Abstract
The number of geriatric patients is increasing. These patients exhibit specific characteristics, which influence the type of fracture care. Many patients have comorbidities, which make them more vulnerable to surgical procedures. The soft tissue envelope around the fracture often is compromised due to pre-existing diseases such as diabetes, chronic venous insufficiency or peripheral vascular disease. Bone mineral density has decreased, which enhances the risk of implant loosening. The goals of treatment differ from those, which are valid for younger adults. Primary goal is preserving independency of the elderly patient in his activities of daily life. Advantages and drawbacks of surgical procedures have to be balanced with those of conservative treatment. Fractures of the lower extremities will more often need surgical treatment than fractures of the upper extremities. Patient´s autonomy is best obtained by creating high stability in the fracture plane, which enables motion and weight-bearing. Second priority is prevention of general and local post-operative complications by the use of less invasive surgical procedures. Restoring anatomy and optimal function are less important goals. The implants, which are used, are inserted through small incisions, placed deep under the skin and use long anatomic or osseous corridors. Intramedullary devices have important advantages. This paradigm shift takes the special challenges and requirements of geriatric patients into account.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The number of elderly persons is steadily increasing in our societies. Thanks to high quality of life and high standard of medical care, life expectancy has steadily grown in recent decades. Life expectancy for a new born female is 83.4 years and for a new born male 78.6 years in Germany in the year 2018 [1]. The median age of the German population was 45.9 years in 2015, the second highest in the world after Japan [2]. In many European populations, median age is similar to that of Germany. Due to this matter of facts, our societies are confronted with a number of interrelated problems such as the increasing demand for adapted housing (service flats), a pension with which one can cover the costs of daily life; and rapidly growing costs for medical care.
Among elderly persons, many remain healthy and independent until in high age. Others need continuous medical or physical support, but remain mobile, still others are completely dependent, wheelchair bound or bedridden. The trauma surgeon needs a differentiated view on these varying groups. Older persons suffer more often from medical diseases than their younger counterparts. These “comorbidities” influence outcome, when older persons suffer a trauma. In a US study on 32.440 patients of 55 years of age and older, who suffered hip fractures, more than 95% had at least one comorbidity. Hypertension, deficiency anemia, and electrolyte disorders were the most common [3]. Loss of physiological reserves and comorbidities are both considered as independently influencing factors in regard to morbidity and mortality after trauma in the elderly [4]. Osteoporosis, which is characterized by a decrease of bone mineral density, is a disease which is often seen in elderly persons, especially in females [5]. Due to visual limitations, malnutrition, hypotrophic muscles, polypharmacia or problems with balance, there is a higher risk of falls in the elderly population. Due to osteoporosis, domestic falls often lead to osteoporotic fractures. Typical osteoporotic fractures are vertebral compression fractures, hip fractures, proximal humerus and distal radius fractures [6]. They are considered as “indicator-fractures” for osteoporosis [7]. The number of osteoporotic fractures increases in parallel with the increase of elderly persons and is expected to further grow in the next decades [8]. Also, the number of fragility fractures of the pelvis is steadily growing [9, 10].
This evolution puts the trauma surgeon for new challenges and new questions. Are the fracture patterns in elderly patients similar to those of the younger adults? Which are the most important goals of treatment? Do the same rules of emergency and urgency apply? Can we use the same principles of fracture treatment? This review looks at principles of fracture treatment since the foundation of the Association for the Study of Internal Fixation (AO/ASIF) in the late 50s of the previous century and its later amendments [11]. Arguments are given for further adaptations, which specifically take the characteristics and requirements of elderly patients into account [12].
Operative fracture care
In the 50s of the last century, fracture care was mainly conservative. The philosophy of Lorenz Böhler, which was published in his standard work on conservative fracture treatment, was widespread and respected in Europe [13]. There were some surgeons, who promoted operative fracture care at that time. External fixation was propagated by Albin Lambotte [14], compression plate osteosynthesis by Robert Danis [15] and intramedullary nailing by Gerhard Küntscher [16]. Although these surgeons published excellent results, their methods were not used by many. Major issues were manufacturing of bio-acceptable implants, fabrication of precise instruments, teaching of the surgeons and distribution of the surgical materials in the hospitals.
At the end of the 50s, Müller, Allgöwer, Schneider and Willenegger were able to convince Swiss insurance companies of the huge advantages of their method of treatment. The loss of working capacity after suffering an upper or lower leg fracture was very high at that time. Immobilization took several months, most of the patients could not regain their previous activity, and a number of them suffered from lifelong sequelae such as malalignment, shortening, non-union or infection. The previously mentioned Swiss surgeons founded in 1958 the Association for the Study of Internal Fixation (ASIF) also known as Arbeitsgemeinschaft für Osteosynthesefragen (AO). The association was built on four pillars: operative fracture care, teaching, documentation, research and development. The method of fracture fixation was based on open reduction and internal fixation (ORIF), mainly by plate osteosynthesis. The original principles of AO were anatomical reduction, rigid fixation, preservation of blood supply, early active mobilization [17]. Following these principles, fracture fragments were exposed, reduced and stabilized, long-time immobilization and malalignment avoided, and early onset of active motion possible. These principles were “universally” valid for joint, metaphyseal and diaphyseal fractures of the upper and lower extremities (Fig. 1a–e). Thanks to an excellent and efficient cooperation with industry partners, an immense variety of plates, screws and reduction tools was developed [11]. Young, healthy adults, suffering from traffic, working or sports accidents were the primary target population of this treatment method. Thanks to a systematic and rigid educational program, which is still one of the main pillars of the AO-Foundation, the method became widespread and obtained excellent results. Introduction of AO principles was a revolution in fracture treatment and forms the base of modern fracture treatment.
a Seventy-eight-year-old woman after fall at home. A–P view of the right humerus. There is a spiral fracture in the distal third of the shaft. b Transscapular view. c Intraoperative view of the operation site. A posterior approach was chosen. The radial nerve was identified and mobilized d post-operative A–P view. An open, anatomical reduction and internal fixation was carried out. A posterior plate with screw osteosynthesis was performed. The spiral fracture was reduced and closed with a lag screw. The plate had the function of a buttress plate. e Post-operative transscapular view
Functional reduction instead of anatomical reduction
Although the method marked an immense progress in fracture care, it was also combined with its own, sometimes serious complications [18, 19]. This was mainly due to violation of the principles of osteosynthesis, published by the founders of AO. When fracture stabilization was not adequate, implant loosening with secondary fracture displacement, malalignment, delayed union or non-union occurred. Aggressive exposure with periosteal stripping of fracture fragments led to bone necrosis. Wound healing problems due to large incisions in traumatized soft tissues, soft tissue defects, bone necrosis and deep infection were a “lethal” combination, which led to many operative revisions, bone defects, and sometimes loss of the extremity [20]. The risk of complications was higher in patients with pre-existing comorbidities [21]. It became clear that open reduction and internal fixation of every fracture fragment could bring more drawbacks than advantages. Whereas anatomical reduction of articular fractures remained an indispensable condition for optimal joint function, this was not the case for extra-articular fractures. The principle of “anatomical reduction” was adapted to “functional reduction” in the early 90s. The ultimate goals of stable fixation and early mobilization remained unchanged, the methods of fixation changed to less invasive techniques, avoiding the devasting complications described above. The AO principles of the 1990s were functional reduction, stable fixation, preservation of blood supply, early active mobilization [22]. For fixation of multi-fragmental meta-diaphyseal fractures, incisions became smaller and long implants were used to bridge an area of instability. Periosteal blood supply was left untouched (Fig. 2a–f) [23]. The absolute stability of a compression plate osteosynthesis after anatomical reduction and fixation was abandoned for a relative, yet adequate stability. Preserved periosteal blood supply and relative stability support secondary fracture healing via periosteal callus. Simultaneously, due to the bridging, the function of the nail or plate changed from weight-sharing to weight-bearing. As a consequence, the risk of implant failure in cases of delayed fracture healing became higher.

(From Seligson D, Severance D, Roberts C. Distal femur. Figure 20.4 of Chap. 20 in “Intramedullary Nailing. A comprehensive guide.” (Rommens PM, Hessmann MH. Eds) Springer-Verlag London 2015 pp. 317–329. With permission)
a Thirty-four-year-old motorcycle driver with severely comminuted right intra-, inter- and supracondylar femoral fracture. b Lateral view. c Post-operative A–P view of the distal femur with knee joint. The intra- and intercondylar fracturess have been treated with open anatomical reduction and internal fixation. The multifragmental supracondylar fracture has been bridged with a retrograde supracondylar nail. The displaced metaphyseal fracture fragments have been left intact. d Lateral view. e A–P view of the distal femur and knee joint after 1 year. The metaphyseal fractures are consolidated and bridged with periosteal callus. f Lateral view.
Internal plate fixators
With the introduction of angular stable plates, the function of plate osteosynthesis moved toward internal fixation. Dynamic compression plate (DCP) designs obtained stability through direct pressure of the plate against the cortical surface. Friction between plate and cortex was so high that movement during stress or weight-bearing was minimized. Disadvantage was stress shielding, which was responsible for weakening of bone and bone loss below the plate [24]. The internal fixator is characterized by an angular stability between the plate and the screws. The plate acts as a bridging implant, leaving the fracture fragments untouched. As the plate does not touch cortical bone, stress shielding is prevented. Thanks to these characteristics, vitality of bone fragments remains very good and motion between fragments boosts callus formation. Techniques of stabilization changed towards less invasive surgery with smaller incisions, using long implants and fewer screws, which bridge the fracture gap but do not compress it. The AO principles changed to preservation of blood supply, functional reduction, stable fixation, and early active mobilization [25, 26].
Special features of elderly trauma patients
Ageing is characterized by a continuous decline in physiological reserves. Moreover, ageing is connected with the appearance of diseases. Almost all geriatric patients have comorbidities, which make them more vulnerable in the posttraumatic phase [3]. Both, loss of physiological reserves and comorbidities are considered as independently influencing factors in regard to morbidity and mortality after trauma [4]. The most important declines of organ function concern the heart, lungs, kidneys and liver. A reduced cardiac output and a low physiologic reserve of the lungs limit the ability to respond to hemodynamic instability due to blood loss. As a result of reduced functions of kidneys and liver, clearance of metabolic and toxic agents and drugs is delayed or hindered [27, 28]. An increasing number of elderly persons receive anticoagulants for prophylactic (e.g. atrial fibrillation, after vascular stent implantation) or therapeutic (after thromboembolism) reasons. These drugs, especially coumadin, low molecular weight heparin and factor X-blockers, may prolong duration and volume of blood loss after trauma [29]. Chronic obstructive pulmonary disease (COPD) is a common disease of the elderly and is often connected with congestive heart failure. COPD leads to a reduced vital capacity and pulmonary function, which increases the risk of pulmonary complications during and after surgery [30]. Anemia is frequently detected in the elderly. Long surgical procedures, which may be connected with important blood loss, may endanger the hemodynamic balance in these patients [31]. The characteristics, which are mentioned above, are arguments against long-lasting surgical procedures with large incisions, important blood loss, low body temperature and high antigenic load [32].
Osteoporosis is a common disease in elderly persons. It is characterized by a decrease in bone mineral density. There is a resorption of cortical and cancellous bone, which makes the bone more vulnerable to external and internal stresses. A similar trauma mechanism will lead to more complex injuries than in the younger adult [5, 6]. The loss of bone mass directly influences the holding power of implants for fracture treatment. A biomechanical construct, which is adequate in younger adults, may fail in elderly persons with osteoporosis [34]. Implants for osteosynthesis in osteoporosis must use the longest possible corridors, be angular stable and be inserted in regions with the most bone mineral density [35,36,37].
Diabetes mellitus is often diagnosed in persons older than 65. This disease is responsible for an important number of consecutive complications such as peripheral microangiopathy, peripheral neuropathy, retinopathy with reduced eyesight and wound healing disturbances [38]. The soft tissue envelope around the fracture of older persons is frequently altered due to other concomitant diseases such as venous insufficiency, peripheral arterial disease, due to long-term cortisone intake or to pre-existing infections or decubitus. In these circumstances, there is a much higher risk of local complications when large incisions are made through compromised soft tissues or when long-lasting surgeries with aggressive manipulations are performed.
Minimal invasive surgery, high stability and full weight-bearing
Consequently, principles of fracture treatment in geriatric patients must be adapted. Most important goal is preserving the patient´s independency, which enables participation in activities of daily life. Therefore, the patient must become pain free and mobile. The advantages and drawbacks of operative fracture care must be compared with those of conservative treatment. In patients with high risks of general or local post-operative complications, conservative treatment must be considered. In fractures with a good intrinsic stability, immobilization with a splint or orthosis may be sufficient. This is especially valid for fractures of the upper extremity (e.g. impacted proximal humerus, impacted distal radius) [39, 40].
When operative treatment is chosen, restoring stability has the highest priority. Second priority is less invasive surgery. Restoring anatomy or optimal function becomes less important. In some fracture types, restoration of stability has higher priority as preservation of blood supply. This paradigm shift of operative fracture care seems to contradict previous principles, where restoration of anatomy and function were the ultimate goals. The shift is nevertheless justified in the light of the different characteristics and functional requirements of geriatric patients. Optimal function of a shoulder, knee or hip joint was often not present at the time of accident. A better function than before the accident cannot be expected. Being independent in activities of daily life such as personal hygiene, cooking, short walking, or shopping is much more important than optimal function of a joint.
This shift of priorities has already been applied since decades in the treatment of intracapsular and intertrochanteric hip fractures. Intracapsular hip fractures are treated with parallel screws or a dynamic plate-screw device, which accepts shortening of the neck for better impaction of the fracture fragments [41]. Intertrochanteric hip fractures are treated with a dynamic hip screw or a cephalomedullary implant. Both allow impaction of the head and neck fragment with shortening of the leg and medialization of the femoral shaft (Fig. 3a–c). Stability and less invasive surgery are considered as higher priorities than restoration of anatomy [42].
a Eighty-three-year-old female with unstable intertrochanteric fracture of the right hip after a domestic fall. A-P-view of the right hip joint. b post-operative A–P view. The fracture was stabilized with a dynamic hip screw with the head and neck fragment in slight valgus position. c Post-operative A–P view after 6 weeks. Impaction of head and neck fragment with shortening and medialization of the femoral shaft took place. The greater trochanter is lateralized. There is callus formation. The patient is limping with crutches and full weight-bearing
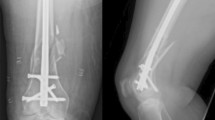
The second priority is minimizing the burden of surgery and preventing local complications. Therefore, the surgical procedure must be as less invasive as possible. The surgeon consequently must choose techniques, which use small incisions, implants which are placed deep under the skin, inside the bone or use long natural or anatomic corridors. Some percutaneous techniques restore stability for the price of blood supply: vertebroplasty for osteoporotic compression fractures of the thoracolumbar spine, and sacroplasty for sacral insufficiency fractures [43, 44]. In long bone fractures, it is advantageous to use intramedullary implants for fracture stabilization. The implant is embedded inside the bone, which minimizes the risk of healing problems of the soft tissue envelope. A long and thick nail acts as a weight-sharing implant and reduces stresses in the fracture plane. There is a smaller risk of implant loosening than in plate osteosynthesis, whereas the risk of axial malalignment is higher [45]. Intramedullary nailing is recommended for treatment of metapyseal fractures of the proximal humerus, unstable fractures of the proximal femur, distal femur, proximal and distal tibia [46]. The entry portal through the shoulder or knee joint puts the cartilage of the joint at risk. But the advantages of small incisions and no-touch of the fracture area overweigh disadvantages of limited joint damage and axis deviation. Intramedullary devices bring a clear advantage in distal fibula fractures with pre-existing and posttraumatic soft tissue compromise [47, 48]. The distal tibia nail protects the soft tissues and realizes high stability (Fig. 4a–e) [49]. In calcaneal fractures, large lateral approaches should be avoided as they bear a high risk of wound healing problems. An intra-osseous implant is a good alternative, creating high stability and allowing early weight-bearing when combined with an orthotic device [50].
a A seventy-three-year-old female was hit by a car. She suffered a left first-degree open oblique distal tibia and multifragmental fibula fracture. A–P view of the left lower leg. b lateral view. c Clinical view at admission. d Post-operative A–P view 16 weeks after trauma. The distal tibia fracture was stabilized with a distal tibia nail (DTN®), which was inserted through the medial malleolus. The fibula fracture was bridged with an angular stable plate. e Lateral view. The patient is walking with full weight-bearing (Courtey Dr. T. Sawaguchi, Toyama, Japan)
The incidence of fragility fractures of the spine is also increasing. The usual technique of bridging fixation of fractured vertebra through posterior spondylodesis of the adjacent levels must be adapted for osteoporotic fractures. There is a high correlation between pedicle pull-out strength and bone mineral density [51]. To avoid fixation failure in fragility fractures of the spine, the dorsal instrumentation should be extended to at least two segments above and below the fracture vertebra [52]. Moreover, pedicle screws should be augmented with bone- or calcium-based cements [53, 54]. A combination of extended dorsal instrumentation, pedicle screw augmentation and augmentation of the fractured vertebrae obtains the highest stability.
Fragility fractures of the pelvic ring are an upcoming entity among osteoporotic fractures [55]. There is reluctance towards operative treatment, as conventional surgery uses long incisions, takes long time and is connected with significant blood loss. Stabilization of slightly displaced fragility fractures is possible though smaller incisions, when using implants, which are placed in long corridors. The trans-sacral bar osteosynthesis and the retrograde transpubic screw are good examples of minimal-invasive techniques, which create high stability (Fig. 5a–c) [56,57,58]. In geriatric acetabular fractures, single anterior approaches such as the ilioinguinal or modified Stoppa approach are well tolerated and adequately buttress typical anterior column fractures. Minor steps in the joint are well tolerated, as long as the patient is allowed to bear weight early (Fig. 6a–e) [59,60,61].
a Sixty-eight-year-old female with pain in the low back after a fall. Pelvic A–P overview shows right-sided superior and inferior pubic rami fractures. b Oblique CT-reconstruction through the longitudinal axis of the sacrum shows fractures at the left and right sacral ala (arrows). c Post-operative A–P pelvic overview. The fractures were stabilized with a trans-sacral bar and additional iliosacral screw on the right. A retrograde transpubic screw has been inserted for the right anterior instability. The arrows show how the washers and nuts on each side of the transsacral bar press on the lateral cortex of the posterior ilium. All implants have been inserted through small incisions, the length of all incisions together was 10 centimetres
a A seventy-year-old male suffered a fall with his bike. A–P pelvic overview reveals an anterior wall fracture of the left acetabulum. b Axial CT-transection through the weight-bearing dome reveals a displaced anterior wall and incomplete anterior column fracture. c A–P pelvic overview 6 months after operative treatment. Reduction and fixation with an infrapectineal plate were done through the modified Stoppa approach, d ala view, e obturator view. The patient has been allowed to walk with full weight-bearing immediately post-operative
Conclusion
Geriatric patients need different principles of fracture care because they exhibit specific characteristics. The geriatric fracture patient is not comparable with the healthy, younger adult. Elderly patients regularly have comorbidities, which restrict their physiological reserves and influence outcome after trauma. Functional demands are different. Bone quality is diminished and soft tissue envelope compromised. Therefore, the goals of geriatric fracture treatment must be adapted. Regaining independence in activities of daily life is the most important goal. This is achieved by creating high stability in the fracture plane. Anatomical reduction, restoration of optimal function and preservation of blood supply are less important. Techniques of osteosynthesis and approaches have to be as less invasive as possible. Intramedullary nails, implants using long anatomical corridors and intra-osseous implants, using small incisions for insertion, are safe and prevent wound healing problems. An individual analysis of the specific benefits and drawbacks of conventional techniques and their alternatives is needed. More than in younger trauma patients, a comprehensive care including treatment of comorbidities and specific support for regaining mobility and independency are indispensable. This can best be guaranteed with geriatric co-management.
References
Nikkel LE, Fox EJ, Black KP, Davis C, Andersen L, Hollenbeak CS. Impact of comorbidities on hospitalization costs following hip fracture. J Bone Joint Surg Am. 2012;94(1):9–17.
McMahon DJ, Shapiro MB, Kauder DR. The injured elderly in the trauma intensive care unit. Surg Clin North Am. 2000;80:1005–19.
Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA. Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos. 2013;8:136.
Watts NB. The Fracture Risk Assessment Tool (FRAX®): applications in clinical practice. J Womens Health (Larchmt). 2011;20(4):525–31.
Dachverband Osteologie eV, Prophylaxe. Diagnostik und Therapie der Osteoporose bei postmenopausalen Frauen und bei Männern. Version 2017. Langfassung. AWMF-Register-Nr. 183/001, 216 pages.
Cheng SY, Levy AR, Lefaivre KA, Guy P, Kuramoto L, Sobolev B. Geographic trends in incidence of hip fractures: a comprehensive literature review. Osteoporos Int. 2011;22(10):2575–86.
Rommens PM, Hofmann A. Comprehensive classification of fragility fractures of the pelvic ring: Recommendations for surgical treatment. Injury. 2013;44(12):1733–44.
Andrich S, Haastert B, Neuhaus E, Neidert K, Arend W, Ohmann C, Grebe J, Vogt A, Jungbluth P, Thelen S, Windolf J, Icks A. Excess mortality after pelvic fractures among older people. J Bone Miner Res. 2017;32(9):1789–801.
Heim UFA. Das Phänomen AO. Gründung und erste Jahre der Arbeitsgemeinschaft für das Studium der Osteosynthese. German: Verlag Hans Huber Bern-Göttingen-Toronto-Seattle; 2001. p. 246.
Bukata SV, Digiovanni BF, Friedmann SM, et al. A guide to improving the care of patients with fragility fractures. Geriatr Orthop Surg Rehabil. 2011;2(1):5–37.
Böhler L. Die Technik der Knochenbruchbehandlung. 12. und 13. vollständig neubearbeitete Auflage. Verlag für medizinische Wissenschaften. Band 1. Wien-Düsseldorf: Wilhelm Maudrich; 1953.
Lambotte A. L’Intervention opératoire dans les fractures récentes et anciennes envisage particulièremnt au point de vue de l’ostéosynthese avec la description de plusieurs techniques nouvelles. Brussels: Henri Lamertin, Libraire-Éditeur; 1907.
Danis R. Théorie et pratique de l’ostéosynthese. Masson et cie. Paris, 1949, 296 pages. French.
Küntscher G. Praxis der Marknagelung. Handschriftlich nach 1. Auflage 1962 überarbeitete bisher unveröffentlichte 2. Ausgabe von 1972. Reprint bei Karger 1986. 349 pages. German.
Müller ME, Allgöwer M, Willenegger H. Manual of internal fixation. Technique recommended by the AO-group. Berlin Heidelberg New York: Springer Verlag; 1969. 298 pages.
SooHoo NF, Krenek L, Eagan MJ, Gurbani B, Ko CY, Zingmond DS. Complication rates following open reduction and internal fixation of ankle fractures. J Bone Joint Surg Am. 2009;91(5):1042–9.
Koso RE, Terhoeve C, Steen RG, Zura R. Healing, nonunion, and re-operation after internal fixation of diaphyseal and distal femoral fractures: a systematic review and meta-analysis. Int Orthop. 2018. https://doi.org/10.1007/s00264-018-3864-4.
Steinau HU, Hebebrand D, Vogt P, Josten C. [Plastic soft tissue coverage in defect fractures of the tibia]. Chirurg. 1996;67(11):1080–6. (German).
Gaunder CL, Zhao Z, Henderson C, McKinney BR, Stahel PF, Zelle BA. Wound complications after open reduction and internal fixation of tibial plateau fractures in the elderly: a multicentre study. Int Orthop. 2018. https://doi.org/10.1007/s00264-018-3940-9.
Mast J, Jakob R, Ganz R. Planning and reduction technique in fracture surgery. Berlin: Springer; 1989. p. 272.
Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, Tscherne H. Minimally invasive plate osteosynthesis: does percutaneous plating disrupt femoral blood supply less than the traditional technique? J Orthop Trauma. 1999;13(6):401–6.
Perren SM, Cordey J, Rahn BA, Gautier E, Schneider E. Early temporary porosis of bone induced by internal fixation implants. A reaction to necrosis, not to stress protection? Clin Orthop Relat Res. 1988;(232):139–51.
Wagner M, Frigg R. AO manual of fracture management. Internal fixators. Concepts and cases using LCP/LISS. Stuttgart, Germany: Thieme; 2006. p. 888.
Babst R, Bavonratanavech S, Pesantes R. Minimally invasive plate osteosynthesis (MIPO), 2nd edition. Stuttgart, Germany: Thieme; 2012. p. 784.
Tornetta P, Mostafavi H, Riina J, Turen C, Reimer B, Levine R, Behrens F, Geller J, Ritter C, Homel P. Morbidity and mortality in elderly trauma patients. J Trauma. 1999;46(4):702–6.
Grossmann MD, Miller D, Scaff DW, Arcona S. When is an elder old? Effect of preexisting conditions on mortality in geriatric trauma. J Trauma. 2002;52(2):242–6.
Pernod G, Albaladejo P, Godier A, Samama CM, Susen S, Gruel Y, Blais N, Fontana P, Cohen A, Llau JV, Rosencher N, Schved JF, de Maistre E, Samama MM, Mismetti P, Sié P. [Management of major bleeding complications and emergency surgery in patients on long-term treatment with direct oral anticoagulants, thrombin or factor-Xa inhibitors. Proposals of the Working Group on Perioperative Haemostasis (GIHP) - March 2013]. Ann Fr Anesth Reanim. 2013;32.(10):691–700
Ramly E, Kaafarani HM, Velmahos GC. The effect of aging on pulmonary function: implications for monitoring and support of the surgical and trauma patient. Surg Clin North Am. 2015;95(1):53–69.
Loftus TJ, Brakenridge SC, Murphy TW, Nguyen LL, Moore FA, Efron PA, Mohr AM. Anemia and blood transfusion in elderly trauma patients. J Surg Res. 2018;229:288–93.
Thaeter M, Knobe M, Vande Kerckhove M, Böhle F, Herold J, Verhaven E, Pape HC. Perioperative inflammatory response in major fracture: do geriatric patients behave differently? Eur J Trauma Emerg Surg. 2016;42(5):547–51.
Tsuei BJ, Kearney PA. Hypothermia in the trauma patient. Injury. 2004;35(1):7–15.
Hoppe S, Uhlmann M, Schwyn R, Suhm N, Benneker LM. Intraoperative mechanical measurement of bone quality with the DensiProbe. J Clin Densitom. 2015;18(1):109–16.
Hepp P, Lill H, Bail H, Korner J, Niederhagen M, Haas NP, Josten C, Duda GN. Where should implants be anchored in the humeral head? Clin Orthop Relat Res. 2003;(415):139–47.
Kamer L, Noser H, Blauth M, Lenz M, Windolf M, Popp AW. Bone mass distribution of the distal tibia in normal, osteopenic, and osteoporotic conditions: an ex vivo assessment using HR-pQCT, DXA, and computational modelling. Calcif Tissue Int. 2016;99(6):588–97.
Wagner D, Kamer L, Sawaguchi T, Richards GR, Noser H, Rommens PM. Sacral bone mass distribution of the sacrum assessed by averaged 3D CT statistical models—implications for pathogenesis and treatment of fragility fractures of the sacrum. J Bone Joint Surg Am. 2016;98:584–90.
Lanzetti RM, Lupariello D, Venditto T, Guzzini M, Ponzo A, De Carli A, Ferretti A. The role of diabetes mellitus and BMI in the surgical treatment of ankle fractures. Diabetes Metab Res Rev 2018;34(2). https://doi.org/10.1002/dmrr.2954.
Krettek C, Wiebking U. [Proximal humerus fracture: is fixed-angle plate osteosynthesis superior to conservative treatment?]. Unfallchirurg. 2011;114(12):1059–67. (German).
Chen Y, Chen X, Li Z, Yan H, Zhou F, Gao W. Safety and efficacy of operative versus nonsurgical management of distal radius fractures in elderly patients: a systematic review and meta-analysis. J Hand Surg Am. 2016;41(3):404–13.
Gruszka D, Dietz SO, Brodt R, Wagner D, Kuhn S, Rommens PM, Kuechle R. Results of the treatment of intracapsular femoral neck fractures with a new dynamic locking plate. Acta orthop belg. 2017;83(4):536–43.
Zhou Z, Zhang X, Tian S, Wu Y. Minimally invasive versus conventional dynamic hip screw for the treatment of intertrochanteric fractures in older patients. Orthopedics 2012;35(2):e244-9.
Savage JW, Schroeder GD, Anderson PA. Vertebroplasty and kyphoplasty for the treatment of osteoporotic vertebral compression fractures. J Am Acad Orthop Surg. 2014;22(10):653–64.
Frey ME, Warner C, Thomas SM, Johar K, Singh H, Mohammad MS, Beall DP. Sacroplasty: a ten-year analysis of prospective patients treated with percutaneous sacroplasty: literature review and technical considerations. Pain Physician. 2017;20(7):E1063–72.
Cornell CN. Internal fracture fixation in patients with osteoporosis. J Am Acad Orthop Surg. 2003;11(2):109–19.
Rommens PM, Pairon P, Kuhn S. [Nailing of metaphyseal fractures]. Unfallchirurg. 2013;116(9):831–46. German.
White TO, Bugler KE, Appleton P, Will E, McQueen MM, Court-Brown CM. A prospective randomised controlled trial of the fibular nail versus standard open reduction and internal fixation for fixation of ankle fractures in elderly patients. Bone Joint J. 2016;98-B(9):1248–52.
Smeets B, Hoekstra H. Fibular nailing seems an effective strategy to decrease treatment crude costs for AO-Type 44B ankle fractures in elderly patients. J Foot Ankle Surg. 2016 ;55(3):684–5.
Kuhn S, Appelmann P, Pairon P, Mehler D, Hartmann F, Rommens P. A new angle stable nailing concept for the treatment of distal tibia fractures. Int Orthop. 2014;38:1255–60.
Zwipp H, Paša L, Žilka L, Amlang M, Rammelt S, Pompach M. Introduction of a New Locking Nail for Treatment of Intraarticular Calcaneal Fractures. J Orthop Trauma. 2016;30(3):e88–92.
Halvorson TL, Kelley LA, Thomas KA, Whitecloud TS, Cook SD. Effects of bone mineral density on pedicle screw fixation. Spine (Phila Pa 1976). 1994;19(21):2415–20.
Weiser L, Dreimann M, Huber G, Sellenschloh K, Püschel K, Morlock MM, Rueger JM, Lehmann W. Cement augmentation versus extended dorsal instrumentation in the treatment of osteoporotic vertebral fractures: a biomechanical comparison. Bone Joint J 2016;98-B(8):1099–105.
Hoppe S, Keel MJ. Pedicle screw augmentation in osteoporotic spine: indications, limitations and technical aspects. Eur J Trauma Emerg Surg 2017;43(1):3–8.
El Saman A, Meier S, Sander A, Kelm A, Marzi I, Laurer H. Reduced loosening rate and loss of correction following posterior stabilization with or without PMMA augmentation of pedicle screws in vertebral fractures in the elderly. Eur J Trauma Emerg Surg 2013;39(5):455–60.
Rommens PM, Wagner D, Hofmann A. Fragility Fractures of the Pelvis. JBJS Rev 2017;5:3.
Mehling I, Hessmann MH, Rommens PM. Stabilisation of fatigue fractures of the dorsal pelvis with a trans-sacral bar. Operative technique and outcome. Injury. 2012;43:446–51.
Rommens PM. Is there a role for percutaneous pelvic and acetabular reconstruction? Injury 2007;38(4):463–477.
Rommens PM, Wagner D, Hofmann A. Minimal invasive surgical treatment of fragility fractures of the Pelvis. Chirurgia (Bucur). 2017;112(5):524–537
Vanderschot P. Treatment options of pelvic and acetabular fractures in patients with osteoporotic bone. Injury 2007;38(4):497–508.
Jeffcoat DM, Carroll EA, Huber FG, Goldman AT, Miller AN, Lorich DG, Helfet DL. Operative treatment of acetabular fractures in an older population through a limited ilioinguinal approach. J Orthop Trauma. 2012;26(5):284–9.
Bastian JD, Tannast M, Siebenrock KA, Keel MJ. Mid-term results in relation to age and analysis of predictive factors after fixation of acetabular fractures using the modified Stoppa approach. Injury 2013;44(12):1793–8.
Funding
There was no funding for this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
He has is no conflict of interest.
Ethical approval
Ethical approval is not applicable for this manuscript.
Informed consent
Informed consent is not applicable for this manuscript.
Additional information
Otmar Trentz lecture at the 20th European Congress for Trauma and Emergency Surgery, Prague, May 5th 2019.
Rights and permissions
About this article
Cite this article
Rommens, P.M. Paradigm shift in geriatric fracture treatment. Eur J Trauma Emerg Surg 45, 181–189 (2019). https://doi.org/10.1007/s00068-019-01080-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-019-01080-x