Abstract
Human type B synoviocytes are involved in joint injury during rheumatic diseases by producing inflammatory mediators such as interleukin-6 (IL-6). The increased level of purine and pirimidine nucleotides in the synovial fluid of rheumatoid arthritis (RA) patients could activate the large family of P2 receptors. Thus, we investigated the presence of P2 receptors in human type B synoviocytes from rheumatoid joints, also evaluating whether the P2X7 receptor is involved in IL-6 release. Reverse transcriptase polymerase chain reaction analysis revealed messenger ribonucleic acid (mRNA) expression for the P2X1, P2X2, P2X4, P2X5, P2X6, P2X7, P2Y1, P2Y4, P2Y11, P2Y12, P2Y13, and P2Y14 but not the P2X3, P2Y2, and P2Y6 receptors. The expression of the P2X7 receptor was confirmed by Western blot analysis. Adenosine triphosphate (ATP) and the P2X7 receptor agonist 2′-3′-O-(4-benzoylbenzoyl)ATP (BzATP) triggered an increase in intracellular calcium, thereby suggesting the expression of functional P2 receptors, including the P2X7 receptor. Moreover, BzATP treatment upregulated both IL-6 mRNA and protein expression. Synoviocytes spontaneously released low quantities of IL-6; the incubation with BzATP induced the release of larger amounts of the cytokine, and such a release was blunted by the P2X7 antagonist oxidized ATP. The selective P2X1 and P2X3 receptor agonist α,β-methylene ATP did not affect IL-6 release. Finally, BzATP failed to induce a significant uptake of the large-molecule YO-PRO, thus suggesting the lack of pore formation after P2X7 receptor stimulation. In conclusion, among the different P2 receptors expressed on human RA type B synoviocytes, the P2X7 receptor may modulate IL-6 release but not inducing changes in cell membrane permeability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Activated synovial fibroblasts (type B synoviocytes) are actively involved in the development of cartilage damage in chronic inflammatory joint diseases, particularly rheumatoid arthritis (RA) [1]. Their ability to induce and perpetuate inflammation is associated with the production of proinflammatory cytokines, such as interleukin (IL)-6, IL-8, and tumor necrosis factor α (TNFα) [2–4]. The extensive tissue damage in inflammatory processes may lead to the occurrence of high levels of purine and pirimidine nucleotides at the sites involved; accordingly, it is well-documented that adenosine triphosphate (ATP) is often found in the synovial fluid of patients with RA [5]. Extracellular ATP and other nucleotides act through specific cell surface receptors known as P2 purinergic receptors [6] and can regulate a variety of cellular responses in many cell types and tissues [7–9]. On the basis of pharmacological, functional, and cloning data, two P2 receptor subfamilies have been described: P2Y and P2X [6, 10]. At the moment, seven members of the human P2X receptor family (P2X1, P2X2, P2X3, P2X4, P2X5, P2X6, P2X7) and eight of the human P2Y receptor family (P2Y1, P2Y2, P2Y4, P2Y6, P2Y11, P2Y12, P2Y13, P2Y14) have been found expressed and cloned [10, 11].
P2Y receptors are membrane spanning, G-protein-coupled receptors. Their activation triggers the release of Ca2+ from intracellular stores. P2X receptors are ligand-gated ionotropic channels, and their activation is associated with fast Na+ entry and K+ release inducing plasma membrane depolarization and consequent cytosolic Ca2+ increase [12, 13]. An interesting member of the P2X subfamily is the P2X7 receptor (P2X7R), which has been demonstrated to be expressed on inflammatory cells (e.g., monocytes/macrophages, dendritic cells) [14–17] and human primary fibroblasts, coupled to ion fluxes, microvescicle formation, and IL-6 release [18].
The aim of the present paper was to investigate P2X and P2Y purinergic receptor expression in human fibroblast-like type B synoviocytes from RA patients. The study was mainly focused at the P2X7R expression and function in terms of intracellular Ca2+ changes and IL-6 release.
Materials and methods
Cell isolation and culture
Synovial fibroblasts were isolated from synovial biopsies obtained for diagnostic purposes from ten RA patients, after obtaining their informed consent according to the principles of the Declaration of Helsinki. Synovial tissue was minced in small pieces and digested for 3 h at 37°C in 5% CO2 in Dulbecco’s Modified Eagle Medium (DMEM; Celbio, Milan, Italy), containing collagenase type I 233 U/ml (Sigma-Aldrich, Milan, Italy). Short-term in vitro adherence (overnight) was performed to remove nonadherent cells. Cell suspension was cultured in DMEM supplemented with heat-inactivated fetal bovine serum 10% (FBS), 100 U/ml penicillin, 100 μg/ml streptomycin, 2 mM glutamine (all from Celbio). HEK293 cells stably transfected with full-length human P2X7 receptor (P2X7-HEK293 cells), and HEK293 cells stably transfected with the empty vector (HEK293-mock cells) were cultured in DMEM-F12 (Celbio). Media were complemented with 10% heat-inactivated FBS, 100 U/ml penicillin, 100 μg/ml streptomycin, and 2 mM glutamine in the presence of 0.8 mg/ml G418 (Invitrogen Life Technologies, Carlsbad, CA, USA). Cells were incubated at 37°C in a humidified incubator in the presence of 5% CO2.
Flow cytometry
Purity and phenotype of the isolated synovial fibroblasts were characterized by flow cytometry as reported by Hirth et al. [4] and Zimmermann et al. [19] with the mouse monoclonal fibroblast antibody mAb AS02 (Calbiochem, San Diego, CA, USA) recognizing the human surface antigen CD90/Thy-1 [20]. The mouse monoclonal antibody CD14 (BD Pharmigen, Milan, Italy) was used to study the presence of macrophages [21]. Cells (3 × 105) were stained with saturating amounts of monoclonal antibody CD90/Thy-1 and CD14 conjugated with fluorescein isothiocyanate fluorochrome in phosphate-buffered saline (PBS), 1% FBS, and 2 mM ethylenediamine tetraacetic acid (EDTA) for 30 min at 4°C. Cells were analyzed with the FACS Calibur flow cytometer (Becton Dickinson, Franklin Lakes, NJ, USA) with Cell Quest software. Forward- and side-scatter gates were set to include all viable cells, and 10,000 events were acquired for each condition.
Reverse transcriptase polymerase chain reaction
Total ribonucleic acid (RNA) from synoviocytes was extracted using RNeasy Mini kit (Qiagen, Milan, Italy) and treated with DNase (Invitrogen Life Technologies). The RNA pellet was dissolved in H2O, and the optical density at 260 nm was determined in a spectrophotometer (Becton Dickinson). For first-strand deoxyribonucleic acid (DNA) synthesis, 1 μg of total RNA was converted to complementary DNA (cDNA) by incubation with Maloney murine leukemia virus reverse transcriptase (200 U/μl per sample), oligo(dT) primers (0.5 μg/μl per sample), and deoxyribonucleotide triphosphate (dNTPs; 10 mM; all Invitrogen Life Technologies) in 20 μl total volume. cDNA was amplified in a 50-μl reaction mixture containing EuroTaq DNA polymerase (1.25 U per sample; Euroclone S.p.A., Pero, Italy), MgCl2 (5 mM), dNTPs (0.25 mM), and 20 pmol of each sense and antisense primer for human purinergic receptors (P2X1, P2X2, P2X3, P2X4, P2X5, P2X6, P2X7, P2Y1, P2Y2, P2Y4, P2Y6, P2Y11, P2Y12, P2Y13, P2Y14; Table 1). The presence of a single band amplified with specific primers for β-actin (sense 5′-GGATCTTCATGAGGTAGTCAGTC-3′; antisense 5′-CCTGCCTTTGCCGATCC-3′) with the same cDNA was used as the internal control. Polymerase chain reaction (PCR) was performed using a minicycler PT-100 (MJ Research, Ramsey, MN, USA) for 35–40 cycles. PCR products were electrophoresed on a 2% agarose gel and stained with ethidium bromide, and bands were visualized and photographed by ultraviolet transillumination.
Western blot
Cells at approximately 80% confluency were harvested by trypsinization. Cell pellets were washed twice with cold PBS and lysed for 20 min at 4°C in a lysis buffer containing 20 mM Tris–HCl (pH 8.0), 150 mM NaCl, 1% Triton-X100, and inhibitor cocktail (104 mM 4-(2-aminoethyl)benzenesulfonyl fluoride hydrochloride, 0.08 mM aprotinin, 2.1 mM leupeptin, 3.6 mM bestatin, 15 mM pepstatin A, 1.4 mM E-64; all Sigma-Aldrich). The detergent insoluble material was removed by centrifugation at 14,000 rpm for 20 min. The supernatant was collected and used for protein quantification according to the Bradford method [22]. Proteins were separated on 4–10% Bis–Tris gel (Invitrogen Life Technologies) at 200 V for 45 min and blotted on nitrocellulose paper (Bio-Rad Laboratories, Milan, Italy) at room temperature at 170 mA for 1 h. The nitrocellulose membrane was blocked with 10% nonfat dry milk in blocking buffer Tris-buffered saline (1.5 M NaCl; 500 mM Tris–HCl; pH 7.4) with 0.05% Tween-20 for 1 h at room temperature and then incubated with primary rabbit polyclonal antibody anti-human P2X7 (1:200; Alomone Labs, Jerusalem, Israel). The antibody was raised against synthetic peptide corresponding to the last 20 amino acids of the P2X7 protein (KIRK EFPKT QGQYS GFKYP Y; accession Q64663). Blots were then incubated for 1 h at room temperature with goat anti-rabbit antibody coupled to horseradish peroxidase (HRP; 1:10,000; Jackson ImmunoResearch Laboratories Europe, Newmarket, UK) in blocking buffer. After washing, the specific proteins were visualized by the Opti-4CN Substrate kit (BioRad Laboratories, Milan, Italy), according the manufacturer’s instructions.
Cytoplasmic free Ca2+ concentration ([Ca2+]i) measurements
Cells (5 × 105) were loaded with the cell-permeant fluorescent calcium dye Fura-2 acetoxymethyl ester (AM; 3 μM; Molecular Probes, Invitrogen, Carlsbad, CA, USA) for 30 min at 37°C [23]. After loading, the cells were kept at room temperature in a medium containing 140 mM NaCl, 5.4 mM KCl, 1 mM MgCl2, 1 mM CaCl2, 15 mM 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES) buffer (pH 7.4) plus 1% BSA. Just prior to the experiment, a 1-ml aliquot of the cell suspension was rapidly centrifuged and resuspended in fresh medium. For experiments performed in the absence of extracellular calcium, the medium contained 0.2 mM ethylene glycol tetraacetic acid (EGTA) with no added Ca2+. Fluorescence was measured with a Varian Cary Eclipse fluorescence spectrophotometer (Palo Alto, CA, USA; excitation wavelengths 340 and 380 nm, emission 510 nm) equipped with magnetic stirring and temperature control, and the images were acquired using digital imaging techniques. To minimize leakage of trapped Fura-2, the assay temperature was 30°C, and 200 μM sulfinpyrazone was included in the medium [24]. Cells were stimulated with 500 μM, 1 mM ATP, and 100–500 μM 2′-3′-O-(4-benzoylbenzoyl)ATP (BzATP; all from Sigma-Aldrich) both in the presence and the absence of extracellular calcium. At the end of each incubation, 50 μg/ml digitonin and 20 mM EGTA were added to measure maximal (R max) and minimal (R min) fluorescence ratio (340/380) values, respectively. For single cell [Ca2+]i measurement experiments, synoviocytes were plated on glass coverslips (13 mm diameter) at the density of 3 × 104 per well in DMEM 10% FBS. When semiconfluence was reached, cells were loaded with 3 μM Fura-2 AM. Calcium measurements were carried out at room temperature. Fura-2-loaded cells were placed on a fluorescence image microscope and perfused with the medium in the presence of ATP, BzATP, or 100 μM α,β-methylene ATP (α,βMeATP) or 1 μM 1-[N,O-bis(5-isoquinoline sulfonyl)-N-methyl-l-tyrosyl] 4 phenylpiperazine (KN62; all from Sigma-Aldrich). The digital fluorescence-imaging microscopy system was mounted on a Nikon Diaphot 300 (Nikon, Tokyo, Japan) inverted microscope. Fluorescence images were collected through a Nikon oil immersion 40 × 13 numerical aperture objective and acquired by a cooled charge-coupled device (CCD) camera (Photometrics, Roper Scientific, USA) and a MetaMorph imaging system (Universal Imaging, Downingtown, PA, USA).
IL-6 release
Sandwich enzyme-linked immunosorbent assay (ELISA) protocol was used to assay for IL-6 in the extracellular media samples. Synoviocytes were cultured at 3 × 104 cells per well in 24-well plates and stimulated in duplicate with 0.1 ng/ml IL-1β, 100 and 500 μM BzATP, 300 μM oxidized ATP (oATP), 100 μM α,βMeATP, 10 U/ml apyrase, 1 μg/ml lipopolysaccharide (LPS; all from Sigma-Aldrich). In the experiments with oATP, cells were pretreated with the antagonist for 3 h before stimulation with BzATP. Apyrase is an ATP-degrading enzyme that was used in combination with α,βMeATP. In the studies where the agonists were incubated in the presence of LPS, cells were pretreated with the endotoxin for 2 h at 37°C. IL-1β was used as a positive control because it has been shown to be a potent inducer of IL-6 synthesis [25]. Times of stimulation are reported in each figure.
At confluency, the medium was changed to DMEM with 2% FBS 24 h before experiments to reduce background activation of cells. Flat-bottom 96-well plates were coated with rat anti-human IL-6 (0.5 mg/ml; BD Pharmigen) in binding solution (0.1 M Na2HPO4, pH 9.0) and blocked 2 h with PBS 10% FBS. The sample of 100 μl per well was applied and incubated for 4 h at room temperature. Wells were washed and incubated with biotinylated rat anti-human IL-6 (0.5 mg/ml) for 1 h at room temperature. The capture immune complexes were further incubated with streptavidin HRP (30 min; Vector Laboratories, Peterborough, UK), and colorimetrically developed with 2,2′-azino-bis-3-ethylbenzthiazoline-6-sulfonic acid (Sigma-Aldrich) substrate solution. The level of the colored product generated by the bound, enzyme-linked detection reagents was measured spectrophotometrically using an ELISA plate reader (Microplate 50 Pc, BioRad Laboratories) at 405 nm. Human recombinant IL-6 served as a positive control (BD Pharmigen) to construct the standard curve.
Cytotoxicity assay
Synoviocytes were plated in 24-well plates (3 × 104 cells per well) and incubated with 0.5 and 1 mM ATP, 100 and 500 μM BzATP, and 100 μM α,βMeATP for 30 min, 1, 3, 6, and 24 h at 37°C in a humidified atmosphere of 95% air and 5% CO2. Samples of 3 × 50 μl of the cell culture medium were collected from each well and assayed for lactate dehydrogenase (LDH) activity with the colorimetric CytoTox 96 Non-Radioactive Cytotoxicity Assay (Promega, Madison, WI, USA). Absorbance was measured in a spectrophotometer at a wavelength of 490 nm. As a positive control, cell cultures were treated with lysis solution (1% Triton X-100, Sigma-Aldrich), and the absorbance of these samples was considered as 100% of lactic dehydrogenase release. Cell death was expressed as percent of cytotoxicity using the formula:
Changes in plasma membrane permeability
Fluorescence microscopy
The increase in plasma membrane permeability was measured with the extracellular fluorescent tracer YO-PRO. Synoviocytes were grown on coverslips (13 mm diameter) at a density of 3 × 104 cells per well in DMEM 10% FBS; P2X7-HEK293 cells and HEK293-mock cells were plated at a density of 2 × 105 cells per well in DMEM-F12 10% FBS. Cells were pretreated for 30 min with 500 μM BzATP at 37°C, and YO-PRO was added during the last 5 min at 1 μM concentration. The cells were washed and resuspended in low divalent solution containing 147 mM NaCl, 2 mM KCl, 12 mM glucose, and 10 mM HEPES (pH = 7.3) without Ca2+ and Mg2+ ions, which have been shown to inhibit pore formation [26]. Cells were then placed on a coverslip and immediately observed with a fluorescence microscope mounted on a Nikon Diaphot 300 inverted microscope. The images were acquired with a cooled CCD camera and a MetaMorph imaging system.
Flow cytometry
Flow cytometry was used to study YO-PRO uptake by the detection of the shift in fluorescence intensity. P2X7-HEK293 and HEK293-mock cells and synoviocytes were suspended in PBS without Ca2+ and Mg2+, 2 mM EDTA, and 0.5% BSA. One micromolar YO-PRO was added, and the cells were treated with 500 μM BzATP for 5 min at 37°C [27]. After incubation, cells were washed twice and analyzed by flow cytometry.
Statistical analysis
Data were expressed as mean ± standard error of the mean (SEM). Statistical analysis was performed by the one-way analysis of variance and the Tukey–Kramer multiple comparison test to evaluate significant differences among groups. The level of significance was set at P < 0.05.
Results
Characterization of primary culture synovial cells isolated from rheumatoid arthritis patients
Synovial cells were characterized by morphology and flow cytometry analysis. Cells isolated from synovia of RA patients showed to be a homogenous population as demonstrated by their fibroblast-like morphology. Under our experimental conditions, the primary culture of synovial cells maintained a spindle shape without any morphological alterations also culturing for several passages (Fig. 1a). The flow cytometry confirmed the population homogeneity by showing that a high percentage (93%) of cells cultured for two to six passages showed a positive surface staining for the fibroblast marker CD90/Thy-1. On the contrary, the average percentage of cells positively stained with CD14 (synovial macrophage marker) was less than 1% (Fig. 1b).
Phenotype analysis of RA synovial cells in primary culture. a Representative images of synovial cells in culture. Synoviocytes appear with a large, spindle-shaped and fibroblast-like morphology at different passages (A′. IIp; A″. IIIp; A″′. IVp; A″″. VIp). b FACS analysis of freshly isolated synoviocytes (n = 3 patients). Cells were labelled with fluorescent antibody to CD90/Thy-1 and CD14. Plots show isotype control IgG staining (upper and lower left panels) versus specific antibody staining (CD90 upper right panel; CD14 lower right panel). Greater than 90% of synoviocytes express CD90 antigen
Human synoviocytes express the mRNA for P2X and P2Y receptor subtypes
We used Reverse transcriptase PCR (RT-PCR) to investigate whether P2 receptor transcripts were expressed by the human type B synoviocytes. The RT-PCR analysis performed with primers specifically designed for the various cloned human P2X receptors revealed bands corresponding to P2X1, P2X2, P2X4, P2X5, P2X6, and P2X7 but not the P2X3 receptor (Fig. 2a). The presence of the P2X7R was also confirmed by Western blot analysis (Fig. 2c). P2X7R was identified by a major protein band of the predicted molecular weight (∼70–75 kDa), whose specificity was investigated by the use of P2X7-HEK293 cells as a positive control and HEK293-mock cells as a negative control. The protein detected in transfected HEK cells lysates was slightly larger than the P2X7R detected in human synoviocytes. The presence of alternative spliced P2X receptor isoforms, together with post-translational modifications, gives rise to potentially large variations in the size of detected proteins. RT-PCR analysis with primers specifically designed for the various cloned human P2Y receptors revealed that synoviocytes express messenger ribonucleic acid (mRNA) for the following P2Y receptors: P2Y1, P2Y4, P2Y11, P2Y12, P2Y13, and P2Y14, with the exception of the P2Y2 and P2Y6 receptors (Fig. 2b). The size of the cDNA fragments for each P2 receptor is reported in Table 1.
Expression of P2 receptors. a, b RT-PCR of P2X and P2Y receptors. Total cellular RNA isolated from synoviocytes was reverse transcripted. The resulting cDNA was amplified with primers specific for each indicated P2X and P2Y receptors subtypes, and the identification of the PCR-amplified products was made on the basis of their predicted size. c Western blotting determination of the P2X7R. Expression of the P2X7R was analyzed in synoviocytes, HEK293-mock, and P2X7-HEK293 cell lysates using a specific anti-P2X7R antibody
Stimulation with ATP and BzATP induces [Ca2+]i increases in human primary synoviocytes
Functional P2 receptors were evaluated by analyzing [Ca2+]i responses induced by the stimulation with ATP or agonists for specific purinergic receptor subtypes. In experiments on cell cultures, the application of 500 μM ATP did not induce calcium rise, while the stimulation with 1 mM ATP in a calcium-free medium resulted in a sharp and transient [Ca2+]i increase, rapidly decreasing to baseline, in a way supporting the idea of a mobilization from intracellular calcium stores. The readdition of extracellular calcium (1.7 mM) resulted in a second rise in [Ca2+]i, followed by a sustained plateau, putatively attributed to the extracellular calcium entry through ligand gated P2X receptors (Fig. 3a). The mean peak calcium response of synoviocytes, expressed as the ratio of fluorescence values (ΔF 340/380), when exposed to 1 mM ATP in Ca2+-free and 0.2 mM EGTA-containing saline solution, was 0.85 ± 0.02 (range 0.83–0.86), while in the presence of extracellular Ca2+, it was 0.53 ± 0.11 (range 0.44–0.74). To determine the specific role of the P2X receptor subtypes, experiments with the P2X7R agonist BzATP were performed. One hundred micromolars of BzATP induced no appreciable response, while 500 μM BzATP induced an increase in [Ca2+]i but only in the presence of extracellular calcium (Fig. 3b). In the absence of extracellular calcium, BzATP application was not able to induce any intracellular calcium modification (data not shown). In single-cell calcium measurements, the stimulation with ATP and BzATP confirmed the results obtained in cell cultures. ATP (1 mM) induced calcium mobilization both in the presence and in the absence of extracellular calcium, respectively, in 83.7 ± 7.02% and 63.1 ± 19% of the analyzed cells (n = 83), while 500 μM BzATP was effective in the presence of extracellular Ca2+, but only 23.17 ± 3.10% of the cells showed [Ca2+]i increase (n = 37; data not shown). In a total number of 20 cells, 1 μM KN62, a P2X7 antagonist, inhibited calcium mobilization following cell stimulation with either 500 μM BzATP or 1 mM ATP in the presence of extracellular calcium (data not shown).
Stimulation with ATP and BzATP induces [Ca2+]i increase in human primary synoviocytes. Representative images of [Ca2+]i changes in the presence of 1 mM ATP, 500 μM BzATP, and 100 μM α,βMeATP. Cells were loaded with the Ca2+ indicator fura-2/AM and stimulated with the agonists. For Ca2+-free conditions, cells were incubated in Ca2+-free, 0.2 mM EGTA-supplemented buffer. a In the absence of extracellular Ca2+, 1 mM ATP induces a rapid transient rise in [Ca2+]i, followed by a decrease to basal levels. The readdition of extracellular calcium resulted in a second rise followed by a sustained plateau. The experiments were performed with a fluorescence spectrophotometer. b Stimulation with 500 μM BzATP induces an increase in [Ca2+]i in the presence of extracellular Ca2+. The experiments were performed with a fluorescence spectrophotometer. c Single cell calcium experiments. The image is representative of the response of 20 cells of the same culture dish. No changes in [Ca2+]i have been detected in the presence of 100 μM α,βMeATP. Under each experimental condition, each trace is representative of similar results obtained from three distinct experiments. The arrow indicates the time when agonists and CaCl2 were added
In consideration of the fact that BzATP could partially act also on the P2X1 and P2X3 receptor subtypes, we also tested the effect of α,βMeATP, a relatively selective agonist for the P2X1 and P2X3 receptors [28], to rule out their possible involvement. The application of a high concentration of α,βMeATP (100 μM) did not result in any increase in [Ca2+]i in all of the analyzed cells (n = 20 cells; Fig. 3c).
BzATP enhances the IL-6 mRNA expression in human synoviocytes
To investigate the possible involvement of the P2X7R in IL-6 gene transcription, mRNA expression was examined in human synoviocytes after 100 and 500 μM BzATP stimulation. IL-6 mRNA expression was induced after 1-h stimulation and declined considerably at 3 h (Fig. 4).
BzATP upregulates the expression of IL-6 mRNA in human synoviocytes. a The image represents the time course of the effect of BzATP on IL-6 mRNA expression. Cells were incubated for 30 min, 1 h, 1 h and 30 min, and 3 h with 100 and 500 μM BzATP. Total RNA isolated from synoviocytes was subjected to reverse transcription, and the resulting cDNA was amplified with specific primers for human IL-6. IL-1β-stimulation was used as a positive control. M: Marker 100 bp; lane 1: untreated cells; lane 2: IL-1β stimulation; lane 3: BzATP 100 μM-treated synoviocytes; lane 4: BzATP 500 μM-treated synoviocytes. b Densitometric analysis at 1 h of stimulation with BzATP. Values (mean ± SEM of four different patients) are expressed as IL-6/β-actin ratio. Triple asterisk, P < 0.001 vs control (C, untreated cells), double asterisk, P < 0.01 vs control (C, untreated cells)
Detection of IL-6 release from human synoviocytes
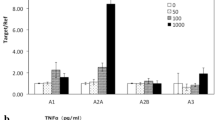
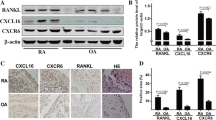
To determine whether the enhanced mRNA transcript was associated to an increase in IL-6 protein release, ELISA experiments following BzATP stimulation were conducted. Figure 5a shows that in the absence of a specific stimulus, IL-6 is measurable in the supernatants of resting synoviocytes showing that these cells spontaneously release a low amount of the cytokine in our experimental conditions. IL-6 release is substantially increased as a consequence of the stimulation with BzATP. The agonist caused a significant IL-6 production compared with untreated cells at both concentrations (100 and 500 μM), and the cytokine secretion reached the maximum level at 24 h of exposure to the agonist (Fig. 5a,b). This result was observed in 60% of experiments performed in duplicate with cells from ten RA patients. The release of IL-6 due to the stimulation with IL-1β (0.1 ng/ml; Boehringer-Mannheim, Germany) was considered as the positive control. To obtain more information on the possible role of the P2X7R in cytokine release, the inhibitory effect of oATP, a P2X7R antagonist [29], was tested. As shown in Fig. 6a, oATP produced an 83.5% reduction in the amount of IL-6 release induced by a 24-h stimulation with 100 and 500 μM BzATP. To further confirm the central role of the P2X7R in cytokine release, in the light of the fact that BzATP could partially act also on the P2X1 and P2X3 receptor subtypes, we tested α,βMeATP, which is typically considered a selective agonist for such receptors [28]. The application of the agonist (100 μM) in the presence or the absence of apyrase did not result in any significant increase in cytokine production compared to untreated cells (control) as shown in Fig. 6b. The addition of apyrase was employed to avoid desensitation of P2X1 and P2X3 receptors by endogenously released ATP. When synoviocytes were pretreated with 1 μg/ml LPS, BzATP induced a very significant IL-6 release in comparison to cells stimulated with LPS only (Fig. 7). All the cell cultures were responsive to BzATP after LPS priming.
Detection of IL-6 release. a Time course of the effect of 100 and 500 μM BzATP on IL-6 release. Cells were incubated for 3, 6, and 24 h. Supernatants were removed and assayed for IL-6 content by the ELISA technique. The release of IL-6 due to the stimulation with IL-1β (0.1 ng/ml) was measured as a positive control. Values are means ± SEM (n = 3). Double asterisk, P < 0.01 vs control (C, untreated cells). b Six additional experiments were performed by incubating synoviocytes with 100 and 500 μM BzATP for 24 h. double asterisk, P < 0.01 vs control (C, untreated cells)
Role of P2X7R in the BzATP-dependent release of IL-6. a Inhibitory effect of oATP on BzATP-induced IL-6 release in synoviocytes. Cells were pretreated with 300 μM oATP for 3 h before the addition of 100 and 500 μM BzATP. After a 24-h stimulation, the medium was collected and used for determining IL-6 concentration. Values are expressed as mean ± SEM (n = 3). Triple number sign, P < 0.001 vs control (C, untreated cells); double number sign, P < 0.01 vs control (C, untreated cells); double asterisk, P < 0.01 vs 100–500 μM BzATP. b α,βMeATP has no effect on IL-6 release. Synoviocytes were stimulated for 24 h with IL-1β as a positive control, 100 μM α,βMeATP, and 100 μM α,βMeATP with 10 U/ml apyrase, an ATP-degrading enzyme. Values are expressed as mean ± SEM (n = 3). Asterisk, P < 0.05 vs control (C, untreated cells)
Effect of BzATP on LPS-primed synoviocytes. Synoviocytes were stimulated with 1 μg/ml LPS and then treated with 100 and 500 μM BzATP for 24 h; the medium was collected and used for determination of IL-6 concentration. IL-1β-treated and untreated cells were used as controls. Data were collected from a minimum of four independent experiments and expressed as mean ± SEM. Asterisk, P < 0.05 vs control (C, untreated cells)
Measurement of LDH
The percentage of cytotoxicity from cultures treated up to 24 h with 100 and 500 μM BzATP (4.47 ± 0.32; 4.60 ± 1.10, respectively), 100 μM α,βMeATP (4.70 ± 0.10), and 0.1, 0.5, and 1 mM ATP (4.88 ± 0.62; 4.24 ± 0.85; 4.48 ± 0.11, respectively) did not differ significantly from untreated cells (control; 3.73 ± 0.67). Similar results were obtained at shorter incubation times (30 min, 1, 3, and 6 h; data not shown).
YO-PRO uptake
Synoviocytes isolated from five distinct patients, P2X7-HEK293 cells and HEK293-mock cells, were examined for permeability to YO-PRO in the presence of 500 μM BzATP. Most of the P2X7-HEK293 cells were positive for YO-PRO uptake when they were stimulated with 500 μM BzATP. As expected, fluorescence was localized in the nucleus; in fact, YO-PRO becomes fluorescent when it binds to nucleic acids. On the contrary, it was not possible to document any change in plasma membrane permeability in P2X7-HEK293 untreated and in HEK293-mock cells stimulated with 500 μM BzATP. In synoviocytes stimulated with the agonist, YO-PRO did not appear as intranuclear fluorescence, but there was a weak increase in cytosolic fluorescence similar to that observed in untreated synoviocytes, suggesting a pinocytosis phenomenon, as also confirmed by experiments performed at room temperature to reduce this effect. The same data were obtained measuring YO-PRO fluorescence by flow cytometry. The stimulation with 500 μM BzATP induced a shift in the fluorescence intensity spectrum of YO-PRO in P2X7-HEK293 cells (77.1% positive cells) but not in HEK293 mock cells (14.8% positive cells). On the contrary, under our experimental conditions, we did not observe any increase in uptake of YO-PRO in human synoviocytes stimulated with BzATP (12.4% positive cells; Fig. 8).
YO-PRO uptake in HEK293 cells and synoviocytes studied by fluorescence microscope. a Cells (2 × 105) were incubated in a medium containing YO-PRO in either the absence of stimuli (A, D) or the presence of BzATP (B, E and C, F). After 30 min, cells were rinsed and photographed using a ×40 objective. BzATP causes permeabilization of the plasma membrane in P2X7-HEK293 cells (B, E) but not in HEK293-mock (C, F). A–C, bright-field photographs of HEK293 cells; D–F, fluorescence images of HEK293 cells. b Synoviocytes (3 × 104) were incubated in a medium containing YO-PRO in the absence (A, C untreated cells), or the presence of BzATP (B, D). After 30 min, cells were rinsed and photographed using a ×40 objective. BzATP does not induce YO-PRO uptake by synoviocytes (B, D). A–B, bright-field photographs of synoviocytes; C–D, fluorescence images of synoviocytes
Discussion
In RA joints, type B synoviocytes grow aggressively and contribute to the tissue damage by producing several cytokines such as IL-1β, TNFα, interferon γ, and IL-6 [30]. The extensive cell injury in the affected joints leads to a significant increase in ATP (and other nucleotides) concentrations in the synovial fluid [5], probably contributing to the amplification of the inflammatory reaction. Indeed, it is increasingly appreciated that receptors for extracellular nucleotides have a central role in inflammation and immunomodulation [14, 31]. They are expressed by monocytes/macrophages, microglial cells, lymphocytes, and dendritic cells [14–17], and more recently, they have also been demonstrated in human primary fibroblast cultures [18]. Moreover, Loredo and Benton [31] have shown that ATP and uridine triphosphate are able to stimulate the mobilization of calcium from intracellular stores in synovial cells, possibly through the activation of a P2Y (formerly P2U) receptor.
In the present paper, by the RT-PCR technique, mRNA transcripts of numerous P2 receptors were detected in the pure fibroblast-like cell population namely, the P2X1, P2X2, P2X4, P2X5, P2X6, and P2X7, and P2Y1, P2Y4, P2Y11, P2Y12, P2Y13, P2Y14 receptors, with the exception of the P2X3, P2Y2, and P2Y6 receptors only. In the case of the P2X7R, the presence of the receptor protein was also demonstrated by Western blot analysis. In different cell types, the stimulation with agonists interacting with the purinergic receptor family leads to a rise in intracellular Ca2+ level either by the influx from the extracellular medium via cation channels (P2X receptors) or by the release from intracellular stores (P2Y receptors) [12]. In our experimental setting, the treatment of human synoviocytes with ATP, an agonist of some of both P2X and P2Y receptor subtypes, triggered a rapid increase in cytosolic Ca2+ both in the presence and in the absence of extracellular calcium, thus strongly suggesting that both P2 receptor subfamilies are functionally expressed in this cell type. To dissect the specific contribution of the various P2X receptors to the ATP-induced [Ca2+]i elevation, also stressing the possible role of the P2X7R, BzATP was employed as a pharmacological tool. Although there are no ligands showing absolute selectivity toward the P2X7R, the pharmacological phenotype of the receptor is relatively well established. Unlike other members of the P2 receptors, homomeric P2X7 receptors are activated by high concentrations of ATP and BzATP, the latter being at least 10–30-fold more potent than ATP at the P2X7R [32]. The specific focus on the P2X7R was due to the fact that the stimulation of such a receptor in inflammatory cells (e.g., monocytes/macrophages, microglial cells) has been shown to be associated with cell activation and cytokine release [9, 14, 18]. BzATP promoted [Ca2+]i increase in the presence of extracellular calcium as expected. However, since BzATP could activate P2X receptor subtypes other than the P2X7 namely, the P2X1 and the P2X3 (the latter subtype possibly not expressed in synoviocytes), the effect of the P2X1- and P2X3-selective agonist α,βMeATP was tested [28]. Since α,βMeATP failed to increase [Ca2+]i in synoviocytes, the conclusion could be reasonably drawn that the BzATP activity was mediated by the P2X7 receptor stimulation.
As mentioned before, synoviocytes are very efficient producers of some inflammatory cytokines, including IL-6 [30]. Under our experimental conditions, the incubation of synoviocytes with 100 and 500 μM BzATP in the presence of extracellular calcium resulted in the expression of IL-6 mRNA, which was maximal after 1 h and declined considerably after 2 h, thus strongly suggesting the direct involvement of the P2X7R activation in the upregulation of IL-6 gene transcription. Next, we wanted to test whether synoviocytes may release IL-6 to the culture medium in response to BzATP stimulation. Resting synoviocytes spontaneously release low amounts of the cytokine; IL-6 release was substantially increased following the stimulation with 100 and 500 μM BzATP with a maximal increase obtained after a 24-h incubation. However, such results were not obtained from all the samples tested. On the contrary, when synoviocytes were pretreated with LPS, the stimulation with BzATP was always able to induce the release of a large amount of IL-6 in the suspension medium. Accordingly, Solini and coworkers have shown that human primary fibroblasts were able to release IL-6 following ATP and BzATP stimulation after a preincubation period of 2 h with phorbol myristate acetate or LPS at the same concentration (1 μg/ml) used in the present study [18]. We would speculate that in our setting, synoviocytes, while releasing significant amounts of IL-6 when stimulated by BzATP alone, do keep a sort of priming as a consequence of the in vivo effect of the inflammatory milieu of the arthritic joint. The same phenomenon could account for IL-6 release from purified synoviocytes primed and exposed to low concentrations of endogenously released ATP. The role of the P2X7R activation by BzATP in IL-6 release was further confirmed by the inhibitory effect of the P2X7R antagonist oATP and by the null activity of the P2X1 and P2X3 receptor agonist α,βMeATP.
A very interesting datum of our study arises from the observation that the treatment of human synoviocytes with BzATP was associated neither to cell death nor to changes in membrane permeability. While in other cell types, including human fibroblasts, sustained stimulation of the P2X7R causes phenotypic changes, membrane permeabilization, and eventually cell death [33], we did not observe any significant cytotoxicity up to 24 h of exposure to BzATP, as demonstrated by the study of LDH release. In addition, prolonged incubation of cells with high ATP concentrations (0.5 and 1 mM) did not induce cell death. Indeed, in several cell types, P2X7R activation is associated with the opening of a large pore of more than 3 nm, which increases permeability to molecules up to 900 Da [34], thereby possibly leading to cell lysis and death [33]. Pore formation can be studied by measuring the ability of cells to take up the fluorescent dye YO-PRO, after exposure to a P2X7R agonist such as BzATP. We were not able to demonstrate YO-PRO uptake by human synoviocytes, while P2X7-transfected HEK293 showed clear evidence of plasma membrane permeabilization. In some tumor cells, the P2X7R has been demonstrated to be nonfunctional in terms of pore formation [35], as a possible expression of a survival strategy. RA synoviocytes are characterized by pronounced proliferating activity [1], thereby putatively sharing some characteristics with tumor cells. Thus, we could speculate that in RA synoviocytes, the P2X7R may have silenced cytotoxic activity, although being able to trigger calcium entry, IL-6 mRNA transcription, and IL-6 release.
Limitations of our study include: synoviocytes from healthy subjects were not evaluated; our data cannot rule out the presence and activity of some P2X and P2Y receptors other than the P2X7R in synoviocytes from patients affected by RA; commercially available anti-human P2X7R antibodies are only polyclonal, and this makes a clear understanding of the protein expression more difficult; there was no availability of an antibody suitable for FACS, thus we could not confirm the P2X7R expression also by flow cytometry.
In conclusion, despite the small number of patients enrolled, we can produce evidence for the first time that: (1) human synoviocytes express the mRNA for numerous P2 receptors, including the P2X7R whose receptor protein was also detected; (2) ATP stimulation is coupled to [Ca2+]i increase dependent on either extracellular calcium entry and intracellular calcium release, thereby producing evidence that both the P2Y and P2X subfamilies are functionally expressed; (3) stimulation with a P2X7R agonist induces the transcription of IL-6 mRNA and the release of the cytokine itself; (4) IL-6 release is not a consequence of cell death; (5) P2X7R stimulation does not cause pore formation in synoviocytes. P2 receptors may represent a pharmacological target for the therapeutic manipulation of the proinflammatory activity of synoviocytes in RA patients.
References
Pap T, Muller-Ladner U, Gay RE, Gay S (2000) Fibroblast biology. Role of synovial fibroblasts in the pathogenesis of rheumatoid arthritis. Arthritis Res 2:361–367
Guerne PA, Zuraw BL, Vaughan JH, Carson DA, Lotz M (1989) Synovium as a source of interleukin 6 in vitro. Contribution to local and systemic manifestations of arthritis. J Clin Invest 83:585–592
Hayashida K, Nanki T, Girschick H, Yavuz S, Ochi T, Lipsky PE (2001) Synovial stromal cells from rheumatoid arthritis patients attract monocytes by producing MCP-1 and IL-8. Arthritis Res 3:118–126
Hirth A, Shapenko A, Kinne RW, Emmrich F, Shultze-Koops H, Sack U (2002) Cytokine mRNA and protein expression in primary-culture and repeated-passage synovial fibroblasts from patients with rheumatoid arthritis. Arthritis Res 4:117–125
Ryan LM, Rachow JW, McCarty DJ (1991) Synovial fluid ATP: a potential substrate for the production of inorganic pyrophosphate. J Rheumatol 18:716–720
Di Virgilio F, Chiozzi P, Ferrari D, Falzoni S, Sanz JM, Morelli A, Torboli M, Bolognesi G, Baricordi OR (2001) Nucleotide receptors: an emerging family of regulatory molecules in blood cells. Blood 97:587–600
La Sala A, Ferrari D, Di Virgilio F, Idzko M, Norgauer J, Girolomoni G (2003) Alerting and tuning the immune response by extracellular nucleotides. J Leukoc Biol 73:339–343
Apasov S, Koshiba M, Redegeld F, Sitkovsky MV (1995) Role of extracellular ATP and P1 and P2 classes of purinergic receptors in T-cell development and cytotoxic T lymphocyte effector functions. Immunol Rev 146:5–19
Hide I, Tanaka M, Inoue A, Nakajima K, Kohsaka S, Inoue K, Nakata Y (2000) Extracellular ATP triggers tumor necrosis factor-alpha release from rat microglia. J Neurochem 75:965–972
Ralevic V, Burnstock G (1998) Receptors for purines and pyrimidines. Pharmacol Rev 50:413–492
Abbracchio MP, Burnstock G, Boeynaems JM, Barnard EA, Boyer JL, Kennedy C, Knight GE, Fumagalli M, Gachet C, Jacobson KA, Weisman GA (2006) International union of pharmacology LVIII: update on the P2Y G protein-coupled nucleotide receptors: from molecular mechanisms and pathophysiology to therapy. Pharmacol Rev 58:281–341
Dubyak GR, el-Moatassim C (1993) Signal transduction via P2-purinergic receptors for extracellular ATP and other nucleotides. Am J Physiol 265:C577–C606
Valera S, Hussy N, Evans RJ, Adami N, North RA, Surprenant A, Buell G (1994) A new class of ligand-gated ion channels defined by P2x receptor for extracellular ATP. Nature 371:516–519
Ferrari D, Chiozzi P, Falzoni S, Hanau S, Di Virgilio F (1987) Purinergic modulation of interleukin-1 beta release from microglial cells stimulated with bacterial endotoxin. J Exp Med 185:579–582
Gudipaty L, Humphreys BD, Buell G, Dubvak GR (2001) Regulation of P2X7 nucleotide receptor function in human monocytes by extracellular ions and receptor density. Am J Physiol Cell Physiol 280:C943–C953
Sluyter R, Barden JA, Wiley JS (2001) Detection of P2X purinergic receptors on human B lymphocytes. Cell Tissue Res 304:231–236
Mutini C, Falzoni S, Ferrari D, Chiozzi P, Morelli A, Baricordi OR, Collo G, Ricciardi-Castagnoli P, Di Virgilio F (1999) Mouse dendritic cells express the P2X7 purinergic receptor: characterization and possible participation in antigen presentation. J Immunol 163:1958–1965
Solini A, Chiozzi P, Morelli A, Fellin R, Di Virgilio F (1999) Human primary fibroblasts in vitro express a purinergic P2X7 receptor coupled to ion fluxes, microvesicle formation and IL-6 release. J Cell Sci 112:297–305
Zimmermann T, Kunisch E, Pfeiffer R, Hirth A, Stahl HD, Sack U, Laube A, Liesaus E, Roth A, Palombo-Kinne E, Emmrich F, Kinne RW (2001) Isolation and characterization of rheumatoid arthritis synovial fibroblasts from primary culture—primary culture cells markedly differ from fourth-passage cells. Arthritis Res 3:72–76
Saalbach A, Aneregg U, Bruns M, Schnabel E, Herrmann K, Haustein UF (1996) Novel fibroblast-specific monoclonal antibodies: properties and specificities. J Invest Dermatol 106:1314–1319
Mulherin D, Fitzgerald O, Bresnihan B (1996) Synovial tissue macrophage populations and articular damage in rheumatoid arthritis. Arthritis Rheum 39:115–124
Bradford MM (1976) A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 72:248–254
Di Virgilio F, Fasolato C, Steinberg TH (1988) Inhibitors of membrane transport system for organic anions block fura2 excretion from PC12 and N2A cells. Biochem J 256:959–963
Grynkiewicz G, Poenie M, Tsien RY (1985) A new generation of Ca2+ indicators with greatly improved fluorescence properties. J Biol Chem 260:3440–3450
Walther Z, May LT, Sehgal PB (1988) Transcriptional regulation of the interferon-beta 2/B cell differentiation factor BSF-2/hepatocyte-stimulating factor gene in human fibroblasts by other cytokines. J Immunol 140:974–977
Virginio C, Church D, North RA, Surprenant A (1997) Effect of divalent cations, protons and calmidazolium at the rat P2X7 receptor. Neuropharmacology 36:1285–1294
Pfeiffer Z, Aga M, Prabhu U, Watters JJ, Hall DJ, Bertics PJ (2004) The nucleotide receptor P2X7 mediates actin reorganization and membrane blebbing in RAW 264.7 macrophages via p38 MAP kinase and Rho. J Leukoc Biol 75:1173–1182
Khakh BS, Burnstock G, Kennedy C, King BF, North RA, Seguela P, Voigt M, Humphrey PP (2001) International union of pharmacology: XXIV, current status of the nomenclature and properties of P2X receptors and their subunits. Pharmacol Rev 53:107–118
Murgia M, Hanau S, Pizzo P, Rippa M, Di Virgilio F (1993) Oxidized ATP. An irreversible inhibitor of the macrophage purinergic P2Z receptor. J Biol Chem 268:8199–8203
Feldmann M, Brennan FM, Maini RN (1996) Rheumatoid arthritis. Cell 85:307–310
Loredo GA, Benton HP (1998) ATP and UTP activate calcium-mobilizing P2U-like receptors and act synergistically with interleukin-1 to stimulate prostaglandin E2 release from human rheumatoid synovial cells. Arthritis Rheum 41:246–255
Jacobson KA, Jarvis MF, Williams M (2002) Perspective: purine and pyrimidine. (P2) receptors as drug targets. J Med Chem 45:4057–4093
Schulze-Lohoff E, Hugo C, Rost S, Arnold S, Gruber A, Brune B, Sterzel RB (1998) Extracellular ATP causes apoptosis and necrosis of cultured mesangial cells via P2Z/P2X7 receptors. Am J Physiol 275:F962–F971
Rassendren F, Buell GN, Virginio C, Collo G, North RA, Surprenant A (1997) The permeabilizing ATP receptor, P2X7. Cloning and expression of a human cDNA. J Biol Chem 272:5482–5486
Slater M, Danieletto S, Gidley-Baird A, Teh LC, Barden JA (2004) Early prostate cancer detected using expression of non-functional cytolytic P2X7 receptors. Histopathology 44:206–215
Acknowledgments
P2X7-HEK293 and HEK293-mock cells were kindly provided by Prof. Francesco Di Virgilio (Ferrara University, Italy).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Caporali, F., Capecchi, P.L., Gamberucci, A. et al. Human rheumatoid synoviocytes express functional P2X7 receptors. J Mol Med 86, 937–949 (2008). https://doi.org/10.1007/s00109-008-0365-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-008-0365-8