Abstract
Purpose
This meta-analysis compares open reduction and internal fixation with a plate (ORIF) versus nailing for humeral shaft fractures with regard to union, complications, general quality of life and shoulder/elbow function.
Methods
PubMed/Medline/Embase/CENTRAL/CINAHL was searched for observational studies and randomised clinical trials (RCT). Effect estimates were pooled across studies using random effects models. Results were presented as weighted odds ratio (OR) or risk difference (RD) with corresponding 95% confidence interval (95% CI). Subgroup analysis was performed stratified for study design (RCTs and observational studies).
Results
Eighteen observational studies (4906 patients) and ten RCT’s (525 patients) were included. The pooled effect estimates of observational studies were similar to those obtained from RCT’s. More patients treated with nailing required re-intervention (RD 2%; OR 2.0, 95% CI 1.0–3.8) with shoulder impingement being the most predominant indication (17%). Temporary radial nerve palsy secondary to operation occurred less frequently in the nailing group (RD 2%; OR 0.4, 95% CI 0.3–0.6). Notably, all but one of the radial nerve palsies resolved spontaneously in each groups. Nailing leads to a faster time to union (mean difference − 1.9 weeks, 95% CI − 2.9 to − 0.9), lower infection rate (RD 2%; OR 0.5, 95% CI 0.3–0.7) and shorter operation duration (mean difference − 26 min, 95% CI − 37 to − 14). No differences were found regarding non-union, general quality of life, functional shoulder scores, and total upper extremity scores.
Conclusion
Nailing carries a lower risk of infection, postoperative radial nerve palsy, has a shorter operation duration and possibly a shorter time to union. Shoulder impingement requiring re-intervention, however, is an inherent disadvantage of nail fixation. Notably, absolute differences are small and almost all patients with radial nerve palsy recovered spontaneously. Satisfactory results can be achieved with both treatment modalities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Humeral shaft fractures represent 1–3% of all fractures [1]. A recent meta-analysis has demonstrated considerable rates of treatment failure among patients managed conservatively for humeral shaft fractures [2]. Operative treatment reduces chances of non-union and possibly leads to better functional results. As such, surgical management is increasingly being used to treat these fractures.
The optimal operative technique, however, remains a point of debate. The most popular treatment options include nailing and open reduction with plate fixation [3,4,5,6,7]. Nailing is a minimally invasive procedure indirectly stabilising the fracture by introducing a nail through the shoulder (or elbow) joint. The fracture zone and surrounding soft tissue are left untouched optimising conditions for fracture healing [6]. The main disadvantage of nailing is the occurrence of shoulder (and/or elbow) complaints. These complaints occur to lesser extent in patients treated with open plate fixation. However, due to extensive dissection, both fracture zone and soft tissue are violated negatively impacting healing and chances of infection [3].
Nailing and open plating have been extensively studied. Several meta-analyses have been published on this topic [3, 6, 7]. However, mostly data from randomised clinical trials was used, while the majority of published literature is in the form of observational studies. Multiple studies have shown that pooled estimates obtained from randomised clinical trials tend to be similar to those from observational studies [2, 8,9,10]. Adding observational studies in meta-analyses increases sample size and could increase the power for detecting small differences in treatment effects. As randomised clinical trials usually include a highly selective study population, including observational studies in meta-analyses might improve generalizability of results.
The aim of the present meta-analysis is to combine the evidence from both study designs and re-evaluate the comparison of nailing versus open plate fixation for humeral shaft fractures in this context. Primary endpoints are non-union, re-intervention, radial nerve palsy, infection, time-to-union, operation duration, general quality of life, shoulder function, elbow function and total upper extremity function by including both randomised clinical trials and observational studies. In addition, sub-group analysis is performed for study design to see what observational studies and randomised clinical trials have been telling us in these past decades.
Methods
This meta-analysis and systematic review was performed according the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guideline and Meta-analysis of Observational Studies in Epidemiology checklist (MOOSE) [11, 12]. No protocol for this review was published prior to performing the present study. Ethical committee approval was not necessary.
Search strategy and selection criteria
The PubMed/Medline, Embase, CENTRAL, and CINAHL database were searched on 2 December 2020 for comparative studies on plate fixation (using open reduction) and nailing for humeral shaft fractures. Supplementary material Table 1 describes the used search syntax. Two reviewers (BJMvdW, NvV) screened title/abstract and full text for eligibility. Both randomised clinical trials as well as observational studies were included. Inclusion criteria were humeral shaft fracture, comparison of plate fixation (using open reduction) with nailing, minimum age of 16 years and reporting on outcomes of interest. Exclusion criteria were comparison of minimally invasive plate fixation to nailing, pathological fractures, treatment for non-union or non-union, studies with an average follow-up less than 6 months, languages other than English, German, French or Dutch and no availability of full text. Disagreements on eligibility was resolved by discussion with a third co-author (FJPB). Cross-reference check was performed for all included articles.
Data extraction
All baseline characteristics were independently extracted by two reviewers (BJMvdW, NvV) using a predefined data extraction sheet and included first author, publication year, study period, country, design of the study (randomised clinical trial or observational study), study population size. In addition, data on patient characteristics was also collected and included implant type, age, gender, whether the fracture was open or closed, AO/OTA Fracture and Dislocation classification, caused by low- or high-energy trauma and duration of follow-up [13].
Quality assessment
The same reviewers (BJMvdW, NvV) assessed the methodological quality of included studies independently using the Methodological Index for Non-randomised Studies (MINORS) [14]. Disagreement was resolved by a third reviewer (FJPB). The score of this instrument ranges from 0 (poor quality) to 24 (high quality). Supplementary material Table 2 describes the details on methodological quality assessment.
Study outcome
Outcomes of interest included non-union, re-intervention, radial nerve palsy following surgery (secondary radial nerve palsy), infection (superficial and deep), operation duration (minutes), time to union (weeks), general quality of life, shoulder and elbow functional scores measured between 6 and 12 months after plate fixation or nailing [15]. All general quality of life scores (Short-Form 36, EuroQol-5D), scores on upper extremity (Disabilities of Arm, Shoulder and Hand), elbow function (Oxford elbow, Mayo elbow performance score, Broberg–Morrey score) and shoulder function (Constant score, American Shoulder and Elbow Surgeons shoulder score, University of California at Los Angeles Shoulder Score, Neer score, Oxford Shoulder score) were standardised and pooled for each field (general quality of life, upper extremity function, shoulder function, elbow function) separately.
Statistical analysis
Review Manager (RevMan, version 5.3.5) was used for all statistical analysis. Information about continuous variables was presented as means with standard deviation (SD) or range, or information was converted to mean and SD using the methods described in the Cochrane Handbook for Systematic Reviews of Interventions [16]. Dichotomous variables were presented as counts and percentages. Treatment effects on binary outcomes were pooled using the (random effects) Mantel–Haenszel method and continuous outcomes using the (random effects) inverse variance weighting method. All outcomes were presented as either weighted odds ratio (OR), risk difference (RD), mean difference (MD) or standardised mean difference (SMD) with corresponding 95% confidence interval (95% CI). None of the observational studies corrected for confounding. Therefore, the estimated relations between treatment and outcome presented for these studies are unadjusted for possible confounding.
Heterogeneity between studies was judged by visual inspection of forest plots and quantified by the I2 statistic. All analyses were stratified according to study design (observational studies, randomised clinical trials). Differences in pooled estimates between the two designs were tested using the χ2-test. The p value was set at a threshold of 0.05. Publication bias was assessed by visual inspection of funnel plots. All forest plots are shown in the added supplementary material.
Sensitivity analysis
A sensitivity analysis was performed for re-intervention (all indications versus indications other than non-union), quality of studies (using MINORS score cut-off point of 16) and year of publication (cut-off point 2013). The cut-off point was chosen based on the median publication year of included studies [8].
Results
Search
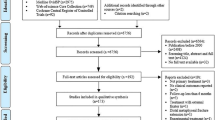
The literature search and study selection are shown in Fig. 1. Full text could not be obtained for two observational retrospective studies [17, 18]. In total 28 articles could be included—10 randomised clinical trials and 18 observational studies [19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46].
Baseline study characteristics
The 28 studies included 5490 patients; 3548 were treated with plate fixation and 1942 with nailing. The overall median age was 42 (range 16–88) years; 41 years in the plate fixation group and 42 years in the nail fixation group, respectively. The studies included 2812 (51.2%) males. Overall mean follow-up ranged from 6 to 48 months. Table 1 shows the baseline characteristics of all studies per treatment group and study design. All characteristics were equally distributed among treatment groups including AO/OTA Fracture and Dislocation classification, open/closed fractures and energy of trauma.
The 10 randomised clinical trials included 525 patients of whom 268 were treated with plate fixation [20, 22, 24, 26, 35, 36, 38, 42, 43, 46]. The median age was 38.5 (range 18–82) years; 38 years in the plate fixation and 39 years in the nailing group, respectively. In the plate fixation group either a dynamic compression plate (DCP) or locking compression plate (LCP) was used. Seven studies reported on type of implant for the nailing group and included Russel–Taylor nails, unreamed humeral nails (UHN), ILN (Sanat Metal) and Ender nails. All nails were introduced in an antegrade fashion.
The 18 observational studies—five prospective and 13 retrospective studies—included 4965 patients, of whom 3280 were treated with plate fixation [19, 21, 23, 25, 27,28,29,30,31,32,33,34, 37, 39,40,41, 44, 45]. The median age was 45 years (range 16–88); 44 years in the plate fixation and 45 years in the nailing group, respectively. All studies reported on type of implant for the plate fixation group and included DCP, LCP and tibia plate. Six studies reported this for the nailing group and included UHN, Russel-Taylor, Hackethal, T2 nail, Küntscher, Seidel and ST-pro nail. In only one study the nail was introduced in a retrograde fashion. The other studies reported using an antegrade approach.
Quality assessment
The methodological quality scores according the MINORS are described in Table 2. The average score among the randomised clinical trials was 21 and 14 for observational studies. The overall average across all studies was 17 (range 1–22).
Non-union rate
Non-union rate was reported in 26 studies—10 randomised clinical trials and 16 observational studies [19,20,21,22, 24,25,26, 28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46]. The risk of non-union was equal in both groups (OR 1.0, 95% CI 0.7–1.4; I2 = 0%) (Fig. 2). Non-union occurred in 3.0% of patients treated with plate fixation and 4.3% treated with nailing (RD 0%, 95% CI 0–0%). There was no difference in pooled effect estimates between randomised trials and observational studies (p value 0.97).
Re-intervention
Re-intervention was reported in 23 studies—10 randomised clinical trials and 13 observational studies [19,20,21,22,23,24,25,26, 30, 31, 33,34,35,36,37,38, 40,41,42,43,44,45,46]. Re-intervention was performed in 12.6% of patients after plate fixation and in 9.7% treated with nailing (RD 1%, 95% CI − 2 to 3%). There was no significant difference in re-intervention risk between treatment groups (OR 1.2, 95% CI 0.9–1.7; I2 = 0%) (Fig. 3) and this was also found when stratifying by design (p value 0.46). Reasons for re-interventions are listed in supplementary material Tables 3 and 4.
Time to union
Nine studies reported on mean time to union—six randomised clinical trials and three observational studies [20, 22, 24, 26, 33, 43,44,45,46]. The time to union was significantly shorter among patients treated with nail fixation (MD − 1.9 weeks, 95% CI −2.9 to − 0.9; I2 = 58%) (Fig. 4). Time to union in the plate fixation group was, on average, 14 weeks versus 12 weeks among patients treated with nailing.
The effect estimates of observational studies and randomised clinical trials were equal (p value 0.79).
Secondary radial nerve palsy
Twenty-six studies reported on secondary radial nerve palsy—10 randomised clinical trials and 16 observational studies [19,20,21,22,23,24,25,26, 29,30,31,32,33,34, 36,37,38,39,40,41,42,43,44,45,46]. The risk was lower among patients treated with nailing (OR 0.4, 95% CI 0.3–0.6; I2 = 0%) (Fig. 5). Radial nerve palsy following surgery occurred in 6.9% of patients treated with plate fixation versus 2.5% in the nailing group (RD − 2.0%, 95% CI − 5% to 1%). There was no difference in pooled estimates between randomised clinical trials and observational studies (p value 0.32).
Nerve function recovered spontaneously in all but one patient in each treatment group leading to a risk of permanent nerve palsy of 0.03% for plate fixation versus 0.05% for nailing.
Infection
Twenty-five studies reported on infection—10 randomised clinical trials and 15 observational studies [19,20,21,22, 24,25,26, 28,29,30,31,32,33,34,35,36, 38,39,40,41,42,43,44,45,46]. No distinction could be made between deep and superficial infection as included studies did not differentiate between the two. Therefore, results represent overall risks of infection.
The risk of infection was lower among patients treated with nailing (OR 0.5, 95% CI 0.3–0.7; I2 = 0%) (Fig. 6) and occurred in 6.8% of patients after plate fixation and in 1.9% treated with nailing (RD − 2%, 95% CI − 3 to 1%). There was no difference in effect estimates between randomised trials and observational studies (p value 0.44).
Operation duration
Eight studies reported on operation duration—four randomised clinical trials and four observational studies [21, 24, 26, 30, 32, 43,44,45,46]. Operation duration was significantly shorter among patients treated with nail fixation (MD − 26 min, 95% CI − 37 to − 14; I2 = 97%) (Fig. 7). The pooled estimates of randomised clinical trials were similar to those from observational studies (p value 0.31).
General quality of life (6–12 months after surgery)
Only one randomised clinical trial reported on general quality of life [19]. No difference was found in general quality of life between both treatment groups with a SF-36 score of 87.4 (SD 7.7) in the plate fixation group versus 84.7 (SD 7.7) for nailing.
Functional upper extremity scores (6–12 months after surgery)
Two retrospective studies reported on general upper extremity function using the DASH score [30, 45]. No differences were observed with a mean DASH score of 23.9 (SD 17.7) and 22.4 (SD 15.2) for plate fixation versus 21.7 (SD 19.8) and 23.7 (SD 16.8) for nailing.
Functional shoulder scores (6–12 months after surgery)
A total of eight studies reported on functional shoulder scores—four randomised clinical trials and four observational studies [26, 27, 30, 32, 35, 36, 38, 44,45,46]. There was no difference in scores between plate fixation and nailing (SMD − 0.2, 95% CI − 0.4 to 0.1; I2 = 54%) (Fig. 8) and pooled estimates were similar across study designs (p value 0.57).
Functional elbow scores (6–12 months after surgery)
No studies reported on functional elbow scores.
Sensitivity analysis
Re-intervention for indications other than non-union was reported in 19 studies [19,20,21,22, 24,25,26, 30, 31, 33,34,35,36,37,38, 40,41,42,43,44]. The pooled analysis showed that significantly more patients required re-intervention (excluding non-union) after nailing (OR 2.0, 95% CI 1.0–3.8; I2 = 0%) (Fig. 9). Shoulder impingement was the most common indication for re-intervention in the nailing group (supplementary material Table 4).
Table 3 shows the pooled effects of plate versus nail fixation on different outcomes stratified by quality of studies and by period of publication. No relevant differences were observed between the main analyses and these stratified analyses.
Discussion
This meta-analysis, including randomised clinical trials as well as observational studies, compared open reduction and plate fixation with nailing among patients with humeral shaft fractures. The risk of non-union was comparable in both groups. Re-intervention was more frequently required in patients treated with nail fixation with shoulder impingement being the most prevalent indication. Nailing, however, had a smaller risk of infection, lower operation duration and faster time to union. Radial nerve palsy secondary to surgery also occurred less often after nailing. Notably, nerve function recovered spontaneously in almost all patients in both groups. General quality of life, upper extremity and shoulder function were comparable in both groups. There appeared to be no difference in effect estimates from randomised clinical trials and observational studies in all outcomes.
Comparison with previous findings
To date several meta-analyses have been published comparing open plate fixation to nailing [3,4,5,6,7, 47]. The most recent one has been published in 2019 by Wen et al. and analysed a total of 839 patients. This present meta-analysis sets itself apart by also including observational studies thereby increasing the total sample size to 5431. In addition, the present study compares the two treatment regimens directly with each other instead of indirectly through sensitivity analysis or network analyses as frequently was the case in previous meta-analyses. This creates the opportunity to study both treatment regimes in more detail and increases reliability of results. We can confirm that non-union rates are equal in both groups and that nailing carries a lower risk for infection at the expense of having a higher risk for shoulder impingement. In contrast to previous meta-analyses we detected a significant difference in secondary radial nerve palsy, time to union, operation duration, all in favour of nailing.
The fact that we found differences in outcomes not previously detected in other meta-analyses, underlines the benefit of adding observational studies. It increases sample size, yielding more power to detect small differences or determine, with greater certainty, where established differences truly lie.
The fact that the present meta-analysis found no difference in effect estimates between the two study designs underlines that these study designs can be seen as equals in meta-analyses on this topic and serves as justification for combining them. In addition, given the large degree of (baseline) comparability between treatment groups, we consider the potential for confounding acceptably low to allow for including observational data in this meta-analysis.
Interpretation of results
This study found a reduced risk of wound infection, radial nerve palsy and shorter operation duration for nailing. The absolute differences, however, are relatively small. Infection occurred in 6.8% in the plate fixation group and 1.9% in patients treated with nailing; mean operation duration was on average 26 min shorter for nailing; Radial nerve palsy was seen in 6.9% after plate fixation and 2.5% after nailing. Notably, all, except one radial nerve palsy in each treatment group were temporary, leading to a permanent radial nerve palsy incidence of 0.03% for plate and 0.05% for nail fixation.
Only the absolute difference in time to union was considerable. Patients treated with nail fixation attained union 2.5 weeks earlier than patients treated with plate fixation. One should, however, consider two issues. First, defining the exact point in time when a fracture is considered healed, is a subjective matter and also related to the intervals between outpatient clinic visits. This most likely caused the large amount of heterogeneity on this outcome between included studies. Second, it is still unclear how this difference translates into a clinical setting. None of the included studies investigated time-to-return-to-work/full-function or pain relief measured on regular basis throughout time. As there is frequently a discrepancy between radiological and clinical signs of healing, it is difficult to ascertain how patients experience this 2.5 week difference [48]. All in all, statistically we quantified the difference; how this difference behaves in a clinical setting cannot be defined.
The disadvantage of nailing is its inherent risk of causing shoulder complaints when introduced in an antegrade fashion. This meta-analysis found a twofold higher risk of re-intervention among patients treated with nailing with shoulder complaints being the most prevalent indication. Comparable to its advantages, it must, however, be acknowledged that the absolute difference is relatively small (2.6% for plate fixation versus 6.4% for nailing). This small difference is also reflected in the functional shoulder scores. Although we found a trend towards better shoulder score in the plate fixation group, it did not reach statistical significance. This underlines the fact that differences are most likely small with regard to shoulder complaints in both groups in contrast to what is often postulated about antegrade nail fixation [5].
Implications for future research
To date there is sufficient evidence to demonstrate that the absolute differences in clinical and functional outcomes between plate fixation and nailing are relatively small. Evidence with regard to rate of pain relief, time-to-return-to work/full-function and cost-effectiveness (including in-hospital and out-hospital costs) are lacking. To our opinion, investigating these outcome parameters would be of great importance in determining superiority or non-inferiority of one treatment over the other.
In addition, only one study included in this meta-analysis compared plate fixation to retrograde nail fixation [41]. As retrograde nailing has the advantage of avoiding an entry point through the shoulder joint, it is known to cause less shoulder complaints, however, at the expense of causing more iatrogenic fractures during introduction [49]. It would be interesting to have more studies elaborating on this comparison.
Implications for clinical practice
We would like to acknowledge that plate fixation is the preferred treatment modality for humeral shaft fractures in our hospital. As this meta-analysis showed that the absolute differences between plate fixation and nailing are small, we do not intend to change our local protocols. Likewise, we do not recommend hospitals which employ nailing as standard treatment, to switch to plate fixation for the same reasons. In our opinion, both treatment modalities are viable and hospitals should use the technique in which they have the most experience.
Limitations of this study
Some limitations should be considered when interpreting the results of this study. First, there is heterogeneity in the pooled analysis on operation duration (I2 = 97%) and time-to-union (I2 = 58%), limiting the value of that analysis. Second, as in any meta-analysis, there is a risk of publication bias. However, given the patterns observed in the various funnel plots, we consider this risk to be low. Third, this meta-analysis also included observational studies. Although other meta-analyses support this concept, it has yet to be proven in other fields of orthopaedic research and, with it, its validity.
Conclusion
The risk of non-union is comparable for both plate fixation and nailing in patients with humeral shaft fractures. Nailing carries a lower risk of infection, secondary radial nerve palsy, shorter operation duration and possibly time to union. Absolute differences, however, are small and all patients, except one in each group, with radial nerve palsy recovered spontaneously. Although shoulder complaints requiring re-intervention is more common in patients treated with nail fixation, functional shoulder score are comparable in both groups. No difference was detected in general quality of life and total upper extremity function; however, this was based on only one study for the first and two for the latter. All in all, satisfactory results can be achieved with both treatment modalities. This review emphasizes the potential benefit of adding observational studies in a meta-analysis of surgical treatment options.
Availability of data
Not applicable.
References
Ekholm R, Adami J, Tidermark J, Hansson K, Tornkvist H, Ponzer S. Fractures of the shaft of the humerus. An epidemiological study of 401 fractures. J Bone Joint Surg Br. 2006;88(11):1469–73.
van de Wall BJM, Ochen Y, Beeres FJP, Babst R, Link BC, Heng M, et al. Conservative vs. operative treatment for humeral shaft fractures: a meta-analysis and systematic review of randomized clinical trials and observational studies. J Shoulder Elbow Surg. 2020;29:1493–504.
Kurup H, Hossain M, Andrew JG. Dynamic compression plating versus locked intramedullary nailing for humeral shaft fractures in adults. Cochrane Database Syst Rev. 2011;6: CD005959.
Liu GD, Zhang QG, Ou S, Zhou LS, Fei J, Chen HW, et al. Meta-analysis of the outcomes of intramedullary nailing and plate fixation of humeral shaft fractures. Int J Surg. 2013;11(9):864–8.
Ma J, Xing D, Ma X, Gao F, Wei Q, Jia H, et al. Intramedullary nail versus dynamic compression plate fixation in treating humeral shaft fractures: grading the evidence through a meta-analysis. PLoS ONE. 2013;8(12): e82075.
Qiu H, Wei Z, Liu Y, Dong J, Zhou X, Yin L, et al. A Bayesian network meta-analysis of three different surgical procedures for the treatment of humeral shaft fractures. Medicine (Baltimore). 2016;95(51): e5464.
Zhao Y, Wang J, Yao W, Cai Q, Wang Y, Yuan W, et al. Interventions for humeral shaft fractures: mixed treatment comparisons of clinical trials. Osteoporos Int. 2017;28(11):3229–37.
Ochen Y, Beks RB, van Heijl M, Hietbrink F, Leenen LPH, van der Velde D, et al. Operative treatment versus nonoperative treatment of Achilles tendon ruptures: systematic review and meta-analysis. BMJ. 2019;364: k5120.
Beks RB, Peek J, de Jong MB, Wessem KJP, Oner CF, Hietbrink F, et al. Fixation of flail chest or multiple rib fractures: current evidence and how to proceed. A systematic review and meta-analysis. Eur J Trauma Emerg Surg. 2019;45(4):631–44.
Smeeing DPJ, van der Ven DJC, Hietbrink F, Timmers TK, van Heijl M, Kruyt MC, et al. Surgical versus nonsurgical treatment for midshaft clavicle fractures in patients aged 16 years and older: a systematic review, meta-analysis, and comparison of randomized controlled trials and observational studies. Am J Sports Med. 2017;45(8):1937–45.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12.
Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and dislocation classification compendium-2018. J Orthop Trauma. 2018;32(Suppl 1):S1–170.
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–6.
Wilson J. Surveillance of surgical site infection in orthopaedic surgery is useful in tackling hospital-acquired infections in England. Euro Surveill. 2005;10(11):E051117.3.
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343: d5928.
Yin P, Mao Z, Zhang L, Tao S, Zhang Q, Liang X, et al. Effectiveness comparison between locking compression plate fixation and locked intramedullary nail fixation for humeral shaft fracture of types B and C. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2013;27(12):1457–61.
Guzman-Guevara J, Lopez-Cazares G, Barragan-Hervella RG, Villegas-Rosas JS, Alvarado-Ortega I, Montiel-Jarquin AJ. Evaluation of patients with humeral midshaft fractures treated with DCP plate vs. intramedullary nail UHN. Rev Med Inst Mex Seguro Soc. 2016;54(Suppl 3):S270–4.
Bisaccia M, Meccariello L, Rinonapoli G, Rollo G, Pellegrino M, Schiavone A, et al. Comparison of plate, nail and external fixation in the management of diaphyseal fractures of the humerus. Med Arch. 2017;71(2):97–102.
Changulani M, Jain UK, Keswani T. Comparison of the use of the humerus intramedullary nail and dynamic compression plate for the management of diaphyseal fractures of the humerus. A randomised controlled study. Int Orthop. 2007;31(3):391–5.
Chao TC, Chou WY, Chung JC, Hsu CJ. Humeral shaft fractures treated by dynamic compression plates, Ender nails and interlocking nails. Int Orthop. 2005;29(2):88–91.
Chapman JR, Henley MB, Agel J, Benca PJ. Randomized prospective study of humeral shaft fracture fixation: intramedullary nails versus plates. J Orthop Trauma. 2000;14(3):162–6.
Chen F, Wang Z, Bhattacharyya T. Outcomes of nails versus plates for humeral shaft fractures: a Medicare cohort study. J Orthop Trauma. 2013;27(2):68–72.
Chiu FY, Chen CM, Lin CF, Lo WH, Huang YL, Chen TH. Closed humeral shaft fractures: a prospective evaluation of surgical treatment. J Trauma. 1997;43(6):947–51.
Denies E, Nijs S, Sermon A, Broos P. Operative treatment of humeral shaft fractures. Comparison of plating and intramedullary nailing. Acta Orthop Belg. 2010;76(6):735–42.
Fan Y, Li YW, Zhang HB, Liu JF, Han XM, Chang X, et al. Management of humeral shaft fractures with intramedullary interlocking nail versus locking compression plate. Orthopedics. 2015;38(9):e825–9.
Flinkkila T, Hyvonen P, Siira P, Hamalainen M. Recovery of shoulder joint function after humeral shaft fracture: a comparative study between antegrade intramedullary nailing and plate fixation. Arch Orthop Trauma Surg. 2004;124(8):537–41.
Goncalves FF, Dau L, Grassi CA, Palauro FR, Martins Neto AA, Pereira PCG. Evaluation of the surgical treatment of humeral shaft fractures and comparison between surgical fixation methods. Rev Bras Ortop. 2018;53(2):136–41.
Gottschalk MB, Carpenter W, Hiza E, Reisman W, Roberson J. Humeral shaft fracture fixation: incidence rates and complications as reported by American Board of Orthopaedic Surgery Part II Candidates. J Bone Joint Surg Am. 2016;98(17):e71.
Hashmi PM, Mohib Y, Abbas K. Functional and radiological outcome of Intramedullary nailing vs. plate fixation for humeral shaft fractures. Does treatment method bring any difference? J Pak Med Assoc. 2014;64(12 Suppl 2):S135–8.
Khan AS, Afzal W, Anwar A. Comparison of shoulder function, radial nerve palsy and infection after nailing versus plating in humeral shaft fractures. J Coll Physicians Surg Pak. 2010;20(4):253–7.
Kulkarni SG, Varshneya A, Jain M, Kulkarni VS, Kulkarni GS, Kulkarni MG, et al. Antegrade interlocking nailing versus dynamic compression plating for humeral shaft fractures. J Orthop Surg (Hong Kong). 2012;20(3):288–91.
Kulkarni VS, Kulkarni MS, Kulkarni GS, Goyal V, Kulkarni MG. Comparison between antegrade intramedullary nailing (IMN), open reduction plate osteosynthesis (ORPO) and minimally invasive plate osteosynthesis (MIPO) in treatment of humerus diaphyseal fractures. Injury. 2017;48(Suppl 2):S8–13.
Kumar R, Singh P, Chaudhary LJ, Singh S. Humeral shaft fracture management, a prospective study; nailing or plating. J Clin Orthop Trauma. 2012;3(1):37–42.
Li Y, Wang C, Wang M, Huang L, Huang Q. Postoperative malrotation of humeral shaft fracture after plating compared with intramedullary nailing. J Shoulder Elbow Surg. 2011;20(6):947–54.
McCormack RG, Brien D, Buckley RE, McKee MD, Powell J, Schemitsch EH. Fixation of fractures of the shaft of the humerus by dynamic compression plate or intramedullary nail. A prospective, randomised trial. J Bone Joint Surg Br. 2000;82(3):336–9.
Mulier T, Seligson D, Sioen W, van den Bergh J, Reynaert P. Operative treatment of humeral shaft fractures. Acta Orthop Belg. 1997;63(3):170–7.
Putti AB, Uppin RB, Putti BB. Locked intramedullary nailing versus dynamic compression plating for humeral shaft fractures. J Orthop Surg (Hong Kong). 2009;17(2):139–41.
Radulescu R, Badila A, Nutiu O, Japie I, Terinte S, Radulescu D, et al. Osteosynthesis in fractures of the distal third of humeral diaphysis. Maedica (Buchar). 2014;9(1):44–8.
Raghavendra S, Bhalodiya HP. Internal fixation of fractures of the shaft of the humerus by dynamic compression plate or intramedullary nail: a prospective study. Indian J Orthop. 2007;41(3):214–8.
Rodriguez-Merchan EC. Compression plating versus hackethal nailing in closed humeral shaft fractures failing nonoperative reduction. J Orthop Trauma. 1995;9(3):194–7.
Singisetti K, Ambedkar M. Nailing versus plating in humerus shaft fractures: a prospective comparative study. Int Orthop. 2010;34(4):571–6.
Wali MG, Baba AN, Latoo IA, Bhat NA, Baba OK, Sharma S. Internal fixation of shaft humerus fractures by dynamic compression plate or interlocking intramedullary nail: a prospective, randomised study. Strategies Trauma Limb Reconstr. 2014;9(3):133–40.
Wang Y, Kayastha Y, Cao Y, Guo Z, Yuan Y, Bi Y. Outcome of humeral shaft fracture treated with intramedullary nail and plate fixation. J Coll Physicians Surg Pak. 2020;30(1):73–8.
Zhang R, Yin Y, Li S, Hou Z, Jin L, Zhang Y. Intramedullary nailing versus a locking compression plate for humeral shaft fracture (AO/OTA 12-A and B): a retrospective study. Orthop Traumatol Surg Res. 2020;106(7):1391–7.
Akalin Y, Sahin IG, Cevik N, Guler BO, Avci O, Ozturk A. Locking compression plate fixation versus intramedullary nailing of humeral shaft fractures: which one is better? A single-centre prospective randomized study. Int Orthop. 2020;44(10):2113–21.
Wen H, Zhu S, Li C, Chen Z, Yang H, Xu Y. Antegrade intramedullary nail versus plate fixation in the treatment of humeral shaft fractures: an update meta-analysis. Medicine (Baltimore). 2019;98(46): e17952.
Morshed S. Current options for determining fracture union. Adv Med. 2014;2014: 708574.
Cheng HR, Lin J. Prospective randomized comparative study of antegrade and retrograde locked nailing for middle humeral shaft fracture. J Trauma. 2008;65(1):94–102.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Beeres, F.J.P., van Veelen, N., Houwert, R.M. et al. Open plate fixation versus nailing for humeral shaft fractures: a meta-analysis and systematic review of randomised clinical trials and observational studies. Eur J Trauma Emerg Surg 48, 2667–2682 (2022). https://doi.org/10.1007/s00068-021-01728-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-021-01728-7