Abstract
Purpose
Stabilizing techniques of flail chest injuries usually need wide approaches to the chest wall. Three main regions need to be considered when stabilizing the rib cage: median-anterior with dissection of pectoral muscle; lateral—axillary with dissection of musculi (mm) serratus, externus abdominis; posterior inter spinoscapular with division of mm rhomboidei, trapezius and latissimus dorsi. Severe morbidity due to these invasive approaches needs to be considered. This study discusses possibilities for minimized approaches to the shown regions.
Method
Fifteen patients were stabilized by locked plate osteosynthesis (MatrixRib®) between May 2012 and April 2014 and prospectively followed up. Flail chest injuries were managed through limited incisions to the anterior, the lateral, and the posterior parts of the chest wall or their combinations. Each approach was 4–10 cm using Alexis® retractor.
Results
One minimized approach offered sufficient access at least to four ribs posterior and laterally, four pairs of ribs anterior in all cases. There was no need to divide latissimus dorsi muscle. Trapezius und rhomboid muscles were only limited divided, whereas a subcutaneous dissection of serratus and abdominis muscles was necessary. A follow-up showed sufficient consolidation. Complications: pneumothorax (2) and seroma (2).
Conclusion
Minimized approaches allow sufficient stabilization of severe dislocated rib fractures without extensive dissection or division of the important muscles. Keeping the arm and, thus, the scapula mobile is very important for providing the largest reachable surface of the rib cage through each approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fractures of sternum and ribs can cause severe interference of respiratory movements, and thoracic organs are at risk of concomitant injuries.
Flail chest injury is defined by the presence of three or more adjacent rib fractures. This type of injury causes an unstable chest wall segment and leads to atypical respiratory movements. Bilateral flail chest is a life-threatening injury with an immediate risk of respiratory failure [1].
Moreover, even single rib fractures as well as serial fractures of ribs may cause a severe loss of quality of life due to pain and a possible deformity of the chest wall [2, 3]. Most fractures of the sternum and the ribs are treated conservatively.
However, some patterns of injuries may not heal completely under conservative treatment and, thus, should be considered to be treated surgically.
The advantages of a surgical rib fixation had been already recognized in severe flail chest injuries and in some types of single rib fractures [4–8]. Possible indications had already been discussed by Nirula et al. [19] (Table 1).
In the past, stabilizing techniques of flail chest injuries have been described with wide surgical approaches to the chest wall [1, 3]. This leads to severe dissection of the soft tissue surrounding the chest wall and, thereby, the possibility of a loss of function due to the partition of muscles additionally to the injuries related to the trauma. Nerves and vessels could be at risk at the same time. For this reason, the procedure might neither be appreciated by the patient nor by the surgeon.
Stabilization of ribs and sternum aims to preserve the anatomic and physiologic function of the chest wall.
Anatomical principles
The chest wall is surrounded by soft tissue, containing the skin, the subcutaneous fat, and a number of muscles. Three main regions need to be considered when establishing surgical approaches to the rib cage: anterior, lateral, and posterior.
Anteriorly, the major pectoral muscle covers the chest wall from next to the sternum to the anterior axillary line, and ensures internal rotation of the humeral head. Underneath this muscle, the minor pectoral muscle arises from the ribs III to V in the anterolateral region with its main function to hold the scapula close to the chest wall. The axillary region is bordered by the latissimus dorsi muscle posteriorly, while the chest wall is covered by the serratus anterior muscle, which guides the scapular’s tip and is connected to the oblique abdominis muscle. Finally, the trapezius and rhomboid muscles are connecting the scapula to the spine, while covering the posterior chest wall next to the latissimus dorsi muscle [9–11]. The scapula covers the second to the eighth rib.
This study describes minimal invasive surgical approaches in the treatment of flail chest injuries. It emphasizes on muscle sparing incisions and the accessability of several chest areas through minimal incisions, while the scapula is kept mobile opposite to other studies [3, 11].
Materials and methods
Between May 2012 and April 2014, 15 patients with severe rib fractures and flail chest injuries were stabilized by limited and muscle-sparing approaches to the chest wall (Table 2). The patients were prospectively followed up. Those with wide open approaches (n = 5) were excluded from this study as well as those with isolated sternal fractures and those who were treated conservatively. The indication was set by a senior surgeon of the department, following the indications shown in Table 1 and approved by the head of the department.
Each patient who was admitted to our department and who was suffering from a severe chest injury received a helical CT-scan in a multisliced technique (Siemens Somatom definition AS, 128 slices, Munich, Germany). Images were assessed in three planes: the axial, the sagittal, and the coronal one as well as in a multiplaned reconstruction in the volume rendering (VRT) mode.
Preoperatively, the procedure was planned by merging a proper clinical examination of the patient and the CT scan of the chest while looking for painful and unstable ribs with the determination of the exact location of the fractures. The most dislocated ribs were defined as the center of instability as well as the region, which shows the most paradoxical movements, respectively.
The procedure was carried out under general anaesthesia, providing the possibility of single-lung ventilation. The time of the procedure was chosen as soon as possible after the trauma in patients under stable conditions, whereas a stabilization of the chest wall was carried out after the recovering from life threat in the patients who were suffering from a polytrauma.
Positioning
For approaches to the anterior chest wall and combination of approaches to the anterior and lateral regions, the patient was lying in a supine position. If posterior and lateral approaches were likely to be used, the patient was put into a lateral decubitus position, while keeping his ipsilateral arm mobile on a TRIMANO 3D Support Arm® (MAQUET Holding B.V. & Co. KG, Rastatt, Germany) (Fig. 1).
Positioning and preparation of the approaches. Lateral decubitus position: a the arm is kept mobile using a TRIMANO 3D Support Arm®, b anterior position of the arm allows access to the posterior chest wall in between the scapula and the spine, and c posterior position of the arm allows access to the axilla and, thus, to the lateral chest wall. d A line is drawn in between the scapula and the spine and then continued in the direction of a typical posterior thoracotomy. The incision will be made following this line but limited to the core of instability of the chest wall. e Supine position the median access to the sternum and the anterior ribs was yet established. A line is drawn in parallel to the lower rim of the major pectoral muscle and in top of the core of instability of the (antero-) lateral chest wall where the approach is going to be made
In case of fractures facing two or even multiple regions, the minimized approaches were established, and subsequently, a submuscular tunnel in between the approaches was established on the surface of the ribs (Fig. 1).
In case of a concomitant lung injury, a limited thoracotomy was carried out through the established approach to explore the lung, rinse the pleural cavity, and insert pleural catheters if indicated, and lung lacerations were primarily sutured or an atypical lung resection was carried out employing classical surgical techniques with resection and suturing or with the use of a stapler (Proximate® 75 mm Linear Cutter, Ethicon, Norderstedt, Germany) (Fig. 2b).
Surgical procedure. a Dissect the covering muscles while keeping them complete, retract the latissimus dorsi muscle, pinpoint the fractures and b explore the pleural cavity if necessary. Repair of lung laceration (c) positioning of the plates (d) reduct the fractures and fix the plates. Plates are tunneled underneath the scapular and fixed through the limited approaches (pat. 9). e Three plates were fixed through on approach (pat. 6). f The dissected muscles are reinserted to their anatomic origin to cover the implants completely
Approaches
The access to the anterior chest wall was performed through a median incision over the sternum with the sternal fracture in the center of the approach or the level of rib intended to treat, respectively [12]. Subsequently, each layer of soft tissue was divided into the midline until reaching the anterior (bony) cortex of the sternum. The pectoral muscle was dissected from the chest wall, respecting anatomical layers and leaving the muscle in toto. Once the need for a treatment of the lower ribs, adjacent to the sternum, was recognized, parts of the rectus abdominis muscles were detached from the chest wall as well as the oblique abdominis muscle.
Identification of anatomical landmarks is crucial for the approach of the axillary region. Those were the lower rim of the major pectoral muscle, the anterior rim of the latissimus dorsi muscle, and the level of ribs intended to treat. After this, a horizontal incision was carried out, following the rib that is supposed to be the one in the center of the fractured area. After preparation through skin and subcutaneous tissue, the anterior edge of the serratus anterior muscle needs to be identified. The major pectoral muscle was moved cranially for this procedure. Then, subsequently, the serratus muscle was detached from the chest wall, again preserving its continuity and, furthermore, respecting anatomical layers. Following this procedure, the long thoracic nerve and its adjacent vessels are preserved in an easy and secure way.
The posterior region of the chest wall was reached through an incision in between the Margo medialis of the scapula and the processus spinosus of the thoracic spine, having the rib in the center of the injured region again. Once the skin and the subcutaneous tissue have been dissected, the trapezius and rhomboid muscles are detached from the spinal processes. This means to dissect the tissue subcutaneously until the muscle’s root can be identified to keep the muscle completely when detaching it.
For each approach, the Alexis wound (Applied Medical, Rancho Santa Margarita, USA) retractor was inserted, thus providing the best overview while protecting the rim of the wound from drying out (Fig. 2).
Fixation of the ribs
Once the approach to the chest wall was made, the fractures of ribs and sternum were pinpointed. Each fracture was reduced to an anatomic alignment of the sternum and the ribs, respectively. Following this important step, a stable osteosynthesis was carried out, employing locked titanium plates in a low-profile design (MatrixRib®, 1.5 mm thickness, 2.9-mm screws; DePuySynthes CMF, Switzerland). Each main fragment was fixed with at least three locked screws, following the instructions of the manufacturer (Fig. 2). Alternatively, an intramedullary splint was employed to stabilize single fractures. Each of the splints was secured with one locked screw of appropriate length (MatrixRib® splints 3, 4, or 5 mm, 2.9-mm screws, DePuySynthes CMF, Switzerland).
Intraoperative fluoroscopy was not employed, since each rib has been directly visible through the approaches.
All ribs showing a dislocated fracture were stabilized. Afterward, the adjacent ribs were checked for their alignment and stability. They were stabilized if it was considered to be necessary.
Fixation was started up in the most posterior part of the injured chest wall. Keeping the arm as much as possible anteriorly provided a very good overview to the posterior parts of the ribs and allowed to fix the plates in this region. Afterward, the arm was moved posteriorly and, thus, allowed proper access to the axillary region of the ribs. Following this procedure, most parts of the ribs became reachable even if there are supposed to be covered by the scapula (Fig. 1b, c).
After finishing the fixation, the approaches were closed, respecting the anatomic layers again. Each muscle was reattached to the ribs or the vertebral spine with strong sutures (Vicryl 1, USB, Ethicon, Summerville, USA) followed by the closure of the skin. If necessary, drainage was inserted for at least 2 days.
Follow-up
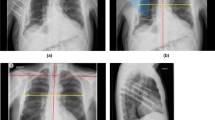
Each patient was followed up immediately after operation as well as after 1, 2, 6, and 12 weeks. At each time, a clinical examination was carried out with the focus of wound healing and soft tissue, stability of the chest wall, respiratory movements, pain, and other concerns the patients complains of. Chest X-rays were taken immediately after the operation, after 1 week (before discharge of the hospital), and after 6 and 12 weeks. They were observed for proper inflation of the lung, pleural effusion, and the alignment of the bony chest wall as well as the position of the implants.
Results
There were 9 male and 6 female out of the 15 patients with a median age of 59, 9 years (min: 25, max: 90, SD = 17.8). Table 2 shows the patients, including the details of their patterns of injuries and the treatment that has been performed.
The indication for the stabilization is individually shown in Table 2. Each of them was following Table 1.
Flail chest injuries could be identified anterior in 11 patients, lateral in 11 patients, and dorsal in 6 patients. Out of them, six suffered from bilateral flail chest injuries, thereunder two involving the anterior chest wall as well as both lateral regions and two showing multiple rib fractures in posterior region bilaterally. Thereby, seven patients suffered from a fracture of the sternum, four located at the manubrium, and five located at the corpus sterni. Thereunder, two multiple fractures were involved in both regions.
The minimized approaches to the chest wall were performed to each of the regions, which were suffering from instable rib fractures as shown above.
Sternal fractures were managed through the anterior approach. The length of the approaches was 6 and 7 cm (min 3 cm, max 10 cm, SD = 2.1). One minimized approach offers sufficient access to at least four ribs posterior and, laterally, four pairs of ribs anterior in all cases. There was no need to divide the latissimus dorsi muscle. Trapezius and rhomboid muscles were only limitedly divided, and a subcutaneous dissection of serratus and abdominis muscles was necessary.
Follow-up
Sufficient consolidation was seen in all cases and no loss of reduction in any case. No plates lost their positions. Drainages could be removed in between the 2nd and the 7th day after the procedure. No recrudescence of pleural effusion could be seen during the follow-ups.
The wounds healed uneventful in all cases (Fig. 3).
Postoperative results. a–d Bilateral anterior flail (pat. 4). The sternum and four ribs were fixed through an anterior approach (a, b), two ribs on each side were fixed through a limited axillary approach. The red circle shows the length of one lateral approach, and the green circle the reachable area (c, d). e–h Bilateral posterolateral flail chest (pat. 9). The chest wall was fixed to a normal shape. Pneumothorax and emphysema have been completely gone 2 weeks after the operation (e, f). At the same time, the patient could move her arms without any limitations. The scars are short and uneventful in both cases
There were no injuries of nerves seen, neither intercostally nor at the periscapular muscles.
All patients began to move their shoulders immediately after the procedure while keeping the arm in the lower part of the range of motion. After the 6th week, the mobilization gained up to a normal level in all patients. No complications were seen involving the mobility of the shoulder after the procedure, even not in the patients who were suffering from a fracture of the clavicle (Fig. 3).
Complications
The only complications we saw were a pneumothorax in two cases, a seroma of the soft tissue in two cases, and a dislocation of a rib splint in one case (pat 4).
Pneumothorax was detected in the X-ray, which has been taken immediately postoperative. Both patients (pat. 2 and 3) did not receive a chest tube during the procedure, but they were treated by a chest tube, since the X-ray showed a pneumothorax. The subsequent follow-ups were uneventful. Both patients were suffering from a long-term and severe lung disease (COLD) for a long time before their accident.
The patient’s no. 4 and 5 showed a seroma in the soft tissue during the first 10 days after the stabilization. The first one was suffering from a crush trauma to the posterolateral chest wall und received anticoagulant medication. The second one had a steering wheel injury and developed a seroma peristernally. Both were successfully treated by the percutaneous application of a Redon drainage.
The dislocated rib splint was removed during the second operation. The follow-up showed a little dislocation of the rib but uneventful healing during the following months.
Discussion
Limited approaches
The approaches to the ribs were carried out, following the principles of common approaches to the chest wall. As the soft tissue was assumed to show a wide-stretched mobility over the chest wall, especially in the lateral and posterior parts, the incisions into the skin, the subcutaneous tissue, and the muscles were kept short. Once the incision was made, Alexis retractor (Applied Medical, Rancho Santa Margarita, USA) had been inserted to establish a window-like approach, which could be moved atop the chest wall. Through this approach, a detachment of the muscles could be carried out as well as a limited division of those muscles, which were not necessarily mobilized in toto, such as the trapezius and the rhomboid muscles. In contrast to the suggestions of other authors, we did not perform a division of the muscles in between the spine and the scapula [11]. This approach preserves the continuity of muscles and the adjacent neurovascular bundles. However, the muscles that cover the anterior and the lateral chest wall needed to be detached from the chest wall, following the suggestions of Bottlang et al. [1] to access the fractured ribs. Again, this was performed through the limited incisions in a safe procedure while preserving the continuity of the muscles, such as the major pectoral muscle and the serratus anterior muscle.
Operation’s convenience
The literature is silent about operation time in flail chest injuries at all. Our purpose was to give an overview for the experience in the treatment of different types of flail chest injuries with and without concomitant injuries to the thoracic organs. Table 2 shows rather short times for the isolated fixation of the ribs and the sternum, whereas the treatment of concomitant injuries results in significant longer operation times.
The described technique is not suggested to cause longer operation times, since all ribs become fully visible during the procedure shown.
Furthermore, a high safety is given in the realignment of multifractured ribs, following the shown technique. Once access to all parts of the ribs that need to be fixed could be gained up directly through the limited approaches, a fluoroscopy has not been necessary in any out of the cases.
Patient’s convenience
The scars caused by the discussed procedure are comparatively short and showed a high patients’ convenience. The soft tissue surrounding the scars showed a smooth consistence, while the scars showed nearly normal mobility during any movements of the trunk and the chest wall itself. It should be highlighted that none of the patients were complaining about numbness around the scars or even any severe complication, such as paresthesia or loss of function of any nerve. In contrast, the discussed complications are relatively common alongside large approaches, such as a posterolateral thoracotomy [13, 14]. Performing rib stabilization through limited approaches suggests the reduction of complications related to the surgical approach while following the protocol discussed in the shown cohort.
Positioning
A prone position was not employed in any case
Injuries at the anterior chest wall could be managed best in a supine position, which is very well known from the cardiac surgery and has been furthermore described to be favorable in the management of sternal fractures [11, 15].
Injuries of the lateral chest wall could be managed best from a limited anterolateral approach similar to the one which is very common in anterolateral thoracotomies. The patient lies in a lateral decubitus position, while the arm is fixed in abducted position over the head [16]. Fractures involving the ribs in between the median clavicle line and the posterior axillary line are perfectly accessible through this approach.
In contrast, the management of flail chest injuries involving the lateral and posterior parts of the chest wall is very challenging. As the arms are fixed to the chest wall by the scapula and its muscles, main parts of the chest wall are covered by these important anatomic structures. Traditional approaches toward the ribs underneath the scapula are described as very invasive, including the dissection of all muscles and the elevation of the scapula with a retractor system [3]. Our innovative procedure with a mobile arm allowed best access to the ribs III to VIII while saving as many muscles as possible. In all cases, the plates were fixed to the posterior part of the ribs at first, while the arm was positioned in front of the anterior axillary line. Afterward, the arm was moved behind the posterior axillary line, thus allowing the fixation of the plates to the anterior–lateral part of the ribs through the axillary approach.
The TRIMANO 3D Support Arm® (MAQUET Holding B.V. & Co. KG, Rastatt, Germany) offered a great choice of dynamic positioning of the arm while keeping the whole arm sterile (Fig. 2a).
Complications
There were only minor complications seen during the follow-up.
The two patients who developed a pneumothorax were both suffering from a chronic lung disease, which is often accompanied with emphysema and adhesions to the chest wall [17]. Hence, the reduction of the fractures and the fixation of the plates could cause a little lung laceration that subsequently leads to pneumothorax. For the risk of a dangerous tension pneumothorax, a chest tube is recommended during the procedure, especially in patients who are suspicious to suffer from a lung disease.
Seroma in the soft tissue was associated with a high risk profile for complications in both cases due to a severe hematoma after the trauma, anticoagulant medication, and obesity. The seroma was evacuated sufficiently in both cases, and the wounds healed uneventfully from this time.
Possible reasons for the dislocation of the splint could be suboptimal application or the impossibility for an insertion in a flat angle as the instructions suggest due to obesity with an 80 mm thickness of the soft tissue. Since no pain or other problems were caused through the dislocated splint, a wait and see procedure would have been possible. At the time, the same patient needed to go to the operation room again for the treatment of his seroma, and he agreed to the removal of the splint under general anesthesia. Hence, the rib showed only a little dislocation and uneventful healing further on. This implicates that the stabilization of the core of instability on the one hand prevents from a dislocation of the adjacent ribs that subsequently could cause a deformity, and on the other hand, it paves the way for uneventful healing.
Of course, the plating of all ribs that are showing fractures might restore the anatomy best. But in this context, the need for larger approaches should be considered.
Conclusions
In conclusion of the shown techniques, further research will be needed to describe the possibilities of limited approaches and their limitations. Hence, a possible focus of future investigations should aim to gain up quantitative data, referring to the length of approaches, their positions, and the effect of the positioning of the arms in a lateral decubitus position.
New instruments, such as 90° drill guides and screw drivers (DePuySynthes CMF, Switzerland) undertake the possibility of further minimization of the approaches as well as trocars, allowing the placement of screws percutaneous with the meaning of a minimized plate osteosynthesis (MIPO) [18].
Minimized approaches allow sufficient stabilization of severe dislocated rib fractures without extensive dissection or division of the important (thoracic) muscles.
The scars are comparatively short that might be beneficial for the patient’s convenience.
Keeping the arm and, thus, the scapula mobile is very important for providing the largest reachable surface of the rib cage through each approach.
The splinting technique should only be employed in ribs, which are accessible through a flat angle to secure the proper sequence of the procedure following the technical guide.
The insertion of a chest tube is recommended during the surgical procedure/operation, especially in patients which are suspicious for the prevalence of a chronic lung disease.
The healing of the wounds and the soft tissue needs to be followed up consequently. A possible complication is the occurence of seroma, which usually related to a high impact trauma as well as in patients taking any anticoagulant medication.
References
Bottlang M, Long WB, Phelan D, Fielder D, Madey SM. Surgical stabilization of flail chest injuries with MatrixRIB implants: a prospective observational study. Injury. 2013;44(2):232–8.
Marasco S, Lee G, Summerhayes R, Fitzgerald M, Bailey M. Quality of life after major trauma with multiple rib fractures. Injury. 2015;46(1):61–5.
Gasparri MG, Tisol WB, Haasler GB. Rib stabilization: lessons learned. Eur J Trauma Emerg Surg. 2010;36:435–40.
Leinicke JA, Elmore L, Freeman BD, Colditz GA. Operative management of rib fractures in the setting of flail chest: a systematic review and meta-analysis. Ann Surg. 2013;258(6):914–21.
Marasco SF, Davies AR, Cooper J, Varma D, Bennett V, Nevill R, Lee G, Bailey M, Fitzgerald M. Prospective randomized controlled trial of operative rib fixation in traumatic flail chest. J Am Coll Surg. 2013;216(5):924–32.
NICE. Insertion of metal rib reinforcements to stabilise a flail chest wall. Issued: October 2010 NICE interventional procedure guidance 361. http://www.nice.org.uk/ipg361.
Khandelwal G, Mathur RK, Shukla S, Maheshwari A. Marasco SF, Davies AR, Cooper J, Varma D, Bennett V, Nevill R, Lee G, Bailey M, Fitzgerald M. Prospective randomized controlled trial of operative rib fixation in traumatic flail chest. Int J Surg. 2013;9(6):478–81.
Lafferty PM, Anavian J, Will RE, Cole PA. Operative treatment of chest wall injuries: indications, technique, and outcomes. J Bone Jt Surg Am. 2011;93(1):97–110.
Gray H. Anatomy oft the human body. 20th ed. Philadelphia and New York: Lea and Febiger; 1918.
Clemens MW, Evans KK, Mardini S, Arnold PG. Introduction to chest wall reconstruction: anatomy and physiology of the chest and indications for chest wall reconstruction. Semin Plast Surg. 2011;25(1):5–15.
Marasco S, Saxena P. Surgical rib fixation—technical aspects. Injury. 2015;46(5):929–32.
Schulz-Drost S, Oppel P, Grupp S, Schmitt S, Carbon RT, Mauerer A, Hennig FF, Buder T. Surgical fixation of sternal fractures: preoperative planning and a safe surgical technique using locked titanium plates and depth limited drilling. J Vis Exp. 2015;. doi:10.3791/52124.
Romero A, Garcia JE, Joshi GP. The state of the art in preventing postthoracotomy pain. Semin Thorac Cardiovasc Surg. 2013;25(2):116–24.
Li S, Feng Z, Wu L, Huang Q, Pan S, Tang X, Ma B. Analysis of 11 trials comparing muscle-sparing with posterolateral thoracotomy. Thorac Cardiovasc Surg. 2014;62(4):344–52.
Schulz-Drost S, Mauerer A, Grupp S, Hennig FF, Blanke M. Surgical fixation of sternal fractures: locked plate fixation by low-profile titanium plates—surgical safety through depth limited drilling. Int Orthop. 2014;38(1):133–9.
Zardo P, Fischer S. Standardtechniken in der Thoraxchirurgie. In: Hachenberg U.A., Anästhesie und Intensivtherapie in der Thoraxchirurgie. p109–111. (ISBN 9783131487711). G. Thieme, Stuttgart, Germany. 2010.
Bintcliffe O, Maskell N. Spontaneous pneumothorax. BMJ. 2014;8:348.
Nickerson TP, Kim BD, Zielinski MD, Jenkins D, Schiller HJ. Use of a 90 drill and screwdriver for rib fracture stabilization. World J Surg. 2015;39(3):789–93.
Nirula R, Diaz JJ Jr, Trunkey DD, Mayberry JC. Rib fracture repair: indications, technical issues, and future directions. World J Surg. 2009;33(1):14–22.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SSD is a member of the thoracic expert group of the AO, and he has a consultant agreement with DePuySynthesCMF. SG, MP, PO, SK, AM, FH, and AL declare that they have no conflict of interest.
Funding
No funds were received in connection to the presented study. The coauthors declare that they have no competing interests.
Informed consent
Informed consent was given from all of the patients for participation in this study. Those patients who contributed to the figures gave their informed consent for the photographs as well.
Rights and permissions
About this article
Cite this article
Schulz-Drost, S., Grupp, S., Pachowsky, M. et al. Stabilization of flail chest injuries: minimized approach techniques to treat the core of instability. Eur J Trauma Emerg Surg 43, 169–178 (2017). https://doi.org/10.1007/s00068-016-0664-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-016-0664-7