- LPS:
-
Lipopolysaccharide
- GM-CSF:
-
Granulocyte macrophage-colony stimulating factor
- MFI:
-
Mean fluorescence intensity
References
Ruckle T, Schwarz M, Rommel C (2006) PI3Kgamma inhibition: towards an ‘aspirin of the 21st century’? Nat Rev Drug Discov 5:903–918
Fruman DA, Cantley LC (2002) Phosphoinositide 3-kinase in immunological systems. Semin Immunol 14:7–18
Rommel C, Camps M, Ji H (2007) PI3K delta and PI3K gamma: partners in crime in inflammation in rheumatoid arthritis and beyond? Nat Rev Immunol 7:191–201
Kong D, Dan S, Yamazaki K, Yamori T (2010) Inhibition profiles of phosphatidylinositol 3-kinase inhibitors against PI3K superfamily and human cancer cell line panel JFCR39. Eur J Cancer 46:1111–1121
Hu L, Zaloudek C, Mills G, Gray J, Jaffe R (2000) In vivo and in vitro ovarian carcinoma growth inhibition by a phosphatidylinositol 3-kinase inhibitor (LY294002). Clin Cancer Res 6:880–886
Ihle N, Williams R, Chow S, Chew W, Berggren M, Paine-Murrieta G, Minion D, Halter R, Wipf P, Abraham R et al (2004) Molecular pharmacology and antitumor activity of PX-866, a novel inhibitor of phosphoinositide-3-kinase signaling. Mol Cancer Ther 3:763–772
Yaguchi S, Fukui Y, Koshimizu I, Yoshimi H, Matsuno T, Gouda H, Hirono S, Yamazaki K, Yamori T (2006) Antitumor activity of ZSTK474: a new phosphatidylinositol 3-kinase inhibitor. J Natl Cancer Inst 98:545–556
Kong D, Yamori T (2007) ZSTK474 is an ATP-competitive inhibitor of class I phosphatidylinositol 3 kinase isoforms. Cancer Sci 98:1638–1642
Kong D, Yamori T (2008) Phosphatidylinositol 3-kinase inhibitors: promising drug candidates for cancer therapy. Cancer Sci 99:1734–1740
Kong D, Yaguchi S, Yamori T (2009) Effect of ZSTK474: a novel phosphatidylinositol 3-kinase inhibitor on DNA-dependent protein kinase. Biol Pharm Bull 32:297–300
Kong D, Yamori T (2009) Advances in development of phosphatidylinositol 3-kinase inhibitors. Curr Med Chem 16:2839–2854
Toyama S, Tamura N, Haruta K, Karakida T, Mori S, Watanabe T, Yamori T, Takasaki Y (2010) Inhibitory effects of ZSTK474: a novel phosphoinositide 3-kinase inhibitor, on osteoclasts and collagen-induced arthritis in mice. Arthritis Res Ther 12:R92
Krishnamoorthy G, Wekerle HEAE (2009) An immunologist’s magic eye. Eur J Immunol 39:2031–2035
Loma I, Heyman R (2011) Multiple sclerosis: pathogenesis and treatment. Curr Neuropharmacol 9(3):409–416
Hazeki K, Nigorikawa K, Hazeki O (2007) Role of phosphoinositide 3-kinase in innate immunity. Biol Pharm Bull 30:1617–1623
Yu Y, Nagai S, Wu H, Neish AS, Koyasu S, Gewirtz AT (2006) TLR5-mediated phosphoinositide 3-kinase activation negatively regulates flagellininduced proinflammatory gene expression. J Immunol 176:6194–6201
Hori S, Takahashi T, Sakaguchi S (2003) Control of autoimmunity by naturally arising regulatory CD4+ T cells. Adv Immunol 81:331–371
Sakaguchi S (2004) Naturally arising CD4+ regulatory T cells for immunologic self-tolerance and negative control of immune responses. Annu Rev Immunol 22:531–562
Dittel BN (2008) CD4 T cells: balancing the coming and going of autoimmune-mediated inflammation in the CNS. Brain Behav Immun 22(4):421–430
Stromnes IM, Goverman JM (2006) Active induction of experimental allergic encephalomyelitis. Nat Protoc 1(4):1810–1819
Ge Z, Da Y, Xue Z, Zhang K, Zhuang H, Peng M, Li Y, Li W, Simard A, Hao J et al (2013) Vorinostat, a histone deacetylase inhibitor, suppresses dendritic cell function and ameliorates experimental autoimmune encephalomyelitis. Exp Neurol 241:56–66
Xue Z, Ge Z, Zhang K, Sun R, Yang J, Han R, Peng M, Li Y, Li W, Zhang D et al (2014) Embelin suppresses dendritic cell functions and limits autoimmune encephalomyelitis through the TGF-β/β-catenin and STAT3 signaling pathways. Mol Neurobiol 49(2):1087–1101
Shakhar G, Lindquist RL, Skokos D, Dudziak D, Huang JH, Nussenzweig MC, Dustin ML (2005) Stable T cell-dendritic cell interactions precede the development of both tolerance and immunity in vivo. Nat Immunol 6:707–714
Del Prete A, Vermi W, Dander E, Otero K, Barberis L, Luini W, Bernasconi S, Sironi M, Santoro A, Garlanda C et al (2004) Defective dendritic cell migration and activation of adaptive immunity in PI3Kgamma-deficient mice. EMBO J 23:3505–3515
Haylock-Jacobs S, Comerford I, Bunting M, Kara E, Townley S, Klingler-Hoffmann M, Vanhaesebroeck B, Puri KD, McColl SR (2011) PI3Kδ drives the pathogenesis of experimental autoimmune encephalomyelitis by inhibiting effector T cellapoptosis and promoting Th17 differentiation. J Autoimmun 36(3–4):278–287
Berod L, Heinemann C, Heink S, Escher A, Stadelmann C, Drube S, Wetzker R, Norgauer J, Kamradt T (2011) PI3Kgamma deficiency delays the onset of experimental autoimmune encephalomyelitis and ameliorates its clinical outcome. Eur J Immunol 41(3):833–844
Okkenhaug K, Bilancio A, Farjot G, Priddle H, Sancho S, Peskett E, Pearce W, Meek SE, Salpekar A, Waterfield MD et al (2002) Impaired B and T cell antigen receptor signaling in p110δ PI 3-kinase mutant mice. Science 297:1031–1034
Okkenhaug K, Patton DT, Bilancio A, Garçon F, Rowan WC, Vanhaesebroeck B (2006) The p110δ isoform of PI3K controls clonal expansion and differentiation of T helper cells. J Immunol 177(8):5122–5128
Oppmann B, Lesley R, Blom B, Timans JC, Xu Y, Hunte B, Vega F, Yu N, Wang J, Singh K et al (2000) Novel p19 protein engages IL-12p40 to form a cytokine IL-23 with biological activities similar as well as distinct from IL-12. Immunity 13:715–725
Yaldizli O, Putzki N (2009) Natalizumab in the treatment of multiple sclerosis. Ther Adv Neurol Disord 2(2):115–128
Cox AL, Thompson SA, Jones JL, Robertson VH, Hale G, Waldmann H, Compston DA, Coles AJ et al (2005) Lymphocyte homeostasis following therapeutic lymphocyte depletion in multiple sclerosis. Eur J Immunol 35:3332–3342
Stromnes IM, Goverman JM (2006) Passive induction of experimental allergic encephalomyelitis. Nat Protoc 1:1952–1960
Fletcher JM, Lalor SJ, Sweeney CM, Tubridy N, Mills KH et al (2010) T cells in multiple sclerosis and experimental autoimmune encephalomyelitis. Clin Exp Immunol 162(1):1–11
Mills KH (2008) Induction, function and regulation of IL-17-producing T cells. Eur J Immunol 38:2636–2649
Acknowledgments
We thank the Tianjin Blood Center for providing us with the buffy coat. We also thank the Experimental Animal Center of Tianjin Medical University (Tianjin, China) for their work in animal husbandry. This work is supported by the Ministry of Science and Technology of China through grant nos. 2012CB932503 and 2011CB933100; the National Natural Science Foundation of China through grant nos. 91029705, 81272317, and 81172864; and the Natural Science Foundation of Tianjin through grant no. 12JCZDJC23500.
Disclosure
The authors have nothing to disclose.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Zhenyi Xue, Wen Li, and Huafeng Wang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Xue, Z., Li, W., Wang, H. et al. ZSTK474, a novel PI3K inhibitor, modulates human CD14+ monocyte-derived dendritic cell functions and suppresses experimental autoimmune encephalomyelitis. J Mol Med 92, 1057–1068 (2014). https://doi.org/10.1007/s00109-014-1158-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-014-1158-x