Abstract
Interactions between peripheral blood mononuclear cells (PBMCs) and those within plaques are suggested to be pathophysiologically relevant to lipid-induced arteriosclerosis. In this study, gene expressions of scavenger receptors (CD36, CD68), LPS receptor (CD14), proinflammatory (tumor necrosis factor alpha [TNFα], CD40, interleukin-1 beta [IL-1β]) and oxidative stress-related (manganese superoxide dismutase [MnSOD]) markers were analyzed in PBMCs of clinically asymptomatic males with classical proatherogenic risk factors such as smoking and/or hyperlipidemia. PBMCs were isolated from venous blood of normolipidemic non-smokers (n = 10) and smokers (n = 8), and hyperlipidemic non-smokers (n = 9) and smokers (n = 8). RNA from PBMCs was used for PCR analyses. Plasma concentrations of oxidized low-density lipoproteins (oxLDL) were measured by ELISA. The gene expressions of CD36, CD68, CD40, TNFα, and MnSOD were significantly higher in PBMCs of hyperlipidemics than in normolipidemics, irrespective of whether they were smoking or not. The individual expression of these genes showed significant positive correlations with each other but also with serum cholesterol or plasma oxLDL concentrations. The higher expressions of scavenger receptors, proinflammatory and oxidative stress-related genes of PBMCs are suggested to result mainly from hyperlipidemia and the accompanied increase of oxLDL concentrations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hyperlipidemia, a classical proatherogenic risk factor, is associated with a low grade systemic inflammation indicated by higher levels of proinflammatory markers in the blood, such as C-reactive protein (CRP) or fibrinogen, and increased proinflammatory processes in the arteriosclerotic intima. In mononuclear cells within arteriosclerotic vessel walls, an increased expression of numerous markers, such as scavenger receptors (CD36, CD68), proinflammatory cytokines like tumor necrosis factor alpha (TNFα), and oxidative stress-related enzymes, such as manganese superoxide dismutase (MnSOD) was found, especially in macrophages (MΦ) [1–4]. Moreover, interactions between peripheral blood mononuclear cells (PBMCs) and those within plaques have been suggested to be pathophysiologically relevant to lipid-induced arteriosclerosis [5].
Several components, such as high LDL, low HDL, and elevated triglycerides were associated with an increased proatherogenic risk. Since oxLDL leads to lipid accumulation in MΦ via an unregulated receptor-mediated uptake by scavenger receptors such as CD36 (macrophage type B scavenger receptor), CLA-1 and CD68, and SR-A or LOX-1, it was suggested as a new risk factor for arteriosclerotic inflammation [6, 7]. However, only CD36, CLA-1, and CD68 seem to be crucial for the progression of MΦ to foam cells [8–11]. Moreover, treatment of human MΦ with oxLDL in in vitro experiments induced an increase in oxidative stress and proinflammatory processes, as indicated e.g. by upregulation of MnSOD or release of TNFα [3, 4, 12]. In CD36-deficient patients, isolated MΦ were shown to secrete significantly less amounts of TNFα and interleukin-1 beta (IL-1β) upon addition of oxLDL or thrombospondin-1 compared to MΦ from control subjects [13]. In human arteriosclerotic lesions, oxLDL was shown to be colocalized with CD40, CD68 or MnSOD in mononuclear cells/MΦ [14, 15].
In addition, besides intralesional processes in which activated MΦ express proinflammatory cytokines, systemic proinflammatory mediators such as circulating cholesterol or lipoproteins are suggested to promote the arteriosclerotic process [16, 17]. Several traditional cardiovascular risk factors, in particular obesity or smoking behaviour, were found to track with inflammatory biomarkers [18]. While the risk-related changes of plasma constituents were established as diagnostic or prognostic markers, alterations of circulating blood cells have rarely been studied. PBMCs are considered as major proatherogenic targets, e.g. for oxLDL action, and could enhance local arteriosclerotic processes when e.g. migrating into the intima after proinflammatory activation.
Because smoking and hyperlipidemia were associated with an increase in systemic prooxidative and proinflammatory shift [19], we chose middle-aged male subjects without clinical symptoms of arteriosclerosis but classical proatherogenic risk factors, i.e. hyperlipidemia or smoking to study the expression of scavenger receptors (CD36, CD68), LPS receptor (CD14), inflammation markers (TNFα, IL-1β, CD40), and an oxidative stress-related marker (MnSOD) in PBMCs. In addition, in the plasma of the subjects under test, we measured oxLDL, soluble forms of vascular cell adhesion molecule-1 (sVCAM-1), intercellular adhesion molecule-1 (sICAM-1) and antioxidative capacity.
Materials and methods
Subjects
A total of 35 male subjects was recruited to the following four groups (1–4): (1) Normolipidemic, healthy non-smokers (NL-NSM; n = 10) and (2) normolipidemic smokers (NL-SM; n = 8; average smoking: 20 cigarettes/day) from the local campus, which all had total serum cholesterol levels <220 mg/dl and triglycerides <150 mg/dl and were without any other known atherogenic risk factors (like diabetes or hypertension) and without medication. (3) Hyperlipidemic non-smokers (HL-NSM; n = 9) and (4) hyperlipidemic smokers (HL-SM; n = 8; average smoking 20 cigarettes/day) from the Lipid Outpatient Clinic of the Internal Medicine of the University of Heidelberg, which all had total serum cholesterol levels >220 mg/dl and/or triglyceride levels >150 mg/dl but were without any form of cardiovascular treatment. A detailed clinical history of these male subjects was obtained to rule out previous atherosclerotic vascular events.
The study was approved by the local ethics committee of the University Hospital of Heidelberg. All subjects provided informed written consent.
Blood samples, blood lipids, plasma homocysteine, plasma antioxidative capacity, sICAM-1, TNFα and sVCAM-1
Blood samples were routinely taken from the cubital vein. Total serum cholesterol, HDL and LDL cholesterol, and triglyceride levels were quantified by standard methods. Homocysteine was determined in EDTA plasma by HPLC at the laboratory of the University Medical Hospital (Heidelberg).
Plasma oxLDL concentration was measured with a commercially available ELISA (Mercodia, Uppsala, Sweden).
Plasma sICAM-1, sVCAM-1 and TNFα concentrations were routinely determined with commercially available sICAM-1-ELISA-Kit or sVCAM-1-ELISA-Kit (Immuno-Biological Laboratories, Hamburg, Germany) or TNFα-EASIA-Kit (Bio Source Europe S.A., Nivelles, Belgium) according to the manufacturer’s specifications.
Furthermore, as marker for antioxidative capacity of human plasma, we used the 2,2′-azobis-(2-amidinopropane) hydrochloride (AAPH) reaction as described by Lissi et al. [20] and modified by Amraei Davijani [21] and Heinle [unpublished data]. Shortly, the thermolytic decomposition of AAPH (10 mM) in phosphate buffered saline (pH 7.4, 500 μl) was used to generate a constant rate of free radicals, which can be followed by luminol-enhanced chemiluminescence (luminol, dissolved in dimethylsulfoxide, final concentration 110 μM). Light emission was measured in a Bethold Biolumat LB9505 (Wildbad, Germany). After reaching a constant light signal, 10 μl of the plasma samples were added and the time of quenching the chemiluminescence by the antioxidants present in the plasma was measured.
Isolation of PBMCs and RNA-preparation
PBMCs were routinely isolated by Histopaque (Sigma, Deisenhofen, Germany) density gradient centrifugation as previously described [4, 19]. RNA of the PBMCs was extracted from 1 × 106 cells using Tripure reagent (Roche, Mannheim, Germany) according to the manufacturer’s specifications, characterized by spectrophotometry (A 280/A 260 > 1.8, A 260/A 230 > 2.4). Denaturating agarose gel electrophoresis was routinely performed to determine RNA integrity.
Semiquantitative PCR
An aliquot of 0.25 μg total RNA was treated with 1 unit RNAse free DNAse (Fermentas, St. Leon-Rot, Germany) 30 min at 37°C. Reverse transcription of RNA was performed with oligo (dT)12–18 primer and 200 units of SUPERSCRIPT II (Invitrogen) and 24 units of Ribo Lock™ RNAse inhibitor (Fermentas) in a 25 μl reaction volume for 1 h at 42°C. The enzyme was then inactivated by 10 min incubation at 70°C. cDNA (1–2 μl) was used for PCR analysis in a 20 μl reaction volume containing 10 mM Tris/HCl (pH 8.3), 50 mM KCl, 0.2 mM each dNTP, 1 U Taq DNA polymerase (Roche), 200 nM each of forward and reverse primer. The MgCl2 concentration was 1.5 mM for CD68, CD14 and MnSOD, 1 mM for CD40, 2 mM for TNFα. The primer sequences and sizes expected in the RT-PCR were for: CD14, 5′-ACT CCC TCA ATC TGT CGT TCG CTG-3′ (forward), 5′-CTG AAG CCA AGG CAG TTT CAG TCC-3′ (reverse), and 338-bp product; CD36, 5′-GCT GAG GAC AAC ACA GTC TC-3′ (forward), 5′-GCT GAT GTC TAG CAC ACC AT-3′ (reverse), and 674-bp product [22]; CD40, 5′-CTG TTT GCC ATC CTC TTG GT-3′ (forward), 5′-CGA CTC TCT TTG CCA TCC TC-3′ (reverse), and 200-bp product [23]; CD68, 5′-CGT CAC AGT TCA TCC AAC AAG C-3′ (forward), 5′-TTG GGG TTC AGT ACA GAG ATG-3′ (reverse), and 332-bp product; IL-1β, 5′-ATG GCA GAA GTA CCT AAG CTC GC-3′(forward), 5′-ACA CAA ATT GCA TGG TGA AGT CAG TT-3′ (reverse), and 750-bp product [24]; MnSOD, 5′-ACG TGA ACA ACC TGA ACG TC-3′ (forward), 5′-CTG CAG TAC TCT ATA CCA CTA CA-3′ and 568-bp product; TNFα, 5′-GAG TGA CAA GCC TGT AGC CCA TGT TGT AGC A-3′ (forward), 5′-GGC AAT GAT GAT CCC AAA GTA GAC CTG CCC AGA CT-3′ (reverse), and 400-bp product [24]. Amplification of part of the β-microglobulin gene was used as a positive control using primers 5′-CTC GCG CTA CTC TCT CTT TCT-3′ (forward) and 5′-TGT CGG ATT GAT GAA ACC CAG-3′ (reverse) and 198-bp product. A PCR reaction profile with initial denaturation for 2 min at 94°C, followed by 30 s at 94°C, 1 min at 63°C and 1.5 min at 72°C (hCD68), 30 s at 94°C, 1 min at 59°C, 90 s at 72°C (CD36), 30 s at 94°C, 30 s at 55°C and 30 s at 72°C (CD40), 1 min at 94°C, 1 min at 56°C and 2 min at 72°C (CD14), 45 s at 94°C, 45 s at 52°C and 2 min at 72°C (TNFα), 1 min at 94°C, 1 min at 55°C, 1 min at 72°C (MnSOD), 45 s at 94°C, 45 s at 50°C, 45 s at 72°C (β-microglobulin) in 35 cycles and a final extension step for 10 min at 72°C was performed using a Genius thermal cycler (Techne Inc., Cambridge, UK). Amplification products were separated on a 2% agarose gel and stained with ethidium bromide. The signals were analyzed using the Scion Image Beta 4.02 Win video image capture and analysis system (Scioncorp, Frederick, MD 21701, USA) integrating intensity over a given band. Gene expression measurements by RT-PCR were repeated at least two times and data are expressed as a ratio between the PCR products formed by the gene of interest relative to that developed by β-microglobulin.
Quantitative PCR
A primer pair sequence within the human CD36, CD40, CD68, MnSOD, TNFα, β-microglobulin and GAPDH was constructed and synthesized (MWG Biotech, Ebersberg, Germany), the primer sequences were the same as for semiquantitative PCR. GAPDH primer sequence was 5′-ATT CCA TGG CAC CGT CAA GGC T-3′ (forward) and 5′-TCA GGT CCA CCA CTG ACA CGT T-3′ (reverse) and 571-bp product, β-actin 5′-AAG GAT TCC TAT GTG GGC-3′ (forward) and 5′-CAT CTC TTG CTC GAA GTC-3′ (reverse) and 520 bp product. Real-time PCR was performed using a ABI Prism 7,000 Sequence Detection System (SDS; Applied Biosystem, Applera Deutschland GmbH, Weiterstadt, Germany) using SYBR Green I technology. In each experiment, duplicates of 25 ng cDNA (total RNA equivalent) of unknown samples were amplified in a 15 μl reaction containing 1X Platinum SYBR green qPCR SuperMix UDG (Invitrogen, Karlsruhe, Germany). The thermal profile consisted of 1 cycle at 50°C for 2 min followed by 1 cycle at 95°C (2 min), 45 cycles at 95°C (15 s), 60°C (1 min). Specificity of the amplified product was confirmed by melting curve analysis and on a 2% agarose gel electrophoresis to confirm the amplicon size in conjunction with melting curve data. For relative quantification, a standard curve was generated from a pool of cDNA from 40 patients and controls. Relative quantity was calculated by the ratio of the target gene and the appropriate β-microglobulin, GAPDH or β-actin expression. Data were analyzed using the ABI Prism 7,000 SDS software for Windows (Applied Biosystems, Foster City, CA, USA). In addition, the software tool REST© (relative expression software tool), which compares two groups (a control group vs a sample group) was used [25–27].
Statistical analyses
Differences in real-time PCR expression between control and samples were assessed by a pair-wise fixed reallocation randomisation test [25–27]. Results are presented as the mean ± SEM. Depending on the mode of distribution, statistical procedures were performed by the Mann–Whitney U test or the unpaired Student’s t test, respectively, using the SPSS Base 11.5 for Windows. Correlation between different parameters was graphically described by scatterplots and linear regression lines. The relation was quantitatively assessed by Pearson’s product correlation coefficient r and by a statistical test for the existence of a positive or negative slope. A P value of 0.05 or less was chosen for statistical significance.
Results
Patient characteristics and plasma/serum parameters
On the average, age, height, weight and body mass index were similar among the groups under test (Table 1). By definition, in both hyperlipidemic groups (HL-NSM and HL-SM) the mean serum triglyceride, cholesterol, and VLDL levels were higher than in normolipidemic subjects (NL-NSM and NL-SM) (Table 2). Plasma oxLDL concentrations in groups 2 to 4 were significantly higher than in group 1 (Table 2). The homocysteine levels were not significantly different among all four groups.
Both groups of smokers (groups 2 and 4) revealed significantly higher (60–70%) plasma sICAM-1 concentrations in comparison to group 1, whereas plasma sVCAM-1 and TNFα concentrations were not significantly different among the groups (Table 2). Furthermore, the AAPH reaction revealed that in the plasma, the suppression time—as an indicator for oxidative stress—was significantly lower (20%) in group 4 compared to groups 1 and 3 (Table 2).
Gene expression in PBMCs and association with hyperlipidemia and/or smoking
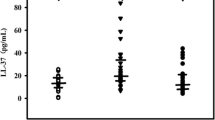
Using semiquantitative PCR, on the average, the CD36, CD40, CD68, TNFα, and MnSOD expressions in PBMCs of HL-NSM and HL-SM (groups 3 and 4) were significantly higher than in NL-NSM and NL-SM (groups 1 and 2) (Fig. 1), while the expressions of CD14 and IL-1β were similar among all groups (Fig. 1). Real-time PCR of PBMC of the majority of the subjects (RNA was available for 24 out of 35 subjects) revealed that gene expressions of CD36, CD68, CD40, TNFα and MnSOD were insignificantly higher in NL-SM than in NL-NSM. In PBMCs of HL-NSM, gene expressions of CD36 (5.8-fold; P = 0.001), CD68 (3.1-fold; P = 0.001), CD40 (2.0-fold), TNFα (4.9-fold; P = 0.001) and MnSOD (3.3-fold; P = 0.001) were higher than in NL-NSM and also of HL-SM than in NL-NSM: CD36 (2.3-fold), CD68 (2.1-fold), CD40 (5.4-fold; P = 0.001), TNFα (3.2-fold; P = 0.001), MnSOD (2.5-fold; P = 0.001). Moreover, significant positive correlations consisted between the expression of genes determined by semiquantitative and quantitative PCR: TNFα (r = 0.5; P = 0.027), MnSOD (r = 0.5; P = 0.0176), CD68 (r = 0.4; P = 0.0483), CD36 (r = 0.6; P = 0.0076) and CD40 (r = 0.4; P = 0.09).
Quantification of the expression of CD36, CD68, CD40, TNFα, MnSOD, IL-1β and CD14 (relative to the respective β-microglobulin [β-micro]) RT-PCR of PBMC of healthy male subjects and persons with cardiovascular risk factors. Healthy subjects (NL-NSM), normolipidemic smokers (NL-SM), hyperlipidemic non-smokers (HL-NSM), hyperlipidemic smokers (HL-SM). ### P < 0.001, ## P < 0.01, # P < 0.05 vs NL-SM; ***P < 0.001, **P < 0.01 vs NL-NSM
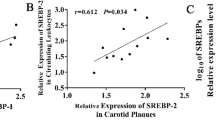
Regression analyses revealed significant positive correlations of individual serum cholesterol or plasma oxLDL levels and the relative expression of CD36, CD68, CD40, TNFα or MnSOD in PBMCs (Figs. 2 and 3). However, there was no significant correlation between serum cholesterol or plasma oxLDL concentration and expression of CD14 (monocyte marker) or IL-1β (not shown). Furthermore, significant positive correlations were found between the expression of scavenger receptors (CD36, CD68) and the expression of markers of oxidative stress and inflammation in PBMCs (MnSOD, CD40, TNFα) (Table 3). Serum HDL levels were inversely correlated with the gene expression of CD36, CD68, CD40, TNFα, MnSOD, IL-1β or CD14 in PBMCs, however, statistically significant only for TNFα (Table 3). There was no significant correlation between plasma homocysteine concentration and the expressions of CD36, CD68, CD40, TNFα, MnSOD, IL-1β or CD14 in PBMCs (Table 3). In addition, we didn’t find any significant correlation between the expression of genes (under test) in PBMCs and plasma sICAM-1, TNFα, sVCAM-1 or suppression time (not shown). Furthermore, there was no significant correlation between gene expression in PBMC and age (with the exception of TNFα [r = 0.45; P = 0.03]).
Scatter plot and regression line of the correlation of individual CD36 (a), CD68 (b), CD40 (c), TNFα (d), MnSOD (e) or CD14 (f) expression in PBMC to serum cholesterol concentration of healthy male subjects and persons with cardiovascular risk factors. Healthy subjects (NL-NSM), normolipidemic smokers (NL-SM), hyperlipidemic non-smokers (HL-NSM), hyperlipidemic smokers (HL-SM). r, correlation coefficient; P, significance
Scatter plots and regression lines of the correlation of individual CD36 (a), CD68 (b), CD40 (c), TNFα (d), MnSOD (e) or CD14 (f) expression in PBMC to plasma oxLDL concentration of healthy male subjects and persons with cardiovascular risk factors. Healthy subjects (NL-NSM), NL-SM (normolipidemic smokers), HL-NSM (hyperlipidemic non-smokers), HL-SM (hyperlipidemic smokers). r, correlation coefficient; P, significance
Discussion
Our clinical study demonstrates that the gene expressions of the scavenger receptors CD36 and CD68, and of proinflammatory cytokines, such as TNFα and CD40, are higher in PBMCs of hyperlipidemic compared to normolipidemic male subjects. Especially the individual serum cholesterol and/or plasma oxLDL levels significantly positively correlated with the expression of these genes. Smoking behaviour had no influence. Hyperlipidemia, a proatherogenic risk factor, might be suggested to induce and to contribute to proinflammatory processes already in PBMCs, which was only known to occur in plaque macrophages until now.
As a novel finding, we show that the PBMCs of asymptomatic hyperlipidemics compared to normolipidemics have an increase in the gene expression of scavenger receptors CD36 and CD68—which both are suggested to contribute to arteriosclerosis. Both receptors (but not SR-A and LOX-1) were recently demonstrated to enhance the endocytotic uptake of oxLDL by MΦ or MΦ-derived cells, which may be a key step in the progression of MΦ to foam cells and in the initiation of arteriosclerosis [11, 28]. Our hypothesis that increased plasma oxLDL and/or serum cholesterol levels could stimulate CD36 and CD68 gene expression in PBMCs is supported by in vitro results in mononuclear cells [29, 30]. Moreover, these gene expressions were found to be inhibited in oxLDL stimulated macrophages by cholesterol synthesis inhibitors, such as pitavastatin (NK-104) and atorvastatin [31, 32] and other compounds [29, 33, 34]. In addition, regression analyses suggest that in hyperlipidemic smokers, compared to normolipidemic smokers, additional proatherogenic factors seem to be involved in the induction of the expression of these genes.
An increase of the proinflammatory marker soluble CD40 ligand, a member of the TNF family, is suggested as an early indicator of heart attack [35]. Higher gene expressions of CD40 and TNFα in the PBMCs of hyperlipidemic male subjects are shown here for the first time. Both proinflammatory cytokines are suggested to participate in arteriosclerosis. Just recently, CD40 was found to be increased on the surface of monocytes of cigarette smokers thereby enhancing platelet–monocyte aggregation [36]. Moreover, the finding that oxLDL promoted CD40 expression in human atheromas and upregulated the TNF production in MΦ in vitro supports our hypothesis that increased plasma oxLDL and/or serum cholesterol levels could contribute to their upregulation in vivo [37]. Furthermore, an upregulation of TNF-related apoptosis-inducing ligand messenger ribonucleic acid and protein expression by oxLDL was found in PBMCs [38]. A limitation of the expression of the CD40 receptor/ligand dyad by statins may be of particular interest because there exist two plausible mechanisms, either a direct inhibition or by diminishing lipoprotein levels, which may account for the anti-inflammatory action of some statins [39]. Preliminary data of another clinical trial in our group reveal a decrease in expression of proinflammatory and oxidative stress-related genes like CD40, TNFα and MnSOD in the PBMC of atorvastatin-treated arteriosclerotic patients (S. Zügel, K. Schottmüller, J. Metz and R. Kinscherf; unpublished observations). Furthermore, there was no difference in plasma TNFα concentration among the four groups under test.
In vitro oxLDL was shown to upregulate TNFα production in human macrophages [12, 37], which is associated with an induction of MnSOD [3, 4]. In this context, oxLDL and its metabolites (ceramide and hydrogen peroxide)—or the cytokine TNFα—were demonstrated to directly induce the expression of MnSOD (RNA and protein level) possibly due to oxidative stress [3, 4]. In the present study, we used the AAPH reaction to measure the suppression time, as an indicator for oxidative stress [20, 21, Heinle (unpublished)]. We found a significant decrease in suppression time in the plasma of the subjects of group 4. However, regression analyses revealed—in contrast to our results concerning oxLDL or cholesterol concentration in serum/plasma—no significant correlation between suppression time and the expression of the CD36, CD68, CD40, TNFα or MnSOD gene in PBMCs.
Our study reveals that there is great evidence that in blood circulation proatherogenic lipids upregulate scavenger receptor expression, and proinflammatory and prooxidative processes in PBMCs. Moreover, our results show that serum HDL levels were inversely correlated with the expression of scavenger receptors (CD36, CD68) and oxidative stress/inflammation (CD40, TNFα, MnSOD, IL-1β) genes. HDL levels, however, are not suggested to affect the expression of these genes in PBMCs. Furthermore, we found no correlation between plasma triglyceride or homocysteine levels and the expression of the above-mentioned genes. The finding of in vitro investigations that homocysteine stimulates IL-1β and TNFα production by human peripheral blood monocytes or by monocyte-derived macrophages [40], cannot be supported by our study because the homocysteine concentrations were similar within the four groups under test, and there were no correlations found in the total or subgroups. In addition, there was no significant correlation between age and the expression of these genes in PBMCs with the exception of TNFα expression. In this context, in a group of elderly persons (aged 81 years) an increased plasma TNFα concentration was found compared to healthy young (aged 25 years) voluntary humans. In addition, the group with highest plasma TNFα concentration revealed a prevalence of atherosclerosis, however only with a weak correlation between plasma TNFα and total or LDL cholesterol concentration in the blood [41].
Our data confirm and extend data of others that sICAM-1 levels were increased in hyperlipidemic patients [42, 43] or smokers [44, 45], whereas sVCAM-1 concentrations were not different compared to normolipidemic subjects [42]. Although hyperlipidemia was found to be associated with increased levels of soluble CAMs, which were suggested as markers for atherosclerosis, aggressive lipid-lowering treatment had only limited effects on the CAM levels [43]. Regression analyses revealed—in contrast to our results concerning oxLDL or cholesterol concentration in serum/plasma—no significant correlation between sCAM concentration and the expression of the CD36, CD68, CD40, TNFα or MnSOD gene in PBMCs.
Taken together, our data suggest that hyperlipidemia, especially elevated plasma oxLDL and/or serum cholesterol levels, are candidate factors to enhance expression of the CD36, CD68, CD40, TNFα or MnSOD gene in PBMCs, while the expression of CD14—a monocyte marker and LPS receptor—and IL-1β, being not significantly different among the four groups under test, appears to be unaffected. Corresponding differences in gene expression in the PBMC of patients with cardiovascular risk factors might also expected on the protein level because we and others showed that LPS and oxidized low-density lipoproteins increase MnSOD, TNFα, CD36, or cyclooxygenase-2 (COX-2) expression on RNA and protein level in human monocytes [3–5, 12, 46, 47]. Increased proinflammatory activation of PBMCs of hyperlipidemic subjects without manifest vascular disease may be viewed as a potential prooxidant and proinflammatory stress marker for cardiovascular risk assessment [48]. Further studies in this context are warranted to address the expressions of the relevant genes at the protein level, their correlation with established circulating inflammatory mediators, such as CRP, and their potential to monitor antiarteriosclerotic therapy.
References
Nakagawa-Toyama Y, Yamashita S, Miyagawa J, Nishida M, Nozaki S, Nagaretani H, Sakai N, Hiraoka H, Yamamori K, Yamane T, Hirano K, Matsuzawa Y (2001) Localization of CD36 and scavenger receptor class A in human coronary arteries—a possible difference in the contribution of both receptors to plaque formation. Atherosclerosis 156:297–305
Depre C, Havaux X, Renkin J, Vanoverschelde JL, Wijns W (1999) Expression of inducible nitric oxide synthase in human coronary atherosclerotic plaque. Cardiovasc Res 41:465–472
Kinscherf R, Deigner HP, Usinger C, Pill J, Wagner M, Kamencic H, Hou D, Chen M, Schmiedt W, Schrader M, Kovacs G, Kato K, Metz J (1997) Induction of mitochondrial manganese superoxide dismutase in macrophages by oxidized LDL: its relevance in atherosclerosis of humans and heritable hyperlipidemic rabbits. FASEB J 11:1317–1328
Kinscherf R, Claus R, Wagner M, Gehrke C, Kamencic H, Hou D, Nauen O, Schmiedt W, Kovacs G, Pill J, Metz J, Deigner HP (1998) Apoptosis caused by oxidized LDL is manganese superoxide dismutase and p53 dependent. FASEB J 12:461–467
Bonaterra GA, Hildebrandt W, Bodens A, Sauer R, Dugi KA, Deigner HP, Droge W, Metz J, Kinscherf R (2005) Increased cyclooxygenase-2 expression in peripheral blood mononuclear cells of smokers and hyperlipidemic subjects. Free Radic Biol Med 38:235–242
Farmer JA, Torre-Amione G (2000) Atherosclerosis and inflammation. Curr Atheroscler Rep 4:92–98
Fruchart JC, Nierman MC, Stroes ES, Kastelein JJ, Duriez P (2004) New risk factors for atherosclerosis and patient risk assessment. Circulation 109(23 Suppl 1):III15–III19
Dhaliwal BS, Steinbrecher UP (1999) Scavenger receptors and oxidized low density lipoproteins. Clin Chim Acta 286:191–205
Boullier A, Bird DA, Chang MK, Dennis EA, Friedman P, Gillotre-Taylor K, Horkko S, Palinski W, Quehenberger O, Shaw P, Steinberg D, Terpstra V, Witztum JL (2001) Scavenger receptors, oxidized LDL, and atherosclerosis. Ann N Y Acad Sci 947:214–222
Takahashi K, Takeya M, Sakashita N (2002) Multifunctional roles of macrophages in the development and progression of atherosclerosis in humans and experimental animals. Med Electron Microsc 35:179–203
Tsukamoto K, Kinoshita M, Kojima K, Mikuni Y, Kudo M, Mori M, Fujita M, Horie E, Shimazu N, Teramoto T (2002) Synergically increased expression of CD36, CLA-1 and CD68, but not of SR-A and LOX-1, with the progression to foam cells from macrophages. J Atheroscler Thromb 9:57–64
Jovinge S, Ares MP, Kallin B, Nilsson J (1996) Human monocytes/macrophages release TNF-alpha in response to Ox-LDL. Arterioscler Thromb Vasc Biol 16:1573–1579
Janabi M, Yamashita S, Hirano K, Sakai N, Hiraoka H, Matsumoto K, Zhang Z, Nozaki S, Matsuzawa Y (2000) Oxidized LDL-induced NF-kappa B activation and subsequent expression of proinflammatory genes are defective in monocyte-derived macrophages from CD36-deficient patients. Arterioscler Thromb Vasc Biol 20(8):1953–1960
Hakkinen T, Karkola K, Yla-Herttuala S (2000) Macrophages, smooth muscle cells, endothelial cells, and T-cells express CD40 and CD40L in fatty streaks and more advanced human atherosclerotic lesions. Colocalization with epitopes of oxidized low-density lipoprotein, scavenger receptor, and CD16 (Fc gammaRIII). Virchows Arch 437:396–405
Schlittenhardt D, Schmiedt W, Bonaterra GA, Metz J, Kinscherf R (2005). Colocalization of oxidized low-density lipoprotein, caspase-3, cyclooxygenase-2, and macrophage migration inhibitory factor in arteriosclerotic human carotid arteries. Cell Tissue Res 322(3):425–435
Linton MF, Fazio S (2004) Cyclooxygenase-2 and inflammation in atherosclerosis. Curr Opin Pharmacol 4:116–123
Kovanen PT, Pentikainen MO (2003) Circulating lipoproteins as proinflammatory and anti-inflammatory particles in atherogenesis. Curr Opin Lipidol 14:411–419
Block G, Jensen C, Dietrich M, Norkus EP, Hudes M, Packer L (2004) Plasma C-reactive protein concentrations in active and passive smokers: influence of antioxidant supplementation. J Am Coll Nutr 23:141–147
Kinscherf R, Cafaltzis K, Roder F, Hildebrandt W, Edler L, Deigner HP, Breitkreutz R, Feussner G, Kreuzer J, Werle E, Michel G, Metz J, Dröge W (2003) Cholesterol levels linked to abnormal plasma thiol concentrations and thiol/disulfide redox status in hyperlipidemic subjects. Free Radic Biol Med 35:1286–1292
Lissi E, Pascual C, Del Castillo MD (1992) Luminol luminescence induced by 2,2′-azobis-(2-amidinopropane) thermolysis. Free Radic Res Commun 17:299–311
Amraei Davijani F (2005) Untersuchungen zur Bedeutung von oxidativem Stress bei Präeklampsie. Thesis Faculty of Chemistry and Pharmacy, University of Tuebingen
Hayden JM, Brachova L, Higgins K, Obermiller L, Sevanian A, Khandrika S, Reaven PD (2002) Induction of monocyte differentiation and foam cell formation in vitro by 7-ketocholesterol. J Lipid Res 43:26–35
Storz M, Zepter K, Kamarashev J, Dummer R, Burg G, Haffner AC (2001) Coexpression of CD40 and CD40 ligand in cutaneous T-cell lymphoma (mycosis fungoides). Cancer Res 61:452–454
Haversen LA, Baltzer L, Dolphin G, Hanson LA, Mattsby-Baltzer I (2003) Anti-inflammatory activities of human lactoferrin in acute dextran sulphate-induced colitis in mice. Scand J Immunol 57:2–10
Pfaffl MW, Horgan GW, Dempfle L (2002) Relative expression software tool (REST) for group-wise comparison and statistical analysis of relative expression results in real-time PCR. Nucleic Acids Res 30:e36
Pfaffl MW, Tichopad A, Prgomet C, Neuvians TP (2004) Determination of stable housekeeping genes, differentially regulated target genes and sample integrity: BestKeeper—Excel-based tool using pair-wise correlations. Biotechnol Lett 26:509–515
Pfaffl MW, Horgan GW, Vainshtein Y, Avery P (2005) http://rest.gene-quantification.info/
Horiuchi S, Sakamoto Y, Sakai M (2003) Scavenger receptors for oxidized and glycated proteins. Amino Acids 25:283–292
Dedoussis GV, Kaliora AC, Psarras S, Chiou A, Mylona A, Papadopoulos NG, Andrikopoulos NK (2004) Antiatherogenic effect of Pistacia lentiscus via GSH restoration and downregulation of CD36 mRNA expression. Atherosclerosis 174:293–303
Ramprasad MP, Terpstra V, Kondratenko N, Quehenberger O, Steinberg D (1996) Cell surface expression of mouse macrosialin and human CD68 and their role as macrophage receptors for oxidized low density lipoprotein. Proc Natl Acad Sci U S A 93:14833–14838
Han J, Zhou X, Yokoyama T, Hajjar DP, Gotto AM Jr, Nicholson AC (2004) Pitavastatin downregulates expression of the macrophage type B scavenger receptor, CD36. Circulation 109:790–796
Llaverias G, Noe V, Penuelas S, Vazquez-Carrera M, Sanchez RM, Laguna JC, Ciudad CJ, Alegret M (2004) Atorvastatin reduces CD68, FABP4, and HBP expression in oxLDL-treated human macrophages. Biochem Biophys Res Commun 318:265–274
Ogru E, Libinaki R, Gianello R, West S, Munteanu A, Zingg JM, Azzi A (2004) Modulation of cell proliferation and gene expression by alpha-tocopheryl phosphates: relevance to atherosclerosis and inflammation. Ann N Y Acad Sci 1031:405–411
Munteanu A, Zingg JM, Ogru E, Libinaki R, Gianello R, West S, Negis Y, Azzi A (2004) Modulation of cell proliferation and gene expression by alpha-tocopheryl phosphates: relevance to atherosclerosis and inflammation. Biochem Biophys Res Commun 318:311–316
Scott J (2004) Pathophysiology and biochemistry of cardiovascular disease. Curr Opin Genet Dev 14:271–279
Harding SA, Sarma J, Josephs DH, Cruden NL, Din JN, Twomey PJ, Fox KA, Newby DE (2004) Upregulation of the CD40/CD40 ligand dyad and platelet–monocyte aggregation in cigarette smokers. Circulation 109:1926–1929
Hsu HY, Chiu SL, Wen MH, Chen KY, Hua KF (2001) Ligands of macrophage scavenger receptor induce cytokine expression via differential modulation of protein kinase signaling pathways. J Biol Chem 276:28719–28730
Michowitz Y, Goldstein E, Roth A, Afek A, Abashidze A, Ben Gal Y, Keren G, George J (2005) The involvement of tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) in atherosclerosis. J Am Coll Cardiol 45:1018–1024
Martin-Ventura JL, Blanco-Colio LM, Gomez-Hernandez A, Munoz-Garcia B, Vega M, Serrano J, Ortega L, Hernandez G, Tunon J, Egido J (2005) Intensive treatment with atorvastatin reduces inflammation in mononuclear cells and human atherosclerotic lesions in one month. Stroke 36:1796–1800
Dalal S, Parkin SM, Homer-Vanniasinkam S, Nicolaou A (2003) Effect of homocysteine on cytokine production by human endothelial cells and monocytes. Ann Clin Biochem 40:534–541
Bruunsgaard H, Skinhoj P, Pedersen AN, Schroll M, Pedersen BK (2000) Ageing, tumour necrosis factor-alpha (TNF-alpha) and atherosclerosis. Clin Exp Immunol 121:255–260
Karasek D, Vaverkova H, Halenka M, Budikova M, Novotny D (2005) Soluble cell adhesion molecules s-VCAM-1 and s-ICAM-1 in subjects with familial combined hyperlipidemia. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 149(1):101–108
Hackman A, Abe Y, Insull W Jr, Pownall H, Smith L, Dunn K, Gotto AM Jr, Ballantyne CM (1996) Levels of soluble cell adhesion molecules in patients with dyslipidemia. Circulation 93(7):1334–1338
Demerath E, Towne B, Blangero J, Siervogel RM (2001) The relationship of soluble ICAM-1, VCAM-1, P-selectin and E-selectin to cardiovascular disease risk factors in healthy men and women. Ann Hum Biol 28(6):664–678
Winkelmann BR, Boehm BO, Nauck M, Kleist P, Marz W, Verho NK, Ranjith N, Kneissl G (2001) Cigarette smoking is independently associated with markers of endothelial dysfunction and hyperinsulinaemia in nondiabetic individuals with coronary artery disease. Curr Med Res Opin 17(2):132–141
Feng J, Han J, Pearce SF, Silverstein RL, Gotto AM Jr, Hajjar DP, Nicholson AC (2000) Induction of CD36 expression by oxidized LDL and IL-4 by a common signaling pathway dependent on protein kinase C and PPAR-gamma. J Lipid Res 41(5):688–696
Pontsler AV, St Hilaire A, Marathe GK, Zimmermann GA, McIntyre TM (2002) Cyclooxygenase-2 is induced in monocytes by peroxisome proliferators activated receptor gamma and oxidized alkyl phospholipids from oxidized low density lipoprotein. J Biol Chem 277(15):13029–13036
Brennan ML, Hazen SL (2003) Amino acid and protein oxidation in cardiovascular disease. Amino Acids 25:365–374
Acknowledgement
This work was supported in part by the “Karl and Lore Klein” foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bonaterra, G.A., Hildebrandt, W., Bodens, A. et al. Increased gene expression of scavenger receptors and proinflammatory markers in peripheral blood mononuclear cells of hyperlipidemic males. J Mol Med 85, 181–190 (2007). https://doi.org/10.1007/s00109-006-0117-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-006-0117-6