Abstract
Initial attempts to inhibit renin in humans have faced numerous difficulties. Molecular modeling and X-ray crystallography of the active site of renin have led to the development of new orally active renin inhibitors such as aliskiren. Aliskiren has a low bioavailality (2.6% to 5%) compensated by its high potency to inhibit renin and a long plasma half-life (24 to 40 h), which makes it suitable for once-daily dosing. The once-daily administration of aliskiren to hypertensive patients lowers blood pressure as strongly as standard doses of established AT1 receptor blockers (losartan, valsartan, and irbesartan), angiotensin-converting enzyme inhibitors (ramipril and lisnopril), hydrochlorothiazide, or long-acting calcium channel blockers (amlodipine). In combination therapy, aliskiren further decreases blood pressure when combined with either hydrochlorothiazide, amlodipine, valsartan, irbesartan, or ramipril. However, the biochemical consequences of renin inhibition differ from those of angiotensin I-converting enzyme inhibition and angiotensin II antagonism, particularly in terms of angiotensin profiles and interactions with the bradykinin-NO-cGMP pathway. Blockade of the renin–angiotensin system with angiotensin I-converting enzyme inhibitors, AT1 receptor blockers, or a combination of these drugs has become one of the most successful therapeutic approaches in medicine. However, it remains unclear how to optimize renin–angiotensin system blockade to maximize cardiovascular and renal benefits. In this context, renin inhibition to render the renin–angiotensin system fully quiescent is a new possibility requiring further study. Preliminary results show that short-term administration of aliskiren has beneficial antialbuminuric effects in diabetic patients with chronic nephropathy and favorable neurohormonal effects in patients with chronic heart failure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renin is a logical target for renin angiotensin system (RAS) blockade because it corresponds to the first highly regulated and rate-limiting step of the system. Initial attempts to inhibit renin started over 30 years ago and were based on diverse strategies including the use of renin antibodies, peptide analogs of the prosegment of the renin precursor, statin-based peptides, and transition-state synthetic analogs [1–3]. However, the clinical development of first orally active transition-state synthetic analogs capable of inhibiting renin has faced a number of technical problems (specificity, potency, pharmacokinetic profile, development costs) for these drugs to be considered clinically useful [4–7]. Molecular modeling and determination of the X-ray crystallographic structure of the active site of renin have led to the identification of new renin inhibitors [1–3]. The first representative of this class of non-peptide drugs is aliskiren, an orally active, alkane carboxamide renin inhibitor with a very high binding affinity for renin, resulting in selectivity for this enzyme over other aspartyl proteases [8, 9]. Aliskiren is a highly hydrophilic transition-state mimetic [9]. It is a potent competitive renin inhibitor (IC50: 0.6 nM) that binds strongly to renin and is highly specific for human and primate renin [9]. Preclinical pharmacology and animal studies of aliskiren are reported elsewhere in the same issue of the journal by D. Müller. This review will focus on the clinical data available on aliskiren. Other direct renin inhibitors (DRIs) are currently being developed by Speedel, Actelion/MSD, Pfizer, and GSK, and some of them have already reached clinical development stages.
Aliskiren pharmacokinetics in humans
Plasma concentrations of aliskiren peak between 2 and 4 h after administration. The mean absolute bioavailability of the hard gelatin capsule containing 75 mg of the drug is 2.6%, and the absorbed fraction of radiolabeled aliskiren is ≈5% [10]. Food intake reduces C max by 85% and AUC0–∞ by 71% [11]. There is a high level of between-subjects variability in aliskiren pharmacokinetic parameters (40–70% for AUC and 30–50% for C max). The distribution volume after a 20 mg IV dose is high (135 L), indicating extensive tissue uptake [2]. Unchanged radiolabeled aliskiren is the principal circulating species in human plasma, accounting for 81% of total plasma radioactivity, with very low exposure to metabolites. Dose recovery over 168 h is nearly complete (91.5% of dose) [10]. Excretion of aliskiren occurs almost completely via the fecal route (90.9% corresponding to unabsorbed drug), with only 0.6% recovered in the urine [10]. Mean terminal half-life is reported to be 24 to 40 h [10, 12, 13], allowing once-daily dosing. Exposure to aliskiren increases following multiple once-daily administrations, with the steady state reached after approximately 7 days [12]. The pharmacokinetic differences between Blacks, Caucasians, and the Japanese are minimal [11]. There is a slight gender difference in aliskiren pharmacokinetics (AUC and C max are, respectively, 24% and 30% lower in healthy men than healthy women), which do not influence the antihypertensive effect (see below [14]). Exposure is increased in elderly patients (AUC and C max are increased by 57% and 28%, respectively) [15], but no adjustment in the starting dose is required if the patient is not sodium-depleted [14]. There is no significant effect on the single-dose pharmacokinetics of aliskiren by hepatic impairment [16]. There is a 65% increase in steady-state aliskiren exposure in patients with renal impairment compared to matched healthy subjects. The steady-state clearance of aliskiren in patients with renal impairment is 60–70% of the values for matched healthy subjects. This observed difference in aliskiren exposure may be explained by reduced efflux transporter P-glycoprotein (Pgp) activity due to renal insufficiency, aliskiren being a substrate of this transporter [17]. It is unlikely that the effect of renal impairment on aliskiren exposure necessitates any adjustment of the aliskiren dose [17]. No clinically significant pharmacokinetic interaction with lovastatin, atenolol, celecoxib, cimetidine [18], and warfarin has been reported [19]. Co-administration of irbesartan reduced aliskiren C max up to 50% after multiple dosing [17], but there was no significant pharmacokinetic interaction reported with amlodipine, valsartan, ramipril, and hydrochlorothiazide (HCTZ) [20]. Because aliskiren is a substrate of the Pgp transporter, the potential for drug interactions at the Pgp site depends on the degree of inhibition of this transporter. Co-administration of potent Pgp inhibitors such as atorvastatin (80 mg), ketoconazole (200 mg b.i.d.), or cyclosporine (200 and 600 mg) resulted in significant increases in aliskiren C max/AUC (atorvastatin: 50%/50%; ketoconazole: 80%/80%; cyclosporine: 250%/500%) [11]. Concomitant use of aliskiren with cyclosporine is not recommended. The next generation of DRIs will probably have different pharmacokinetic profiles, which may influence their pharmacodynamic effects.
Proof of concept pharmacodynamic studies in normotensive subjects
In normotensive healthy subjects on a 100 mmol/day sodium diet, aliskiren treatment for 8 days (40 to 640 mg in solution) inhibited plasma renin activity (PRA), suppressed the production of plasma angiotensin (Ang) I and Ang II, decreased plasma and urinary aldosterone concentrations, and increased plasma renin concentration (PRC) in a dose-dependent manner [12]. We also found that in mildly sodium-depleted normotensive subjects, the administration of 300 mg aliskiren increased PRC more strongly, and for much longer, decreased urinary aldosterone excretion for longer than 160 mg of the AT1 receptor blocker (ARB), valsartan, for a similar blood pressure (BP)-lowering effect [13]. The administration of 300 mg of aliskiren decreased PRA, Ang I, and Ang II levels for 48 h, whereas 160 mg of valsartan increased these levels. In the same study, we also showed that the RAS inhibition induced by valsartan was enhanced by the coadministration of aliskiren to inhibit renin activity [13]. For the combination treatment, 150 mg of aliskiren neutralized the valsartan-induced increase in plasma Ang I and II concentrations [13]. Similar results were obtained using higher doses of valsartan and aliskiren in sodium-replete subjects [21].
Phase II and III clinical studies in hypertensive patients
Two early phase II trials performed in patients with essential hypertension and predominantly low baseline PRA compared the BP-lowering effects and safety of aliskiren with losartan (100 mg o.d.) and irbesartan (150 mg o.d.). In the first trial, aliskiren (at doses of 75, 150, and 300 mg o.d.) and losartan (100 mg o.d.) gave similar results in terms of changes in ambulatory daytime systolic BP (SBP) at 4 weeks [22]. In the second trial, aliskiren (150, 300, 600 mg o.d.) significantly decreased trough diastolic BP at 8 weeks in a dose-dependent manner compared to placebo [23]. This trial also compared aliskiren with 150 mg o.d. irbesartan [23]: 150 mg o.d. aliskiren had a similar BP-lowering effect than 150 mg o.d. irbesartan, and doses of aliskiren >300 mg o.d. had a stronger antihypertensive effect than 150 mg o.d. irbesartan [23]. Aliskiren demonstrated similar efficacy in men and women, in patients aged ≥65 years vs. <65 years and in different ethnic populations [14].
A sustained 24-h BP-lowering effect on ambulatory BP monitoring was found in hypertensive patients after 8-week treatment with aliskiren (150, 300, 600 mg o.d.) [24]. The dose–response curve on BP was flat between 150 and 600 mg o.d., and trough to peak ratios were reported to be high (0.64, 0.98, 0.86 for aliskiren 150, 300, and 600 mg o.d., respectively) [24]. No rebound on withdrawal after an 8-week treatment was reported [24].
In comparison studies with other antihypertensive agents, aliskiren 150 or 300 mg o.d. was as effective as or more effective than hydrochlorothiazide (6.25, 12.5, 25 mg o.d.) [25], valsartan (160 to 320 mg o.d.) [26], irbesartan (150 mg o.d.) [23], losartan (100 mg o.d.) [22], ramipril (5 to 10 mg o.d.) [27], lisinopril (20–40 mg o.d.) [28], or amlodipine (5 to 10 mg o.d.) [29].
Combination therapies with aliskiren
In a factorial design trial in patients with hypertension, aliskiren (75, 150, 300 mg o.d.) and HCTZ (6.25, 12.5, 25 mg o.d.) in combination provided significant additional BP reductions compared to the respective component monotherapies with response rates >75% for combinations including 300 mg of aliskiren [25]. HCTZ monotherapy dose dependently increased in parallel both PRA and PRC in response to sodium depletion. In contrast, aliskiren monotherapy decreased PRA from baseline even though it increased dose dependently PRC in response to inhibition of Ang II production [30]. The aliskiren–HCTZ combination had a synergistic effect on renin release stimulation compared to the respective component monotherapies. Aliskiren in the combination neutralized the HCTZ-induced increase in PRA. Finally, the combination was well tolerated, with aliskiren reducing the incidence of HCTZ-induced mild hypokalemia [25].
An additive BP-lowering effect has also been reported when certain doses of aliskiren were combined with the calcium channel blocker, amlodipine [31], the ACE inhibitor, ramipril [32] or the ARB, valsartan [26, 33]. In a factorial design trial in patients with hypertension, aliskiren (75, 150, 300 mg o.d.) and valsartan (80, 160, 320 mg o.d.), in combination, decreased BP more strongly than the respective component monotherapies and almost as strongly as the combination of 160 mg o.d. of valsartan and 12.5 mg o.d. of HCTZ [26]. The results of this study were hampered by a large placebo effect. In another double-blind study including 1,797 patients with hypertension, Oparil et al. [33] have shown that the combination of maximum recommended doses of aliskiren (300 mg o.d.) and valsartan (320 mg o.d.) provided significantly greater reductions in BP than each component monotherapy. In terms of safety, the proportion of patients with a transient increase of serum potassium >5.5 mmol/L was higher in the combination group (4%) than in the aliskiren (2%) and valsartan monotherapy groups (2%) or in the placebo group (3%) [33].
The mechanism of additivity for the BP-lowering effect of the aliskiren/valsartan combination probably involves the mutual reinforcement of RAS suppression; the inhibition of renin with aliskiren neutralizes the compensatory increase in PRA and plasma Ang I and Ang II in response to ARBs such as valsartan, as shown in sodium-depleted and replete normotensive volunteers [13, 21]. The combination of two RAS inhibitors acting at different points in the system may also lead to a higher response rate for other pharmacokinetic or pharmacodynamic reasons [34]. The benefits of using combinations of RAS blockers for BP control only remains questionable at the present time for both efficacy and safety reasons [35–37]. Indeed, Stergiou et al. [38] have shown that a combination of an ARB with either a diuretic or calcium channel blocker is more effective than a combination of ARB with an ACE inhibitor to decrease BP in hypertensive patients. Dual RAS blockade with ACE inhibitors and ARBs is more effective in reducing proteinuria in patients with proteinuric nephropathy [39] and in reducing cardiovascular morbidity and mortality in patients with congestive heart failure [35] than single-site RAS blockade. Similarly, preliminary results show that (1) dual RAS blockade with aliskiren 300 mg o.d. and losartan 100 mg o.d. for 3 months has an additive antialbuminuric effect in hypertensive type 2 diabetic patients with nephropathy compared to losartan 100 mg o.d. alone [40] and (2) aliskiren 150 mg o.d. given for 3 months to patients with chronic heart failure already treated with ACE inhibitors (84%), ARBs (15%), beta-blockers (94%), or aldosterone antagonists (33%) induces additional and potentially beneficial neurohumoral effects [41]. These approaches still need additional longer term efficacy and safety evaluation.
Safety
Aliskiren is generally well tolerated in hypertensive patients with placebo-like tolerability profile [14]. Aliskiren produces dose-related diarrhea especially marked with the 600 mg dose (not on the market). Diarrhea was reported by 2.3% of patients at 300 mg compared to 1.2% in placebo patients [11, 14, 42]. Although aliskiren does not interfere with the bradykinin pathway contrary to ACE inhibitors (see below), very rare cases of angioedema associated with its use have been reported (incidence rate of 0.06%) [11]. Aliskiren use was also associated with a slight increase in cough in the placebo-controlled studies (aliskiren: 1.1% vs. placebo: 0.6%), but the rates of cough for aliskiren-treated patients were about one-third to one-half the rates in ACE inhibitors-treated patients [11]. Aliskiren is contraindicated during pregnancy [11]. Because of its pharmacokinetic and pharmacodynamic profile, aliskiren shares the same potential hazards of RAS inhibition, especially in situations in which BP and renal function are renin dependent: elderly or salt-depleted patients, patients receiving cyclo-oxygenase inhibitors, patients with renal artery stenosis, and patients placed under anesthesia. The incidence of hyperkalemia is increased especially in patients with diabetes and/or renal insufficiency or when aliskiren is given in combination with another RAS blocker [11, 33]. The risk of anemia may also be increased especially in patients with renal insufficiency, as reported with other RAS blockers [11]. A more complete and rigorous assessment of these risks is needed in the “real world” of clinical practice. This will require a careful post-marketing surveillance of large numbers of diverse patients with hypertension, renal insufficiency, diabetes, or congestive heart failure in whom the incidence of adverse effects may be higher than in selected patients included in clinical trials, as reported for aldosterone antagonists [43].
Aliskiren has been launched as an antihypertensive drug in the US in March 2007 and has been approved in Europe in August 2007. The appropriate dose of aliskiren for administration as monotherapy is between 150 and 300 mg o.d.
Differences between DRIs and other RAS blockers
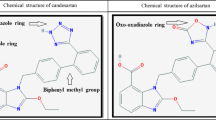
Several mechanisms contribute to the beneficial effects of RAS blockers in cardiovascular and renal therapy: the hemodynamic consequences of Ang II neutralization [44] and the suppression of the Ang II-dependent generation of growth-promoting cytokines, free oxygen radicals, and fibrosis mediators in tissues [45]. However, the various methods used to inhibit the RAS differ biochemically [2] (Fig. 1). As with ACE inhibitors and ARBs, the administration of a DRI increases circulating and intrarenal enzyme (renin) levels by interrupting the Ang II-renin negative feedback loop. However, with a DRI, the catalytic activity of the renin molecules newly released from the kidney is completely inhibited throughout the day, resulting in very low circulating levels of Ang I, Ang II, and other Ang I-derived peptides, thereby rendering the RAS quiescent. In contrast, the renin molecules newly released from the kidney remain enzymatically active after administration of an ARB or an ACE inhibitor, resulting in high circulating levels of Ang I, with much lower levels of Ang II. This counter-regulatory renin release could offset the pharmacological inhibition of the RAS at the end of each dosing interval when the amount of competitive inhibitor or antagonist on the enzyme (ACE) or receptor (AT1) is declining [35]. Given its high affinity for renin, its potency to inhibit renin, its very slow apparent dissociation rate from renin active site, and its long pharmacokinetic half-life, aliskiren should inhibit each new renin molecule released into the bloodstream or kidney. Sealey and Laragh [46] have suggested that the aliskiren-induced increase in PRC may limit its BP-lowering efficacy and confer a cardiovascular risk. This hypothesis has been extensively argued [47–49]. Finally, all these issues must take into account various difficult methodological problems concerning both PRC and PRA measurements, which occur in the presence of a DRI [47, 49].
Taking into account the very different angiotensin profiles achieved with the various single-site RAS blockers, the similarity and differences of acute and long-term BP reductions achieved with certain doses of aliskiren, ARBs, or ACE inhibitors in various clinical settings should improve our understanding of the role of increased Ang (1–7) [50, 51], Ang II type 2 (AT2) receptor stimulation [52], bradykinin-cyclic GMP-NO-mediated AT2 receptor stimulation [53], N-acetyl SDKP accumulation [54, 55] in addition to the hemodynamic effects of these drugs on peripheral vascular resistance, and large vessel compliance [56]. Finally, DRIs may provide additional protection over other RAS inhibitors by interfering with the enhanced catalytic activity of renin and prorenin after the binding of these molecules to the (pro)renin receptor [57]. In addition, if renin inhibitors not only block the enzymatic activity of renin in vivo but also change the conformation of prorenin both in vitro [58] and in vivo [59], then they may also modify renin metabolism [60] and binding to various receptors, including the (pro)renin receptor [57] or the mannose 6 phosphate receptor [61, 62]. These specific characteristics of DRIs may be potentially useful in patients with diabetes mellitus in whom prorenin levels are a powerful predictor of microvascular complications [63, 64] or if prorenin has a direct toxic effect [65].
At the present time, some of the properties of DRIs may have important clinical implications. DRIs induce a stronger renal vasodilator response than ACE inhibitors in sodium-restricted healthy subjects [66], and this was also reported for aliskiren [67]. In circumstances in which Ang II generation within the kidney is activated by pathways dependent on or independent of ACE, as in patients with diabetic nephropathy [68], or in African–American hypertensive patients on a high-salt diet [69], one would expect to see specific renal benefits of renin inhibition in renal tissue [70] following the administration of an orally active DRI. Interestingly, preliminary results of the Aliskiren in the Evaluation of Proteinuria in Diabetes (AVOID) study show that aliskiren 300 mg o.d. reduces urinary albumin-to-creatinine ratio by 20% (95% CI: 9–30%) compared to placebo after 3 months when added to losartan 100 mg o.d. [40]. Whether this approach will have a longer term additional nephroprotective and cardioprotective effect will be tested in the ALiskiren Trial In Type 2 Diabetes Using Cardio-Renal Disease Endpoints (ALTITUDE) trial.
Conclusion
It has taken 30 years to carry out and interpret large-scale mortality-morbidity studies with the different blockers of the RAS and to translate their results into practice. The dose dependency of their cardiovascular and renal benefits is especially evident when comparing the results of the HOPE [71], SECURE [72], and DIABHYCAR [73] trials carried out with daily doses of 1.25 to 10 mg ramipril. The use of ACE inhibitor/ARB combinations [35] or of ultrahigh doses of ARBs [74–76] has also been proposed as a means of maximizing the cardiovascular and renal benefits of RAS blockade. Another alternative is to block the effects of aldosterone [77]. These approaches are still under investigation [78]. Indeed, the results of ONTARGET will show whether adding telmisartan (80 mg o.d.) to ramipril (10 mg o.d.) in patients with high cardiovascular risk enhances the cardiovascular benefits achieved with each single-site RAS blocker given alone without generating more risk. It is still unknown whether aliskiren administered at a maximally tolerated daily dose of 300 mg o.d. can achieve “full” RAS inhibition similar to, or greater than, what can be obtained at lower doses by combining two RAS blockers acting at different sites. Such comparison studies will be needed if the combination of telmisartan (80 mg) and ramipril (10 mg) becomes the gold standard for RAS blockade after the results of ONTARGET are known.
Particular benefits for patients may also be discovered during the careful clinical use of aliskiren and the long-term morbidity and mortality trials and during the development of new DRIs. However, time and effort will be required as it is still necessary to investigate the differences between the effects of ACE inhibitors and ARBs [79].
References
Fisher ND, Hollenberg NK (2005) Renin inhibition: what are the therapeutic opportunities? J Am Soc Nephrol 16:592–599
Azizi M, Webb R, Nussberger J, Hollenberg NK (2006) Renin inhibition with aliskiren: where are we now, and where are we going? J Hypertens 24:243–256
Staessen JA, Li Y, Richart T (2006) Oral renin inhibitors. Lancet 368:1449–1456
de Gasparo M, Cumin F, Nussberger J, Guyenne TT, Wood JM, Menard J (1989) Pharmacological investigations of a new renin inhibitor in normal sodium-unrestricted volunteers. Br J Clin Pharmacol 27:587–596
van den Meiracker AH, Admiraal PJ, Man in’t Veld AJ, Derkx FH, Ritsema van Eck HJ, Mulder P, van Brummelen P, Schalekamp MA (1990) Prolonged blood pressure reduction by orally active renin inhibitor RO 42-5892 in essential hypertension. BMJ 301:205–210
MacFadyen RJ, Jones CR, Doig JK, Birnbock H, Reid JL (1995) Responses to an orally active renin inhibitor, remikiren (Ro 42-5892), after controlled salt depletion in humans. J Cardiovasc Pharmacol 25:347–353
Menard J, Boger RS, Moyse DM, Guyene TT, Glassman HN, Kleinert HD (1995) Dose-dependent effects of the renin inhibitor zankiren HCl after a single oral dose in mildly sodium-depleted normotensive subjects. Circulation 91:330–338
Rahuel J, Rasetti V, Maibaum J, Rueger H, Goschke R, Cohen NC, Stutz S, Cumin F, Fuhrer W, Wood JM, Grutter MG (2000) Structure-based drug design: the discovery of novel nonpeptide orally active inhibitors of human renin. Chem Biol 7:493–504
Wood JM, Maibaum J, Rahuel J, Grutter MG, Cohen NC, Rasetti V, Ruger H, Goschke R, Stutz S, Fuhrer W, Schilling W, Rigollier P, Yamaguchi Y, Cumin F, Baum HP, Schnell CR, Herold P, Mah R, Jensen C, O’Brien E, Stanton A, Bedigian MP (2003) Structure-based design of aliskiren, a novel orally effective renin inhibitor. Biochem Biophys Res Commun 308:698–705
Waldmeier F, Glaenzel U, Wirz B, Oberer L, Schmid D, Seiberling M, Valencia J, Riviere GJ, End P, Vaidyanathan S (2007) Absorption, distribution, metabolism, and elimination of the direct renin inhibitor aliskiren in healthy volunteers. Drug Metab Dispos 35:1418–1428
(Tekturna, tablets) a (2007) US prescribing information. Novartis Pharmaceutical Corporation, East Hanover (NJ)
Nussberger J, Wuerzner G, Jensen C, Brunner HR (2002) Angiotensin II suppression in humans by the orally active renin inhibitor Aliskiren (SPP100): comparison with enalapril. Hypertension 39:E1–E8
Azizi M, Menard J, Bissery A, Guyenne TT, Bura-Riviere A, Vaidyanathan S, Camisasca RP (2004) Pharmacologic demonstration of the synergistic effects of a combination of the renin inhibitor aliskiren and the AT1 receptor antagonist valsartan on the angiotensin II–renin feedback interruption. J Am Soc Nephrol 15:3126–3133
Weir MR, Bush C, Anderson MR, Zhang J, Keefe DL, Satlin A (2007) Antihypertensive efficacy, safety, and tolerability of the oral direct renin inhibitor aliskiren in patients with hypertension: a pooled analysis. J Am Soc Hypertens 1:264–277
Vaidyanathan S, Reynolds C, Yeh CM, Bizot MN, Dieterich HA, Howard D, Dole WP (2007) Pharmacokinetics, safety, and tolerability of the novel oral direct renin inhibitor aliskiren in elderly healthy subjects. J Clin Pharmacol 47:453–460
Vaidyanathan S, Warren V, Yeh C, Bizot MN, Dieterich HA, Dole WP (2007) Pharmacokinetics, safety, and tolerability of the oral renin inhibitor aliskiren in patients with hepatic impairment. J Clin Pharmacol 47:192–200
Vaidyanathan S, Bigler H, Yeh C, Bizot MN, Dieterich HA, Howard D, Dole WP (2007) Pharmacokinetics of the oral direct renin inhibitor aliskiren alone and in combination with irbesartan in renal impairment. Clin Pharmacokinet 46:661–675
Dieterle W, Corynen S, Vaidyanathan S, Mann J (2005) Pharmacokinetic interactions of the oral renin inhibitor aliskiren with lovastatin, atenolol, celecoxib and cimetidine. Int J Clin Pharmacol Ther 43:527–535
Dieterle W, Corynen S, Mann J (2004) Effect of the oral renin inhibitor aliskiren on the pharmacokinetics and pharmacodynamics of a single dose of warfarin in healthy subjects. Br J Clin Pharmacol 58:433–436
Vaidyanathan S, Valencia J, Kemp C, Zhao C, Yeh CM, Bizot MN, Denouel J, Dieterich HA, Dole WP (2006) Lack of pharmacokinetic interactions of aliskiren, a novel direct renin inhibitor for the treatment of hypertension, with the antihypertensives amlodipine, valsartan, hydrochlorothiazide (HCTZ) and ramipril in healthy volunteers. Int J Clin Pract 60:1343–1356
Azizi M, Menard J, Bissery A, Guyene TT, Bura-Riviere A (2007) Hormonal and hemodynamic effects of aliskiren and valsartan and their combination in sodium-replete normotensive individuals. Clin J Am Soc Nephrol 2:947–955
Stanton A, Jensen C, Nussberger J, O’Brien E (2003) Blood pressure lowering in essential hypertension with an oral renin inhibitor, aliskiren. Hypertension 42:1137–1143
Gradman AH, Schmieder RE, Lins RL, Chiang Y, Bedigian MP (2004) Aliskiren, a novel orally effective renin inhibitor, provides antihypertensive efficacy and placebo-like tolerability similar to an AT1-receptor blocker in hypertensive patients. Am J Hypertens 17:S108 (Abstract)
Oh BH, Mitchell J, Herron JR, Chung J, Khan M, Keefe DL (2007) Aliskiren, an oral renin inhibitor, provides dose-dependent efficacy and sustained 24-hour blood pressure control in patients with hypertension. J Am Coll Cardiol 49:1157–1163
Villamil A, Chrysant SG, Calhoun D, Schober B, Hsu H, Matrisciano-Dimichino L, Zhang J (2007) Renin inhibition with aliskiren provides additive antihypertensive efficacy when used in combination with hydrochlorothiazide. J Hypertens 25:217–226
Pool JL, Schmieder RE, Azizi M, Aldigier JC, Januszewicz A, Zidek W, Chiang Y, Satlin A (2007) Aliskiren, an orally effective renin inhibitor, provides antihypertensive efficacy alone and in combination with valsartan. Am J Hypertens 20:11–20
Uresin Y, Taylor A, Kilo C, Tschope D, Santonastaso M, Ibram G, Fang H, Satlin A (2006) Aliskiren, a novel renin inhibitor, has greater BP lowering than ramipril and additional BP lowering when combined with ramipril in patients with diabetes and hypertension. J Hypertens 24(Suppl 4):S82
Strasser RH, Puig JG, Farsang C, Croket M, Li J, van Ingen H (2007) A comparison of the tolerability of the direct renin inhibitor aliskiren and lisinopril in patients with severe hypertension. J Hum Hypertens 21:780–787
Jordan J, Engeli S, Boye SW, Le Breton S, Keefe DL (2007) Direct Renin inhibition with aliskiren in obese patients with arterial hypertension. Hypertension 49:1047–1055
Calhoun D, Chrysant S, Villamil A, Schober B, Hsu H, Prescott MF (2006) The novel renin inhibitor aliskiren decreases plasma renin activity (PRA) and neutralizes hydrochlorothiazide-induced RAAS activation in hypertensive patients. J Clin Hypertens 8(Suppl A):A77
Frampton JE, Curran MP (2007) Aliskiren: a review of its use in the management of hypertension. Drugs 67:1767–1792
O’Brien E, Barton J, Nussberger J, Mulcahy D, Jensen C, Dicker P, Stanton A (2007) Aliskiren reduces blood pressure and suppresses plasma renin activity in combination with a thiazide diuretic, an angiotensin-converting enzyme inhibitor, or an angiotensin receptor blocker. Hypertension 49:276–284
Oparil S, Yarows SA, Patel S, Fang H, Zhang J, Satlin A (2007) Efficacy and safety of combined use of aliskiren and valsartan in patients with hypertension: a randomised, double-blind trial. Lancet 370:221–229
Morgan T, Griffiths C, Delbridge L (2002) Low doses of angiotensin converting enzyme inhibitors and angiotensin type 1 blockers have a synergistic effect but high doses are less than additive. Am J Hypertens 15:1003–1005
Azizi M, Menard J (2004) Combined blockade of the renin–angiotensin system with angiotensin-converting enzyme inhibitors and angiotensin II type 1 receptor antagonists. Circulation 109:2492–2499
Doulton TW, He FJ, MacGregor GA (2005) Systematic review of combined angiotensin-converting enzyme inhibition and angiotensin receptor blockade in hypertension. Hypertension 45:880–886
Birkenhager WH, Staessen JA (2007) Dual inhibition of the renin system by aliskiren and valsartan. Lancet 370:195–196
Stergiou GS, Makris T, Papavasiliou M, Efstathiou S, Manolis A (2005) Comparison of antihypertensive effects of an angiotensin-converting enzyme inhibitor, a calcium antagonist and a diuretic in patients with hypertension not controlled by angiotensin receptor blocker monotherapy. J Hypertens 23:883–889
Kunz R, Friedrich C, Wolbers M, Mann JF (2008) Meta-analysis: effect of monotherapy and combination therapy with inhibitors of the renin angiotensin system on proteinuria in renal disease. Ann Intern Med 148:30–48
Parving HH, Lewis JB, Lewis EJ, Hollenberg NK (2007) Aliskiren in the evaluation of proteinuria in diabetes (AVOID). ASN Renal Week, San Francisco
Pitt B, McMurray JJ, Latini R, Maggioni A, Solomon SD, Smith BA, Bush CA, Prescott MA (2007) Neurohumoral effects of a new oral direct renin inhibitor in stable heart failure: the Aliskiren Observation Of Heart Failure Treatment Study (ALOFT). Circulation 116:II–549 (Abstract)
Gradman AH, Schmieder RE, Lins RL, Nussberger J, Chiang Y, Bedigian MP (2005) Aliskiren, a novel orally effective renin inhibitor, provides dose-dependent antihypertensive efficacy and placebo-like tolerability in hypertensive patients. Circulation 111:1012–1018
Juurlink DN, Mamdani MM, Lee DS, Kopp A, Austin PC, Laupacis A, Redelmeier DA (2004) Rates of hyperkalemia after publication of the Randomized Aldactone Evaluation Study. N Engl J Med 351:543–551
Gavras H, Biollaz J, Waeber B, Brunner HR, Gavras I, Davies RO (1981) Antihypertensive effect of the new oral angiotensin converting enzyme inhibitor “MK-421”. Lancet 2:543–547
Dzau VJ (2001) Theodore Cooper lecture: tissue angiotensin and pathobiology of vascular disease: a unifying hypothesis. Hypertension 37:1047–1052
Sealey JE, Laragh JH (2007) Aliskiren, the first renin inhibitor for treating hypertension: reactive renin secretion may limit its effectiveness. Am J Hypertens 20:587–597
Menard J, Azizi M (2007) The difficult conception, birth and delivery of a renin inhibitor: controversies around aliskiren. J Hypertens 25:1775–1782
Hollenberg NK (2007) A brief response to Sealey and Laragh. J Renin Angiotensin Aldosterone Syst 8:53
Campbell DJ (2008) Interpretation of plasma renin concentration in patients receiving aliskiren therapy. Hypertension 51:15–18
Reudelhuber TL (2006) A place in our hearts for the lowly angiotensin 1–7 peptide? Hypertension 47:811–815
Ferrario CM (2006) Angiotensin-converting enzyme 2 and angiotensin-(1–7): an evolving story in cardiovascular regulation. Hypertension 47:515–521
Zhao Y, Biermann T, Luther C, Unger T, Culman J, Gohlke P (2003) Contribution of bradykinin and nitric oxide to AT2 receptor-mediated differentiation in PC12 W cells. J Neurochem 85:759–767
Carey RM, Siragy HM (2003) Newly recognized components of the renin–angiotensin system: potential roles in cardiovascular and renal regulation. Endocr Rev 24:261–271
Azizi M, Rousseau A, Ezan E, Guyene TT, Michelet S, Grognet JM, Lenfant M, Corvol P, Ménard J (1996) Acute angiotensin-converting enzyme inhibition increases the plasma level of the natural stem-cell regulator N-Acetyl-Seryl-Aspartyl-Lysyl-Proline. J Clin Invest 97:839–844
Peng H, Carretero OA, Liao TD, Peterson EL, Rhaleb NE (2007) Role of N-acetyl-seryl-aspartyl-lysyl-proline in the antifibrotic and anti-inflammatory effects of the angiotensin-converting enzyme inhibitor captopril in hypertension. Hypertension 49:695–703
London GM, Pannier B, Guerin AP, Marchais SJ, Safar ME, Cuche JL (1994) Cardiac hypertrophy, aortic compliance, peripheral resistance, and wave reflection in end-stage renal disease. Comparative effects of ACE inhibition and calcium channel blockade. Circulation 90:2786–2796
Nguyen G, Delarue F, Burckle C, Bouzhir L, Giller T, Sraer JD (2002) Pivotal role of the renin/prorenin receptor in angiotensin II production and cellular responses to renin. J Clin Invest 109:1417–1427
Derkx FH, Deinum J, Lipovski M, Verhaar M, Fischli W, Schalekamp MA (1992) Nonproteolytic “activation” of prorenin by active site-directed renin inhibitors as demonstrated by renin-specific monoclonal antibody. J Biol Chem 267:22837–22842
Menard J, Guyene TT, Peyrard S, Azizi M (2006) Conformational changes in prorenin during renin inhibition in vitro and in vivo. J Hypertens 24:529–534
Stubbs AJ, Skinner SL (2004) Lectin chromatography of extrarenal renin protein in human plasma and tissues: potential endocrine function via the renin receptor. J Renin Angiotensin Aldosterone Syst 5:189–196
van Kesteren CA, Danser AH, Derkx FH, Dekkers DH, Lamers JM, Saxena PR, Schalekamp MA (1997) Mannose 6-phosphate receptor-mediated internalization and activation of prorenin by cardiac cells. Hypertension 30:1389–1396
Danser AH, Deinum J (2005) Renin, prorenin and the putative (pro)renin receptor. Hypertension 46:1069–1076
Luetscher JA, Kraemer FB, Wilson DM, Schwartz HC, Bryer-Ash M (1985) Increased plasma inactive renin in diabetes mellitus. A marker of microvascular complications. N Engl J Med 312:1412–1417
Deinum J, Ronn B, Mathiesen E, Derkx FH, Hop WC, Schalekamp MA (1999) Increase in serum prorenin precedes onset of microalbuminuria in patients with insulin-dependent diabetes mellitus. Diabetologia 42:1006–1010
Veniant M, Menard J, Bruneval P, Morley S, Gonzales MF, Mullins J (1996) Vascular damage without hypertension in transgenic rats expressing prorenin exclusively in the liver. J Clin Invest 98:1966–1970
Fisher ND, Hollenberg N (1995) Renal vascular responses to renin inhibition with zankiren in men. Clin Pharmacol Ther 57:342–348
Fisher ND, Hollenberg NK (2007) Unprecedented renal responses to direct blockade of the renin–angiotensin-system with aliskiren, a novel renin inhibitor. Circulation 116:II–556 (Abstract)
Price DA, Porter LE, Gordon M, Fisher ND, De’Oliveira JM, Laffel LM, Passan DR, Williams GH, Hollenberg NK (1999) The paradox of the low-renin state in diabetic nephropathy. J Am Soc Nephrol 10:2382–2391
Aviv A, Hollenberg NK, Weder AB (2004) Sodium glomerulopathy: tubuloglomerular feedback and renal injury in African Americans. Kidney Int 65:361–368
van Paassen P, de Zeeuw D, de Jong PE, Navis G (2000) Renin inhibition improves pressure natriuresis in essential hypertension. J Am Soc Nephrol 11:1813–1818
Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G (2000) Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med 342:145–153
Lonn E, Yusuf S, Dzavik V, Doris C, Yi Q, Smith S, Moore-Cox A, Bosch J, Riley W, Teo K (2001) Effects of ramipril and vitamin E on atherosclerosis: the study to evaluate carotid ultrasound changes in patients treated with ramipril and vitamin E (SECURE). Circulation 103:919–925
Marre M, Lievre M, Chatellier G, Mann JF, Passa P, Menard J (2004) Effects of low dose ramipril on cardiovascular and renal outcomes in patients with type 2 diabetes and raised excretion of urinary albumin: randomised, double blind, placebo controlled trial (the DIABHYCAR study). BMJ 328:495
Rossing K, Schjoedt KJ, Jensen BR, Boomsma F, Parving HH (2005) Enhanced renoprotective effects of ultrahigh doses of irbesartan in patients with type 2 diabetes and microalbuminuria. Kidney Int 68:1190–1198
Schmieder RE, Klingbeil AU, Fleischmann EH, Veelken R, Delles C (2005) Additional antiproteinuric effect of ultrahigh dose candesartan: a double-blind, randomized, prospective study. J Am Soc Nephrol 16:3038–3045
Hollenberg NK, Parving HH, Viberti G, Remuzzi G, Ritter S, Zelenkofske S, Kandra A, Daley WL, Rocha R (2007) Albuminuria response to very high-dose valsartan in type 2 diabetes mellitus. J Hypertens 25:1921–1926
Hollenberg NK (2004) Aldosterone in the development and progression of renal injury. Kidney Int 66:1–9
Yusuf S (2002) From the HOPE to the ONTARGET and the TRANSCEND studies: challenges in improving prognosis. Am J Cardiol 89:18A–25A
Turnbull F, Neal B, Pfeffer M, Kostis J, Algert C, Woodward M, Chalmers J, Zanchetti A, MacMahon S (2007) Blood pressure-dependent and independent effects of agents that inhibit the renin–angiotensin system. J Hypertens 25:951–958
Disclosure
Michel Azizi is a member of the “Renin Academy” sponsored by Novartis since 2004. He has received clinical research contracts between 1993 and 2007 from several pharmaceutical industries involved in research on the inhibition of the renin angiotensin aldosterone system to perform investigator-driven clinical studies of the RAS and the kallikrein–kinin system at the Clinical Investigation Center AP-HP/INSERM, George Pompidou European Hospital, Paris, France.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article has been retracted due to copyright issues that cannot be resolved.
An erratum to this article can be found at http://dx.doi.org/10.1007/s00109-011-0850-3
About this article
Cite this article
Azizi, M. RETRACTED ARTICLE: Direct renin inhibition: clinical pharmacology. J Mol Med 86, 647–654 (2008). https://doi.org/10.1007/s00109-008-0329-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-008-0329-z