Abstract
Gastric emptying regulates food intake. Oleoylethanolamide (OEA), an endogenous acylethanolamide chemically related to the endocannabinoid anandamide, inhibits food intake, but its effect on gastric emptying is unknown. Here, we investigated the effect and the role of OEA on gastric emptying in mice fed either a standard (STD) or a high-fat diet (HFD) for 14 weeks. Gastric emptying was reduced by OEA, but not by its saturated analog, palmitoylethanolamide. The effect of OEA was unaffected by rimonabant (cannabinoid CB1 receptor antagonist), SR144528 (cannabinoid CB2 receptor antagonist), 5′-iodoresiniferatoxin (transient receptor potential vanilloid type 1 antagonist), or MK886 (peroxisome proliferator-activated receptor-α) antagonist. Compared to STD mice, HFD mice showed delayed gastric emptying and higher levels of gastric OEA. HFD-induced increase in OEA levels was accompanied by increased expression of the OEA-synthesizing enzyme N-acyl-phosphatidylethanolamine-selective phospholipase D and decreased expression of the OEA-degrading enzyme fatty acid amide hydrolase. These results might suggest that elevation of gastric OEA could possibly contribute to the delayed gastric emptying observed in HFD-fed animals. HFD regulates OEA levels in the stomach through an increase of its biosynthesis and a decrease of its enzymatic degradation. The inhibitory effect of OEA on gastric emptying here observed might underlie part of the anorexic effects of this compound previously reported.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oleoylethanolamide (OEA) – the amide of oleic acid and ethanolamine – belongs to a family of animal and plant bioactive fatty acid amides, the ethanolamides, which also includes the endocannabinoid anandamide, i.e., the amide of arachidonic acid and ethanolamide [1, 2]. Like anandamide, OEA is produced by neurons and other cells through on-demand synthesis from a phospholipid precursor found within the membrane bilayer and is inactivated through enzymatic hydrolysis, suggesting that it may participate in cell-to-cell signaling processes [1–3]. However, in contrast to anandamide, OEA does not bind to or activate cannabinoid receptors and, hence, cannot be considered an endocannabinoid [1]. Pharmacological and molecular biological experiments have demonstrated that OEA induces satiation, reduces body weight gain (without causing visceral illness [4]) and stimulates fat utilization in rodents [5–10] through activation of the nuclear receptor peroxisome proliferator-activated receptor (PPAR)-α [6]. Transient receptor potential vanilloid type-1 receptors (TRPV1), which can also be activated by OEA [11], have also been suggested to mediate some of its anorectic effects [12].
There is a considerable interest in the role of OEA in the gut, mostly because experimental evidence suggests that this fatty-acid ethanolamide acts as a “satiety factor” in the upper part of the small intestine. Intestinal OEA levels in the gut may change in response to food intake. In rodents, food deprivation markedly reduces OEA levels in the small intestine; refeeding normalizes OEA levels [5, 6, 13, 14]. Moreover, OEA levels in the small intestine display diurnal fluctuations. They are higher during the daytime, when animals are satiated, and lower during the night, when they are awake and actively feeding [1]. Unlike classical satiety factors such as cholecystokinin, which are released into the bloodstream to terminate an ongoing meal, OEA may be produced from the small intestine and act within the gut to evoke satiation [1, 14]. There is also evidence that OEA may be involved in the regulation of fatty acid absorption in the gut. In the upper portion of the small intestine, OEA regulates the expression of genes encoding for proteins involved in intestinal lipid transport, including fatty acid translocase (FAT/CD36) and fatty acid transport protein 1 (FATP1) [6, 15]. Consistently, experimental evidence suggests that OEA increases fatty acid uptake in isolated enterocytes in vitro [15]. Finally, OEA levels in the blood of human individuals also change in relation to food consumption by being lowest after a meal inducing transient hyperglycemia and permanently elevated in type 2 diabetes patients with noncorrected hyperglycemia [2].
It is well known that gastric emptying plays an important role in regulating food intake and, hence, obesity [16–18]. Indeed, the inhibition of the gastric emptying of ingested nutrients represents an important brake against overfilling the gut [19]. However, the effect of OEA on gastric motility has been never reported to date. Because OEA inhibits food intake [1], including that in obese rodents [10, 20], in the present study we investigated the effect of this fatty acid ethanolamide on gastric emptying, both in control mice and in mice fed a high-fat diet (HFD) for 14 weeks, and analyzed the changes in its gastrointestinal levels following 8 and 14 weeks of HFD.
Materials and methods
Animals and diet
Male ICR mice (22–24 g) were generally used. Mice were fed ad libitum with standard mouse food, except for the 12-h period immediately preceding the measurement of gastric emptying. In another set of experiments, male 7-week-old C57Bl/6J mice were used. After 1 week acclimatization, C57Bl/6J mice were fed a diet containing 25.5% fat (49% of calories), 22% protein, and 38.4% carbohydrate (TD97366, Harlan Italy, Corezzana, Milan, Italy) for 14 weeks. Control C57B1/6J mice received standard diet (STD). Mice were fed ad libitum except for the 12-h period immediately preceding the experiments. Animals were purchased from Harlan Italy. Fasting plasma glucose levels were determined in 12-h fasted animals using the glucose test kit with an automatic analyzer (Accu-Chek® Active, Roche, Basel, Switzerland) in blood samples obtained from tail vein [21].
Principles of laboratory animal care (NIH publication No. 86–23, revised 1985) were followed. Moreover, all experiments complied with the Italian D.L. no. 116 of 27 January 1992 and associated guidelines in the European Communities Council Directive of 24 November 1986 (86/609/ECC).
Drug administration
OEA (1–15 mg/kg), palmitoylethanolamide (PEA) (1–15 mg/kg), WY14643 (6 mg/kg) or vehicles were given intraperitoneally (IP) 30 min before the administration of the marker (phenol red solution) used to evaluate gastric emptying. In some experiments, rimonabant (0.1 mg/kg), 5′-iodo-resiniferatoxin (I-RTX, 0.75 mg/kg), SR144528 (1 mg/kg) or the PPAR-α antagonist MK886 (6 mg/kg) were given IP 10 min before OEA (5 mg/kg). The timing of administration and the doses of the antagonists used in the present manuscript (i.e., rimonabant, SR144528, 5′-iodo-resiniferatoxin, and MK886) were selected on the basis of previous work [22–24]. In some experiments, the effect of IP-injected OEA (2–12 mg/kg) was evaluated in mice fed a HSD and, for comparison, in aged-matched mice fed a STD. Finally, OEA (5 mg/kg, IP) was also given at different times (0.5, 1, 2, 4, and 8 h) before the administration of phenol red solution.
Gastric emptying
Gastric emptying in both control and HFD-fed mice (14 weeks of dietary treatment) was performed as previously described [24, 25]. Briefly, after an overnight fast, the animals received by gavage 0.2 ml of a solution of 50 mg phenol red in 100 ml 1.5% carboxymethylcellulose, which was constantly stirred and held at 37°C. After 20 min, mice were euthanized and the stomach was quickly ligated at the lower esophageal sphincter and pyloric region and removed. The stomach was opened and its contents were poured into a test tube and washed with 4 ml distilled water. At the end of the experiment, 2 ml 1 M NaOH was added to each tube to develop the maximum intensity of color. The solutions were assayed with spectrometer at 560 nm. Percent gastric emptying was calculated according to the following formula:
Identification and quantification of OEA, PEA, anandamide, and 2-arachidonoylglycerol
Full-thickness stomachs and small intestines from HFD-fed mice and aged-matched mice fed a STD (8 and 14 weeks of dietary treatment) were removed and tissue specimens were immediately weighed, immersed into liquid nitrogen, and stored at −70°C until chromatographic separation of endocannabinoids. Tissues were extracted with chloroform/methanol (2:1, by volume) containing each 200 pmol of d4-OEA and d4-PEA, synthesized as described previously [26]. The lipid extracts were purified by silica column chromatography, carried out as described previously for anandamide [26], and the fractions containing OEA and PEA were analyzed by isotope dilution liquid chromatography–atmospheric pressure–chemical ionization mass spectrometry carried out in the selected monitoring mode as described for anandamide in detail elsewhere [27, 28]. Results were expressed as picomoles or nanomoles per gram of wet tissue.
In another set of experiments, we evaluated the gastric content of OEA, PEA, and the endocannabinoids anandamide and 2-arachidonoylglycerol (2-AG) in STD-fed mice treated with the fatty acid amide hydrolase (FAAH) inhibitor N-arachidonoylserotonin (AA-5-HT, 15 mg/kg IP, 30 min before killing the animals) [29]. Tissues were extracted with chloroform/methanol (2:1, by volume) containing each 200 pmol of d4-OEA and d4-PEA and 10 pmol each of d5-2-arachidonoylglycerol (d5-2-AG) and d8-anandamide, synthesized as described previously [26]. The extracts were then processed as described above.
Quantitative real-time PCR
Full-thickness stomachs (antrum plus fundus) from control and HFD mice were homogenized in 1 ml of Trizol® (Invitrogen, Carlsbad, CA, USA). Total RNA was extracted according to manufacturer recommendations, dissolved in RNA-storage-solution (Ambion, Foster City, CA, USA), UV-quantified by a Bio-Photometer® (Eppendorf, Hamburg, Germany), and stored to −80°C. RNA aliquots (6 μg) were digested by RNAse-free DNAse I (Ambion DNA-free™ kit) in a 20-μl final volume reaction mixture to remove contaminating genomic DNA. After DNAse digestion, concentration and purity of RNA samples were evaluated by the RNA-6000-Nano® microchip assay, using a 2100 Bioanalyzer® equipped with a 2100-Expert-Software® (Agilent, Santa Clara, CA, USA), following the manufacturer’s instructions. For all samples tested, the RNA integrity number was greater than 6 (relative to a 0–10 scale). Three micrograms of total RNA, as evaluated by the 2100 Bioanalyzer, was reverse transcribed in a 25-μl reaction mixture containing 50 mM Tris–HCl pH 8.3, 75 mM KCl, 3 mM MgCl2, 10 mM dithiothreitol, 1 mM dNTPs, 20 units of RNAse inhibitor (Invitrogen), 0.125 A260 units of hexanucleotide mixture (Invitrogen) for random priming, and 200 units of MoMuLV Superscript® III reverse transcriptase (Invitrogen). The reaction mixture was incubated in a termocycler iCycler-iQ® for a 5-min step at 55°C, followed by a rapid chilling for 2 min at 4°C. The protocol was stopped at this step and the MoMuLV reverse transcriptase was added to the samples, excepting the negative controls (-RT). The incubation was resumed by two thermal steps: 10 min at 20°C followed by 90 min at 50°C. Finally, the reaction was terminated by heating at 95°C for 10 min. Quantitative real-time PCR was performed by an iCycler-iQ® in a 25-μl reaction mixture containing 1× iQ-SYBR®-Green-Supermix (Bio-Rad, Hercules, CA, USA), 20 ng of cDNA (calculated on the basis of the retro-transcribed RNA), and 330 nM for each primer. The amplification profile consisted of an initial denaturation of 2 min at 94°C and 40 cycles of 30 s at 94°C, annealing for 30 s at TaOpt (optimum annealing temperature—see below), and elongation for 45 s at 68°C. Fluorescence data were collected during the elongation step. A final extension of 7 min was carried out at 72°C, followed by melt-curve data analysis. Optimized primers for SYBR®-Green analysis (and relative TaOpt) were designed by the Beacon-Designer® software 6.0 version (Biosoft International, Palo Alto, CA, USA) and were synthesized (HPLC-purification grade) by MWG-Biotech AG, Germany. Assays were performed in quadruplicate (maximum ΔCt of replicate samples <0.5), and a standard curve from consecutive fivefold dilutions (100 to 0.16 ng) of a cDNA pool representative of all samples was included for PCR-efficiency determination. Relative expression analysis, correct for PCR efficiency and normalized respect to reference genes β-actin and glyceraldehyde-3-phosphate dehydrogenase, was performed by GENEX software (Bio-Rad) for group-wise comparison and statistical analysis.
Drugs
OEA, PEA, 5′-iodoresiniferatoxin (I-RTX), WY14643 (4-Chloro-6-[(2,3-dimethylphenyl)amino]-2-pyrimidinyl)thioacetic acid, and MK866 (1H-Indole-2-propanoic acid)1-((4-chlorophenyl)methyl)-3-((1,1-dimethylethyl)thio)-alpha,alpha-dimethyl-5-(1-methylethyl)-3-(1-(4-chlorobenzyl)-3-t-butylthio-5-isopropylindol-2-yl)-2,2-dimethylpropanoic acid) where purchased from Tocris Cookson (Bristol, UK). Rimonabant (5-(p-chlorophenyl)-1-(2,4-dichlorophenyl)-4-methyl-N-piperidinopyrazole-3-carboxamide and SR144528 (N-[-1S-endo-1,3,3-trimethyl bicyclo [2.2.1] heptan-2-yl]-5-(4-chloro-3-methylphenyl)-1-(4-methylbenzyl)-pyrazole-3-carboxamide) were a kind gift from Drs. Madaleine Mossè and Francis Barth (SANOFI-Recherche, Montpellier, France). AA-5-HT was synthesized as described previously [29].
OEA, I-RTX, WY14643 and MK866 were dissolved in dimethylsulfoxide (DMSO), PEA in ethanol. For endocannabinoid and acylethanolamide measurements, AA-5-HT was dissolved in DMSO/Tween 80 (1:4) (4 μl/mouse). The drug vehicles (2 μl/10 g of DMSO, 2 μl/10 g of ethanol, 4 μl/mouse DMSO/Tween 80) had no significant effect on the responses under study.
Statistics
Data are expressed as the mean ± SEM of experiments in n mice. To determine statistical significance, Student’s t test was used for comparing a single treatment mean with a control mean, and a one-way analysis of variance followed by a Tukey–Kramer multiple comparisons test was used for analysis of multiple treatment means (or Bonferroni’s for endocannabinoids, OEA, and PEA levels). P values less than 0.05 were considered significant.
Results
Gastric emptying in control (STD-fed) mice
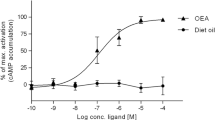
IP administration of OEA (1–15 mg/kg) produced a dose-dependent inhibition of gastric emptying (Fig. 1). A significant inhibitory effect was achieved starting from the 5-mg/kg dose. By contrast, PEA, at the same dose, did not affect significantly gastric emptying. A trend towards inhibition for PEA was observed for the 1–10-mg/kg doses only (Fig. 1). The inhibitory effect of OEA (5 mg/kg) was not counteracted by a per se noneffective dose of the CB1 receptor antagonist rimonabant (0.1 mg/kg), the CB2 receptor antagonist SR144528 (1 mg/kg), or the TRPV1 antagonist I-RTX (0.75 mg/kg) (Fig. 2). In addition, the inhibitory effect of OEA on gastric emptying was also not modified by pretreatment with the PPAR-α antagonist MK886 (6 mg/kg) (Fig. 3). Moreover, the PPAR-α agonist WY14643 (6 mg/kg) did not significantly modify gastric emptying (% gastric emptying: control 66.9 ± 8.4; WY14643 66.6 ± 5.4, n = 8). Figure 4 shows the time course of the inhibitory effect of OEA on gastric emptying. It appears that the effect of OEA is maximal after 0.5 h, declines after 1–4 h, and is absent after 8 h from its administration (Fig. 4).
Effect of IP-injected oleoylethanolamide (OEA) and palmitoylethanolamide (PEA) (both these bioactive amides were used at doses ranging from 1 to 15 mg/kg) on gastric emptying in control mice. Bars represent the mean ± SEM of 9–11 animals for each experimental group. Single asterisks, P < 0.05, and double asterisks, P < 0.01 vs corresponding vehicle
Effect of IP-injected oleoylethanolamide (OEA, 5 mg/kg) alone or in the presence of the CB1 receptor antagonist rimonabant (SR1, 0.1 mg/kg IP), or the CB2 receptor antagonist SR144528 (SR2, 1 mg/kg, IP) or the TRPV1 antagonist 5′-iodoresiniferatoxin (I-RTX, 0.75 mg/kg IP) on gastric emptying in control mice. Bars represent the mean ± SEM of 7–10 mice for each experimental group. Asterisks, P < 0.05 vs vehicle. The differences between OEA and OEA plus antagonists (i.e., OEA + SR1, OEA + SR2, or OEA + I-RTX) were not statistically different
Effect of IP-injected oleoylethanolamide (OEA, 5 mg/kg) alone or in the presence of the PPAR-α antagonist MK886 (6 mg/kg, IP) on gastric emptying in control mice. Bars represent the mean ± SEM of 7–10 mice for each experimental group. Asterisks, P < 0.05 vs vehicle. The difference between OEA and OEA + MK886 was not statistically different
Time course of inhibition of gastric emptying by IP-injected oleoylethanolamide (OEA 5 mg/kg). OEA was given at different times (0.5, 1, 2, 4, and 8 h) before the oral administration of the marker (phenol red) used to assess gastric emptying. Results are means ± SEM of 6–7 mice for each experimental group. Asterisks, P < 0.05 vs vehicle
Given alone (i.e., in absence of any agonist), the CB1 receptor antagonist rimonabant (0.1 mg/kg, IP), the CB2 receptor antagonist SR144528 (1 mg/kg IP), the TRPV1 antagonist I-RTX (0.75 mg/kg IP), and the PPAR-α antagonist MK886 (6 mg/kg IP) did not significantly modify gastric emptying (% of gastric emptying: control 78 ± 8, rimonabant 82 ± 7 control 70 ± 6, SR144528 68 ± 5; control 72 ± 5, I-RTX 64. ± 7; control 67 ± 8, MK886 71 ± 6; n = 8–10 for each experimental group).
Gastric emptying in HFD-fed mice
Compared to aged-matched STD-fed animals, HFD mice showed significantly increased body weight (STD 29.6 ± 0.4 g; HFD 41.5 ± 0.7 g, n = 38 for each experimental group), higher blood glucose (STD 121 ± 6; HFD 167 ± 5 per 100 ml, n = 6–8 for each experimental group), and delayed gastric emptying (percentage gastric emptying STD 79 ± 5 HFD 65 ± 3.5, n = 9 for each experimental group). OEA reduced gastric emptying both in control and HFD-fed animals (Fig. 5a). Statistical significance was achieved starting from the 8-mg/kg dose in control animals and from 4 mg/kg in HFD-fed animals (Fig. 5a). However, no statistical significance was observed between the curves representing the percent of the inhibitory effects of OEA on gastric emptying (Fig. 5b).
Effect of oleoylethanolamide (OEA, 2–12 mg/kg, IP) on gastric emptying in animal fed for 14 weeks a standard or a high-fat diet (HFD). Results (mean ± SEM of 3–5 mice for each experimental group) are expressed as percentage of gastric emptying (a) or percentage of inhibition of corresponding control values (b). a Asterisks, P < 0.05 vs corresponding vehicle
Levels of OEA and PEA
Gastric and small intestinal OEA and PEA levels were measured after 8 and 14 weeks of a HFD or a STD. As shown in Table 1, after 14 weeks of HFD, the levels of OEA and PEA in the stomach were increased by 2.3- and 1.7-fold, respectively, compared to STD. The changes in OEA and PEA levels were already significant after 8 weeks of HFD. OEA and PEA levels also increased with age. By contrast, OEA and PEA levels in the small intestine of 14-week HFD mice were not significantly different from those in STD mice, whereas they were significantly decreased after 8 weeks of HFD. Intestinal OEA, but not PEA, levels in HFD, but not STD, mice increased when passing from 8 to 14 weeks.
Table 2 reports the levels of OEA; PEA; and endocannabinoids, anandamide, and 2-AG in STD-fed mice treated with the FAAH inhibitor AA-5-HT. Compared to vehicle-treated animals, AA-5-HT caused a significant increase of anandamide, OEA, and PEA, whereas no differences were observed for 2-AG.
Expression of N-acyl-phosphatidylethanolamine-selective phospholipase D and FAAH
HFD caused a 3.9-fold decrease in the levels of FAAH mRNA (P = 0.03) in the antrum and a 2.0-fold increase of the levels of N-acyl-phosphatidylethanolamine-selective phospholipase D (NAPE-PLD) mRNA (P = 0.05) in the fundus (Table 3). FAAH expression in the fundus, and NAPE-PLD expression in the antrum, appeared to also be decreased and increased, respectively, but these changes did not achieve statistical significance (Table 3).
Discussion
The inhibition of gastric emptying represents an important brake against overfilling the gut [16–18]. Many intestinal “satiety signals,” including cholecystokinin, inhibit gastric emptying, and this probably helps limiting ingestion by enhancing gastric mechanoreceptor stimulation [16–19]. OEA is an anorexic lipid molecule that acts as a “satiety signal” in the gut [1]. In the present study, we have shown that OEA potently inhibited gastric emptying, both in control and in overweight mice, and this action could contribute, at least in part, to its anorectic effect.
The spectrum of the pharmacological actions of OEA is largely unexplored. Previous investigators have shown that OEA exerts analgesic [30], antioxidative [31] action and regulates food intake [5, 6] and fatty acid absorption [15]. In the present study, we have shown that OEA inhibited gastric emptying in a dose-dependent fashion. By contrast, PEA, a close structural analog of OEA, was without effect, an intriguing finding in the light of the observation that both these acylethanolamides have been shown to inhibit motility in the small intestine [22]. It is worth noting that the effects of OEA on gastric emptying shown here, as well as the effect of OEA on food intake previously reported [7], were found to be relatively short-lasting. The temporal correlation between the anorectic effect and the inhibition of gastric emptying suggest that the latter might contribute to the anorectic activity of OEA; of course, we cannot exclude the possibility that this correlation is coincidental.
To investigate the mode of action of OEA in reducing gastric emptying, we evaluated the possible involvement of (1) cannabinoid receptors, (2) TRPV1, and (3) PPAR-α. This is because (1) OEA may inhibit the inactivation of anandamide [32], an endogenous cannabinoid that reduces gastric emptying [24] and intestinal motility through activation of CB1 receptors in physiological states and CB2 receptors in pathophysiological states [33–36]; (2) OEA activates TRPV1 channels expressed in Xanopus oocytes [37] and mesenteric sensory fibers in rats [11], and it has been suggested that this amide exerts anorexic effects also via these receptors [12]. TRPV1 is present in the gastrointestinal tract, where it is primarily associated with axons of spinal afferent neurones and, to some extent, vagal afferents; activation of such receptors is known to affect gastrointestinal motility [38]; (3) OEA regulates feeding and body weight, stimulates fat utilization, and has neuroprotective effects mediated through activation of PPAR-α [1, 3]. However, the experiments performed here argue against the involvement of such receptors in the inhibitory action of OEA on gastric emptying. In fact, specific antagonists for such receptors (i.e., the CB1 antagonist rimonabant, the CB2 antagonist SR144528, the TRPV1 antagonist I-RTX, and the PPAR-α antagonist MK886) failed to affect OEA-induced changes in gastric motility. The lack of involvement of PPAR-α was strengthened by the observation that the PPAR-α agonist, WY14643, at a dose previously shown to reduce oxidative stress and inflammatory response evoked by transient cerebral ischemia/reperfusion in the rat [23], did not affect gastric emptying. Importantly, the dose of rimonabant in the present study has been recently shown to counteract anandamide-induced delay in gastric emptying in mice [24]. Others have recently shown that OEA is an endogenous ligand of the orphan receptor GP119, a G protein-coupled receptor expressed predominantly in the human and rodent pancreas and in the gastrointestinal tract [39]. The possibility that this receptor mediates some of the effects of OEA reported here could not be tested due to the lack of commercially available GPR119 antagonists, and this will have to be assessed in future studies.
Additional evidence about a physiological role of OEA in the modulation of gastric emptying comes from the gastric assays of acylethanolamides in animals treated with the FAAH inhibitor AA-5-HT. We have recently shown the FAAH enzyme is a physiological regulator of gastric emptying [24]. Moreover, the inhibitory effect of the FAAH inhibitor AA-5-HT involves both a cannabinoid CB1- and a noncannabinoid receptor-mediated component [24]. In the present study we have shown that AA-5-HT increased the gastric content of not only the endogenous ligand anandamide (but not 2-AG), but also that of OEA and PEA. These results suggest that (1) anandamide, but not 2-AG, is responsible of the CB1-mediated component of the inhibitory effect of AA-5-HT, and (2) OEA (and possibly to a very minor extent, PEA) might contribute to the noncannabinod receptor-mediated effect of AA-5-HT.
In men, gastric emptying is slowed in proportion to the energy density of the meal, which will level out the rate of energy delivery to the duodenum [40]. In the present study, we have shown that gastric emptying was reduced in mice made overweight and hyperglycemic with a HFD for 14 weeks. Our data are in agreement with previous investigators who reported delayed gastric emptying in ob/ob mice, a genetic model of obesity and diabetes [41]. The reduced gastric emptying in HFD-fed animals was found here to be accompanied by a significant ∼2-fold increase in gastric OEA levels, which instead was not observed in the small intestine. It has been reported that, in lean rats, OEA levels increase after food intake in the small intestine but not the stomach, possibly because this compound has anorexic properties and this change might represent an adaptive reaction to turn off food intake [14]. In our case, however, we found increased OEA levels after HFD in the stomach but not in the small intestine, and both STD and HFD mice were killed after a few hours of fasting. Therefore, our finding of increased OEA levels in the stomach of HFD mice is unlikely to be due to an acute dietary effect and seems to be, rather, the consequence of a prolonged dietary regimen. The increased levels of OEA, which potently reduces gastric emptying (see above), might contribute, at least in part, to the decreased motility observed in HFD-fed mice, although we cannot definitively exclude the possibility that delayed gastric emptying and increased OEA levels are independent events. On the other hand, it is very unlikely that anandamide, which is known to dose-dependently reduce gastric emptying via CB1 receptor activation, contributes to the delay in gastric emptying observed in HFD-fed mice. In fact, the stomach levels of both anandamide and CB1 receptor expression are down-regulated following HFD [24]. Importantly, the levels of both OEA and PEA were already significantly higher in the stomach of HFD mice after 8 weeks of this dietary regimen and increased with age, indicating that these lipid mediators are particularly sensitive to both changes in dietary fat intake and age. In addition, the ability of HFD to increase OEA levels in the stomach is tissue-specific because no significant changes after 14 weeks, and even a decrease after 8 weeks, were observed in the small intestine of the same mice. Intriguingly, previous investigators reported that, also in food-deprived lean mice, the levels of OEA in the small intestine (but not in the stomach) are markedly decreased and return to baseline after refeeding [5]. Thus, both short-term food deprivation and prolonged HFD cause a decrease of OEA intestinal levels, similar to what was previously found for the orexigenic endocannabinoid anandamide, whose levels instead increase in the hypothalamus of both lean food-deprived and obese rats [42].
In view of the changes in gastric OEA levels observed following a HFD, we decided to analyze by quantitative reverse-transcription PCR the levels of OEA biosynthesizing and degrading enzymes in the gastric antrum and fundus of STD and HFD mice after 14 weeks of either dietary regimen. Results indicate that that the elevated levels of OEA were likely to be caused by both increased biosynthesis, due to the up-regulation of NAPE-PLD expression observed in the fundus, and decreased degradation, suggested by the decreased FAAH expression found in the antrum. In addition, we found that OEA preferentially inhibited gastric emptying in HDF-fed animals, although this difference did not reach statistical significance. Interestingly, at the dose of 4 mg/kg, OEA significantly reduced gastric in HFD but not in control mice, thus suggesting a preferential effect at least of this dose of the amide in inhibiting gastric motility in overweight/hyperglycemic animals. This latter finding might be explained also with the reduced expression of FAAH mRNA levels observed here after HFD, which might result in reduced inactivation of exogenously administered OEA by FAAH.
In conclusion, we have shown here that the naturally occurring amide OEA exerts an inhibition of gastric emptying that might underlie part of the anorexic actions previously reported in rodents for this compound, both in control and in overweight mice. The pharmacological target of OEA still requires further investigation; however, the inhibitory action of OEA on gastric motility does not involve PPAR-α, TRPV1 or cannabinoid receptors. HFD appears to increase gastric OEA levels through a concerted regulation of its biosynthesis and degradation. The increased gastric levels of OEA suggest (although do not definitively prove) a possible contribution of this mediator in the delayed gastric emptying observed here in HFD-fed mice. A pharmacological modulation of gastric OEA levels might offer novel therapeutic strategies in the treatment of gastric motility diseases, with a potential in diabetic obese patients, where the blood levels of this compound are permanently elevated [2].
Abbreviations
- AA-5-HT:
-
N-arachidonoylserotonin
- 2-AG:
-
2-arachidonoylglycerol
- DMSO:
-
Dimethylsulfoxide
- FAAH:
-
Fatty acid amide hydrolase
- HFD:
-
High-fat diet
- OEA:
-
Oleoylethanolamide
- I-RTX:
-
5′-iodoresiniferatoxin
- NAPE-PLD:
-
N-acyl-phosphatidylethanolamine-selective phospholipase D
- PEA:
-
Palmitoylethanolamide
- PPAR:
-
Peroxisome proliferator-activated receptor
- RT-PCR:
-
Reverse-transcription polymerase chain reaction
- TRPV1:
-
Transient receptor potential vanilloid type-1
- STD:
-
Standard diet
References
Lo Verme J, Gaetani S, Fu J, Oveisi F, Burton K, Piomelli D (2005) Regulation of food intake by oleoylethanolamide. Cell Mol Life Sci 62:708–716
Matias I, Gonthier MP, Petrosino S, Docimo L, Capasso R, Hoareau L, Monteleone P, Roche R, Izzo AA, Di Marzo V (2007) Role and regulation of acylethanolamides in energy balance: focus on adipocytes and beta-cells. Br J Pharmacol 152:676–690
O’Sullivan SE (2007) Cannabinoids go nuclear: evidence for activation of peroxisome proliferator-activated receptors. Br J Pharmacol 152:576–582
Proulx K, Cota D, Castaneda TR, Tschop MH, D’Alessio DA, Tso P, Woods SC, Seeley RJ (2005) Mechanisms of oleoylethanolamide-induced changes in feeding behavior and motor activity. Am J Physiol Regul Integr Comp Physiol 289:R729–R737
Rodriguez de Fonseca F, Navarro M, Gomez R, Escuredo L, Nava F, Fu J, Murillo-Rodriguez E, Giuffrida A, LoVerme J, Gaetani S, Kathuria S, Gall C, Piomelli D (2001) An anorexic lipid mediator regulated by feeding. Nature 414:209–212
Fu J, Gaetani S, Oveisi F, Lo Verme J, Serrano A, Rodriguez De Fonseca F, Rosengarth A, Luecke H, Di Giacomo B, Tarzia G, Piomelli D (2003) Oleylethanolamide regulates feeding and body weight through activation of the nuclear receptor PPAR-α. Nature 425:90–93
Gaetani S, Oveisi F, Piomelli D (2003) Modulation of meal pattern in the rat by the anorexic lipid mediator oleoylethanolamide. Neuropsychopharmacology 28:1311–1316
Guzman M, Lo Verme J, Fu J, Oveisi F, Blazquez C, Piomelli D (2004) Oleoylethanolamide stimulates lipolysis by activating the nuclear receptor peroxisome proliferator-activated receptor alpha (PPAR-alpha). J Biol Chem 279:27849–27854
Nielsen MJ, Petersen G, Astrup A, Hansen HS (2004) Food intake is inhibited by oral oleoylethanolamide. J Lipid Res 45:1027–1029
Fu J, Oveisi F, Gaetani S, Lin E, Piomelli D (2005) Oleoylethanolamide, an endogenous PPAR-alpha agonist, lowers body weight and hyperlipidemia in obese rats. Neuropharmacology 48:1147–1153
Movahed P, Jonsson BA, Birnir B, Wingstrand JA, Jorgensen TD, Ermund A, Sterner O, Zygmunt PM, Hogestatt ED (2005) Endogenous unsaturated C18 N-acylethanolamines are vanilloid receptor (TRPV1) agonists. J Biol Chem 280:38496–38504
Wang X, Miyares RL, Ahern GP (2005) Oleoylethanolamide excites vagal sensory neurones, induces visceral pain and reduces short-term food intake in mice via capsaicin receptor TRPV1. J Physiol 564:541–547
Petersen G, Sorensen C, Schmid PC, Artmann A, Tang-Christensen M, Hansen SH, Larsen PJ, Schmid HH, Hansen HS (2006) Intestinal levels of anandamide and oleoylethanolamide in food-deprived rats are regulated through their precursors. Biochim Biophys Acta 1761:143–150
Fu J, Astarita G, Gaetani S, Kim J, Cravatt BF, Mackie K, Piomelli D (2007) Food intake regulates oleoylethanolamide formation and degradation in the proximal small intestine. J Biol Chem 282:1518–1528
Yang Y, Chen M, Georgeson KE, Harmon CM (2007) Mechanism of oleoylethanolamide on fatty acid uptake in small intestine after food intake and body weight education. Am J Physiol Regul Integr Comp Physiol 292:R235–R241
Cuomo R, Sarnelli G (2004) Food intake and gastrointestinal motility. A complex interplay. Nutr Metab Cardiovasc Dis 14:173–179
Park MI, Camilleri M (2005) Gastric motor and sensory functions in obesity. Obes Res 13:491–500
Cummings DE, Overduin J (2007) Gastrointestinal regulation of food intake. J Clin Invest 117:13–23
Hellstrom PM, Naslund E (2001) Interactions between gastric emptying and satiety, with special reference to glucagon-like peptide-1. Physiol Behav 74:735–741
Serrano A, Del Arco I, Javier Pavon F, Macias M, Perez-Valero V, Rodriguez de Fonseca F (2008) The cannabinoid CB1 receptor antagonist SR141716A (Rimonabant) enhances the metabolic benefits of long-term treatment with oleoylethanolamide in Zucker rats. Neuropharmacology 54:226–234
Darmani NA, Izzo AA, Degenhardt B, Valenti M, Scaglione G, Capasso R, Sorrentini I, Di Marzo V (2005) Involvement of the cannabimimetic compound, N-palmitoyl-ethanolamine, in inflammatory and neuropathic conditions: review of the available pre-clinical data, and first human studies. Neuropharmacology 48:1154–1163
Capasso R, Matias I, Lutz B, Borrelli F, Capasso F, Marsicano G, Mascolo N, Petrosino S, Monory K, Valenti M, Di Marzo V, Izzo AA (2005) Fatty acid amide hydrolase controls mouse intestinal motility in vivo. Gastroenterology 129:941–951
Collino M, Aragno M, Mastrocola R, Benetti E, Gallicchio M, Dianzani C, Danni O, Thiemermann C, Fantozzi R (2006) Oxidative stress and inflammatory response evoked by transient cerebral ischemia/reperfusion: effects of the PPAR-alpha agonist WY14643. Free Radic Biol Med 41:579–589
Di Marzo V, Capasso R, Matias I, Aviello G, Petrosino S, Borrelli F, Orlando P, Capasso F, Izzo AA (2008) The role of endocannabinoids in the regulation of gastric emptying: alterations in mice fed a high fat diet. Br J Pharmacol Jan 28 [Epub ahead of print]
El-Salhy M (2001) Gastric emptying in an animal model of human diabetes type 1: relation to endocrine cells. Acta Diabetol 38:139–144
Bisogno T, Berrendero F, Ambrosino G, Cebeira M, Ramos JA, Fernandez-Ruiz JJ, Di Marzo V (1999) Brain regional distribution of endocannabinoids: implications for their biosynthesis and biological function. Biochem Biophys Res Commun 256:377–380
Izzo AA, Aviello G, Petrosino S, Orlando P, Marsicano G, Lutz B, Borrelli F, Capasso E, Nigam S, Capasso D, Di Marzo V (2008) Increased endocannabinoid levels reduce the development of precancerous lesions in the mouse colon. J Mol Med 86:89–98
D’Argenio G, Petrosino S, Gianfrani C, Valenti M, Scaglione G, Grandone I, Nigam S, Sorrentini I, Mazzarella G, Di Marzo V (2007) Overactivity of the intestinal endocannabinoid system in celiac disease and in methotrexate-treated rats. J Mol Med 85:523–530
Bisogno T, Melck D, De Petrocellis L, Bobrov MYu, Gretskaya NM, Bezuglov VV, Sitachitta N, Gerwick WH, Di Marzo V (1998) Arachidonoylserotonin and other novel inhibitors of fatty acid amide hydrolase. Biochem Biophys Res Commun 248:515–522
Suardiaz M, Estivill-Torrus G, Goicoechea C, Bilbao A, Rodriguez de Fonseca F (2007) Analgesic properties of oleoylethanolamide (OEA) in visceral and nflammatory pain. Pain 133:99–110
Ambrosini A, Zolese G, Ambrosi S, Ragni L, Tiano L, Littarru G, Bertoli E, Mantero F, Boscaro M, Balercia G (2006) Oleoylethanolamide protects human sperm cells from oxidation stress: studies on cases of idiopathic infertility. Biol Reprod 74: 659–665
Jonsson KO, Vandevoorde S, Lambert DM, Tiger G, Fowler CJ (2001) Effects of homologues and analogues of palmitoylethanolamide upon the inactivation of the endocannabinoid anandamide. Br J Pharmacol 133:1263–1275
Duncan M, Davison JS, Sharkey KA (2005) Review article: endocannabinoids and their receptors in the enteric nervous system. Aliment Pharmacol Ther 22:667–683
Massa F, Storr M, Lutz B (2005) The endocannabinoid system in the physiology and pathophysiology of the gastrointestinal tract. J Mol Med 83:944–954
Di Marzo V, Izzo AA (2006) Endocannabinoid overactivity and intestinal inflammation. Gut 55:1373–1376
Izzo AA (2007) The cannabinoid CB(2) receptor: a good friend in the gut. Neurogastroenterol Motil 19:704–708
Ahern GP (2003) Activation of TRPV1 by the satiety factor oleoylethanolamide. J Biol Chem 278:30429–30434
Holzer P (2004) TRPV1 and the gut: from a tasty receptor for a painful vanilloid to a key player in hyperalgesia. Eur J Pharmacol 500:231–241
Overton HA, Babbs AJ, Doel SM, Fyfe MC, Gardner LS, Griffin G, Jackson HC, Procter MJ, Rasamison CM, Tang-Christensen M, Widdowson PS, Williams GM, Reynet C (2006) Deorphanization of a G protein-coupled receptor for oleoylethanolamide and its use in the discovery of small-molecule hypophagic agents. Cell Metab 3:167–175
Wisen O, Hellstrom PM (1995) Gastrointestinal motility in obesity. J Intern Med 237:411–418
Asakawa A, Inui A, Ueno N, Makino S, Uemoto M, Fujino MA, Kasuga M (2003) Ob/ob mice as a model of delayed gastric emptying. J Diabetes Complications 17:27–28
Di Marzo V, Goparaju SK, Wang L, Liu J, Batkai S, Jarai Z, Fezza F, Miura GI, Palmiter RD, Sugiura T, Kunos G (2001) Leptin-regulated endocannabinoids are involved in maintaining food intake. Nature 410:822–825
Acknowledgements
This work was supported by Prin, Regione Campania, “Fondazione Enrico ed Enrica Sovena,” Epitech, S.r.l. (to SP and VDM), and Sanofi-Aventis (to VDM).
Competing interests
The authors declare no competing interests.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Aviello, G., Matias, I., Capasso, R. et al. Inhibitory effect of the anorexic compound oleoylethanolamide on gastric emptying in control and overweight mice. J Mol Med 86, 413–422 (2008). https://doi.org/10.1007/s00109-008-0305-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-008-0305-7