Abstract
Glutathione (GSH) is one of the most important defense mechanisms against oxidative stress in the respiratory epithelial lining fluid. Considering that GSH secretion in respiratory cells has been postulated to be at least partially electrogenic, and that the mucoregulator S-carbocysteine lysine salt monohydrate (S-CMC-Lys) can cause an activation of epithelial Cl− conductance, the purpose of this study was to verify whether S-CMC-Lys is able to stimulate GSH secretion. Experiments have been performed by patch-clamp technique, by high-performance liquid chromatography (HPLC) assay, and by Western blot analysis on cultured lines of human respiratory cells (WI-26VA4 and CFT1-C2). In whole-cell configuration, after cell exposure to 100 μM S-CMC-Lys, a current due to an outward GSH flux was observed, which was inhibitable by 5-nitro-2-(3-phenylpropylamino)-benzoate and glibenclamide. This current was not observed in CFT1-C2 cells, where a functional cystic fibrosis transmembrane conductance regulator (CFTR) is lacking. Inside-out patch-clamp experiments (GSH on the cytoplasm side, Cl− on the extracellular side) showed the activity of a channel, which was able to conduct current in both directions: the single channel conductance was 2–4 pS, and the open probability (Po) was low and voltage-independent. After preincubation with 100 μM S-CMC-Lys, there was an increase in Po, in the number of active channels present in each patch, and in the relative permeability to GSH vs Cl−. Outwardly directed efflux of GSH could also be increased by protein kinase A, adenosine 5′-triphosphate, and cyclic adenosine monophosphate (cAMP) added to the cytoplasmic side (whole-cell configuration). The increased secretion of GSH observed in the presence of S-CMC-Lys or 8-bromoadenosine-3′,5′-cyclic monophosphate was also confirmed by HPLC assay of GSH on a confluent monolayer of respiratory cells. Western blot analysis confirmed the presence of CFTR in WI-26VA4 cells. This study suggests that S-CMC-Lys is able to stimulate a channel-mediated GSH secretion by human respiratory cells: electrophysiological and pharmacological characteristics of this channel are similar to those of the CFTR channel.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The anionic tripeptide glutathione (GSH) is the most important antioxidant in the fluids lying on the respiratory epithelia, and its concentration in the airway surface liquid is about 50–100 times higher than that observed in other extracellular liquid [1, 2]. Extracellular GSH can defend against free radicals formation [3] as a result of invading neutrophils during inflammatory processes. GSH level could be due to a number of factors, such as enhanced consumption or reduced removal, but most of it should be due to cellular secretions, which implies partly unidentified mechanisms of transport across the apical membrane of epithelial cells. GSH transport is partially dependent from membrane potential [4], and in some nonrespiratory cell types (e.g., hepatocytes), GSH efflux is possibly carried through members of the multidrug resistance protein (MRP) family [5]. Low levels of GSH in air surface liquid have been observed in cystic fibrosis (CF) patients [6, 7], suggesting a possible role of cystic fibrosis transmembrane conductance regulator (CFTR) anion channel in GSH secretion [7–9]. CF patients with chronic pulmonary inflammation exhibit an oxidative stress, which is likely increased by the reduced antioxidant capacity of air surface liquid consequent to the decreased GSH content [7, 10]. CFTR could thus be the mechanism directly responsible for GSH transport [7, 9] or could be a regulator of this [11].
Research performed in the past by patch-clamp technique [12] suggested a role of S-carbocysteine lysine salt monohydrate (S-CMC-Lys) in activating Cl− conductance in human respiratory cells (WI-26VA4 cells). S-CMC-Lys is a mucoactive drug used in the treatment of different respiratory diseases, which is able not only to correct the balance between sialo- and fuco-mucins [13, 14] but also to modulate Cl− and water secretions [15], thus improving the removal of mucus. In particular, in human respiratory epithelia, S-CMC-Lys seems to modulate an anion channel whose electrophysiological characteristics are compatible with those of the CFTR channel [12, 16].
The aim of this study was to verify, by patch-clamp techniques on human respiratory cells, the mechanisms of the electrogenic secretion of GSH, the possible involvement of CFTR in this process, and, primarily, the effect of S-CMC-Lys on GSH secretion. The extent of this effect has also been evaluated by high-performance liquid chromatography (HPLC) assays of GSH in air surface liquid.
Materials and methods
Drugs and chemicals
Eagle’s minimum essential medium (MEM), F12 Ham’s nutrient mixture medium, N-[2-hydroxyethyl]-piperazine-N′-[2-ethanesulfonic acid] (HEPES), N-Tris[hydroxymethyl]-methyl-2-aminoethane-sulfonic acid (TES), N-methyl-d-glucamine (NMG), ethylenediaminetetraacetic acid (EDTA), ethyleneglycol-bis-[aminoethylether]-N,N,N′,N′-tetraacetic acid (EGTA), hormones, adenosine 5′-triphosphate (ATP), 8-bromoadenosine-3′,5′-cyclic monophosphate (8-Br-cAMP), protein kinase A bovine heart (PKA), 5-nitro-2-(3-phenylpropylamino)-benzoate (NPPB), glibenclamide (N-p-[2-(5-chloro-2-methoxybenzamido)ethyl]benzensulfonyl-N′-cyclohexylurea), theophylline, acivicin (α-amino-3-chloro-4,5-dihydro-5-isoxazoleacetic acid), Ellman’s reagent [5,5′-dithiobis(2-nitrobenzoic acid)], and GSH were purchased from Sigma (St. Louis, MO, USA). S-CMC-Lys was purchased from Dompé spa (Milan, Italy). The lactate dehydrogenase (LDH) liquid assay kit was purchased from Sentinel CH s.r.l. (Milan, Italy).
Cell lines and solutions for cell maintenance
We used a human respiratory cell line (WI-26VA4) supplied by ATCC-LGC Promochem (UK). The cells were placed in a small Petri dish and incubated (37°C; 5% CO2) in a culture medium (MEM, +2% l-glutamine, +10% fetal bovine serum) for 44–48 h to attain nearly 70% confluence. During the long-term exposure to S-CMC-Lys or 8-Br-cAMP, the Petri dishes were kept in an incubator, except during the electrophysiological measurements. During the patch-clamp experiments (before the seal formation), cells were maintained in Hank’s balanced salt solution or, when specified, in the Krebs–Henseleit solution containing the following (mM): 110 NaCl, 4.7 KCl, 1.2 MgSO4, 1.2 KH2PO4, 2.5 CaCl2, 10 TES, 5 glucose, and 50 mannitol (pH 7.4).
We also used human tracheobronchial epithelial cells, both CF (CFT1-C2, homozygous for F508 deletion of the CFTR gene [17]) and functionally corrected for CFTR (LCFSN-infected CFT1 cells [18]). These cells were grown in the same conditions as WI-26VA4, except for the culture medium (F12 Ham’s nutrient mixture medium supplemented with hormones and growth substances, as reported [17]). CFT1-C2 and LCFSN-infected CFT1 cell lines were a kind gift from James Yankaskas (The University of North Carolina at Chapel Hill, Chapel Hill, NC, USA).
Solutions for whole-cell configuration
The micropipette solution contained the following (mM): 143 NMGglutathione, 3 theophylline, 5 glucose, 10 HEPES/NMG (pH 7.2), 1.9 CaCl2, and 3 EGTA (free [Ca2+] of 2×10−7 M). The symmetrical extracellular solution contained (mM): 143 NMGglutathione, 5 glucose, 10 HEPES/NMG (pH 7.4), 1 MgCl2, and 1.8 CaCl2. NMGCl replaced NMGglutathione in Cl− asymmetrical solution. The experiments were conducted on cells in control condition, on cells pretreated with 100 μM S-CMC-Lys, and in the presence of 150 U/ml PKA, 1 mM ATP, and 250 μM cAMP in the pipette solution.
Solutions for single-channel recording
In cell-attached configuration, the bath solution was Krebs–Henseleit solution (pH 7.4). The micropipette solution (cell-attached and inside-out configurations) contained (mM): 145 NMGCl, 10 HEPES/NMG (pH 7.4), 1.8 CaCl2, and 1 MgCl2. In inside-out configuration, the bath symmetrical solution contained (mM): 145 NMGCl, 10 HEPES/NMG (pH 7.2), 3 EGTA, 0.05 MgCl2, and 1.9 CaCl2 (free [Ca2+] of 2×10−7 M). In the bath asymmetrical solution, the 145 mM NMGCl was substituted with NMGglutathione. All intracellular solutions contained 3 mM theophylline. The experiments were conducted on cells in control condition and pretreated with S-CMC-Lys (100 μM for at least 5 h).
Patch-clamp technique
Patch-clamp technique and relative statistics were applied as reported [19]. In whole-cell configuration, the resistances of the microelectrodes (\(R_{{\mu {\text{el}}}} \)) and of the seals (Rs) were 2–8 MΩ and 1–2 GΩ, respectively. Signals were filtered at 5 kHz with an eight-pole Bessel filter. In single-channel recording, the \(R_{{\mu {\text{el}}}} \) was 15–18 MΩ, and Rs was 15–50 GΩ. Signals were filtered at 0.2 kHz (eight-pole Bessel filter). In whole-cell and cell-attached configurations, potential differences were expressed as overall potential differences, considering the junction potential, the holding potentials, and the cell membrane potential (pdcm) (cell-attached only). The bath was grounded with an Ag/AgCl electrode immersed in a 1 M KCl agar bridge.
HPLC assays
High-performance liquid chromatography assays of GSH were performed as for the method proposed by Raggi et al. [20]. The measurements were performed on the incubation medium (Eagle’s MEM without phenol red + 250 μM acivicin) of cells at 90–100% confluence, either in control conditions or after a 5-h incubation with 100 μM S-CMC-Lys or 250 μM 8-Br-cAMP. To avoid the oxidation of GSH, the medium was deproteinized before the injection: 1 ml medium was diluted in 1 ml perchloric acid (HClO4) and centrifuged (3,100×g, 15 min, 4°C); a 1.75 M K3PO4 solution was added to the supernatant in a 5:0.9 ratio; the solution was then left in ice bath for 15 min, and the perchlorate precipitate was filtered off.
The HPLC system included a pump (Jasco PU-980), a UV detector (Jasco UV-975), a degassing unit (Gastorr GT-103), and a Peltier-thermostatted (20°C) 125×4 mm reverse-phase column (5 μm; LiChrospher 100 RP-18, Merck). The employed software was ChromCard (Thermo Electron). The GSH concentration was read at 280 nm after a derivatization reaction of GSH with Ellman’s reagent.
Cell viability
Lactate dehydrogenase release from cells was used as an index of cell damage or death, employing a LDH assay test kit (Sentinel Diagnostics). The quantity of LDH released by the cells into the medium was measured by the decrease in the absorbance at 340 nm for β-NADH2 disappearance at a spectrophotometer (Ultrospec 3000, Pharmacia Biotech). Supernatants were collected from plates grown in experimental conditions. Results were expressed as the percentage of total LDH activity in the extracellular medium where cells were lysed with Triton X-100.
Western blot experiments
A confluent layer of WI-26VA4 cells from a 10 cm plate was lysed for total protein extraction in 1 ml of lysis buffer [20 mM Tris–HCl, pH 7.5, 150 mM NaCl, 1 mM EDTA, 1% NP40, 0.2 mM phenylmethylsulfonyl fluoride, protease cocktail (complete, EDTA-free, protease inhibitor cocktail tablets; Roche, Mannheim, Germany), and 0.08% deoxycholic acid], incubated at 4°C for 30 min, and centrifuged at 13,000×g for 30 min. The supernatant was collected, and the protein concentration was measured using the Bradford method with bovine serum albumin as the standard.
Proteins (100 μg) were solubilized in sample buffer [50 mM Tris–HCl, 2% sodium dodecyl sulfate (SDS), 0.1% bromophenol blue, and 10% glycerol], resolved on a 7.5% SDS–polyacrylamide gel, and electrophoretically transferred to Immuno-Blot polyvinylidene difluoride membranes (Bio-Rad Laboratories, Italy). The membranes were blocked with 5% nonfat dried milk in TBS-Tween (150 mM Tris, pH 7.5, 150 mM NaCl, 0.1% Tween 20) for 1 h at RT plus 3 h at 4°C and were incubated with a polyclonal antibody to CFTR (1:1,000, N-term, H-182, Santa Cruz Biotechnology, Inc., Santa Cruz, CA, USA) in TBS plus 1% nonfat dried milk, overnight at 4°C. The membrane was washed three times in TBS-Tween for 15 min and once in TBS for 15 min, and the bound antibody was detected by the enhanced chemiluminescence procedure (Amersham Corp.) using horseradish peroxidase-conjugated goat anti-rabbit IgG diluted 1:4,000 in TBS plus 1% nonfat dried milk.
Total protein extractions were done from control plates (incubated for 5 h in medium plus 250 μm acivicin), S-CMC-Lys-treated plates (100 μM S-CMC-Lys for 5 h and 250 μM acivicin), and cAMP-treated plates (250 μM 8-Br-cAMP for 5 h and 250 μM acivicin).
Statistics
The experimental values are expressed as mean±SEM of n experiments. Student’s t test was used (with unpaired data unless otherwise specified) for the statistical analysis. Statistical difference was accepted for P values less than 0.05. Best fittings were performed by linear and nonlinear regression analyses. One-way ANOVA was used to analyze multiple data from HPLC experiments, corrected with Bonferroni posttest.
Results
Anionic currents measured in whole-cell configurations
Whole-cell experiments were carried out with high GSH concentration (143 mM) in the pipette, i.e., on the intracellular side, with the aim of showing the occurrence of electrogenic GSH secretion by human respiratory epithelium cells. Experiments were made in control conditions (Fig. 1a–e) and after preincubation with 100 μM S-CMC-Lys (Fig. 2a–e). Additional experiments were performed with PKA (150 U/ml), ATP (1 mM), and cAMP (250 μM) in the pipette solution (Fig. 3a–d) to characterize the channel mediating GSH secretion. All intracellular solutions had a pH of 7.2 (buffered by HEPES/NMG).
Anion currents in WI-26VA4 human respiratory cells, whole-cell configuration. a Impulse protocol; b whole-cell currents in symmetrical GSH solution ([GSH]in=[GSH]out=143 mM); c in asymmetrical GSH solution ([GSH]in=143 mM; [GSH]out=0 mM; [Cl−]out=148.6 mM); d in asymmetrical GSH solution and in the presence of 10−4 M glibenclamide; e in asymmetrical GSH solution and in the presence of 10−4 M NPPB. f Current–voltage (I/V) relationship for the asymmetrical effect (Δ: asymmetrical, ▪: symmetrical; mean±SEM, n=10); g for the inhibitory effect (Δ: asymmetrical, ▾: glibenclamide, ○: NPPB; mean±SEM, n=6)
Anion currents in WI-26VA4 cells after incubation with 100 mM S-CMC-Lys, whole-cell configuration. a Impulse protocol; b whole-cell currents in symmetrical GSH solution ([GSH]in=[GSH]out=143 mM); c in asymmetrical GSH solution ([GSH]in=143 mM; [GSH]out=0 mM; [Cl−]out=148.6 mM); d in asymmetrical GSH solution and in the presence of 10−4 M glibenclamide; e in asymmetrical GSH solution and in the presence of 10−4 M NPPB. f Current–voltage (I/V) relationship for the asymmetrical effect (Δ: asymmetrical, ▪: symmetrical; mean±SEM, n=7); g for the inhibitory effect (Δ: asymmetrical, ▾: glibenclamide, ○: NPPB; mean±SEM, n=3)
Anion currents in WI-26VA4 cells in the presence of 150 U/ml PKA, 1 mM ATP, and 250 μM cAMP in micropipette solution, whole-cell configuration. a Impulse protocol; b whole-cell currents in symmetrical GSH solution ([GSH]in=[GSH]out=143 mM); c asymmetrical GSH solution ([GSH]in=143 mM; [GSH]out=0 mM; [Cl−]out=148.6 mM); d in asymmetrical GSH solution and in the presence of 10−4 M NPPB. e Current–voltage (I/V) relationship for the asymmetrical effect (Δ: asymmetrical, ▪: symmetrical; mean±SEM, n=13); f for the inhibitory effect (Δ: asymmetrical, •: NPPB; mean±SEM, n=9)
I/V relationships shown in Fig. 1f,g were obtained in symmetrical and asymmetrical GSH solutions (intracellular side GSH 143 mM, pH 7.2, extracellular side GSH 0 mM and Cl− 148.6 mM, pH 7.4; both solutions buffered by HEPES/NMG; Fig. 1f) and in the presence (extracellular side) of two anion channel inhibitors: glibenclamide (100 μM) and NPPB (100 μM) (asymmetrical GSH solutions; Fig. 1g). In symmetrical GSH solutions (Fig. 1b,f), a very small current was recorded, both at positive and negative potentials (0.04±0.01 nA at +94.6 mV and −0.03±0.01 nA at −105.4 mV, n=10). In asymmetrical GSH solutions, the inward current was still very small, but the outward current was higher (from 0.04±0.01 nA at +94.6 mV to 0.30±0.09 nA at +90.6 mV, P<0.01, n=10) and sustained by a Cl− efflux. The resulting outward rectification was consequently due to the Cl− permeability, which was higher than that of intracellular GSH. The reversal potential (Vrev) recorded in these conditions was shifted towards the Nernst equilibrium potential for Cl−. By means of the reversal potential observed (−53.3±4.6 mV, n=10), it was possible to calculate a GSH/Cl− permeability ratio (Pglutathione/PCl) of 0.10±0.02 (n=10).
In addition, the outward current—that was the one ascribable to the Cl− cellular uptake—was inhibited by NPPB (0.1 mM; Fig. 1e,g) by 76.6% at about 90 mV (from 0.30±0.09 nA at +90.6 mV to 0.07±0.03 nA, P<0.05, n=6). The outward current observed in the presence of glibenclamide was not statistically lower than control. The inhibitors did not seem to significantly affect negative currents (outward GSH flux), suggesting that those currents were at least partially due to leakage or unspecific membrane conductances.
In contrast, after incubation with S-CMC-Lys, an inward (negative) current higher than control was observed (Fig. 2b,c,f), both in symmetrical (−0.20±0.06 nA at −94.4 mV, n=7) and in asymmetrical solutions (−0.24±0.06 nA at −109.4 mV, n=7). The Vrev shift (now −31.1±5.6 mV, n=7) led to a rise in PGSH/PCl from the control value of 0.1 to 0.30±0.04 (n=7). The increase in the negative currents (attributable to the exit of GSH from the cell) and in the GSH relative permeability denoted a positive action of S-CMC-Lys on GSH secretion. Unlike in control conditions, NPPB and glibenclamide inhibited both the positive and the negative currents (Fig. 2d,e,g), showing an inhibition of GSH secretion by the Cl− channel inhibitors.
When PKA, cAMP, and ATP were in the pipette (intracellular side), with symmetrical solutions (Fig. 3b,e), we recorded a current, which was higher than those of the two former situations (0.63±0.19 nA at +92.6 mV, n=13, P<0.05 against 0.04±0.01 nA, n=10 in control conditions, P>0.05 against 0.28±0.05 nA, n=7 in the presence of S-CMC-Lys; and −0.55±0.17 nA at −107.4 mV, n=13, P<0.01 against −0.03±0.01 nA, n=10 in control conditions, at −105.4 mV, P>0.05 against −0.22±0.06 nA, n=7, in the presence of S-CMC-Lys). Substitution of the extracellular symmetrical solution with the asymmetrical one produced a statistically significant increase in outward currents (from 0.63±0.19 nA in symmetrical solutions to 2.83±0.71 nA in asymmetrical solutions, P<0.01, n=13). Moreover, in asymmetrical solutions, we recorded a shift of Vrev towards the theoretical Nernst value, in the hypothesis that the channel was mainly selective for Cl− (−91.2 mV). The observed value (−43.5±2.62 mV, n=13) allowed the computation of a PGSH/PCl of 0.17±0.02 (n=13), which was significantly higher than the PGSH/PCl obtained in control conditions.
In addition, we performed preliminary experiments using CFT1-C2 and LCFSN-infected CFT1 cells in similar conditions (whole-cell configuration, intracellular side GSH 143 mM, extracellular side GSH 0 mM and Cl− 148.6 mM). On S-CMC-Lys-pretreated CFT1-C2 cells, we observed no inward currents (outward GSH efflux) significantly different (at voltages from −30 to −120 mV) with respect to those obtained after 100 μM NPPB treatment (−0.057±0.029 nA at −100 mV, n=9, n.s., against −0.048±0.018 nA in the presence of 100 μM NPPB, n=9). In contrast, using LCFSN-infected CFT1 cells, we observed currents giving an I/V relationship similar to that shown in Fig. 2g (−0.337±0.085 nA at −100 mV, n=14, P<0.05, against −0.118±0.024 nA, n=14 in the presence of 100 μM NPPB; 0.473±0.074 nA, n=14 at 80 mV, P<0.01, against 0.202±0.036 nA, n=14 in the presence of 100 μM NPPB). Currents obtained from LCFSN-infected CFT1 cells were significantly higher (P<0.05) than those obtained from CFT1-C2 cells at all the voltages from −140 to −60 mV and from 20 to 80 mV.
Single-channel experiments
Cell-attached experiments were performed on both control cells and cells pretreated (5 h) with S-CMC-Lys 100 μM in the incubation medium (145 mM NMGCl in the pipette, pH 7.4, buffered by HEPES/NMG, and Krebs–Henseleit solution as external solution, pH 7.4, buffered by TES.
Using untreated cells (Fig. 4b), the presence of a small conductance (5.1±2.2 pS, n=5) anion channel was observed in 75% of the experiments, with voltage-independent Po (mean value 0.084±0.013, n=8, voltage ranging from −166 to +74 mV; Fig. 4d). In the remaining 25% of the experiments, no small conductance anion channels were observed. Higher conductance (20/40 pS) outwardly rectifying anion channels insensitive to both S-CMC-Lys and cAMP have sporadically been seen, as already reported [12]. The density of active channels (calculated as the ratio between the number of active channels observed and the number of patches used, NC/p) approached 1.8±0.4, n=13 (Fig. 4c). The Vrev was −39±6.6 mV, n=5, a value consistent with the behavior of a Cl− channel: this ion was at about the electrochemical equilibrium, given that the electrical membrane potential, measured in previous experiments using conventional electrodes [12], was −46±2.6 mV (n=15, a value not statistically different from the observed Vrev). In S-CMC-Lys-incubated cells (Fig. 4b), an outwardly rectifying anion channel with single-channel conductance of 4.8±1.4 pS (n=5) was again observed. The presence of anion channels was detected in all the seals. With respect to control conditions, there was a significant (P<0.01) increase in Po (still voltage-independent though—mean value 0.157±0.012, n=5, from −156 to +84 mV; Fig. 4d) and an increase in the number of active channels per patch (3.5±0.43, P<0.01 compared to control conditions; Fig. 4c). The Vrev was shifted towards less negative values (−18.8±6.2 mV), suggesting a Cl− movement out of the cell at the resting membrane potential (measured as above but in S-CMC-Lys incubation conditions and resulting to −36±2.1 mV, n=12) following the channel activation.
Effect of S-CMC-Lys (100 μM) treatment on anion channel activity in WI-26VA4 cells, cell-attached configuration. a Tracings observed at −166 mV in control (upper tracing) and S-CMC-Lys-treated cells (lower tracing). b Current–voltage (I/V) relationship for control condition (▪, mean±SEM, n=5) and S-CMC-Lys incubation condition (□, mean±SEM, n=5). c Effects of S-CMC-Lys treatment on the number of channels observed/number of patches (NC/p); d on open probability (Po). *Data are significantly different from control (P<0.05)
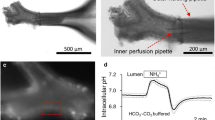
In inside-out experiments (145 mM GSH on the intracellular side, pH 7.2, and Cl− in the pipette, pH 7.4, both solutions buffered by HEPES/NMG), intracellular solutions contained 3 mM theophylline to prevent the dephosphorylation of the channel, as previously described [12]. In control cells with asymmetrical solutions, an outwardly rectifying anion channel was observed (Fig. 5b), with voltage-independent Po (mean value 0.105±0.02, n=9, voltages from −128 to +112 mV; Fig. 5d) and single-channel conductance of 3.45±0.62 pS (n=7). The number of active channels per patch (NC/p) was 1.9±0.4 (n=13; Fig. 5c). Both Po and NC/p values were not significantly different from those obtained in cell-attached or untreated cells. The Vrev obtained in inside-out experiments was −54.6±5.9 mV (n=7), far from the Nernst theoretical Vrev predicted for a channel exclusively selective for Cl−. On account of the Vrev, the GSH/Cl− relative permeability ratio (Pglutathione/PCl) was computed to be 0.101±0.025 (n=7), not a significantly different value compared with that obtained under the same conditions in whole-cell experiments.
Effect of S-CMC-Lys (100 μM) treatment on anion channel activity in WI-26VA4 cells, inside-out configuration. a Tracings observed at −130 mV in control (upper tracing) and S-CMC-Lys-treated cells (lower tracing). b Current–voltage (I/V) relationship for control condition (●, mean±SEM, n=5) and in S-CMC-Lys incubation condition (○, mean±SEM, n=5). c Effects of S-CMC-Lys treatment on the number of channels observed/number of patches (NC/p); d on open probability (Po). *Data are significantly different from control (P<0.05)
Similar experiments were performed in S-CMC-Lys-incubated cells, and again, an increase in the mean Po value was observed for the examined range of potentials (0.141±0.01, n=7; Fig. 5d), as well as an increased number of active channels per patch (5.3±0.5, n=7; Fig. 5c). In the same conditions, a shift of the Vrev towards less negative values (−35.7±7.0, n=6; Fig. 5b) was also noticed, giving a Pglutathione/PCl permeability ratio of 0.29±0.09 (n=6), which implies a rise in GSH permeability in the presence of S-CMC-Lys.
Cell viability
We assessed the effect of S-CMC-Lys on cell viability by performing a LDH release assay upon LCFSN-infected CFT1 cells after incubation with S-CMC-Lys or in control conditions. S-CMC-Lys incubation induced no significant increase in LCFSN-infected CFT1 cells (5.77±1.15% of total LDH, n=4) compared to control (13.60±2.94% of total LDH, n=4).
HPLC assay of secreted GSH
The injection of standards reveals a peak at 11 min, representing GSH-Ellman. Its area variations are directly proportional to changes in the GSH concentration. Results obtained by injecting samples of the incubation medium from S-CMC-Lys-treated cells seem to point to the presence of a peak between 10 and 11 min, corresponding to GSH.
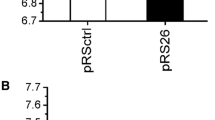
Calculated GSH concentration in the incubation medium after 5 h was in the range of 7–10 μM (n=6). HPLC assay showed that, both in S-CMC-Lys (n=6) and in 8-Br-cAMP (n=4) preincubation conditions, WI-26VA4 cells secreted a significantly higher amount of GSH than in control conditions (n=4; Fig. 6). The fluxes are expressed relative to the amount of total proteins present in the support from which the medium was taken for assays.
HPLC assay of extracellular glutathione secreted by WI-26VA4 cell monolayer. The cells were incubated for 5 h in a culture medium in the presence of 100 μM S-CMC-Lys (T1, mean±SEM, n=7) or 250 μM 8-Br-cAMP (T2, mean±SEM, n=5) or in control condition (C, mean±SEM, n=7). Data are significantly different from control (*P<0.05)
Western blot analysis
We studied the presence of CFTR protein in freshly isolated human respiratory epithelial cells (WI-26VA4) with rabbit polyclonal antibody raised against the amino terminus of CFTR (H-182, Santa Cruz Biotechnology). Total protein extract was obtained from WI-26VA4 control cells (Fig. 7, lane C) or WI-26VA4 cells incubated for 5 h in the presence of S-CMC-Lys (Fig. 7, lane S) or 8-Br-cAMP (data not shown). A 170-kDa band corresponding to the expected molecular mass of mature CFTR (band C) and a lower band corresponding to the unglycosylated form of CFTR (band B) were detected [21, 22] in both protein preparations. The quantity of CFTR protein was not affected by either S-CMC-Lys or 8-Br-cAMP incubation.
Discussion
Cell-attached data and whole-cell currents confirmed that, as previously proved [12], the incubation of human respiratory epithelia cells with S-CMC-Lys increases the activity (intensification of the cell membrane overall current, rise in Po, and in active channel density) of a small conductance anion channel. Cell-attached configuration, even though the most similar to physiological conditions, is hardly a functional condition to illustrate the electrogenical GSH secretion, given the difficulty to attain exact intracellular GSH concentrations. For such purpose, better results can be obtained in whole-cell and inside-out configuration experiments performed with high GSH concentrations on the cytoplasmic side. The use of asymmetrical solutions (GSH on intracellular side, Cl− on the extracellular side) was favored to rule out the possible effects of an anomalous extracellular Cl− concentrations on the activity of the channels. In control conditions (no cAMP or S-CMC-Lys pretreatment of cells) and in whole-cell configuration, the inward current, ascribable to the GSH efflux from the cell, is very small, both in symmetrical and asymmetrical solutions, indicating an apparently undetectable electrogenic secretion of the thiole. In inside-out configuration experiments, a channel with low apparent GSH permeability (PGSH/PCl=0.10), low Po, and low active channel density was also observed. Such values could be affected by the loss of possible cytoplasmic proteins regulating the channel. Electrophysiological data are in agreement with the results of HPLC assays for secreted GSH, suggesting the presence of a small GSH secretion also in the presence of intact cells. It must be remembered that not all the GSH secretion is necessarily electrogenic. Some ABC family members thought to mediate GSH flux, e.g., MRP1 and MRP2/cMOAT, were shown, in respiratory epithelia, to be localized on the basolateral membrane [23] or expressed, although at a very low level [24]. Inward (GSH-dependent) currents recorded in the whole-cell configuration rise when the cells are pretreated with S-CMC-Lys. The shift of the reversal potential (Vrev) on the passage between symmetrical and asymmetrical solutions, as well as NPPB and glibenclamide inhibition, corroborates the anionic nature of the channel. Compared to control conditions, pretreatment with S-CMC-Lys also produced an increase in the PGSH/PCl (0.29). Inside-out experiments confirmed an increase in GSH permeability when cells were pretreated with S-CMC-Lys (PGSH/PCl rises to 0.29). The increase in Po and in the active channel density is in agreement both with the overall current intensification detected in whole-cell configuration and with the growth of GSH secretion assayed in intact cells by HPLC. In whole-cell configuration and in the presence of PKA, cAMP, and ATP on the cytoplasmic side, an activation takes place both of the inward (due to GSH) and of the outward (due to Cl−) current. Both pretreatment with S-CMC-Lys and the presence of PKA + cAMP + ATP at the intracellular side led to a rise in PGSH/PCl. This suggests that S-CMC-Lys stimulates the electrogenic secretion of GSH by acting upon the very channel activated by PKA + cAMP + ATP, presumably CFTR. Supporting this possibility, NPPB (an inhibitor effective on many Cl− channels) and glibenclamide (a relatively CFTR-specific inhibitor) inhibited the inward (negative) S-CMC-Lys-activated currents. Furthermore, the presence of CFTR in these WI-26 VA4 cells was verified by Western blot experiments. Preliminary experiments performed (in asymmetrical GSH solution) on S-CMC-Lys-pretreated CFT1-C2 cells revealed that no electrogenic GSH secretion (inward current) was observed in the presence of homozygotic ΔF508 CFTR. On the contrary, using S-CMC-Lys-pretreated CFT1 cells corrected for CFTR, an inward (GSH-dependent) and an outward (Cl−-dependent) current could be observed. These results confirm the importance of CFTR in the appearance of the current and demonstrate that GSH-sustained currents are not associated to a specific respiratory cell line.
These data are also consistent with present and previous data [12] on CFTR-mediated Cl− currents, which can be stimulated by S-CMC-Lys.
As a conclusion, GSH can be secreted in an electrogenic way, which seems mediated or dependent by CFTR. The channel involved in GSH secretion presents some CFTR anion channel electrophysiological characteristics since it is cAMP- and S-CMC-Lys-active and NPPB- and glibenclamide-inhibitable, with low single channel conductance and no voltage-dependent Po.
A GSH electrogenic secretion through a channel was already suggested [9], as well as the involvement of CFTR [9, 25], though its role has not been elucidated yet. Some hypothesize that the CFTR protein just plays a regulatory role [11], suggesting a GSH secretion not directly mediated by CFTR. Furthermore, taking into account the structural similarity between CFTR and the related ABC transporters MRP1 and MRP2, the export of GSH could be due, at least theoretically, to functional aspects of CFTR, which would be very different from those observed as a Cl− channel. Our single-channel data, though, referring to GSH export, rule out this possibility, pointing out the involvement of a true channel.
The high permeability to GSH shown here is in agreement with the significant permeability of CFTR for a broad range of large organic anions [26], and the relative permeability of different anions, including GSH, seems dependent on the presence of large anions at the intracellular site [9, 27]. Furthermore, it must be considered that the nature of the CFTR pore properties, in particular, its involvement in GSH secretion, seems to be influenced by the interaction with nucleotides [25].
Oxidation/reduction is an important mechanism regulating ion channels, and GSH actually is a strongly reducing agent. Increased GSH levels obviously imply increased levels of its oxidized form (GSSG) as well. Strongly oxidizing agents, as GSSG, are hypothesized to influence CFTR gating [28], and some authors have recently speculated that oxidized GSH forms could interact with CFTR by “glutathionylation” [29]. However, both in whole-cell and in inside-out configurations, the entire intracellular medium is completely substituted. Therefore, in control cells and S-CMC-Lys-pretreated cells, the reduced/oxidized ratio of GSH on the intracellular side should be constant. Thus, the presence of GSH alone is not likely to justify the activity variations of the observed anion channel in S-CMC-Lys-pretreated conditions. During patch-clamp experiments with high GSH concentration, S-CMC-Lys cell pretreatment is already over. This should rule out a direct interaction between GSH and S-CMC-Lys (in experimental conditions). S-CMC-Lys seems able to stimulate GSH secretion without damaging cells, as shown by LDH release assay. The effect takes place through a complex mechanism implying an increased number of active channels in the membrane, increased Po of the channel, and higher GSH permeability. The rise in Po and active channels could be partly mediated by a cAMP-dependent phosphorylation, as already suggested for S-CMC-Lys action on Cl− secretion [12]. We cannot exclude that the S-CMC-Lys action upon Cl− secretion partially takes place through its suggested role as intracellular antioxidant [30] and thus by a possible channel activity regulation by oxidation/reduction.
Many metabolites of S-carbocysteine have been identified (for instance, S-carbocysteine-sulfoxide, N-acetyl-carbocysteine, N-acetylcysteine-sulfoxide, N-acetyl-S-methyl-cysteine-sulfoxide, and others [31, 32]) after oral administration in healthy volunteers. It is hard to exclude the possibility that the clinical effect of S-CMC-Lys could be partially ascribed to one of its metabolites. An intracellular increase in cysteine could lead to increased GSH levels [33]. However, the experiments (both in whole-cell and inside-out configurations) have all been performed at the same known intracellular GSH concentration. Thus, we can rule out an S-CMC-Lys-mediated stimulation given by an increase in intracellular GSH.
Since the molecule is produced as lysine salt, we did not deem it important, from a clinical perspective, to verify whether lysine alone could affect the currents; we focused more on assessing the effect of the product as a whole, at least for now. In any case, there are data in literature supporting an action on Cl− channels by nonsalt S-carboxymethyl-l-cysteine [16].
Preliminary data from whole-cell experiments on LCFSN-infected CFT1 cells pretreated with lysine alone do not suggest any stimulation of GSH-dependent currents (data not shown).
Interestingly, GSH is a promoter of mucolysis because of its ability to cleave disulfide bonds in mucus [34]. Therefore, the mucoactive action of S-CMC-Lys could be potentiated by an increased secretion of GSH. Future works will be particularly focused on the specificity of the S-CMC-Lys-dependent increase in GSH permeability, bearing also in mind the recent findings about the human CFTR structure [26, 35]. Finally, the evaluation of the ability of S-CMC-Lys to stimulate GSH secretion could be significant in CF patients with mutations that impair CFTR channel activity (but yet allow its presence in the plasma membrane) or in patients affected by pulmonary diseases with an associated deficiency of GSH in air surface liquid such as acute respiratory distress syndrome [36], chronic obstructive pulmonary disease [37], idiopathic pulmonary fibrosis [38], and other respiratory pathologies [39, 40].
References
Cantin AM, North SL, Hubbard RC, Crystal RG (1987) Normal alveolar epithelial lining fluid contains high levels of glutathione. J Appl Physiol 63:152–157
Smith JJ, Travis SM, Greenberg EP, Welsh MJ (1996) Cystic fibrosis airway epithelia fail to kill bacteria because of abnormal airway surface fluid. Cell 85:229–236
Kelly FJ (1999) Glutathione: in defence of the lung. Food Chem Toxicol 37:963–966
Fernandez-Checa JC, Ren C, Aw TY, Ookhtens M, Kaplowitz N (1988) Effect of membrane potential and cellular ATP on glutathione efflux from isolated rat hepatocytes. Am J Physiol 255:G403–G408
Rappa G, Lorico A, Flavell RA, Sartorelli AC (1997) Evidence that the multidrug resistance protein (MRP) functions as a co-transporter of glutathione and natural product toxins. Cancer Res 57:5232–5237
Roum JH, Buhl R, McElvaney NG, Borok Z, Crystal RG (1993) Systemic deficiency of glutathione in cystic fibrosis. J Appl Physiol 75:2419–2424
Gao L, Kim KJ, Yankaskas JR, Forman HJ (1999) Abnormal glutathione transport in cystic fibrosis airway epithelia. Am J Physiol 277:L113–L118
Hudson VM (2004) New insights into the pathogenesis of cystic fibrosis: pivotal role of glutathione system dysfunction and implications for therapy. Treat Respir Med 3:353–363
Linsdell P, Hanrahan JW (1998) Glutathione permeability of CFTR. Am J Physiol 275:C323–C326
Brown RK, Wyatt H, Price JF, Kelly FJ (1996) Pulmonary dysfunction in cystic fibrosis is associated with oxidative stress. Eur Respir J 9:334–339
Gao L, Broughman JR, Iwamoto T, Tomich JM, Venglarik CJ, Forman HJ (2001) Synthetic chloride channel restores glutathione secretion in cystic fibrosis airway epithelia. Am J Physiol Lung Cell Mol Physiol 281:L24–L30
Meyer G, Doppierio S, Daffonchio L, Cremaschi D (1997) S-carbocysteine-lysine salt monohydrate and cAMP cause non-additive activation of the cystic fibrosis transmembrane regulator channel in human respiratory epithelium. FEBS Lett 404:11–14
Havez R, Degand P, Roussel P, Randoux A (1970) Biochemical mode of action of cysteine by-products on the bronchial mucus. Poumon Coeur 26:81–90
Ishibashi Y, Kobayashi F, Idesawa A, Taniguchi A, Matsuzawa S (2004) Effects of carbocysteine on altered activities of glycosidase and glycosyltransferase and expression of Muc5ac in SO2-exposed rats. Eur J Pharmacol 487:7–15
Colombo B, Turconi P, Daffonchio L, Fedele G, Omini C, Cremaschi D (1994) Stimulation of Cl− secretion by the mucoactive drug S-carboxymethylcysteine-lysine salt in the isolated rabbit trachea. Eur Respir J 7:1622–1628
Kottgen M, Busch AE, Hug MJ, Greger R, Kunzelmann K (1996) N-Acetyl-l-cysteine and its derivatives activate a Cl− conductance in epithelial cells. Pflugers Arch 431:549–555
Yankaskas JR, Haizlip JE, Conrad M, Koval D, Lazarowski E, Paradiso AM, Rinehart CA Jr, Sarkadi B, Schlegel R, Boucher RC (1993) Papilloma virus immortalized tracheal epithelial cells retain a well-differentiated phenotype. Am J Physiol 264:C1219–C1230
Olsen JC, Johnson LG, Stutts MJ, Sarkadi B, Yankaskas JR, Swanstrom R, Boucher RC (1992) Correction of the apical membrane chloride permeability defect in polarized cystic fibrosis airway epithelia following retroviral-mediated gene transfer. Hum Gene Ther 3:253–266
Meyer G, Garavaglia ML, Bazzini C, Botta G (2000) An anion channel in guinea pig gallbladder epithelial cells is highly permeable to HCO(−)(3). Biochem Biophys Res Commun 276:312–320
Raggi MA, Mandrioli R, Casamenti G, Musiani D, Marini M (1998) HPLC determination of glutathione and other thiols in human mononuclear blood cells. Biomed Chromatogr 12:262–266
Fuller CM, Howard MB, Bedwell DM, Frizzell RA, Benos DJ (1992) Antibodies against the cystic fibrosis transmembrane regulator. Am J Physiol 262:C396–C404
Farinha CM, Mendes F, Roxo-Rosa M, Penque D, Amaral MD (2004) A comparison of 14 antibodies for the biochemical detection of the cystic fibrosis transmembrane conductance regulator protein. Mol Cell Probes 18:235–242
Wright SR, Boag AH, Valdimarsson G, Hipfner DR, Campling BG, Cole SP, Deeley RG (1998) Immunohistochemical detection of multidrug resistance protein in human lung cancer and normal lung. Clin Cancer Res 4:2279–2289
Cherrington NJ, Hartley DP, Li N, Johnson DR, Klaassen CD (2002) Organ distribution of multidrug resistance proteins 1, 2, and 3 (Mrp1, 2, and 3) mRNA and hepatic induction of Mrp3 by constitutive androstane receptor activators in rats. J Pharmacol Exp Ther 300:97–104
Kogan I, Ramjeesingh M, Li C, Kidd JF, Wang Y, Leslie EM, Cole SP, Bear CE (2003) CFTR directly mediates nucleotide-regulated glutathione flux. EMBO J 22:1981–1989
Linsdell P, Evagelidis A, Hanrahan JW (2000) Molecular determinants of anion selectivity in the cystic fibrosis transmembrane conductance regulator chloride channel pore. Biophys J 78:2973–2982
Linsdell P, Hanrahan JW (1998) Adenosine triphosphate-dependent asymmetry of anion permeation in the cystic fibrosis transmembrane conductance regulator chloride channel. J Gen Physiol 111:601–614
Harrington MA, Gunderson KL, Kopito RR (1999) Redox reagents and divalent cations alter the kinetics of cystic fibrosis transmembrane conductance regulator channel gating. J Biol Chem 274:27536–27544
Wang W, Oliva C, Li G, Holmgren A, Lillig CH, Kirk KL (2005) Reversible silencing of CFTR chloride channels by glutathionylation. J Gen Physiol 125:127–141
Brandolini L, Allegretti M, Berdini V, Cervellera MN, Mascagni P, Rinaldi M, Melillo G, Ghezzi P, Mengozzi M, Bertini R (2003) Carbocysteine lysine salt monohydrate (SCMC-LYS) is a selective scavenger of reactive oxygen intermediates (ROIs). Eur Cytokine Netw 14:20–26
Rogers KM, Barnsley EA (1977) The metabolism of S-carboxyalkylcysteines in man. Xenobiotica 7:409–414
Waring RH, Mitchell SC (1982) The metabolism and elimination of S-carboxymethyl-l-cysteine in man. Drug Metab Dispos 10:61–62
Deneke SM, Fanburg BL (1989) Regulation of cellular glutathione. Am J Physiol 257:L163–L173
Smith CV, Jones DP, Guenthner TM, Lash LH, Lauterburg BH (1996) Compartmentation of glutathione: implications for the study of toxicity and disease. Toxicol Appl Pharmacol 140:1–12
Rosenberg MF, Kamis AB, Aleksandrov LA, Ford RC, Riordan JR (2004) Purification and crystallization of the cystic fibrosis transmembrane conductance regulator (CFTR). J Biol Chem 279:39051–39057
Moss M, Guidot DM, Wong-Lambertina M, Ten Hoor T., Perez RL, Brown LA (2000) The effects of chronic alcohol abuse on pulmonary glutathione homeostasis. Am J Respir Crit Care Med 161:414–419
Rahman I, MacNee W (1999) Lung glutathione and oxidative stress: implications in cigarette smoke-induced airway disease. Am J Physiol 277:L1067–L1088
Rahman I, Skwarska E, Henry M, Davis M, O’Connor CM, FitzGerald MX, Greening A, MacNee W (1999) Systemic and pulmonary oxidative stress in idiopathic pulmonary fibrosis. Free Radic Biol Med 27:60–68
Behr J, Degenkolb B, Maier K, Braun B, Beinert T, Krombach F, Vogelmeier C, Fruhmann G (1995) Increased oxidation of extracellular glutathione by bronchoalveolar inflammatory cells in diffuse fibrosing alveolitis. Eur Respir J 8:1286–1292
Boda D, Nemeth I, Pinter S (1998) Surface tension, glutathione content and redox ratio of the tracheal aspirate fluid of premature infants with IRDS. Biol Neonate 74:281–288
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guizzardi, F., Rodighiero, S., Binelli, A. et al. S-CMC-Lys-dependent stimulation of electrogenic glutathione secretion by human respiratory epithelium. J Mol Med 84, 97–107 (2006). https://doi.org/10.1007/s00109-005-0720-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-005-0720-y