Abstract
Introduction
Current treatment guidelines for patients with severe TBI (sTBI) are aimed at preventing secondary brain injury targeting specific endpoints of intracranial physiology to avoid the development of metabolic crisis. We sought to identify factors contributing to development of metabolic crisis in the setting of a Multi-modality Monitoring and Goal-Directed Therapy (MM&GDTP) approach to patients with severe TBI.
Methods
Prospective monitoring of sTBI patients was performed, with retrospective data analysis. MM&GDTP was targeted to intracranial pressure (ICP) ≤ 20 mmHg, cerebral perfusion pressure (CPP) ≥ 60 mmHg, brain tissue oxygen pressure (PbtO2) ≥ 20 mmHg, and cerebral oxygen extraction measured by bi-frontal Near infrared Spectroscopy (NIRS) > 55%. Brain flow abnormality was defined by one of the following combinations: CPP < 60 mmHg with NIRS < 55% (Type 1), CPP < 60 mmHg with PbtO2 < 20 mmHg (Type 2), or PbtO2 < 20 mmHg with NIRS < 55% (Type 3). Cerebral micro-dialysate was analyzed hourly for glucose, lactate, pyruvate, glutamate, glycerol, and lactate/pyruvate ratio (LPR). Statistical analysis was performed with student t-test, chi-square and Pearson’s tests as applicable.
Results
A total of 109,474 consecutive minutes of recorded multimodality monitoring was available for analysis. There was a significant difference in the number of minutes of brain flow abnormalities between survivors and non-survivors: 0.8% (875) versus 7.49% (8,199), respectively (p < 0.05). The duration of Type 1–3 flow abnormality per patient was higher in non-survivors (5.7 ± 2.5 h) compared to survivors (0.7 ± 0.6 h) as well as the duration of metabolic crisis, namely, 5.2 ± 2.2 versus 0.6 ± 1.0 h per patient. The occurrence of severe metabolic crisis was associated with a Type 2 flow abnormality (CPP < 60 mmHg and PbtO2 < 20 mmHg), r = 0.97, p < 0.001, but not with Type 1 and 3.
Conclusions
Metabolic crisis can occur despite a MM&GDTP approach aimed at optimizing cerebral blood flow. Severe metabolic crisis is associated to failure to maintain CPP and PbtO2 above 60 and 20 mmHg, respectively. The occurrence of severe metabolic crisis portends a poor prognosis in patients with sTBI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Severe traumatic brain injury (sTBI) remains the leading cause of death and disability in children and adults accounting for more than 50,000 deaths each year and for the requirement of life-long assistance in a large subset of patients [1, 2]. Patients with sTBI are conventionally treated using the Brain Trauma Foundation (BTF) monitoring and the suggested treatment thresholds for intracranial pressure (ICP), cerebral perfusion pressure (CPP) and more recently, brain oxygen tension (PbtO2) [3, 4]. Recent evidence [5] suggests that during the first 48 h following sTBI, even when systolic blood pressure (SBP) is maintained > 90 mmHg there may be episodes of brain hypoperfusion; therefore, a higher systolic blood pressure may be necessary to prevent secondary brain injury.
In the absence of advanced monitoring techniques such near infra-red spectroscopy (NIRS) oxygen saturation, and cerebral microdialysis (CMD), it is unclear whether a CPP-PbtO2 targeted treatment strategy ensures an adequate balance between oxygen supply and demand. Theoretically, a CPP ≥ 60 mmHg with a PbtO2 ≥ 20 mmHg should provide the brain with the oxygen supply needed to prevent secondary brain ischemia from the activation of the hypoxia-induced pathways responsible for the progression of brain injury. The monitoring of the additional down-stream metabolic variables, such as lactate and pyruvate provided by the analysis of cerebral micro-dialysis, provide a more precise and specific assessment of brain metabolism.
To date, the correlation between cerebral oxygen dynamics obtained by surrogate variables such as SBP, CPP, NIRS oxygen saturation and brain metabolism remains unclear. It is within this context that we sought to determine the relationship between brain flow and oxygen variables, and brain metabolism as measured by CMD data in patients with sTBI.
Methods
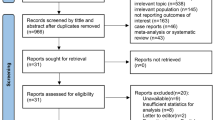
Patients with severe TBI admitted to our Level I trauma center were considered for inclusion. Patients were evaluated as part of an observational prospective database with Institutional Review Board approval. Inclusion criteria included an admission GCS score less than eight following initial emergency room resuscitation. Twenty consecutive patients who underwent the MM&GDTP (Fig. 1) for at least 3 days were analyzed. Patients with TBI from penetrating injuries and patients with bilateral fixed and dilated pupils were excluded from analysis.
Multimodality monitoring included ICP, CPP, PbtO2 (Licox, Integra Life Science; Saint Priest, France), bi-frontal brain oxygen saturation by NIRS (Covidien, Medtronic; Minneapolis, MN), and cerebral microdialysis (M Dialysis; Stockholm, Sweden). Cerebral microdialysis was performed via a dual lumen catheter inserted in juxtaposition to the brain oxygen catheter. The CMD catheter was perfused at a rate of 0.3 microL per minute and analyzed every hour. Samples were analyzed for glucose (normal values 14.4–46.8 mmol/L), lactate (2.0–3.8 mmol/L), pyruvic acid (119–213 µmol/L), glutamate (0.0–32.0 µmol/L), glycerol (38.0–126 µmol/L), and lactate/pyruvate ratio (LPR). All intracranial monitors were inserted within 2–4 h of admission except for patients who went directly to the operating room for evacuation of mass lesions who had monitors placed after the craniotomy.
The goal-directed therapy protocol included maintenance of ICP ≤ 20 mm Hg, CPP ≥ 60 mm Hg, PbtO2 ≥ 20 mm Hg, NIRS ≥ 55%, CMD LPR ≤ 25. Normothermia (37 °C) was maintained with dry water immersion technique utilizing Arctic Sun 5000 Temperature Management System (Medivance, Bard; Louisville, CO). Post-pyloric peptide-based enteral nutrition was started upon completion of the resuscitation phase and targeted to a respiratory quotient (RQ) measured by indirect calorimetry (IC) on day 3 and 5 of 0.83 with calories adjustment as needed based on the day 3 RQ, and positive nitrogen balance (NB) by day 7. All patients were sedated to synchrony with the ventilator, avoidance of cough and a modified Ramsey score of two with a combination of midazolam infusion and propofol.
Osmotherapy for elevated ICP included the administration of 3% saline and the addition of mannitol when appropriate. Burst suppression (BS) was initiated when ICP, low PbtO2 or low NIRS were not responsive to therapy. Burst suppression was achieved with an infusion of midazolam at a dose up to 15 mg/hr and propofol at a dose up to 100 µg/kg/min; infusions were titrated to 2–4 burst/screen while using continuous EEG (cEEG). Decompressive hemicraniectomy (DC) was performed in patients with surgical lesions causing mass effect and increased ICP.
Brain flow abnormality was defined by the occurrence of any one of the following combinations: CPP < 60 mmHg and NIRS < 55% (Type 1); CPP < 60 mmHg and PbtO2 < 20 mmHg (Type 2); PbtO2 < 20 mmHg and NIRS < 55% (Type 3). The number and duration of brain flow abnormality was determined for each group and on a per-patient basis.
Metabolic crisis (MC) was defined by an LPR > 25 and correlated with the presence of one of the three types of brain flow abnormality. Metabolic crisis was further defined as ischemic when the LPR was > 25 with pyruvate < 120 or secondary to mitochondrial dysfunction (MD) when with pyruvate > 120. Severe metabolic crisis included an LPR > 40 with pyruvate < 120 and glucose < 10 mmol/L. The frequency of MC was determined on a per-patient basis. Episodes of MC were dichotomized into the percentage of ischemic as opposed MD.
A multi-channel monitor (Moberg CNS Monitor, Moberg Research, Inc; Ambler, PA) recorded continuously ICP, CPP, PbtO2, NIRS which were averaged every minute. The hourly average of recorded data was used to assess the correlation between the brain flow variables with the hourly CMD data.
The 14-day mortality was predicted by the web-based CT CrasH model. In brief, CrasH6 uses a combination of four demographic and clinical variables, namely age, GCS, pupil reactivity and the presence of major extra-cranial injuries and the CT presence of petechial hemorrhages, obliteration of the third ventricle or basal cisterns, subarachnoid bleeding, midline shift and non-evacuated hematoma [6].
Statistical analysis
Data acquired included demographics, ISS, GCS, Abbreviated Injury Score- Head (AIS-H), Marshall class, brain flow oxygen crisis events (Type 1–3), metabolic crisis events, and mortality. Parametric data were analyzed with student t-test whereas nonparametric data were analyzed with chi-square or Fisher exact test. Correlation was established with Pearson and Spearman test. Data are presented as means ± standard deviation, median and IQR, and as proportions. Statistical significance was accepted to correspond to a p value < 0.05.
Results
Twenty consecutive patients with sTBI, who underwent MM&GDTP for at least three days were identified. Sixteen patients sustained sTBI from a motor vehicle crash and four from a fall. Shown in Table 1 are the demographic data, the injury severity scores by GCS, AIS-H, ISS, and Marshall classification, and the predicted mortality (PM) by the CrasH model. In 18 patients post-pyloric enteral feeding was started within 24 h of injury upon completion of the resuscitation phase that included restoration of normovolemia, acid–base balance and appropriate minute ventilation and in two patients between 24 and 48 h. All 20 patients had indirect calorimetry on day 3 and 5 with measurement of nitrogen balance by day 7. By day 5, all patients had achieved a RQ 0.83 with a positive NB by day 7.
Brain flow oxygen crisis events
The duration of monitoring in survivors was 75,910/13 = 5839 min/pt, which corresponds to 97 h/pt, or conversely, to 4.0 days/pt as opposed to a duration of monitoring of 33,564/7 = 4794 min/pt, 79.9 h/pt or conversely, 3.3 days/pt in NS. The shorter duration of monitoring in non-survivors (NS) was due to the death of four patients between day 3 and 4 of the MM&GDTP. Endpoints of goal-directed therapy of ICP, CPP, PbtO2, and NIRS were achieved 97.2% of the recorded time. However, despite the protocolized endpoints of therapy, brain flow oxygen crisis events occurred in the 20 patients for a total of 3128/109,474 (2.8%) minutes. The distribution of brain flow oxygen crisis included 69 min (2%) of Type 1, 2889 min (92%) of Type 2, and 170 min (6%) of Type 3 crisis. Type 1–3 brain flow abnormality was recorded in NS for 2515 of 33,564 min (7.49%) as opposed to survivors who had 613 min of 75,910 min (0.80%) of brain flow abnormality. NS had 5.1 ± 7.9 h/patient of Type 2 brain flow abnormality as opposed to 0.5 ± 0.6 h/patient for survivors (p = 0.04) (Table 2).
Metabolic crisis
Metabolic crisis was identified in 983 of the 1,771 (56%) CMD samples despite the attempt at achievement of the thresholds of the goal-directed protocol. LPR values of 25–40 were identified more frequently than LPR > 40, 781 (86%) and 202 (14%), respectively (p < 0.05). Non-survivors had a statistically higher number of LPR > 40 compared to survivors, 104/316 (32.9%) and 98/667 (14.7%), respectively (p < 0.05).
Severe metabolic crisis, defined by an LPR > 40 with pyruvate < 120 and glucose < 10 mmol/L, was identified in 71/983 (4.0%) of MC; 62 (87%) hours in the seven NS as opposed to only 9 hours (13%) in the 13 survivors. The duration of severe metabolic crisis per patient was greater in non-survivors than in survivors, 5.8 ± 2.2 vs. 0.6 ± 1.0 h, respectively (Table 3). While the metabolic crisis was secondary to ischemia in NS, it was attributable to mitochondrial dysfunction in survivors (Table 4). There was a strong association between the presence of Type 2 brain flow abnormality and the occurrence of severe metabolic crisis (r = 0.97, p = 0.01).
Outcome
The overall PM by the CrasH model was 38 ± 24. Two patients underwent craniotomy followed by the placement of intracranial monitors in the operating room, both were among the survivors. Four patients with increased ICP that remained refractory to osmotherapy and developed mass lesions underwent DC within 24 h of initiation of the treatment protocol; three survived and one died. The median and interquartile range of the length of stay for the 13 survivors was 18 (18–20) days. In the 13 patients who survived there was an association between the number of metabolic crisis events and lower Glasgow Outcome Scores (r2 = 0.292).
Seven of the 20 patients died yielding a mortality of 35%. The causes of death included brain death in five patients, one cardiac arrest from TBI, and one from withdrawal of care. The median and interquartile range of time to death was 6 (5–23) days. There was no difference between survivors and NS with respect to age, gender distribution, GCS, AIS-H, and Marshall class and Marshall unfavorable outcome score; however, NS had a statistically significant higher ISS score and a higher PM compared to survivors.
Discussion
Current treatment guidelines for patients with sTBI emphasize the prevention of secondary brain injury by targeting treatment thresholds to specific endpoints of ICP, CPP, PbtO2 and oxygen saturation values for at least the first 48 h after injury [7, 8]. However, CMD data suggest that metabolic crisis may occur even when CBF and brain oxygen supply is presumed normal in the setting of normal ICP and CPP [9]. As a result, ICP-CPP with PbtO2 targeted therapy has become a common treatment paradigm [4, 10,11,12]. In this study, we sought to determine the correlation between measurable variables that contribute to brain flow and oxygen input with the downstream biochemical variables measured by cerebral microdialysis. A secondary objective was to determine the association between multimodality monitoring variables, CMD, and outcome.
MM&GDTP endpoints and rationale
The selection of the endpoints of our protocol in combination with the use of CMD data was based on physiological and pathophysiological principles applicable to patients with sTBI. Temperature control is vital in critical patients. Hyperthermia, which occurs commonly after sTBI, has been shown to be associated with a worse outcome. We sought to limit the brain oxygen consumption and elected to target temperature control to normothermia [13].
The target CPP ≥ 60 mmHg with a PbtO2 > 20 mmHg with a NIRS > 55%, incorporates the individual monitor endpoints into one goal. Targeting NIRS > 55% is based on the physiologic assumption that a decreased saturation may indicate suboptimal cerebral blood flow (CBF). Increased oxygen extraction (O2Ex) is typically a compensatory response needed to maintain consumption constant in the setting of decreased oxygen delivery [14]. We chose to group variables together as we do not routinely use one monitor in isolation. However, when two variables are not at their target values, interventions may be undertaken to attain the goals. The targeted nutritional approach was based on recent evidence showing that aggressive nutritional support in patients with sTBI provides a survival advantage [15]. The duration of the treatment was based on evidence suggesting that CMD LPR ratios typically do not normalize for at least 3 days following sTBI as well as the 5-day FDA approved use of many of the intracranial monitoring devices [16].
Metabolic crisis
The main observation of our analysis is that patients with sTBI, despite attempts at adequate resuscitation of ICP, CPP, PbtO2, and oxygen saturation, experience episodes of brain flow oxygen crisis as well as metabolic crisis. Monitoring and maintaining adequate CPP and PbtO2 is a key component of neurocritical care monitoring. We observed that 97% of the events with CPP < 60 mmHg and PbtO2 < 20 mmHg were associated with severe metabolic crisis. Moreover, this was the most common finding in patients that did not survive. Our findings corroborate those of Stein and associates [17] in a group of 89 patients with moderate to severe TBI where metabolic crisis occurred despite adequate resuscitation.
Our experience shows that the most common type of brain flow oxygen crisis is a combination of CPP < 60 mmHg with a PbtO2 < 20 mmHg. Moreover, this is more likely to be associated with severe metabolic crisis and ischemia as the underlying etiology of the metabolic crisis as compared to the combinations of CPP < 60 mmHg and NIRS < 55% or PbtO2 < 20 mmHg and NIRS < 55%. Our data supports that of Nelson and colleagues [18] who found a weak relationship between ICP and/or CPP and perturbed metabolism in 90 patients with more than 7350 hourly CMD samples. Unfortunately, due to the small sample size of our study we could not perform multivariate analyses and were unable to correlate CMD values with mortality. We are intrigued by the lack of a correlation between PbtO2 < 20 and NIRS < 55% with ischemia, especially since increased O2Ex has been previously correlated with an increased LPR [19]. There is an obvious association between Type 2 brain flow abnormality (CPP < 60 mm Hg and Pbto2 < 20 mmHg) and severe MC. It is clear from this association, as opposed to the lack of association between Type 1 and Type 3 abnormalities and MC, that an increased oxygen extraction at the bifrontal level is not necessarily associated with changes of oxygen tension at the mitochondrial level since the LPR is not affected. This corroborates the findings of Menon and associates [20] who have reported that O2Ex may not accurately reflect the presence of tissue hypoxia after TBI because increased diffusion barriers may reduce the ability to increase O2Ex in response to hypoperfusion.
It is plausible that elevated LPR, whether secondary to brain flow oxygen abnormality or occurring in the setting of adequate CPP, PbtO2, and NIRS, is a potentially useful therapeutic target that should be incorporated into monitoring and management strategies. Episodes of metabolic crisis associated with a brain flow oxygen crisis of CPP < 60 mmHg and NIRS < 55% or PbtO2 < 20 mmHg and NIRS < 55%, respectively, can be addressed by increasing fractional oxygen. Moreover, one or more of the input variables may be affected by narcotics, sedatives and vasopressors either alone or in combination. In our study, goal endpoints of resuscitation (ICP, CPP, PbtO2, and NIRS oxygen saturation) were achieved 97% of time yet metabolic crisis was observed in 56% of the CMD samples collected. These findings corroborate and further extend those of Stein et al. [17] by showing that even the addition of PbtO2 as an endpoint of resuscitation fails to preclude the incidence of metabolic crisis and potentially poor outcomes.
The metabolic crises that occur with normal cerebral flow and oxygen dynamics require an approach aimed at decreasing brain oxygen demand because of the uncoupling of the systemic variables and the brain oxygen utilization. In the absence of CMD data it is unlikely that any treatment would be undertaken in the setting of the achievement of thresholds values of ICP, CPP, PbtO2, and NIRS. The results of our study suggest that direct monitoring of brain metabolism rather that blind achievement of cerebral flow and brain oxygenation endpoints is necessary to minimize the risk of cellular injury that may be caused by an imbalance between brain oxygen demand and supply due to increased energy demand.
Our data further show that the cumulative duration of brain flow oxygen crisis, Type 2 abnormality, and severer metabolic crisis are predictors of mortality in patients with sTBI. Taken together, our data suggests that limiting both the incidence and duration of brain flow oxygen crises and metabolic crisis would have a direct impact on improving outcome in patients with severe TBI.
However, in the absence of increased brain oxygen demand, it remains unclear why metabolic crises occur and persist despite the sustained achievement of adequate brain oxygen supply provided by adequate cerebral flow dynamics. We observed that some patients with normal cerebral flow dynamics and normal oxygen extraction as depicted by NIRS > 55%, a value above the anaerobic threshold, have elevated LPR. This introduces the possibility of an oxygen debt secondary to mal distribution of CBF, namely, increased flow to low demand regions of the brain. Such events could be associated with compromised vaso-reactivity, since the association between cerebral vasoconstriction/vasodilatation and increased LPR has been established in patients with TBI [21]. This condition can be unmasked by the use of low dose systemic vasodilator such as prostacyclin at 0.5–1.0 ng/kg/min or theoretically by local vasodilators. The beneficial effect of systemic prostacyclin, a powerful vasodilator and potent inhibitor of platelet aggregation with fibrinolytic and cytoprotective properties, has been documented in a patient with a traumatic focal brain lesion associated with increased LPR in the setting of normal CPP and ICP [22]. The addition of CBF monitoring may identify the specific impact of local blood flow on these events.
It is clear that in the presence of adequate brain flow and oxygen variables, an abnormal LPR with a pyruvate < 120 µmol and glucose < 10 mmol/L may indicate the need to intentionally suppress metabolism. The selection of drugs would be based on those that do not affect mitochondrial function while utilizing continuous EEG to decrease the metabolic rate of the brain. The presence of the abnormal LPR in the setting of normal input variables would indicate an imbalance between brain oxygen supply and demand. In the setting of optimized supply as documented by the achievement of the target input thresholds, a therapeutic alternative is to decrease oxygen demand by decreasing the metabolic rate of the brain.
Limitations of the study
The study has the following limitations. First, it is based on observational data that can only show relationships and correlation without causal evidence that brain flow oxygen variables affect CMD data and outcome. Second, due to the small number of patients, only univariate analyses were possible, therefore, no conclusions can be reached regarding the independent predictive value of brain flow oxygen variables and CMD data on patients’ outcome. Third, measurements of PbtO2 are restricted to a small cerebral volume with the assumption that it reflects hemispheric conditions. Fourth, despite an early association between the number of severe metabolic crisis events and lower Glasgow Outcome Scores in the survivors, the absence of six- and 12-months functional outcome scores, and the limited number of patients in the study, prevents us from drawing any conclusion regarding the association of the number of metabolic crisis events with long-term functional outcome.
Conclusions
We have clearly shown that metabolic crisis may occur despite attempts at adequate resuscitation of intracranial physiology including ICP, CPP, PbtO2, and oxygen saturation. Our data suggest that mitochondrial dysfunction is the most common etiology for the impaired metabolism and that severe metabolic crisis may portend a poor prognosis in patients with sTBI. Based on the conclusions of our study, we believe that further studies are warranted to validate the usefulness of an approach that uses a Multimodality Monitoring and Goal-Directed Therapy Protocol with monitoring of cerebral microdialysis data for the treatment of patients with severe TBI.
References
Langlois J, Rutland-Brown W, Wald M. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21(5):375–8.
Thurman D, Alverson C, Dunn K, Guerrero J, Sniezek J. Traumatic brain injury in the United States: a public health perspective. J Head Trauma Rehabil. 1999;14(6):602–15.
Brain Trauma Foundation American Association of Neurological Surgeons, Congress of Neurological Surgeons. Guidelines for the management of severe head injury. J Neurotrauma. 2007;24:S1–106.
Bratton SL, Chestnut RM, Ghajar J, McConnell HFF, Harris OA, Hartl R, Manley GT, Nemecek A, Newell DW, Rosenthal G, et al. Guidelines for the management of severe traumatic brain injury. X. Brain oxygen monitoring and thresholds. J Neurotrauma. 2007;24(Suppl 1):S65–70.
Brenner M, Stein DM, Hu PF, Aarabi B, Sheth K, Scalea TM. Traditional systolic blood pressure targets underestimate hypotension-induced secondary brain injury. J Trauma. 2012;72:1135–9.
MRC CrasH Collaborators. Predicting outcome after traumatic brain injury: practical prognostic models based on large cohort of international patients. BMJ. 2008;336:425–9.
Stein SC, Georgoff P, Meghan S, Mirza KL, Falaky EI. Relationship of aggressive monitoring and treatment to improved outcomes in severe traumatic brain injury. J Neurosurg. 2010;112(5):1105–12.
Stein SC, Georgoff P, Meghan S, Mizra K, Sonnad SS. 150 years of treating severe traumatic brain injury: a systematic review of progress in mortality. J Neurotrauma. 2010;27(7):1343–53.
Stiefel MF, Udouteuk JD, Spiotta AM, Gracias VH, Goldberg A, Maloney-Wilensky E, Bloom S, LeRoux PD. Conventional neurocritical care and cerebral oxygenation after traumatic brain injury. J Neurosurg. 2006;105:568–75.
Bardt TF, Unterberg AW, Hartl R, Kiening KL, Schneider GH, Lanksch WR. Monitoring of brain tissue PO2 in traumatic brain injury: effect of cerebral hypoxia on outcome. Acta Neurochir Suppl. 1998;71:153–6.
Chang JJ, Youn TS, Benson D, Mattick H, Andrade N, Harper CR, Moore CB, Madden CJ, Diaz-Arrastia RR. Physiologic, functional outcome correlates of brain tissue hypoxia in traumatic brain injury. Crit Care Med. 2009;37(1):283–90.
Valadka AB, Gopinath SP, Contant CF, Uzura M, Robertson CS. Relationship of brain tissue PO2 to outcome after severe head injury. Crit Care Med. 1998;26(9):1576–81.
Greer DM, Funk SE, Reaven NL, Ouzounelli M, Uman GC. Impact of fever on outcome in patients with stroke and neurological injury. Stroke. 2008;39:3029–35.
Siegal J, Kohli C. Correlation of noninvasive cerebral oximetry with cerebral perfusion in the severe head injured patient: a pilot study. J Trauma. 2002;52:40–6.
Hartl R, Gerber LM, Ni Q, Ghajar JG. Effect of early nutrition on deaths due to severe traumatic brain injury. J Neurosurg. 2008;109:50–6.
Timofeev I, Carpenter KLH, Nortje J, Al-Rawi PG, O’Connell MT, Czosnyka M, Smielewski P, Pickard JD, Menon DK, Kirkpatrick PJ, et al. Cerebral extracellular chemistry and outcome following traumatic brain injury: a Microdialysis study of 223 patients. Brain. 2011;1:1–11.
Stein NR, McArthur DL, Etchepare M, Vespa PM. Early cerebral metabolic crisis after TBI influences outcome despite adequate hemodynamic resuscitation. Neurocrit Care. 2012;17:49–57.
Nelson DW, Thornquist B, MacCallum RM, Nyström H, Holst A, Rudehill A, Wanacek M, Bellander BM, Weitzberg E. Analyses of cerebral microdialysis in patients with traumatic brain injury: relations to intracranial pressure, cerebral perfusions pressure and catheter placement. BMC Medicine. 2011;9:21.
Hutchinson PJ, Gupta AK, Fryer TF, Al-Rawi PG, Chatfield DA, Coles JP, O’Connell MT, Kett-White R, Minhas PS, Aigbirhio FI, et al. Correlation between cerebral blood flow, substrate delivery, and metabolism in head injury: a combined microdialysis and triple oxygen positron emission tomography study. J Cereb Blood Flow Metab. 2002;22(6):735–45.
Menon DK, Coles JP, Gupta AK, Fryer TD, Smielewski P, Chatfield DA, Aigbirhio F, Skepper JN, Minhas PS, Hutchinson PJ, et al. Diffusion limited oxygen delivery following head injury. Crit Care Med. 2004;32(6):1384–90.
Asgari S, Vespa P, Hu X. Is there any association between cerebral vasoconstriction/vasodilatation and microdialysis lactate to pyruvate ratio increase? Neurocrit Care. 2013;19(1):56–64.
Reinstrup P, Nordström CH. Prostacyclin infusion may prevent secondary damage in pericontusional brain tissue. Neurocrit Care. 2011;14:441–6.
Author information
Authors and Affiliations
Contributions
Design: CPM. Data acquisition: CS. Analysis: CPM. Interpretation of data: CPM. Drafting of the manuscript: CPM, KP, PP. Critical revision: CPM, PP, JM, VDD.
Corresponding author
Ethics declarations
Conflict of interest
Corrado P. Marini, Christy Stoller, John McNelis, Vito Del Deo, Kartik Prabhakaran, and Patrizio Petrone declare that they have not conflict of interest.
Informed consent
This study is a retrospective chart review, and as such, there is no need for an informed consent. The New York Medical College Institutional Review Board approved the study design and methodology.
Rights and permissions
About this article
Cite this article
Marini, C.P., Stoller, C., McNelis, J. et al. Correlation of brain flow variables and metabolic crisis: a prospective study in patients with severe traumatic brain injury. Eur J Trauma Emerg Surg 48, 537–544 (2022). https://doi.org/10.1007/s00068-020-01447-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-020-01447-5