Abstract
Platelets have been regarded as static cells that do not move once they adhere to a matrix. The present study explored, whether platelets are able to migrate. In contrast to the current opinion, we found that platelets were mobile, able to migrate over a surface, and transmigrate through a transwell membrane and endothelium toward a source of stromal cell-derived factor 1 (SDF-1). Platelet migration was stimulated by SDF-1, which led to the downstream activation and phosphorylation of Wiskott–Aldrich syndrome protein. SDF-1 signaling and subsequent platelet migration could be inhibited by CXCR4-receptor blocker AMD3100, pertussis toxin, inhibition of phosphoinositol 3-kinase (PI3 kinase) with LY294002 or wortmannin, and disruption of actin polymerization with cytochalasin B. The potential of platelets to migrate in an SDF-1-mediated fashion may redefine the role of platelets in the pathophysiology of vascular inflammation, subsequent atherosclerotic degeneration, and vascular regeneration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Once in contact with the endothelium, platelets are activated, start to roll, adhere loosely, and then adhere firmly. Immediately after firm adherence, platelets start to spread and offer binding sites to other platelets and circulating cells in the blood stream. According to the traditional view, the function of platelets is confined to their role in hemostasis, i.e., providing the ground for thrombotic and hemostatic processes; however, once activated or adherent, platelets stay alive and functionally active for hours and even days [1].
Moreover, activated platelets have recently been discovered to actively regulate cytoskeletal rearrangement and to upregulate the synthesis of proteins and peptides, such as the cytokine interleukin (IL)-1β [2–4]. Some of these synthesized proteins are also important for specific platelet functions like adhesion, cytoskeletal rearrangement, organization of focal adhesion points and cell spreading, all of which are known to be involved in the migration of other cell types [5–8]. During evolution, platelets may have conserved their capability to migrate from their progenitor cell, the ancient amebocyte. The amebocyte was the universal blood cell that embodied multiple functions like host defense, tissue repair, and hemostasis [9]. So far, little is known about platelet mobility, and few chemotactic stimuli from infectious or allergic inflammation have been identified. Platelet migration was described as a pharmacological readout for toxicity of pharmaceutical components and in canine ehrlichiosis [10, 11]. Other previous reports demonstrated platelet extravasation into inflamed tissue and chemotaxis towards N-formyl-methionyl-leucyl-phenylalanine (fMLP) [12, 13]. Recently, Pitchford et al. showed the effect of IgE-mediated platelet extravasation in lung tissue [14].
However, the signaling mechanisms of platelet migration and the role of stromal cell-derived factor 1 (SDF-1), a potent chemokine in inflammation which is highly expressed in the atherosclerotic plaque [15], have not been investigated in platelets. SDF-1, which is also stored in platelet granules, is known to induce chemotactic migration in a variety of cells [16–19], and platelets also express the corresponding CXCR4-receptor [20]. SDF-1 is also involved in the interaction between platelets and stem cells [21].
In this study we identify SDF-1 as a novel, potent mediator of platelet migration and transmigration and show that SDF-1-mediated platelet migration is PI3 kinase dependent.
Material and methods
Platelet isolation
Washed platelets were isolated from acid-citrate-dextrose-anticoagulated human blood of healthy volunteers as described previously [3, 4]. Volunteers on medications were excluded as platelet donors. Analysis of platelet purity by a whole blood analyzer (Sysmex) and flow cytometry for CD11b as a neutrophil marker showed no detection of cells other than platelets. Prior to the platelet experiments, one sample of every isolated cell population was measured by flow cytometry for the platelet-specific markers CD42b and P-selectin to rule out pre-activation. Platelets were stored in Iscove’s modified Dulbecco’s medium (IMDM) or phosphate-buffered saline until further use within 30 min.
Platelet chemotaxis toward a source of SDF-1 analyzed by light transmission microscopy
The migration model consisted of a fibrinogen-coated chamber slide (Nunc) with a pellet of low-melting agarose (1%, 250 μl) in the center of each well. This pellet of agarose contained a total of 300 ng recombinant SDF-1 (R&D Systems) at the source, generating a maximal concentration of 300 ng/ml with complete release. We ensured sustained SDF-1 release from the gel pellet by the gradual release of a fluorescent dye of equal molecular weight. Platelets were added at 5 × 107 platelets/ml (750 μl) of IMDM medium. After 30 min of adhesion, the plates were washed to remove non-adherent platelets. Platelet migration was then recorded using an Axiovert 200 polarization microscope (Carl Zeiss Inc., ×20 magnification) at 30 frames/hour and replayed at ten frames/second. For the negative control, the platelets were exposed to a gel matrix without chemokine and recorded accordingly. In an identical parallel experiment, platelets were recorded at a greater magnification in a chamber slide using a Cell Observer microscope (Carl Zeiss Inc., ×60 magnification) with six frames/minute and replayed with 20 frames/second. To identify surface receptors involved in platelet migration, platelets were allowed to adhere to a fibrinogen and collagen surface and exposed to a SDF-1 gradient. GPIIb/IIIa receptor was blocked with Abciximab (100 μg/ml; Eli Lilly and Company), glycoprotein VI (GPVI) (100 μg/ml, generously provided by Dr. E. Kremmer, Helmholtz-Zentrum, München, Germany). In a subset of experiments, the platelets were fixed afterwards and stained for immunofluorescent markers. All movies are representative for at least three independent experiments.
Transwell experiments for platelet transmigration
For transmigration experiments, we used transwell inserts (24-well, Falcon) separating the upper and the lower chamber with a membrane with pores that were 0.4 μm in diameter. The lower chamber contained SDF-1 (100 ng/ml, R&D Systems), IL-1ß (0.02 ng/ml, PeproTech Inc.), tumor necrosis factor (TNF)-α (50 ng/ml, PeproTech Inc.) or epithelial cell-derived neutrophil-activating peptide 78 (ENA-78) (150 ng/ml; R&D Systems). Platelets (2 × 106 platelets/ml, 250 μl) were carefully transferred into the upper chamber and were allowed to migrate through the membrane for 8 h. Migration experiments were performed under cell culture conditions in a stable humidified atmosphere (5% CO2, pH 7.4, 37°C). Afterwards, the platelet suspension in the lower compartment was stained with an antibody against glycoprotein Ib (CD42b, platelet specific; Beckman Coulter). Platelets were counted by flow cytometry (BD FACSCalibur) in the platelet gate. Flow cytometric readout was confirmed by the visual counting of platelets with a hemocytometer.
Images of the boyden chamber membranes were taken on a Zeiss LSM 5 EXCITER confocal laser scanning microscope (Carl Zeiss Micro Imaging GmbH, Germany) with an A-plan 40×/0.65 PH2 ocular.
Where indicated, inhibitors were added to the upper compartment, including AMD3100 (5 μg/ml, Sigma-Aldrich), cytochalasin B (2 μg/ml, Sigma-Aldrich), LY294002 (8 μg/ml, Calbiochem), wortmannin (2 μM, Calbiochem) as well as water-soluble and membrane-permeable pertussis toxin (240 ng/ml, Sigma-Aldrich). AMD3100 was used to specifically block the CXCR4-receptor. Actin polymerization was inhibited with cytochalasin B. LY294002 and wortmannin were used for inhibition of PI3 Kinase. All experiments containing dimethyl sulfoxide (DMSO) (AppliChem) or other solvents were compared to a DMSO/solvent control. The viability of inhibitor-treated platelets was assured by trypan blue exclusion and confirmed by MTT assay (data not shown).
In some transwell experiments, cultured arterial endothelial cells (105 endothelial cells per transwell insert) were grown on the transwell membrane to confluence. The endothelial cells were activated with IL-1β (100 pg/ml, PeproTech Inc.) for 4 h and washed three times with phosphate-buffered saline. For comparison and validation of the transmigration assay, equal concentrations of SDF-1 were used for transmigration assays with lymphocytes and neutrophils. Pore sizes of 3 μm for lymphocytes and 5 μm for neutrophils were used.
Confocal microscopy
Washed platelets were allowed to adhere to a fibrinogen surface (20 μg/ml) on a cover glass or a chamber slide for 20 min and were then fixed with paraformaldehyde (2%) and permeabilized with TX-100. The adherent platelets were washed and blocked with 2% bovine serum albumin for 30 min followed by incubation with the primary antibody for 2 h at room temperature. Primary antibodies against P-selectin (CD62P, Santa Cruz), glycoprotein Ib (CD42b, Santa Cruz), vinculin (Calbiochem), and phospho-Wiskott–Aldrich syndrome protein (WASP)-antibody (pSer483/484, Calbiochem) were used in 1:50 dilution. Chamber slides were then washed and incubated with Cy2 or Cy5-linked secondary antibodies (Dianova). In selected experiments, the actin cytoskeleton was stained with rhodamine phalloidin (Invitrogen). Confocal microscopy was performed using a Zeiss LSM 5 EXCITER confocal laser scanning microscope (Carl Zeiss Micro Imaging) with an A-plan 40×/0.65 PH2 ocular.
Western blot
Freshly isolated human platelets were centrifuged for 5 min at 240 g and the pellet was resuspended in lysis buffer (50 mM Tris–HCl, pH 7.4, 150 mM NaCl, 1% Trion-X, 0.5% Na2HPO4, 0.4% β-mercaptoethanol) containing protease inhibitor cocktail (Sigma-Aldrich). The protein concentration was measured with Bradford (Bio-Rad). Western blot analysis was carried out according to manufacturer’s protocol (ECL detection, Amersham), primary antibody: anti-WASP-phospho, AB1966; Chemicon; secondary anti-rabbit HRP-antibody: cell signaling.
The statistical analysis of western blots for phospho-WASP was performed by densitometric measurements, and the results were shown as logarithmic data of opacity.
Intravital fluorescence microscopy
C57Bl/6J mice were anesthetized by intraperitoneal injection of midazolam (5 mg/kg body weight; Ratiopharm), medetomidine (0.5 mg/kg body weight; Pfizer), and fentanyl (0.05 mg/kg body weight; CuraMed Pharma GmbH) and were placed on a heating pad for maintenance of body temperature between 36°C and 37°C. Polyethylene catheters (Portex) were implanted into the left jugular vein for injection of the platelets. After transverse laparotomy, a segment of the jejunum was gently exteriorized. Segmental intestinal ischemia was induced by ligation of the supplying vessels and the segment itself for 1 h. Before ischemia and after reperfusion (5, 10, 30, 60, 90 min), the fluorescent platelets were visualized in situ by in vivo microscopy of four to five non-overlapping, randomly selected regions of interest with arterioles and venules using a Zeiss Axiotech microscope (water immersion objective, 20X, W 20X/0.5; Zeiss) with a 100-W HBO mercury bulb for epi-illumination. Although platelets accumulated outside the vessel lumen, intravital microscopy was not able to visualize platelet infiltrates within the vessel wall directly. Therefore, the mice were sacrificed, and slices of vessel walls were stained with an anti-green fluorescent protein (GFP) secondary antibody to stain for platelet infiltrates. The institutional review board for animal studies approved these experiments.
Statistical analysis
Data are given as mean ± SEM. Student’s t test for unpaired data or ANOVA was applied where appropriate, n denotes the number of independent experiments, a p value less than 0.05 was considered statistically significant.
Results
Chemotaxis and fast migration of platelets toward a source of SDF-1
Platelets were exposed to SDF-1 released from a gel matrix to test the chemotactic effect on platelets and a migratory platelet response. After 3 h of observation, we found an accumulation of platelets around the source of SDF-1 (Fig. 1a, f; ESM movie I), whereas only a few platelets gathered around the gel matrix without chemokine (Fig. 1e, ESM movie II). Throughout the observation, the platelets remained in the optical focus and stayed in contact with the surface. ESM movie III shows an example of a migrating platelet out of the cohort in a later stage of migration that migrates towards the source of SDF-1 (top of the picture, slow migration). We stained the accumulated cells after fixation (Fig. 1b, c; enlarged segment of Fig. 1a) to identify platelets with the platelet-specific marker P-selectin (green, Fig. 1c) and to assure contact of platelets to the surface by staining for focal adhesions (vinculin, blue) (Fig. 1d). Platelet chemotaxis and fast migration allows platelets to travel large distances (200 μm/3 h) toward a chemokine source by periodic focal attachment during which they gradually become more adherent (Fig. 1F1–F4) and continue to perform slow, directed migration towards the chemokine source.
Platelet chemotaxis and fast migration toward a source of SDF-1. a A platelet migration model was designed to generate a gradient of the cytokine SDF-1. The migration chamber consists of a fibrinogen-coated six-well plate with a pellet of low-melting agarose (1%, 250 μl) containing 300 ng total SDF-1 in the center of each well. Platelets (5 × 107/ml) were added to the migration model. Platelets initially migrate with 200 μm/3 hrs (fast migration) towards a SDF-1 source visible on the left side of the image (see also ESM movie I). b Magnified immunofluorescence staining of platelets that accumulated around the SDF-1 source for the platelet-specific marker P-selectin (green) and the focal adhesion marker vinculin (blue) shows focal platelet adhesion. Rhodamine phalloidin (red). c Further magnification shows that platelets are in contact with the fibrinogen matrix and have isolated focal adhesions as a sign of cell attachment to the matrix. d Staining for vinculin (blue) demonstrates just few focal adhesion points for loose, fast migrating platelets. Image shows the same platelets from a–d. e No platelet accumulation occurred around a control (without SDF-1) source visible on the left side of the image. (ESM movie II) (×20, magnification). The images and movies represent three independent experiments. f Gradual accumulation and adhesion of platelets at the SDF-1 source (F1–F4) after which they continue to perform slow directed migration
In the early stages of migration (fast migration) platelets only have few focal adhesion contacts and generate more adhesion contacts as migration speed slows down. Quantitative correlation revealed that fast migrating platelets on average had less focal adhesion contacts (1.4 ± 0.1) as compared to slow migrating platelets with more focal adhesion contacts (2.4 ± 0.1).
ESM movie IV shows an example of a migrating platelet that stays in constant contact with the surface and within the optical focus while migrating in a well-coordinated manner with rapid pseudopod extension. Figure 2c illustrates the focal adhesion contacts of platelets (vinculin, blue) which all stain positive for the platelet-specific marker P-selectin (green). Within the platelet population we identified three groups based upon their migratory activity that are shown in Fig. 2d. While adherent to a fibrinogen matrix, approximately 10% of the platelets showed distant migration beyond 5 μm, whereas the majority of platelets in the observed samples showed active movements without traveling beyond 5 μm. The remaining platelets (30%) immediately became fully adherent and did not leave the point of adhesion. Platelets were more mobile on fibrinogen than collagen. The cellular activity and ability of platelets to migrate was not significantly increased when the platelets were exposed to a SDF-gradient, but significantly, more platelets performed migration directed towards the SDF-1 source. Arrow trajectories in Fig. 2a visualize on a cellular level that more platelets direct their migration towards SDF-1, whereas platelets without a target chemokine source perform random, undirected migration. Calculation of the chemotactic index, defined as movement into the direction of SDF-1 divided by the total distance traveled, emphasized the increased directional migration of platelets towards SDF-1 (0.45 ± 0.07 versus 0.25 ± 0.05). Additional activation with thrombin did not enhance migration; in contrast, thrombin was able to abolish platelet migration partially (Supplemental Fig. 5) The GPIIb/IIIa receptor appears to be involved in platelet migration over coated fibrinogen since receptor blockage with Abciximab resulted in a decreased number of migrating cells (Fig. 2e). Inhibition of GPVI did not affect platelet mobility on collagen (Fig. 2e); however, in the transwell experiments, inhibition of GPIIbIIIa, GPVI, and GPIb did not affect platelet transmigration through the transwell membrane (n = 3, data not shown).
Migration of SDF-1-activated platelets on a fibrinogen and collagen matrix. a Illustration of directional platelet migration with and without an SDF-1 gradient. In the presence of an SDF-1 source, more platelets perform directed migration towards the target source compared to a control source. Arrows indicate the direction and distance of migration of the individual platelet. Horizontal bars represent absent or non-directed migration or mobility. Platelet migration velocity was 0.04–0.25 μm/min (slow migration). b Platelets exposed to an SDF-1 source show increased chemotactic activity towards SDF-1 compared to the control source. The chemotactic index defined the average SDF-1-directed distance of migration based on the total distance traveled expressed as a fraction of 1. c Immunofluorescence staining shows the different groups of platelets ranging from immobile, fully adherent platelets (*) with classical multifocal adhesions to mobile platelets with single focal adhesions at the site of surface contact (arrow). Platelets are stained with the platelet-specific marker P-selectin (green) and vinculin (blue) to show focal adhesions. Rhodamine phalloidin (actin, red). d Relative distribution of total migratory activity per 100 platelets on a fibrinogen (Fib) or collagen (Coll) matrix; platelets are subdivided into three groups: significant migration (more than 5 μm/2 h), intermediate migration (below 5 μm), or no migration. (arithmetic means ± SEM, n = 3). e Effect of GPIIbIIIa and GPVI receptor inhibition on platelet migration based on the amount of mobile platelet. Inhibition of GPIIbIIIa with abciximab on fibrinogen resulted in reduced migratory activity, whereas inhibition of GPVI receptor on collagen had no effect on platelet migration. Arithmetic means ± SEM (n = 3). * denotes significant difference to control (p ≤ 0.05)
SDF-1 leads to gradient-dependent transmigration of human platelets through porous membranes and activated endothelium
Different cytokines were tested for their chemotactic effect in a Boyden-like transwell chamber experiment (0.4 μm pore size). We found that if SDF-1 was added to the lower compartment; platelet transmigration was significantly enhanced compared to the control medium (Fig. 3a, Supplemental Fig. 1). The chemotactic effect of SDF-1 increased platelet transmigration from 0.7 ± 0.1% to 1.6 ± 0.3% of the total platelet number (Supplemental Fig. 3). SDF-1-mediated transmigration was a dose-dependent effect (Fig. 3a, insert). Other tested cytokines, including IL-1β, TNF-α, and ENA-78 did not affect platelet transmigration (Fig. 3a). The chemotactic effect of SDF-1 appears to affect the directional orientation of platelets and is apparently not a matter of increased platelet activation. Although activation of platelets with thrombin results in a slightly increased transmigration on its own, it does not explain the marked increase in transmigration with SDF-1 (Supplemental Fig. 5).
Platelet transmigration assay. a Effect of different chemokines/cytokines on platelet migration in a transwell experiment. SDF-1 induced a significant increase in platelet transmigration toward an SDF-1 gradient. Undirected baseline migration was set as 100% and relative transmigration was compared accordingly. Classical leukocyte-derived cytokines like IL-1β, TNF-α, and ENA-78 did not significantly affect platelet migration compared to baseline migration. Cytochalasin B was used to block actin polymerization and inhibited platelet migration. Insert, dose dependency of SDF-1-mediated platelet migration. Arithmetic means ± SEM (n = 4), * denotes significant difference to control (p ≤ 0.05). b Platelets show a significant increase in transmigration toward an SDF-1 gradient also through an endothelial monolayer (quiescent endothelium). Transmigration is further enhanced when endothelial cells are additionally activated with IL-1β. Undirected baseline migration was set as 100% and relative transmigration was compared accordingly. Arithmetic means ± SEM (n = 3), * denotes significant difference to control (p ≤ 0.05)
Platelet migration was effectively inhibited by disruption of actin polymerization with cytochalasin B (2 μg/ml, Fig. 3a; ESM movie V). We then tested if platelets could also pass through endothelium. Endothelial cells were grown to confluency and platelets were added onto the endothelial monolayer with SDF-1 (100 ng/ml) or control medium in the lower compartment. Although platelet transmigration decreased about eightfold when the porous membrane was endothelialized, we still found a significant increase in platelet transmigration towards SDF-1 through the endothelium from 0.16 ± 0.01% to 0.23 ± 0.02% of total platelets (Fig. 3b, Supplemental Fig. 2). This effect was further increased to 0.30 ± 0.02% (Supplemental Fig. 2) if endothelial cells were activated with IL-1β (100 pg/ml).
SDF-1-dependent effects on platelet mobility are mediated by CXCR4-receptor, G-protein, and PI3 kinase
Figure 4a and b show the inhibitory effects of different inhibitory substances that target crucial regulatory proteins in the SDF-1 signaling cascade on SDF-1-mediated platelet transmigration. With AMD3100, a CXCR4-receptor-specific inhibitor, platelet transmigration toward SDF-1 could be effectively blocked. Transmigration through the transwell pores (0.4 μm) to the lower chamber could further be significantly reduced with pertussis toxin (PTX) which inhibits G-protein-dependent CXCR4-receptor signaling. It was also significantly reduced by PI3-kinase inhibitors like LY294002 and wortmannin (Fig. 4a, b; Supplemental Fig. 4). Platelet transmigration was further reduced when the SDF-1 gradient was neutralized with equal cytokine concentrations in both compartments of the transmigration chamber (Fig. 4a, b; SDF-1/SDF-1).
PI3 kinase dependence of SDF-1-induced platelet transmigration. Inhibition of SDF-1-induced platelet transmigration by blockers of the CXCR4-receptor (AMD3100, 5 μg/ml), G-protein (PTX, 240 ng/ml), and PI3 kinase (wortmannin, 2 μM; LY 294002, 8 μg/ml). Arithmetic means ± SEM (n = 4), * denotes significant difference to control (p ≤ 0.05). DMSO used to dilute inhibitors does not significantly affect migration. The SDF-1 gradient was abolished by adding SDF-1 in equal concentrations (100 ng/ml) in the lower as well as in the upper chamber (SDF-1/SDF-1). a Results of flow cytometric analysis of platelets (CD42b positive) that transmigrated through the transwell pores (0.4 μm) to the lower chamber. b Representative immunofluorescence stainings of migrated platelets after transmigration through porous membranes of a transwell chamber. Migrated platelets at the bottom of the removed transwell membranes were stained with rhodamine phalloidin (red) and the platelet-specific glycoprotein Ib (blue) and analyzed by confocal microscopy
SDF-1 increases platelet transmigration by a factor of 2.3
Platelets show a significant 2.3-fold increase in transmigration toward SDF-1 (Fig. 5). A comparison was made between SDF-1-induced platelet migration and the chemotactic effect of SDF-1 on classical chemotactic cells like lymphocytes (tenfold increase) or neutrophils which are known not to respond to SDF-1. As a result, following stimulation of chemotaxis with SDF-1 1.6% of total platelets, 9% of lymphocytes, and 0.2% of neutrophils (no increase over baseline) migrated into the lower compartment.
SDF-1-induced migration of platelets, lymphocytes, and polymorphonuclear neutrophils (PMNs). Comparison of the transmigration of platelets, lymphocytes, and PMNs toward SDF-1 (100 ng/ml). Transmigration was calculated against the individual control of each cell type and expressed as relative increase (x-fold). Lymphocytes and platelets show a significant increase in transmigration toward SDF-1 with relative increase of tenfold and 2.3-fold, respectively. Percentage of transmigration cells based on total cell number is given. Neutrophils do not show a significant increase in transmigration. Arithmetic means ± SEM (n = 3), * denotes significant difference to control (p ≤ 0.05)
SDF-1 signaling induces WASP phosphorylation
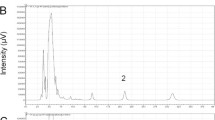
We visualized WASP as a central component of the migratory apparatus that regulates actin assembly and cell motility by immunofluorescence. We stimulated platelets with SDF-1 and stained them for the phosphorylated form of WASP. We found an increased phosphorylation of WASP in SDF-1-stimulated platelets (Fig. 6a, b), which could be confirmed by quantitative Western blot analysis as a threefold increase above baseline (Fig. 6c).
SDF-1 induces phophorylation of WASP, an important regulatory element of actin rearrangement and mobility. a Immunofluorescence staining and confocal microscopy of WASP phosphorylation in human platelets under SDF-1 exposure. Rhodamine phalloidin (red), WASP-P (green). b Representative western blot of increased SDF-1 induced WASP phosphorylation of four independent experiments. c Quantitative analysis of WASP phosphorylation by densitometry (Lg opacity) (n = 4, * denotes significant difference, p ≤ 0.05)
Platelets transmigrate into post-ischemic inflamed vessel walls in vivo
With intravital fluorescence microscopy we compared transmigration of eGFP platelets into vascular areas that were exposed to post-ischemic inflammation to non-inflamed vascular areas. Vascular inflammation was induced by ligation of intestinal arteries in mice with the subsequent septic, inflammatory vascular reaction. Platelets isolated from eGFP transgenic mice were infused during the reperfusion phase. We found an accumulation of transmigrated eGFP transgenic platelets within the vessel wall of inflamed arteries after the mice had been sacrificed and vessels had been stained with anti-GFP antibody (Fig. 7).
Platelets transmigrate into areas of post-ischemic vascular inflammation in vivo. Platelets invade the vessel wall of mesenteric artery after systemic inflammation. Transgenic eGFP platelets were transfused into murine mesenteric artery after the vessel had been exposed to systemic inflammation during intestinal ligation in vivo. Mesenteric arteries that had been exposed to vascular inflammation (ischemic) showed increased accumulation of transmigrated GFP-labeled platelets within the vessel wall compared to control tissue without exposure to inflammation (non-ischemic)
Discussion
In this study, we disclosed SDF-1-stimulated platelet migration and characterized the signaling cascade, which involves PTX-sensitive G-protein and PI3 kinase. We showed platelet transmigration through a porous transwell membrane and (activated) endothelium along an SDF-1 gradient in vitro.
We found that SDF-1-activated platelets are able to migrate on a fibrinogen and collagen surface. Based on microscopic observations, platelets appear to go through different stages of adhesion which determine their velocity of migration during the migration process.
Fast migrating platelets are not firmly adherent and show just a few isolated focal adhesion points (1.4 focal adhesion contacts), whereas platelets in later migration stages are characterized by more focal adhesions and slower migration (2.4 focal adhesion contacts). The amount of focal adhesion contacts correlates with the speed of migration.
SDF-1 exerts a classical chemotactic stimulus and guides the mobile platelets towards the source of SDF-1. Cell movement trajectories in Fig. 2a exemplify the increased directional mobility in the presence of SDF-1, whereas platelets that are not exposed to the chemokine are almost as mobile, but lack the directional sense and move randomly and undirected. Platelet integrin GPIIb/IIIa, at least, partially contributes to a coordinated surface mobility of platelets on fibrinogen since initial platelet adhesion to the fibrinogen surface and migratory activity after surface contact was reduced with a GPIIb/IIIa blocking antibody (Abciximab) (Fig. 2e). Inhibition of GPVI on collagen did not affect platelet mobility. Inhibition of neither GPIIbIIIa, GPVI, nor GPIb significantly affected platelet transmigration in transwell experiments. Further research is needed to identify critical surface receptors involved in platelet migration as targets for inhibitory control.
We visualized the phosphorylation of WASP, a crucial component of the migratory apparatus under SDF-1 exposure. WASP is activated by SDF-1 stimulation in lymphocytes [22, 23] and activates the actin-related protein (Arp) 2/3 complex via Rho-GTPases [24, 25]. We could show that SDF-1 increased phosphorylation of WASP in human platelets (Fig. 6). These effects have also been shown during cell migration in other cells [22, 24]. SDF-1 is a particularly interesting chemokine since few chemotactically active substances are known in platelets, and SDF-1 is highly expressed in atherosclerotic plaques [15], which emphasize its role in vascular inflammation.
We also tested whether platelets have also the potential to transmigrate through a porous membrane and through the endothelium. In a Boyden-like transwell chamber experiment, different cytokines were placed into the lower compartment. The actual pore size (0.4 μm) that was used is about five times smaller than the size of a regular platelet to exclude passive passage. SDF-1 led to a dose-dependent increase in platelet transmigration compared to the control medium. In contrast to SDF-1, other cytokines like IL-1β, TNF-α (for which platelets lack specific receptors), and ΕΝΑ−78, did not affect platelet transmigration. Thus, platelet migration appears to be specifically mediated through a limited number of chemokines. The SDF-1 effect does not appear to be a matter of activation since classical platelet activators such as thrombin failed to induce a significant increase in platelet transmigration. On the contrary, excessive thrombin activation appears to negatively affect transmigration based on the relative decrease in transmigration with thrombin/SDF-1 compared to SDF-1 alone. We conclude that the SDF-1 effect is indeed a chemotactic signal that affects the directional orientation of the cell (steering wheel) rather than the intrinsic migratory activity (engine). Furthermore, when the directing SDF-1 gradient was neutralized, platelet transmigration was reduced. We compared platelet transmigration under the influence of SDF-1 to other mobile cells like lymphocytes and neutrophils to validate our transmigration assay. It appears that only few platelets perform complete transmigration towards SDF-1 (1.6% of total platelets) compared to classical migrating cells such as lymphocytes; however, the abundance of platelets in the blood stream still represents a remarkable volume of migrating cells.
The transmigration of platelets through endothelium as a physiological barrier was significantly enhanced when compared to the control (0.16% versus 0.23% of platelets). We mimicked an inflammatory milieu by stimulating the endothelium with IL-1β, which indeed further facilitated platelet transmigration through the activated endothelium. The capability of platelets to transmigrate through endothelium suggests that platelets are able to invade the vessel wall. Although the amount of platelets that passes through the endothelial barrier is about eightfold less than without endothelium; the large quantity of platelets in the blood stream could still generate a significant, long-term invasion of platelets into the vessel wall. Previous reports demonstrated platelet chemotaxis towards fMLP in vitro [12] and extravasation into inflamed tissue [13]. Pitchford et al. showed the effect of IgE-mediated platelet extravasation in lung tissue [14]; however, the role of SDF-1 in platelet migration and the underlying signaling mechanisms of chemokine-mediated platelet migration have not yet been described. SDF-1 is of particular interest since platelets themselves store SDF-1 in intracellular granules and could thus subsequently attract other platelets or inflammatory cells to the vessel wall after transmigration to augment the chemoattractant effect. In contrast to fMLP, SDF-1 is physiological and is a more specific chemotactic agent in cell–cell interaction. Most of all, SDF-1 is involved in vascular inflammation and was found in atherosclerotic plaques [15].
So far, the SDF-1 signal transduction pathway and extended SDF-1 function have not been examined in platelets. In other cells, binding of SDF-1 to the chemokine receptor CXCR4 activates PI3 kinase [26] and induces aggregation in platelets [15]. PI3 kinase in turn regulates further downstream kinases like phosphoinositide-dependent kinase 1 (PDK1). PDK1 was shown to be involved in migration of endothelial cells [27].
We thus focused on the SDF-1 signaling pathway with regard to platelet migration. To examine crucial components of the SDF-1 signaling pathway on different levels of regulation, we analyzed the CXCR4-receptor level, G-protein level, and PI3 kinase level. SDF-1-induced transmigration could be effectively blocked in platelets on the receptor level with AMD3100, a CXCR4-receptor-specific inhibitor, as shown in other cells [28, 29]. PTX and PI3-kinase inhibitors like LY294002 and wortmannin, all reduced the transmigration of platelets significantly (Fig. 4a). In most cells, PTX affects signaling on the G-protein level downstream of the CXCR4-receptor by an ADP-ribosylation of G-protein subunits; however, in intact platelets, PTX has been shown to be unable to ADP-ribosylate the G-protein α subunit [30]. In parallel, several other reports [15, 31, 32] have demonstrated that PTX alters platelet activity, but probably by signaling mechanisms independent of ADP-ribosylation of G-protein α subunits. It therefore remains unclear by what exact mechanisms PTX disrupts G-protein-coupled intracellular signaling pathway in platelets.
Inhibition of PI3 kinase has also been successfully used to inhibit cell migration in other cells [33]. SDF-1-mediated transmigration proved to be a gradient-dependent process since neutralization of the SDF-1 gradient with equal amounts of chemokine on both sides reduced transmigration. With intravital microscopy, we tested the ability of murine platelets to transmigrate into the vessel wall of inflamed blood vessels after intestinal artery ligation in vivo. Although platelets accumulated outside the vessel lumen, intravital microscopy was not able to visualize platelet infiltrates within the vessel wall directly. Therefore, the mice were sacrificed and slices of vessel walls were stained with an anti-GFP secondary antibody to stain for platelet infiltrates. We found accumulation of GFP-labeled platelets in areas of the post-ischemically inflamed vessel wall compared to non-ischemic vessel areas. The increased subendothelial accumulation of platelets in this animal model suggests a transient invasion of platelets into areas of ischemia and inflammation that could reveal a new functional role of platelets in vascular biology. Since platelets appear to have the capacity to transmigrate through intact or minimally inflamed endothelium, they could function as pilot cells that guide further platelets or inflammatory cells like monocytes or stem cells.
In summary, SDF-1-mediated platelet migration is a novel and as yet uncharacterized phenomenon. SDF-1-mediated platelet transmigration involves signaling through PI3 kinase. Furthermore, transient platelet migration into the vessel wall could contribute to vascular mechanisms during the initiation of atherosclerosis and vascular regeneration.
References
Berger G, Hartwell DW, Wagner DD (1998) P-selectin and platelet clearance. Blood 92:4446–4452
Denis MM, Tolley ND, Bunting M, Schwertz H, Jiang H, Lindemann S, Yost CC, Rubner FJ, Albertine KH, Swoboda KJ et al (2005) Escaping the nuclear confines: signal-dependent pre-mRNA splicing in anucleate platelets. Cell 122:379–391
Lindemann S, Tolley ND, Dixon DA, McIntyre TM, Prescott SM, Zimmerman GA, Weyrich AS (2001) Activated platelets mediate inflammatory signaling by regulated interleukin 1beta synthesis. J Cell Biol 154:485–490
Lindemann S, Tolley ND, Eyre JR, Kraiss LW, Mahoney TM, Weyrich AS (2001) Integrins regulate the intracellular distribution of eukaryotic initiation factor 4E in platelets. A checkpoint for translational control. J Biol Chem 276:33947–33951
Jakab M, Ritter M (2006) Cell volume regulatory ion transport in the regulation of cell migration. Contrib Nephrol 152:161–180
Papakonstanti EA, Stournaras C (2008) Cell responses regulated by early reorganization of actin cytoskeleton. FEBS Lett 582:2120–2127
Ridley AJ, Schwartz MA, Burridge K, Firtel RA, Ginsberg MH, Borisy G, Parsons JT, Horwitz AR (2003) Cell migration: integrating signals from front to back. Science 302:1704–1709
Schwab A, Nechyporuk-Zloy V, Fabian A, Stock C (2007) Cells move when ions and water flow. Pflugers Arch 453:421–432
Lewin J (2002) The evolution of mammalian platelets. In: Michelson ED (ed) platelets. Academic, San Diego, pp 3–17
Kakoma I, Carson CA, Ristic M, Stephenson EM, Hildebrandt PK, Huxsoll DL (1978) Platelet migration inhibition as an indicator of immunologically mediated target cell injury in canine ehrlichiosis. Infect Immun 20:242–247
Valone FH, Austen KF, Goetzl EJ (1974) Modulation of the random migration of human platelets. J Clin Invest 54:1100–1106
Czapiga M, Gao JL, Kirk A, Lekstrom-Himes J (2005) Human platelets exhibit chemotaxis using functional N-formyl peptide receptors. Exp Hematol 33:73–84
Feng D, Nagy JA, Pyne K, Dvorak HF, Dvorak AM (1998) Platelets exit venules by a transcellular pathway at sites of F-met peptide-induced acute inflammation in guinea pigs. Int Arch Allergy Immunol 116:188–195
Pitchford SC, Momi S, Baglioni S, Casali L, Giannini S, Rossi R, Page CP, Gresele P (2008) Allergen induces the migration of platelets to lung tissue in allergic asthma. Am J Respir Crit Care Med 177:604–612
Abi-Younes S, Sauty A, Mach F, Sukhova GK, Libby P, Luster AD (2000) The stromal cell-derived factor-1 chemokine is a potent platelet agonist highly expressed in atherosclerotic plaques. Circ Res 86:131–138
Bleul CC, Fuhlbrigge RC, Casasnovas JM, Aiuti A, Springer TA (1996) A highly efficacious lymphocyte chemoattractant, stromal cell-derived factor 1 (SDF-1). J Exp Med 184:1101–1109
Hamada T, Mohle R, Hesselgesser J, Hoxie J, Nachman RL, Moore MA, Rafii S (1998) Transendothelial migration of megakaryocytes in response to stromal cell-derived factor 1 (SDF-1) enhances platelet formation. J Exp Med 188:539–548
Phillips R, Ager A (2002) Activation of pertussis toxin-sensitive CXCL12 (SDF-1) receptors mediates transendothelial migration of T lymphocytes across lymph node high endothelial cells. Eur J Immunol 32:837–847
Zheng H, Fu G, Dai T, Huang H (2007) Migration of endothelial progenitor cells mediated by stromal cell-derived factor-1alpha/CXCR4 via PI3K/Akt/eNOS signal transduction pathway. J Cardiovasc Pharmacol 50:274–280
Clemetson KJ, Clemetson JM, Proudfoot AE, Power CA, Baggiolini M, Wells TN (2000) Functional expression of CCR1, CCR3, CCR4, and CXCR4 chemokine receptors on human platelets. Blood 96:4046–4054
Stellos K, Langer H, Daub K, Schoenberger T, Gauss A, Geisler T, Bigalke B, Mueller I, Schumm M, Schaefer I et al (2008) Platelet-derived stromal cell-derived factor-1 regulates adhesion and promotes differentiation of human CD34+ cells to endothelial progenitor cells. Circulation 117:206–215
Haddad E, Zugaza JL, Louache F, Debili N, Crouin C, Schwarz K, Fischer A, Vainchenker W, Bertoglio J (2001) The interaction between Cdc42 and WASP is required for SDF-1-induced T-lymphocyte chemotaxis. Blood 97:33–38
Okabe S, Fukuda S, Broxmeyer HE (2002) Activation of Wiskott–Aldrich syndrome protein and its association with other proteins by stromal cell-derived factor-1alpha is associated with cell migration in a T-lymphocyte line. Exp Hematol 30:761–766
Higgs HN, Pollard TD (1999) Regulation of actin polymerization by Arp2/3 complex and WASp/Scar proteins. J Biol Chem 274:32531–32534
Thrasher AJ (2002) WASp in immune-system organization and function. Nat Rev Immunol 2:635–646
Fernandis AZ, Prasad A, Band H, Klosel R, Ganju RK (2004) Regulation of CXCR4-mediated chemotaxis and chemoinvasion of breast cancer cells. Oncogene 23:157–167
Primo L, di Blasio L, Roca C, Droetto S, Piva R, Schaffhausen B, Bussolino F (2007) Essential role of PDK1 in regulating endothelial cell migration. J Cell Biol 176:1035–1047
Hartmann TN, Grabovsky V, Pasvolsky R, Shulman Z, Buss EC, Spiegel A, Nagler A, Lapidot T, Thelen M, Alon R (2008) A crosstalk between intracellular CXCR7 and CXCR4 involved in rapid CXCL12-triggered integrin activation but not in chemokine-triggered motility of human T lymphocytes and CD34+ cells. J Leukoc Biol 84:1130–1140
Hatse S, Princen K, Bridger G, De Clercq E, Schols D (2002) Chemokine receptor inhibition by AMD3100 is strictly confined to CXCR4. FEBS Lett 527:255–262
Ui M (1984) Islet-activating protein, pertussis toxin: a probe for functions of the inhibitory guanine nucleotide regulatory component of adenylate cyclase. Trends Pharmacol Sci 5:277–279
Schäfer A, Schulz C, Eigenthaler M, Fraccarollo D, Kobsar A, Gawaz M, Ertl G, Walter U, Bauersachs J (2004) Novel role of the membrane-bound chemokine fractalkine in platelet activation and adhesion. Blood 103:407–12
Banga HS, Walker RK, Winberry LK, Rittenhouse SE (1987) Pertussis toxin can activate human platelets. Comparative effects of holotoxin and its ADP-ribosylating S1 subunit. J Biol Chem 262:14871–4
Choudhury GG, Karamitsos C, Hernandez J, Gentilini A, Bardgette J, Abboud HE (1997) PI-3-kinase and MAPK regulate mesangial cell proliferation and migration in response to PDGF. Am J Physiol 273:F931–F938
Acknowledgements
We thank Jadwiga Kwiatkowska, Christina Neff, and Birgit Fehrenbacher for providing outstanding technical assistance and Uwe Renzland for the help in preparing and formatting the movies. This study was supported by the Deutsche Forschungsgemeinschaft (Li 849/3-1 to S.L., SFB-TR19 TP B8 to K.S., M.G., and S.L.), the fortüne programme (1934-0-0 to O.B.) and the Karl-Kuhn-Stiftung (to S.L.).
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Bjoern F. Kraemer and Oliver Borst contributed equally to this work and share first authorship.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(recording time: 180 min, 30 frames/hour; replay 10 frames/second) Platelet chemotaxis toward a source of SDF-1. (Representative movie out of three experiments) (AVI 4567 kb)
(recording time: 180 min, 30 frames/hour; replay 10 frames/second) Control experiment to Movie I without chemokine at the target source. (Representative movie out of three experiments) (AVI 5222 kb)
(recording time: 57 min, six frames/minute; replay 20 frames/second) Example of a platelet that migrates toward the source of SDF-1 in the platelet cohort shown in Movie I. SDF-1 source at the top of the image (AVI 1091 kb)
(recording time: 85 min, 6 frames/minute; replay 20 frames/second) Platelet migration on a fibrinogen matrix. (Representative movie out of three experiments) (AVI 5968 kb)
(recording time: 20 min, six frames/minute; replay 20 frames/second) Inhibition of platelet migration with cytochalasin B. (Representative movie out of three experiments) (AVI 2188 kb)
Supplemental Figure 1
SDF-1 mediated Platelet Transmigration. Absolute numbers of transmigrating platelets towards a source of SDF-1 (supplemental to Figure 3A) (PDF 10 kb)
Supplemental Figure 2
SDF-1-mediated transmigration of platelets through activated and unactivated endothelium, absolute numbers and percentage of platelets transmigrating (%), supplemental to Fig. 3b (PDF 8 kb)
Supplemental Figure 3
Table summary of SDF-1 mediated platelet transmigration with and without endothelium, absolute numbers and percentage of transmigrating platelets (%) (PDF 7 kb)
Supplemental Figure 4
Absolute numbers of platelet transmigration and inhibition of SDF-1-induced platelet transmigration by blockers of the CXCR4-receptor (AMD3100), G-protein (PTX) and PI3 kinase (wortmannin; LY 294002), supplemental to Fig. 4a (PDF 8 kb)
Supplemental Figure 5
Role of platelet activation for transmigrational activity. Platelet baseline transmigration is slightly increased with thrombin activation which does not meet the robust increase in transmigration with SDF-1 alone. On the contrary, excessive pre-activation of platelets with thrombin appears to negatively interfere with the SDF-1 effect compared to SDF-1 alone (PDF 7 kb)
Rights and permissions
About this article
Cite this article
Kraemer, B.F., Borst, O., Gehring, EM. et al. PI3 kinase-dependent stimulation of platelet migration by stromal cell-derived factor 1 (SDF-1). J Mol Med 88, 1277–1288 (2010). https://doi.org/10.1007/s00109-010-0680-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-010-0680-8