Abstract
In the human colon, vanilloid receptor TRPV1 is overexpressed both in afferent nerve terminals and in epithelial cells during inflammation. In the past years, pharmacological experiments using TRPV1 agonists and antagonists revealed that TRPV1 receptors may play proinflammatory and protective roles in the gastrointestinal tract. Here, we applied a genetic approach to define the role of TRPV1 and analyzed the effects of dinitrobenzene sulfonic acid (DNBS)-induced colitis in TRPV1-deficient (TRPV1−/−) mice. Intrarectal infusion of DNBS induced increased inflammation in TRPV1−/− mice compared to wild-type littermates (TRPV1+/+) as evaluated by macroscopic scoring and myeloperoxidase assays. This finding indicates that TRPV1 receptors are required for the protection within sensory pathways that regulate the response following the initiation of colonic inflammation. Electrophysiological recordings from circular smooth-muscle cells, performed 8 and 24 h after DNBS treatment, revealed strong spontaneous oscillatory action potentials in TRPV1−/− but not in TRPV1+/+ colons, indicating an early TRPV1-mediated control of inflammation-induced irritation of smooth-muscle activities. These unexpected results suggest that TRPV1 receptors mediate endogenous protection against experimentally induced colonic inflammation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colitis induced by dinitrobenzene or trinitrobenzene sulfonic acid (TNBS) in mice and rats is a well-established experimental model of human inflammatory colonic diseases [1]. Similarly, as observed in inflammatory bowel diseases in humans, this experimental model involves the immune and neuroendocrine systems and leads to long-lasting ulcerative damages of the colonic mucosa.
Intestinal inflammation leads to structural and functional changes of the enteric nervous system, including changes in the excitability, synaptic properties, and neurochemical content of some functional classes of enteric neurons [2]. During inflammatory processes, stimulation of intrinsic and/or extrinsic sensory neurons results not only in the transmission of nociceptive information to the central nervous system but also in the stimulation of local inflammatory and immune responses in the peripheral tissues [2].
The vanilloid receptor type 1 (TRPV1) is a nonselective cation channel with six transmembrane domains and is a member of the transient receptor potential (TRP) channel family [3]. TRPV1 can be activated by a variety of stimuli, including capsaicin (the pungent ingredient of red chili pepper), acid (protons), and temperature. Because of its ability to respond to different kind of noxious stimuli, TRPV1 has been described as a molecular integrator of chemical and physical stimuli that elicits pain [4]. TRPV1-like immunoreactivity is present on nerve terminals within the myenteric ganglia and interganglionic fiber tract throughout the gastrointestinal tract [5]. Since TRPV1 is known to be located on sensory neurons, the distribution suggests an involvement in processing chemical, physical, and inflammatory stimuli. Moreover, TRPV1 mediates responses to inflammation rather than acute thermal pain and can be activated by the proinflammatory peptide bradykinin [6]. In the past years, several pharmacological studies showed that local administration of the TRPV1 antagonist capsazepine prevent intestinal inflammation [7–9]. Remarkably and surprisingly, capsaicin was also shown to protect against TNBS-induced colitis [10]. Several aspects in the pharmacology of TRPV1 receptors have still remained unclear, including non-TRPV1-specific effects of agonists and antagonists, the capacity of TRPV1 agonists not only to desensitize the receptors but also to reduce the responses of the neurons to other stimuli, and finally, the contrasting results on the basis of experimental models, targeted organs, and animal species used.
To better understand the role of TRPV1 receptors in mouse, we examined the effect of genetic ablation of TRPV1 receptors in DNBS-induced colitis.
Methods
Animals
TRPV1-deficient (TRPV1−/−) female mice (8–10 weeks old) and corresponding wild-type littermates (TRPV1+/+) were used for experiments [11]. Mice were in mixed genetic background, with a predominant C57BL/6N contribution (five backcrosses). Experimental animals were genotyped by polymerase chain reaction (PCR) under standard buffer conditions using the primer pair 5′-CGA GGA TGG GAA GAA TAA CTC ACT G-3′ and 5′-GGA TGA TGA AGA CAG CCT TGA AGT C-3′ for the wild-type locus. The primer pair 5′-GAA CAA GAT GGA TTG CAC GCA-3′ and 5′-CCC TCA GAA GAA CTC GTC AAG AAG-3′ was used to detect a fragment in the Neo cassette, specific for the mutant TRPV1 locus. All four primers were used together in the reaction mix (1×95°C/1 min; 35×95, 55, and 72°C/1 min; 1×72°C/10 min). Homozygous TRPV1−/− and wild-type littermates (TRPV1+/+) from heterozygous breedings were used for experiments. Mice were housed under standard conditions and supplied with drinking water and food ad libitum. All animal procedures complied with the guidelines for care and use of laboratory animals of the government of the state of Bavaria, Germany.
Induction of colitis
Colitis was induced by intrarectal administration of DNBS as described [12]. Briefly, mice were lightly anaesthetized with isoflurane, and DNBS (5 mg in 100 μl of 50% ethanol) was infused into the rectum through a catheter (outer diameter 0.8 mm) inserted 4–5 cm proximally to the anus. Solvent alone (100 μl of 50% ethanol) was administered in control experiments.
Macroscopic evaluation of colonic damage and determination of tissue myeloperoxidase activity
Three days after DNBS treatment, macroscopic colonic damage was assessed by a semiquantitative scoring system, and samples of colon were processed for determination of myeloperoxidase (MPO) activity as described [12].
Electrophysiological experiments
The colon was exposed by an abdominal midline incision. The complete large bowel was removed, and distal colon was separated. Mucosa and submucosa were removed, resulting in sheets of tissue consisting of circular and longitudinal muscle layers, together with the attached myenteric plexus. Experiments with TRPV1−/− and wild-type littermates at the same time point after induction of inflammation were performed simultaneously in one electrophysiological chamber. Resting membrane potentials (RMPs) of circular smooth-muscle cells and spontaneous action potentials were recorded as described [12].
Statistical analysis
Macroscopic scores are expressed as median and range values, and were compared by using the test of Mann and Whitney. MPO levels are normalized and expressed as mean±SEM and were compared by using Student's t test. P<0.05 was considered as statistically significant.
Results
Genetic ablation of TRPV1 receptors increases severity of DNBS-induced colitis
Without administration of DNBS, the colons of TRPV1−/− and TRPV1+/+ mice were macroscopically and histologically normal and did not differ between genotypes (data not shown, n=8 per group, P>0.05). To study the involvement of TRPV1 receptors in colon inflammation, we used the DNBS model of colitis. Intrarectal administration of 100 μl of 50% ethanol did not induce detectable inflammation in TRPV1−/− nor in TRPV1+/+ mice after 3 days as macroscopically evaluated (data not shown, n=8 per group, P>0.05). After intrarectal administration of DNBS (5 mg/100 μl per mouse), macroscopic evaluation of TRPV1−/− colons revealed stronger inflammation as compared to TRPV1+/+ colons (Fig. 1a). Macroscopic score in TRPV1−/− was 66% higher than in TRPV1+/+ mice: TRPV1+/+, 2.41±0.36 (mean±SEM, n=13) vs TRPV1−/−, 4.00±0.44 (n=12) (P<0.05; Fig. 1a).
Myeloperoxidase assay revealed that the degree of inflammation was higher in knockout than in wild−type mice: TRPV1+/+, 100.00±22.44% (mean % of control group±SEM, n=13) vs TRPV1−/−, 208.20±43.24% (n=12) (P<0.05; Fig. 1b).
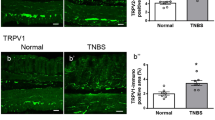
Electrophysiological analysis shows spontaneous oscillatory activities in TRPV1−/− mice at early stages of colonic inflammation
Circular smooth-muscle cells of uninflamed TRPV1+/+ mice displayed a stable RMP of 52.0±1.1 mV (mean±SEM, n=4), which was not different from the RMP measured in TRPV1−/− mice (52.7±2.3 mV, n=4, P>0.05, Fig. 2a). RMP was not different between genotypes 8 and 24 h after DNBS treatment (8 h: TRPV1+/+, 48.4±2.1 mV vs TRPV1−/−, 53.4±4.1 mV, n=4, P>0.05, Fig. 2b; 24 h: TRPV1+/+, 49.1±2.9 mV vs TRPV1−/−, 52.4± 4.5 mV, n=3, P>0.05, Fig. 2c). In both genotypes, RMP was not changed in the presence of atropine (1 μM), an inhibitor of cholinergic transmission (data not shown, n=5 per group, P>0.05). After DNBS treatment, however, TRPV1−/− mice displayed spontaneous action potentials with a frequency of 28.8±3.3 min−1 and an amplitude of 27.3±4.1 mV 8 h after initiation of inflammation (mean±SEM, n=5) and a frequency of 35.2±1.4 min−1 and an amplitude of 32.4±2.2 mV 24 h after initiation of inflammation (n=5). These spontaneous action potentials were not observed in neither TRPV1+/+ mice at any time point after DNBS treatment nor in untreated mice (Fig. 2). The rhythmic action potentials were unchanged in the presence of atropine (1 μM) (data not shown, n=5 per group, P>0.05).
Intracellular recordings from circular smooth muscles in distal colon of TRPV1+/+ and TRPV1−/− mice to monitor resting membrane potentials (RMP). Representative traces are shown for mice a before, b 8 h and c 24 h after induction of colitis. In b and c, note the occurrence of oscillatory action potentials in TRPV1−/− colons
Discussion
In this study, we present direct evidence that TRPV1 is required to guard intestinal inflammation induced by DNBS. During the last years, the TRPV1 agonist capsaicin and the structurally related antagonist capsazepine have been extensively used in several pharmacological studies to reveal a direct role of TRPV1 in different models of inflammation [7–10, 13–16], but several aspects of the involvement of TRPV1 have remained unclear. Both capsaicin and capsazepine have been shown to have non-TRPV1-specific effects [17–20]. Moreover, application of capsaicin could lead, after an initial excitatory response, not only to the desensitization of TRPV1 [14] but also to a rather unspecific functional reduction or even a loss of responsiveness of the neurons to other stimuli [14]. In this case, the worsening effects of capsaicin during inflammation may not be due to the specific activation and/or desensitization of TRPV1 receptors but may be due to the unspecific functional inactivation of the entire neurons involved. Consequently, the ability of capsazepine to antagonize capsaicin effects and to revert the detrimental effects of the agonist on inflammatory processes might be due to the reversal of the functional neuronal inactivation induced by the TRPV1 agonist rather than to the blockade of a specific function of TRPV1 receptors.
Moreover, capsazepine has been demonstrated to be able to block calcium channels, and this might explain some of its beneficial effects during colitis [20, 21]. Because capsaicin treatment leads to overt sensory nerve inactivation [14], these studies have not been able to distinguish the importance of capsaicin-sensitive neurons from that of the endogenous TRPV1 function.
Moreover, pharmacological stimulation of TRPV1 revealed a protective role in TNBS-induced colitis [10], HCl-induced gastritis [22], and carrageenan-induced inflammation in rats [23]. On the other hand, pharmacological blockade of TRPV1 receptors has also been shown to protect against colonic inflammation [7, 9]. Recently, Kimball et al. [8] reported that a novel TRPV1 channel blocker, JNJ 10185734, is able to reduce the severity of colitis induced by dextran sulfate sodium (DSS) in mice. Interestingly, they observed a bell-shaped dose response. The authors suggested that this may be due to the interaction of this compound with other as-yet-unidentified receptors.
To further address these intriguing findings, we choose a genetic approach and studied colonic-induced inflammation in mice with inactivated TRPV1 genes. While anatomically and morphologically normal, these mice showed increased levels of DNBS-induced inflammation, strongly indicating a protective role of TRPV1 receptors during the initiation of inflammation.
Recently, it has been shown that instability of the RMP of smooth-muscle cells and spontaneous spiking activity at the smooth-muscle cell membrane are present at early stages of colonic inflammation when macroscopic signs of inflammation were not yet visible [12] (and unpublished results). These disturbances are reported both in smooth-muscle cells and in neuronal cells. In neurons, an increased spontaneous spiking activity after TNBS-induced colitis was described, suggesting that apart from local muscular electrophysiological changes, the afferent limb of motor reflexes is disrupted during inflammation [24]. Within these changes, the release of tachykinins and/or substance P from capsaicin-sensitive neurons might play a major role [25], whereas cholinergic mechanisms do not seem to be involved.
In our study, increased spontaneous spiking activity of smooth-muscle cell membrane of DNBS-treated colons from TRPV1−/− mice was already visible 8 h after DNBS treatment, indicating that inflammation-induced irritation of smooth muscles occurs at an earlier stage as compared to wild-type mice.
Our study supports the notion that TRPV1 is protective against inflammatory changes, and this indicates that the activation of TRPV1 is an early and important physiological step during the defense from inflammatory events. This function might be exerted by the controlled synthesis/release of endogenous TRPV1 ligands (endovanilloids), whose nature is not yet completely elucidated [26]. Among them, the endogenous cannabinoid agonist anandamide has been suggested to act as an agonist of TRPV1 receptors, although at relatively high doses [26, 27]. Interestingly, anandamide seems to play a key role during inflammation; genetic ablation of fatty acid amide hydrolase (FAAH), the degrading enzyme of anandamide [28], resulted in a strong protection during DNBS-induced colitis [12]. Furthermore, genetic deletion of both the cannabinoid receptor type 1 CB1 (the target of anandamide) [12] and TRPV1 receptors (present results) leads to decreased protection against DNBS-induced colitis. Despite the fact that high doses of exogenously locally applied anandamide have been shown to induce intestinal inflammation [16], one could speculate that the balanced endogenous synthesis and release of this compound and its controlled action at both CB1 and TRPV1 might mediate protection against colon inflammation. If this notion holds true in further studies, the pharmacological enhancement of anandamide activity (or of other endogenous ligands of CB1 and TRPV1 receptors) might provide a very promising therapeutic tool to efficiently control excessive inflammatory responses in the colon.
Abbreviations
- TRPV1:
-
Vanilloid receptor type 1
- TRPV1−/− :
-
TRPV1-deficient mice
- TRPV1+/+ :
-
TRPV1 wild-type littermates
- DNBS:
-
Dinitrobenzene sulfonic acid
- MPO:
-
Myeloperoxidase
- RMP:
-
Resting membrane potentials
References
Selve N (1992) Chronic intrajejunal TNBS application in TNBS-sensitized rats: a new model of chronic inflammatory bowel diseases. Agents Actions Spec No:C15–C17
Lomax AE, Fernandez E, Sharkey KA (2005) Plasticity of the enteric nervous system during intestinal inflammation. Neurogastroenterol Motil 17:4–15
Caterina MJ, Schumacher MA, Tominaga M, Rosen TA, Levine JD, Julius D (1997) The capsaicin receptor: a heat-activated ion channel in the pain pathway. Nature 398:816–824
Tominaga M, Caterina MJ, Malmberg AB, Rosen TA, Gilbert H, Skinner K, Raumann BE, Basbaum AI, Julius D (1998) The cloned capsaicin receptor integrates multiple pain-producing stimuli. Neuron 21:531–543
Ward SM, Bayguinov J, Won KJ, Grundy D, Berthoud HR (2003) Distribution of the vanilloid receptor (VR1) in the gastrointestinal tract. J Comp Neurol 465:121–135
Tang HB, Inoue A, Oshita K, Nakata Y (2004) Sensitization of vanilloid receptor 1 induced by bradykinin via the activation of second messenger signaling cascades in rat primary afferent neurons. Eur J Pharmacol 498:37–43
Kihara N, de la Fuente SG, Fujino K, Takahashi T, Pappas TN, Mantyh CR (2003) Vanilloid receptor-1 containing primary sensory neurones mediate dextran sulphate sodium induced colitis in rats. Gut 52:713–719
Kimball ES, Wallace NH, Schneider CR, D'Andrea MR, Hornby PJ (2004) Vanilloid receptor 1 antagonists attenuate disease severity in dextran sulphate sodium-induced colitis in mice. Neurogastroenterol Motil 16:811–818
Fujino K, Takami Y, de la Fuente SG, Ludwig KA, Mantyh CR (2004) Inhibition of the vanilloid receptor subtype-1 attenuates TNBS-colitis. J Gastrointest Surg 8:842–847
Goso C, Evangelista S, Tramontana M, Manzini S, Blumberg PM, Szallasi A (1993) Topical capsaicin administration protects against trinitrobenzene sulfonic acid-induced colitis in the rat. Eur J Pharmacol 249:185–190
Caterina MJ, Leffler A, Malmberg AB, Martin WJ, Trafton J, Petersen-Zeitz KR, Koltzenburg M, Basbaum AI, Julius D (2000) Impaired nociception and pain sensation in mice lacking the capsaicin receptor. Science 288:306–313
Massa F, Marsicano G, Hermann H, Cannich A, Monory K, Cravatt BF, Ferri GL, Sibaev A, Storr M, Lutz B (2004) The endogenous cannabinoid system protects against colonic inflammation. J Clin Invest 113:1202–1209
McVey DC, Vigna SR (2001) The capsaicin VR1 receptor mediates substance P release in toxin A-induced enteritis in rats. Peptides 22:1439–1446
Geppetti P, Trevisani M (2004) Activation and sensitisation of the vanilloid receptor: role in gastrointestinal inflammation and function. Br J Pharmacol 141:1313–1320
Menendez L, Lastra A, Hidalgo A, Baamonde A (2004) The analgesic effect induced by capsaicin is enhanced in inflammatory states. Life Sci 74:3235–3244
McVey DC, Schmid PC, Schmid HH, Vigna SR (2003) Endocannabinoids induce ileitis in rats via the capsaicin receptor (VR1). J Pharmacol Exp Ther 304:713–722
Fujimoto S, Mori M (2004) Characterization of capsaicin-induced, capsazepine-insensitive relaxation of ileal smooth muscle of rats. Eur J Pharmacol 487:175–182
Ray AM, Benham CD, Roberts JC, Gill CH, Lanneau C, Gitterman DP, Harries M, Davis JB, Davies CH (2003) Capsazepine protects against neuronal injury caused by oxygen glucose deprivation by inhibiting I(h). J Neurosci 23:10146–10153
Nocerino E, Izzo AA, Borrelli F, Capasso F, Capasso R, Pinto A, Sautebin L, Mascolo N (2002) Relaxant effect of capsazepine in the isolated rat ileum. Naunyn Schmiedebergs Arch Pharmacol 365:187–192
Liu L, Simon SA (1997) Capsazepine, a vanilloid receptor antagonist, inhibits nicotinic acetylcholine receptors in rat trigeminal ganglia. Neurosci Lett 228:29–32
Docherty RJ, Yeats JC, Piper AS (1997) Capsazepine block of voltage-activated calcium channels in adult rat dorsal root ganglion neurones in culture. Br J Pharmacol 121:1461–1467
Horie S, Yamamoto H, Michael GJ, Uchida M, Belai A, Watanabe K, Priestley JV, Murayama T (2004) Protective role of vanilloid receptor type 1 in HCl-induced gastric mucosal lesions in rats. Scand J Gastroenterol 39:303–312
Costa B, Giagnoni G, Franke C, Trovato AE, Colleoni M (2004) Vanilloid TRPV1 receptor mediates the antihyperalgesic effect of the nonpsychoactive cannabinoid, cannabidiol, in a rat model of acute inflammation. Br J Pharmacol 143:247–250
Linden DR, Sharkey KA, Mawe GM (2003) Enhanced excitability of myenteric AH neurones in the inflamed guinea-pig distal colon. J Physiol 547:589–601
Holzer P, Holzer-Petsche U (1997) Tachykinins in the gut. Part II. Roles in neural excitation, secretion and inflammation. Pharmacol Ther 73:219–263
Van der Stelt M, Di Marzo V (2004) Endovanilloids. Putative endogenous ligands of transient receptor potential vanilloid 1 channels. Eur J Biochem 271:1827–1834
Zygmunt PM, Petersson J, Andersson DA, Chuang H, Sorgard M, Di Marzo V, Julius D, Hogestatt ED (1999) Vanilloid receptors on sensory nerves mediate the vasodilator action of anandamide. Nature 400:452–457
Cravatt BF, Lichtman AH (2002) The enzymatic inactivation of the fatty acid amide class of signaling lipids. Chem Phys Lipids 121:135–148
Acknowledgements
We wish to thank Dr. Peter Holzer for discussions and suggestions on the manuscript and Dr. David Julius for providing the TRPV1 mutant mice. This work was supported by grants from the Deutsche Forschungsgemeinschaft (DFG) (LU755/1-3), Förderprogramm für Forschung und Lehre der Medizinischen Fakultät der LMU München (FöFoLe), and by a scholarship from the Hertie Foundation (to B.L.).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Massa, F., Sibaev, A., Marsicano, G. et al. Vanilloid receptor (TRPV1)-deficient mice show increased susceptibility to dinitrobenzene sulfonic acid induced colitis. J Mol Med 84, 142–146 (2006). https://doi.org/10.1007/s00109-005-0016-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-005-0016-2