Abstract
Large epidemiological studies suggest a clear relation between low birth weight and adverse renal outcomes evident as early as during childhood. Such adverse outcomes may include glomerular disease, hypertension, and renal failure. Data from autopsy material and from experimental models suggest that reduction in nephron number via diminished nephrogenesis may be a major mechanism, and factors that lead to this reduction are incompletely elucidated. Other mechanisms appear to be renal (e.g., via the intrarenal renin–angiotensin–aldosterone system) and nonrenal (e.g. changes in endothelial function). It also appears likely that the outcomes of fetal programming may be influenced postnatally, for example, by the amount of nutrients given at critical times.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
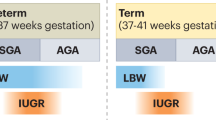
Recent studies have demonstrated an increased prevalence of end-stage renal failure in adults who were small for gestational age (SGA) at birth [2, 3]. However, whether low birth weight is a primary risk factor for renal dysfunction in later life requires further examination. Such questions as whether epidemiological evidence that low birth weight infants have a higher risk of renal dysfunction in later life is robust and whether a reduction in nephron number is involved must be more definitively answered. Whether specific mechanisms are involved and whether programming of renal disease ends with birth or continues with postnatal modification are questions requiring further study. The present review aims to address these issues.
Epidemiological and experimental evidence for altered renal function after low birth weight at term
A relatively lower birth weight has been associated with many subsequent health problems. Approximately 10 years ago, Lackland and coworkers reported that low birth weight was associated with early onset end-stage renal failure in US residents from a variety of ethnic backgrounds [1]. Of 1,230 cases with ESRD, 70% of patients (858) were black, 72% (892) were male, 19% (233) had diabetes, 29% (359) had hypertension, and 46% (571) were “other.” The odds ratio (OR) for renal failure was 1.4 (95% confidence interval [95%CI], 1.1–1.8) for the entire group including patients with diabetes mellitus and hypertension. More recently, Li et al. reported that more men who self-reported having had a relatively low or a relatively high birth weight also had evidence of chronic kidney disease (CKD) when screened using estimated glomerular filtration rate (eGFR) [4]. A U-shaped association between birth weight and CKD in men was observed, compared with men whose birth weight was between 3,000 and 3,999 g, those whose birth weight was less than 2,500 g had 1.65-fold odds (95%CI, 1.24–2.20) of CKD, and those whose birth weight was 4,500 g or over had 1.41-fold odds (95%CI, 1.06–1.88) of CKD [4].
One difficulty with such associational studies is that the primary effects of low birth weight on renal function cannot be separated from conditions that were also associated with SGA birth, such as maternal diabetes mellitus type 2 and arterial hypertension during gestation.
A recently published report from a population-based cohort of 7,457 young Norwegian adults participating in the Nord Trøndelag Health [HUNT 2] Study was of great interest because the subjects were young and generally free of chronic conditions such as diabetes mellitus and hypertension [5]. The authors observed a birth weight-dependent increase in the incidence of renal failure that was evident as early as 20–30 years of age in a cohort without obvious confounders. Compared with men with birth weight appropriate for gestational age (n = 2,755), ORs for low–normal creatinine clearance (<100 mL/min) were 1.66 (95%CI, 1.16–2.37) if SGA (n = 261) and 2.40 (95%CI, 1.46–3.94) if very SGA (n = 101); similar results were seen in women [5]. Lopez et al. reported similar results in children [6].
Focusing on end-stage renal disease, a hard clinical endpoint, a recent large population-based cohort study reported that of 2,183,317 children born in Norway between 1967 and 2004, 526 developed end-stage renal disease. Those with a birth weight below the tenth percentile (SGA) had a higher risk of end-stage renal failure than those who were not SGA (relative risk 1.5; 95%CI, 1.2–1.9). Furthermore, the development of end-stage renal disease in former SGA patients compared to controls appeared to be more probable below 14 years of age than after age 15 [2]. Patients under the age of 14 years are unlikely to have factors predisposing for chronic renal failure such as diabetes mellitus and hypertension. Thus, the reason for higher incident end-stage renal disease under age 15 is unclear, particularly whether a separate analysis excluding congenital malformations would come up with the same results. While the study of Vikse et al. was able to show an association between birth weight and end-stage renal disease, not all studies have been able to demonstrate altered renal function in SGA children [7].
In a current meta-analysis by White and coworkers that included 32 studies, 16 reported a significant association between low birth weight and risk of CKD and 16 observed a null result. The combination of weighted estimates from the 18 studies for which risk estimates were available (n = 46,249 plus 2,183,317 from the record linkage study) gave an overall OR of 1.73 (95%CI, 1.44–2.08). Combined ORs were consistent in magnitude and direction for risks of albuminuria (OR, 1.81; 95%CI, 1.19–2.77), end-stage renal disease (OR, 1.58; 95%CI, 1.33–1.88), or low eGFR (OR, 1.79; 95%CI, 1.31–2.45) [8].
Glomerular disease in childhood and relation to birth weight
Idiopathic or minimal lesion nephrotic syndrome in childhood is usually associated with a good prognosis and an initial complete response to glucocorticoids with resolution of proteinuria in about 90% of patients [9]. A poor course is either characterized by steroid dependence (relapses when glucocorticoids are tapered) or steroid resistance (lack of response to glucocorticoids). Retrospective clinical studies have reported that children with a history of low birth weight who have idiopathic nephrotic syndrome have a higher incidence of relapses and steroid dependence [10, 11, 15]. Children with such a course have a higher need for additional therapy to control their nephritic syndrome, for example, alkylating agents and cyclosporine A. Other, more recent studies have confirmed a more severe course and a higher rate of steroid resistance in children with nephrotic syndrome with a history of having been SGA babies [12, 13]. However, the underlying mechanisms are not yet delineated.
Data reported in the 1990s indicate that up to 30% of patients with IgA nephropathy presenting in childhood eventually develop end-stage renal failure [14]. A retrospective study of 62 children with IgA nephropathy reported a threefold greater number of sclerotic glomeruli among those children with IgA nephropathy who were born SGA compared to those who were not [11, 15]. However, no recent data linking birth weight with progression of IgA nephropathy appear to be available.
Most children who develop acute post streptococcal glomerulonephritis recover well. However, a recent paper speculated that low birth weight [16] may be associated with adverse outcomes. In a case report of a child with bilateral renal hypoplasia and, at age 8, an episode of acute glomerulonephritis, a poor outcome was hypothesized due to the low nephron endowment [17]. The authors review the literature on acute post infectious nephritis and suggest that fewer nephrons may be associated with poorer outcome. Whether children with a history of low birth weight are more prone to develop focal renal scarring has been addressed in both a study by Hellström et al. [19] and in a commentary by Winberg [18], both raise the possibility that renal endowment may play a role in the response to acquired renal disease in the context of an influence of low birth weight on renal scarring due to urinary tract infection.
Intrauterine growth restriction and later morbidity: animal models
Most data originating from human studies are based on epidemiological associations. Although epidemiological methods minimize confounding factors as much as possible, such studies are associative and cannot prove causal relationships between an initial programming event such as intrauterine growth restriction (IUGR) and later morbidity. Therefore, animal studies have been utilized to demonstrate causal relationships. The most widely used models are a physical model of uterine artery ligation in the rat and protein restriction in the rat and other mammalian species. In this section, space limitations permit us to cover only principles of the animal models.
The ligation of both uterine arteries reduces blood flow to the placentas of individual rat fetuses. This model is, therefore, considered reminiscent of placental insufficiency in humans. Uterine artery ligation is commonly used to examine metabolic disorders such as diabetes mellitus [20, 21] and also to explore the effects on renal disease [25].
Protein restriction has been the most widely used method for demonstrating how IUGR affects the cardiovascular system and the kidney [22–24]. Although a number of mammalian models of protein restriction have been employed, most studies have been carried out in rats. In such work, pregnant rats are fed an isocaloric but protein-restricted diet, varying from 10% to 40% of normal protein intake. This model mimics protein restriction, which is thought to be a frequent cause for IUGR in developing countries.
Recently, the protein-restricted model was employed to examine susceptibility to acquired renal diseases. For example, using a protein restriction animal model, we studied male IUGR offspring of protein-restricted mothers and observed that these offspring subsequently had increased susceptibility to a more severe and potentially chronic course when an acute mesangioproliferative glomerulonephritis [injection of an anti-Thy-1.1 antibody] was induced [24]. Such studies suggest that animal models may have additional utility for addressing putative causal relationships between IUGR and kidney disease and may help to delineate the mechanisms of fetal programming of renal disease.
More details on animal models and their use in unraveling mechanisms of fetal programming may be obtained from recent overviews [26, 27].
Low nephron number and fetal programming of renal function
Nephron number has been acknowledged as a determinant of susceptibility to renal disease [28, 29] and, possibly, to the development of hypertension both in animal models [30] and in human beings [31–33]. During nephrogenesis, both intrinsic and extrinsic factors with myriad interactions “program” nephron number, ultimately resulting in what has been called “nephron endowment” [34]. Following the completion of nephrogenesis, no further nephrons are formed, but subsequent nephron loss due to aging or renal injury decreases nephron number.
The sequence and timing of nephrogenesis (in rodents, usually complete by 14 days of life) and a number of the mechanisms by which the different steps occur appear tightly regulated [34, 35]. Table 1 shows some of the genes involved in nephrogenesis and lists abnormalities that may occur when there are mutations. Mice with deletion of genes that are important for crucial steps of nephrogenesis, such as paired homeobox-2 (Pax-2) or glial cell line-derived neurotrophic growth factor (GDNF) [36], have a decrease in nephron number. Likewise, patients with specific mutations in genes involved in nephrogenesis may have a decrease in nephron number [35].
It was recently reported that common variants of two genes, PAX2 [37] and RET [38], are associated with renal size in humans. However, a variant in GDNF did not appear linked with renal size in humans [39]. However, such association studies require replication in additional populations before conclusions can be reached.
Although the final complement of nephrons is likely genetically predetermined to some extent, it may be compromised by adverse environmental conditions. IUGR is probably the best investigated condition that results in impaired nephrogenesis and nephron underdosing. Among the factors that have been shown to interfere with nephrogenesis during the critical period are selective vitamin deficiencies, certain antibiotics, maternal infections, hyperglycemia, and steroid administration [40, 41]. Unfortunately, the data from studies of such factors are difficult to interpret, since timing and dosage appears to be important—e.g., steroid administration can program the renin–angiotensin–aldosterone system (RAAS), but the effect depends on when during gestation the drug is administered.
Given the complexity of nephrogenesis, it is doubtful that low nephron number is the sole consequence of materno-fetal disturbances during the critical period of nephrogenesis. However, it seems likely that an adverse intrauterine environment may result in additional structural and/or functional defects, for example, altered tubular handling of sodium, potassium, or chloride or aberrant or inappropriate activation of other vasoactive systems (i.e., the RAAS) that may have detrimental consequences on long-term kidney function [41].
In most human studies, a strong correlation has been noted between glomerular number and low birth weight on one hand [42] and kidney mass on the other, suggesting that either birth weight or kidney volume might roughly correlate with nephron number, permitting these measures to be used as surrogate markers. Another surrogate marker for nephron number might be glomerular size or volume. It is well known that nephron reduction in animal models and human beings is accompanied by glomerular enlargement, presumably as a compensatory mechanism. Glomerular enlargement is most likely caused by hyperfiltration of remaining glomeruli in order to sustain whole kidney function [43]. The concept that hyperfiltering glomeruli progress to glomerular sclerosis in the setting of low nephron number was first addressed by Brenner in his hyperperfusion injury hypothesis [31, 44], which posited that hyperfiltration had the potential to accelerate the progression of renal insufficiency.
Increased blood pressure is often present in the setting of renal insufficiency, but a relationship between low nephron number and higher blood pressure likely develops much earlier in the pathophysiological cascade. Support for this concept was provided most clearly by Keller et al. [32] who reported a small case control autopsy study that observed that persons dying with hypertension had about 50% fewer glomeruli with a mean volume about 50% larger compared to people without hypertension. Limitations included the fact that there were only ten people in each group and all were Caucasian. These relationships have been confirmed in a larger autopsy study in white Americans, but could not be confirmed in African Americans [33]. The general paucity of glomerulosclerosis in both studies would argue against accelerated nephron loss as the primary cause of lower nephron number. These findings are at least compatible with the concept that higher blood pressure might derive, in part, from reduced nephron endowment [31]. The underlying pathogenic mechanisms, however, are not as yet clear from human studies. These issues have been studied in greater depth in rats and sheep. Such animal studies indicate that an experimentally induced loss of a critical nephron mass during fetal development or shortly after birth favors the development of hypertension and subsequent kidney damage [45]. In human beings with unilateral kidney aplasia [46] as well as in kidney transplant recipients of small donor kidneys with lower nephron number, there is an increased risk of hypertension and, in the case of transplants, graft failure [47, 48]. In children with congenital unilateral renal agenesis, elevated 24 h blood pressure was noted compared with children who had unilateral renal nephrectomy after birth [49]. On the other hand, donation of a kidney or unilateral nephrectomy of the adult [either man or rat] leads to increased risk of proteinuria, but not necessarily to marked hypertension [50].
Other mechanisms contributing to fetal programming of renal function
A number of vasoactive systems that contribute to nephrogenesis appear to be altered in response to change in the intrauterine milieu. An important indicator of changes in the intrauterine milieu that might lead to fetal programming of renal disease is thought to be alteration in the RAAS. Experimental models of fetal programming have reported an increased renal renin expression in adult rats that had been born IUGR after maternal protein restriction [51–53]. Furthermore, in neonatal rats born to protein-restricted dams, there was a suppression of the RAAS [22]. More recently, it was reported that the adrenal expression of the angiotensin II 1b receptor [AT1b-R] in rats with IUGR is increased. This is likely due to an epigenetic mechanism, as the authors observed that the proximal promoter of the AT1b-R gene was hypomethylated, which would facilitate heightened transcriptional activity [53]. In humans, there is only one AT1 receptor, rendering it unclear whether these findings would apply to humans. However, in a recent clinical study, increased salt sensitivity was reported to be present in children with low birth weight, which might indicate a higher aldosterone activity or a change in AT1 receptor expression or affinity [54].
These results may indicate that the RAAS is primarily suppressed after IUGR before it becomes hyperactive later in life, which might contribute to hypertension and renal disease.
Another renal alteration that has been reported in models of maternal protein restriction is an alteration in the activity of 11β-hydroxysteroid dehydrogenase [11βHSD]. This enzyme, present in the cells of the distal renal tubule, converts active cortisol into inactive cortisone [55]. Under physiological circumstances, this reaction protects the mineralocorticoid receptor from stimulation by cortisol. In the IUGR rat model, renal 11βHSD expression is reduced, allowing for increased mineralocorticoid activity [56]. Interestingly, a reduction of 11βHSD has been reported in the placenta of human pregnancies complicated by IUGR [57, 58]. These observations might imply that maternal cortisol, which is usually inactivated by the placental 11βHSD2 can pass to the fetus. As a consequence, cortisol may lead to growth restriction and potentially to a programming of renal 11βHSD in the unborn child [55, 56].
In addition to renal mechanisms, programming of extrarenal tissues has been investigated with regard to potential roles in increasing the risk of future renal and vascular disease. For example, the endothelium and its interaction with vascular smooth muscle cells may contribute to the likelihood of future renal and vascular disease. Low-birth-weight human newborns at 3 days of life have been demonstrated to have an attenuated forearm skin vasodilation response to local application of acetylcholine [59]. Similar findings have been reported on older children and young adults [60]. In addition, a study in which sodium nitroprusside, which causes endothelium-independent vasodilation, was administered did not reveal differences between children with low and normal birth weight [61]. Thus, the endothelium, with its multiple signaling systems, particularly the NO system, may be important in programming of adult disease. Impaired NO-mediated vasodilation, increased generation of superoxide, and decreased expression of soluble guanylate cyclase have been proposed as potential mechanisms [27]. Whether such mechanisms might contribute to renal dysfunction is unknown at present.
Another extrarenal mechanism that has been considered in the context of fetal programming of kidney disease is increased sympathetic nerve activity, since there is a relation between birth weight and basal heart rate in adulthood [62]. The hypothesis that increased sympathetic nerve activity is a consequence of a challenging intrauterine environment is supported by animal data reporting that denervation of renal sympathetic nerve supply leads to a normalization of blood pressure in IUGR rats [63]. Such a mechanism is of almost certain importance for renal function, since sympathetic nerve activity regulates intrarenal renin synthesis and salt retention.
Postnatal modification of fetal programming of kidney disease
One of the first potential strategies considered to prevent morbidity after IUGR is the avoidance of hyperalimentation. Data concerning the offspring of two famines that occurred during World War II, the Dutch famine, and the Siege of Leningrad show different results. Offspring of women who endured the Dutch famine at the end of World War II had a higher incidence of metabolic diseases such as diabetes mellitus type 2 later in life if their mothers had been in the third trimester during the nutrient deprivation [64]. In contrast, there was no increase in either the incidence of glucose intolerance or type 2 diabetes among offspring whose mothers were pregnant during the Siege of Leningrad [65]. The traditional explanation, although challenged, is that intrauterine nutrient deprivation led to a programming of endocrine systems towards energy saving in fetal life. If there was continued nutrient deprivation after birth, this would be well tolerated by a baby whose intrauterine environment was also deprived [as in the Leningrad offspring]. In contrast, rapid reconstitution of energy supplies and, therefore, relative surplus of energy, as in the offspring of the Dutch famine, would lead to deposition of adipose tissue, predisposing to pathological glucose tolerance. Details concerning this so-called match–mismatch phenomenon is summarized in a recent review by Gluckman et al. [66]. There is considerable evidence that rapid increase in caloric and protein intake postnatally plays an important pathophysiological role in developmental origins of health and disease [67]. Low birth weight and premature infants grow at different rates, and rapid “catch-up” growth may not be good. For example, babies who had higher calorie and protein intake from infant formula boosted from 284 to 301 kcal/100 ml and from 1.4 to 1.8 g/100 ml of protein had an increase of diastolic blood pressure by 3.5 mmHg at the age of 6–8 years [68]. In another study, accelerated catch-up growth was associated with higher blood pressure [69]. Given such reports, the International Societies of Paediatric Endocrinology and the Growth Hormone Research Society presently discourage nutrient-enriched diets for low-birth-weight infants [67].
Whether these observations are of importance for renal function as well is not yet known and might be subject for future studies. In the previously mentioned retrospective study in 62 children with idiopathic nephrotic syndrome in which the authors looked at the course of the disease and related it to birth weight and weight gain in the first 24 months of life, there was no association between the extent of postnatal catch-up growth and the severity of disease [12].
Conclusions
Adverse outcomes after low birth weight include glomerular disease, hypertension, and renal failure. Reduction in nephron number may be a major mechanism, and factors that lead to this reduction must be elucidated. It also appears likely that the outcomes of fetal programming may be influenced postnatally, for example, by the amount of nutrients given at critical times (Fig. 1). Thus, it is important to consider how much hyperalimentation should be provided during a newborn intensive care unit stay, or whether, in some circumstances, it should be avoided.
References
Lackland DT, Egan BM, Fan ZJ, Syddall HE (2001) Low birth weight contributes to the excess prevalence of end-stage renal disease in African Americans. J Clin Hypertens 3:29–31
Vikse BE, Irgens LM, Leivestad T, Hallan S, Iversen BM (2008) Low birth weight increases risk for end-stage renal disease. J Am Soc Nephrol 19:151–157
Lackland DT, Bendall HE, Osmond C, Egan BM, Barker DJ (2000) Low birth weights contribute to high rates of early-onset chronic renal failure in the Southeastern United States. Arch Intern Med 160:1472–1476
Li S, Chen SC, Shlipak M, Bakris G, McCullough PA, Sowers J, Stevens L, Jurkovitz C, McFarlane S, Norris K, Vassalotti J, Klag MJ, Brown WW, Narva A, Calhoun D, Johnson B, Obialo C, Whaley-Connell A, Becker B, Collins AJ, Kidney Early Evaluation Program Investigators (2008) Low birth weight is associated with chronic kidney disease only in men. Kidney Int 73:637–642
Hallan S, Euser AM, Irgens LM, Finken MJ, Holmen J, Dekker FW (2008) Effect of intrauterine growth restriction on kidney function at young adult age: the Nord Trøndelag Health [HUNT 2] Study. Am J Kidney Dis 51:10–20
López-Bermejo A, Sitjar C, Cabacas A, Vázquez-Ruíz M, García-González MM, Mora C, Soriano P, Calvo M, Ibáñez L (2008) Prenatal programming of renal function: the estimated glomerular filtration rate is influenced by size at birth in apparently healthy children. Pediatr Res 64:97–99
Franco MC, Nishida SK, Sesso R (2008) GFR estimated from cystatin C versus creatinine in children born small for gestational age. Am J Kidney Dis 51:925–932
White SL, Perkovic V, Cass A, Chang CL, Poulter NR, Spector T, Haysom L, Craig JC, Salmi IA, Chadban SJ, Huxley RR (2009) Is low birth weight an antecedent of CKD in later life? A systematic review of observational studies. Am J Kidney Dis 54(2):248–261
Dötsch J, Dittrich K, Plank C, Rascher W (2006) Is tacrolimus for childhood steroid-dependent nephrotic syndrome better than ciclosporin A? Nephrol Dial Transplant 21:1761–1763
Sheu JN, Chen JH (2001) Minimal change nephrotic syndrome in children with intrauterine growth retardation. Am J Kidney Dis 37:909–914
Zidar N, Avgustin Cavic M, Kenda RB, Ferluga D (1998) Unfavorable course of minimal change nephrotic syndrome in children with intrauterine growth retardation. Kidney Int 54:1320–1323
Plank C, Östreicher I, Rascher W, Dötsch J (2007) Born SGA, but not postnatal weight gain aggravates the course of nephrotic syndrome in children. Pediatr Nephrol 22:1881–1889
Teeninga N, Schreuder MF, Bökenkamp A, de Waal HA Delemarre-van, van Wijk JA (2008) Influence of low birth weight on minimal change nephrotic syndrome in children, including a meta-analysis. Nephrol Dial Transplant 23:1615–1620
Goldstein AR, White RH, Akuse R, Chantler C (1992) Long-term follow-up of childhood Henoch–Schönlein nephritis. Lancet 339:280–282
Zidar N, Cavic MA, Kenda RB et al (1998) Effect of intrauterine growth retardation on the clinical course and prognosis of IgA glomerulonephritis in children. Nephron 79:28–32
Herrera J, Rodríguez-Iturbe B (2003) End-stage renal disease and acute glomerulonephritis in Goajiro Indians. Kidney Int Suppl (83):S22–S26
Naito-Yoshida Y, Hida M, Maruyama Y, Hori N, Awazu M (2005) Poststreptococcal acute glomerulonephritis superimposed on bilateral renal hypoplasia. Clin Nephrol 63:477–480
Winberg J (2001) Does low birthweight facilitate postinfectious focal renal scarring? Acta Paediatr 90:835–836
Hellström J, Hessel H, Jacobsson B, Jodal U, Niklasson A, Wennerström M et al (2001) Association between urinary tract infection, renal damage and birth size. Acta Paediatr 90:628–631
Stoffers DA, Desai BM, DeLeon DD, Simmons RA (2003) Neonatal exendin-4 prevents the development of diabetes in the intrauterine growth retarded rat. Diabetes 52:734–740
Nüsken KD, Dötsch J, Rauh M, Rascher W, Schneider H (2008) Uteroplacental insufficiency after bilateral uterine artery ligation in the rat: impact on postnatal glucose and lipid metabolism and evidence for metabolic programming of the offspring by sham operation. Endocrinology 149:1056–1063
Woods LL, Ingelfinger JR, Nyengaard JR, Rasch R (2001) Maternal protein restriction suppresses the newborn renin–angiotensin system and programs adult hypertension in rats. Pediatr Res 49:460–467
Elmes MJ, Gardner DS, Langley-Evans SC (2007) Fetal exposure to a maternal low-protein diet is associated with altered left ventricular pressure response to ischemia–reperfusion injury. Br J Nutr 98:93–100
Plank C, Östreicher I, Hartner A, Marek I, Struwe FG, Amann K, Hilgers KF, Rascher W, Dötsch J (2006) Intrauterine growth retardation aggravates the course of acute mesangioproliferative glomerulonephritis in the rat. Kidney Int 70:1974–1982
Wlodek ME, Westcott K, Siebel AL, Owens JA, Moritz KM (2008) Growth restriction before or after birth reduces nephron number and increases blood pressure in male rats. Kidney Int 74:187–195
Langley-Evans SC (2009) Nutritional programming of disease: unravelling the mechanism. J Anat 215:36–51
Nuyt AM (2008) Mechanisms underlying developmental programming of elevated blood pressure and vascular dysfunction: evidence from human studies and experimental animal models. Clin Sci (Lond) 114:1–17
Brenner BM, Mackenzie HS (1997) Nephron mass as a risk factor for progression of renal disease. Kidney Int Suppl 63:S124–S127
Hoy WE, Bertram JF, Denton RD, Zimanyi M, Samuel T, Hughson MD (2008) Nephron number, glomerular volume, renal disease and hypertension. Curr Opin Nephrol Hypertens 17:258–265
Woods LL, Weeks DA, Rasch R (2004) Programming of adult blood pressure by maternal protein restriction: role of nephrogenesis. Kidney Int 65:1339–1348
Brenner BM, Garcia DL, Anderson S (1988) Glomeruli and blood pressure: less of one, more of the other? Am J Hypertens 1:335–347
Keller G, Zimmer G, Mall G, Ritz E, Amann K (2003) Nephron number in patients with primary hypertension. N Engl J Med 348:101–108
Hughson MD, Douglas-Denton R, Bertram JF, Hoy WE (2006) Hypertension, glomerular number, and birth weight in African Americans and white subjects in the southeastern United States. Kidney Int 69:671–678
Kuure S, Vuolteenaho R, Vainio S (2000) Kidney morphogenesis: cellular and molecular regulation. Mech Dev 92:31–45
Ingelfinger JR (2003) Is microanatomy destiny? N Engl J Med 348:99–100
Cullen-McEwen LA, Kett MM, Dowling J, Anderson WP, Bertram JF (2003) Nephron number, renal function, and arterial pressure in aged GDNF heterozygous mice. Hypertension 41:335–340
Quinlan J, Lemire M, Hudson T, Qu H, Benjamin A, Roy A, Pascuet E, Goodyer M, Raju C, Zhang Z, Houghton F, Goodyer P (2007) A common variant of the PAX2 gene is associated with reduced newborn kidney size. J Am Soc Nephrol 18:1915–1921
Zhang Z, Quinlan J, Hoy W, Hughson MD, Lemire M, Hudson T, Hueber PA, Benjamin A, Roy A, Pascuet E, Goodyer M, Raju C, Houghton F, Bertram J, Goodyer P (2008) A common RET variant is associated with reduced newborn kidney size and function. J Am Soc Nephrol 19:2027–2034
Zhang Z, Quinlan J, Grote D, Lemire M, Hudson T, Benjamin A, Roy A, Pascuet E, Goodyer M, Raju C, Houghton F, Bouchard M, Goodyer P (2009) Common variants of the glial cell-derived neurotrophic factor gene do not influence kidney size of the healthy newborn. Pediatr Nephrol (in press)
Schreuder MF, Nauta J (2007) Prenatal programming of nephron number and blood pressure. Kidney Int 72:265–268
Koleganova N, Piecha G, Ritz E (2009) Prenatal causes of kidney disease. Blood Purif 27:48–52
Hughson M, Farris AB 3 rd, Douglas-Denton R, Hoy WE, Bertram JF (2003) Glomerular number and size in autopsy kidneys: the relationship to birthweight. Kidney Int 63:2113–2122
Fogo A, Ichikawa I (1991) Evidence for a pathogenetic link between glomerular hypertrophy and sclerosis. Am J Kidney Dis 17:666–669
Brenner BM, Lawler EV, Mackenzie HS (1996) The hyperfiltration theory: a paradigm shift in nephrology. Kidney Int 49:1774–1777
Moritz KM, Wintour EM, Dodic M (2002) Fetal uninephrectomy leads to postnatal hypertension and compromised renal function. Hypertension 39:1071–1076
Argueso LR, Ritchey ML, Boyle ET Jr, Milliner DS, Bergstralh EJ, Kramer SA (1992) Prognosis of patients with unilateral renal agenesis. Pediatr Nephrol 6:412–416
Brenner BM, Milford EL (1993) Nephron underdosing: a programmed cause of chronic renal allograft failure. Am J Kidney Dis 21(5 Suppl 2):66–72
Douverny JB, Baptista-Silva JC, Pestana JO, Sesso R (2007) Importance of renal mass on graft function outcome after 12 months of living donor kidney transplantation. Nephrol Dial Transplant 22:3646–3651
Mei-Zahav M, Korzets Z, Cohen I, Kessler O, Rathaus V, Wolach B, Pomeranz A (2001) Ambulatory blood pressure monitoring in children with a solitary kidney—a comparison between unilateral renal agenesis and uninephrectomy. Blood Press Monit 6:263
Boudville N, Prasad GV, Knoll G, Muirhead N, Thiessen-Philbrook H, Yang RC, Rosas-Arellano MP, Housawi A, Garg AX (2006) Donor Nephrectomy Outcomes Research (DONOR) Network. Meta-analysis: risk for hypertension in living kidney donors. Ann Intern Med 145:185–196
Langley-Evans SC, Sherman RC, Welham SJ, Nwagwu MO, Gardner DS, Jackson AA (1999) Intrauterine programming of hypertension: the role of the renin–angiotensin system. Biochem Soc Trans 27:88–93
Sahajpal V, Ashton N (2003) Renal function and angiotensin AT1 receptor expression in young rats following intrauterine exposure to a maternal low-protein diet. Clin Sci (Lond) 104:607–614
Bogdarina I, Welham S, King PJ, Burns SP, Clark AJ (2007) Epigenetic modification of the renin–angiotensin system in the fetal programming of hypertension. Circ Res 100:520–526
Simonetti GD, Raio L, Surbek D, Nelle M, Frey FJ, Mohaupt MG (2008) Salt sensitivity of children with low birth weight. Hypertension 52:625–630
Seckl JR, Meaney MJ (2004) Glucocorticoid programming. Ann N Y Acad Sci 1032:63–84
Bertram C, Trowern AR, Copin N, Jackson AA, Whorwood CB (2001) The maternal diet during pregnancy programs altered expression of the glucocorticoid receptor and type 2 11beta-hydroxysteroid dehydrogenase: potential molecular mechanisms underlying the programming of hypertension in utero. Endocrinology 142:2841–2853
Schoof E, Girstl M, Frobenius W, Kirschbaum M, Dörr HG, Rascher W, Dötsch J (2001) Reduced placental gene expression of 11ß hydroxysteroid dehydogenase type 2 and 15-hydrodroxy prostaglandin dehydrogenase in patients with preeclampsia J. Clin Endocrinol Metab 86:1313–1317
Struwe E, Berzl D, Schild RL, Beckmann MW, Dörr HG, Rascher W, Dötsch J (2007) Simultaneously reduced gene expression of cortisol-activating and cortisol-inactivating enzymes in placentas of small-for-gestational-age neonates. Am J Obstet Gynecol 197:43.e1–43.e6
Martin H, Gazelius B, Norman M (2000) Impaired acetylcholine-induced vascular relaxation in low birth weight infants: implications for adult hypertension? Pediatr Res 47:457–462
Franco MC, Christofalo DM, Sawaya AL, Ajzen SA, Sesso R (2006) Effects of low birth weight in 8- to 13-year-old children: implications in endothelial function and uric acid levels. Hypertension 48:45–50
Martin H, Hu J, Gennser G, Norman M (2000) Impaired endothelial function and increased carotid stiffness in 9-year-old children with low birth weight. Circulation 28(102):2739–2744
Phillips DI, Barker DJ (1997) Association between low birth weight and high resting pulse in adult life: is the sympathetic nervous system involved in programming the insulin resistance syndrome? Diabet Med 14:673–677
Alexander BT, Hendon AE, Ferril G, Dwyer TM (2005) Renal denervation abolishes hypertension in low-birth-weight offspring from pregnant rats with reduced uterine perfusion. Hypertension 45:754–758
Ravelli AC, van der Meulen JH, Michels RP, Osmond C, Barker DJ, Hales CN, Bleker OP (1998) Glucose tolerance in adults after prenatal exposure to famine. Lancet 351:173–177
Stanner SA, Yudkin JS (2001) Fetal programming and the Leningrad Siege study. Twin Res 4:287–292
Gluckman PD, Hanson MA, Cooper C, Thornburg KL (2008) Effect of in utero and early-life conditions on adult health and disease. N Engl J Med 359:61–73
Clayton PE, Cianfarani S, Czernichow P, Johannsson G, Rapaport R, Rogol A (2007) Management of the child born small for gestational age through to adulthood: a consensus statement of the International Societies of Pediatric Endocrinology and the Growth Hormone Research Society. J Clin Endocrinol Metab 92:804–810
Singhal A, Cole TJ, Fewtrell M, Kennedy K, Stephenson T, Elias-Jones A, Lucas A (2007) Promotion of faster weight gain in infants born small for gestational age: is there an adverse effect on later blood pressure? Circulation 115:213–220
Ben-Shlomo Y, McCarthy A, Hughes R, Tilling K, Davies D, Davey Smith G (2008) Immediate postnatal growth is associated with blood pressure in young adulthood: the Barry Caerphilly Growth Study. Hypertension 52:638–644
Schedl A (2007) Renal abnormalities and their developmental origin. Nat Rev Genet 8:791–802
Acknowledgments
This study was supported by a grant from the Deutsche Forschungsgemeinschaft, Bonn, Germany; Sonderforschungsbereich 423. The authors report no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dötsch, J., Plank, C., Amann, K. et al. The implications of fetal programming of glomerular number and renal function. J Mol Med 87, 841–848 (2009). https://doi.org/10.1007/s00109-009-0507-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-009-0507-7