Abstract
Purpose
The purpose of this large-animal study was to assess the safety and effects of negative pressure therapy (NPT) when used as temporary abdominal closure in the immediate post-decompression period after abdominal compartment syndrome (ACS).
Methods
Using a hemorrhagic shock/resuscitation and mesenteric venous pressure elevation model, ACS was physiologically induced in 12 female Yorkshire swine. At decompression, animals were allocated to either NPT (n = 6) or Bogota bag (n = 6) as temporary abdominal closure and studied for a period of 48 h or until death. Outcomes measured included morbidity and mortality, as well as hemodynamic parameters, ventilator-related measurements, blood gases, coagulation factors, and organ (liver, kidney, lung, and intestinal) edema and histology at the time of death/sacrifice.
Results
All animals developed ACS. Early application of NPT was associated with decreases in mesenteric venous and central venous pressure, and significantly increased drainage of peritoneal fluid. In addition, there was no increase in the incidence of mortality, recurrent intra-abdominal hypertension/ACS, or any deleterious effects on markers of organ injury.
Conclusions
Early application of NPT in this porcine ACS model is safe and does not appear to be associated with an increased risk of recurrent intra-abdominal hypertension. The results of this animal study suggest that the application of NPT following decompression from ACS results in greater peritoneal fluid removal and may translate into augmented intestinal edema resolution secondary to more favorable fluid flux profiles.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the last several decades, the morbidity and mortality associated with traumatic injuries have decreased secondary to aggressive resuscitation strategies and the widespread adoption of damage control surgery. While early aggressive intervention improves patient survival, there are a number of resulting pathophysiological derangements, including hemodilution and increased capillary permeability from global ischemia/reperfusion injury. An end consequence is the development of edema in various organ systems and the translocation of fluid into the peritoneum. When allowed to progress without timely intervention, these factors contribute to the development of abdominal compartment syndrome (ACS). The World Congress on Abdominal Compartment Syndrome consensus statement defines ACS as an intra-abdominal pressure (IAP) >20 mmHg, leading to new-onset organ dysfunction [1]. This may include elevated peak airway pressures (as a reflection of increased IAP), deceased urine output, decreased PaO2/FiO2 (P:F) ratio (<150), and/or decreased cardiac index [2]. ACS is associated with significant morbidity and mortality (approximately 50% by current estimates) [2, 3]. Key factors in the development of ACS include continued hemorrhage and hemorrhagic shock, uncontrolled bleeding, tissue edema, and the translocation of fluid (third spacing) into the intestinal lumen and peritoneal cavity.
Decompressive laparotomy is widely accepted as definitive immediate therapy for ACS. There are a number of choices for temporary abdominal closure after decompression; the most common class used for management of the open abdomen includes vacuum/negative pressure-associated devices [4]. There are few studies examining the choice of temporary abdominal closure and outcome in the setting of decompression after ACS. Preliminary results indicate that Vacuum Assisted Closure® therapy (Kinetic Concepts, Inc., San Antonio, TX) in the setting of intra-abdominal sepsis not only improves fluid removal but also attenuates the inflammatory response and secondary organ injury [5]. However, two recent laboratory papers have suggested that, in the immediate post-decompression period after ACS, negative pressure therapy (NPT) may be detrimental secondary to decreased intra-abdominal volume resulting from the application of negative pressure and the theoretical “reperfusion” syndrome occurring after decompression that may exacerbate organ edema [6, 7].
We hypothesized that the immediate post-decompression application of NPT would be safe in a clinically severe, large-animal model of ACS. To accomplish this, we sought to determine the effect of the application of the ABThera™ Open Abdomen Negative Pressure Therapy System (ABThera™; KCI Licensing, Inc., San Antonio, TX) as compared to Bogota bag closure on organ physiology and injury measurements and mortality when used after decompression from ACS.
Materials and methods
All procedures were approved by the University of Texas Health Science Center at Houston Institutional Animal Care and Use Committee and were consistent with the National Institutes of Health’s “Guide for the Care and Use of Laboratory Animals”.
Animal model
All experiments were based off a previously published and validated large-animal model of ACS developed by Shah et al. [8]. Female Yorkshire swine were fasted overnight (12–16 h) with free access to water. General anesthesia was induced and maintained by continuous intravenous infusion of pentobarbital and ketamine. The animals were intubated and ventilated in volume control mode, with a starting fraction of inspired oxygen (FiO2) of 21%, positive end expiratory pressure (PEEP) of 5 mmHg, and a tidal volume of 10 cc/kg; these values were adjusted based on the results of arterial blood gas analysis done at sequential time points.
Catheters were placed into the femoral artery and vein for hemodynamic monitoring and fluid infusion, respectively. A Swan-Ganz pulmonary artery thermodilution catheter (Millar Instruments, Houston, TX) was placed into the internal jugular vein and positioned into the pulmonary artery by flow direction. A midline laparotomy was then performed. Additional instrumentation consisted of placing a suprapubic bladder catheter, a peritoneal catheter for the collection of peritoneal fluid, a silastic catheter connected to a pressure transducer in a distal mesenteric vein, as well as an umbilical vein snare around the portal vein for the induction of mesenteric venous hypertension. A saline-filled bag connected to a pressure transducer was placed into the peritoneal cavity as an abdominal pressure manometer. Transducers were leveled to the height of the pig and zeroed prior to insertion. The bladder catheter, peritoneal fluid catheter, mesenteric venous pressure (MVP) catheter, pressure tubing from the abdominal pressure manometer, and portal vein snare exited the abdomen through 2-cm incisions; they were secured in place with purse-string sutures. At the conclusion of instrumentation, the abdominal fascia and skin were closed with suture in a running fashion.
After instrumentation, hemorrhagic shock was induced by bleeding via the femoral venous catheter to a mean arterial pressure (MAP) of approximately 35 mmHg. The animals were allowed to stabilize for a period of 1 h. After stabilization, the collected blood (anticoagulated with 100 units/kg heparin) plus two equal volumes of crystalloid (Lactated Ringer’s, Baxter, Deerfield, IL) were re-infused rapidly. The MVP was increased to approximately 30 mmHg by tightening the previously placed portal vein snare. Lactated Ringer’s solution was infused to maintain an MAP above 65 mmHg. When the IAP reached 30 mmHg with development of organ dysfunction in at least one organ system, a decompressive laparotomy was performed. New organ dysfunction was manifested by changes in hemodynamic parameters, peak airway pressures, P:F ratios, lactate, anion gap, and base excess.
Experimental groups
Temporary abdominal closure was achieved either by the placement of a Bogota bag (n = 6) or NPT (ABThera™; KCI Licensing, Inc., San Antonio, TX) (n = 6). The Bogota bag was placed as per standard published descriptions and consisted of sewing an empty, sterilized polyvinyl chloride irrigation fluid bag to the skin of the anterior abdominal wall [9]. The ABThera™ Dressing (KCI Licensing, Inc., San Antonio, TX) was placed as per the manufacturer’s suggested protocol and negative pressure was applied continuously throughout the experimental period (−125 mmHg). Animals were monitored for 48 h (at which time they were sacrificed) or until the time of death.
Primary outcome measures
The primary outcome measures utilized were incidence of recurrent intra-abdominal hypertension (defined as an IAP ≥ 20 mmHg), time to death (measured in hours), and total volume of peritoneal fluid evacuated over the study period. A variety of secondary outcome measures were utilized in order to evaluate the effects of NPT on organ physiology and injury.
Secondary outcome measures
Organ edema
Wet to dry ratios were determined in the lung (right superior and inferior lobe), intestine (duodenum, jejunum, and ileum), liver (left lobe), and kidney (right). Tissues were weighed immediately after collection and allowed to dry in a 60°C oven for a period of 2–3 days or until the dry weight did not change. The wet to dry ratio was then calculated based on the following equation: wet to dry ratio = (wet weight − dry weight)/(dry weight).
Organ histology
All histomorphologic examinations were performed in a blinded fashion by a board-certified veterinary pathologist. At the time of death and/or sacrifice, tissues from the right lung, intestine (duodenum, jejunum, and ileum), right kidney, and left lobe of the liver were placed in 10% neutral buffered formalin. The parameters utilized to delineate organ injury were as follows.
Lung
Each sample was evaluated and scored on the following parameters: hyperdistension, atelectasis, congestion, fibrin, and neutrophils.
Intestine
Histological assessments were made by giving each section a score from 0 to 4 as follows: 0 = no significant abnormality; 1 = mild abnormality; 2 = moderate abnormality; 3 = severe abnormality (localized); 4 = severe abnormality (generalized). The pathologic criteria used for the determination of intestinal injury are described in Table 1.
Kidney
A semi-quantitative score for tubular injury and acute tubular necrosis (ATN score) in the outer stripe of the outer medulla and cortex was assigned to each animal. Neutrophil infiltration was quantitatively assessed on periodic acid-Schiff (PAS)-stained tissue by counting the number of neutrophils per high-powered field (400×). Apoptotic tubular cells were quantitatively assessed per high-powered field in the cortex and outer stripe of the outer medulla.
Liver
The tissues were analyzed for total cytoplasmic and nuclear areas, mean cytoplasmic and nuclear intensity, and the amount of blood in the sinusoids.
Physiology
Cardiac output (CO), MAP, pulmonary artery pressure (PAP), central venous pressure (CVP), pulmonary capillary wedge pressure (PCWP), tidal volume, peak inspiratory pressure, and pulse oxygenation (SaO2) were recorded hourly. Additionally, P:F ratios were determined at the time of decompression (V0), 6 h after decompression (V6), 12 h post-decompression (V12), and at 12-h intervals thereafter (V24, V36, and V48). Urine output and total volume infused were recorded hourly. IAP, MVP, and body temperature were recorded hourly.
Blood chemistries
Blood pH, pCO2, pO2, bicarbonate (HCO3), base excess (BE), lactate, prothrombin time (PT), international normalized ratio (INR), creatinine, blood urea nitrogen (BUN), glucose, chloride, sodium, potassium, hemoglobin, anion gap, and total protein were determined at V0, V6, V12, V24, V36, and V48.
Statistical analysis and data presentation
A sample size of six animals per group was chosen, as it would allow us to detect a difference of 1.8 standard deviations or more (p = 0.05; power 0.80) in continuous variables. All values are represented as mean ± standard error of the mean (SEM), unless otherwise specified. The baseline represents the time period before any intervention. Tx represents the time period after hemorrhage and prior to the application of temporary abdominal coverage. Vx represents the time periods upon decompression and application of temporary abdominal coverage. Statistical analysis was performed using SAS software (release 9.1, Cary, NC). A p-value of ≤0.05 was considered to be significant.
Pre-decompression, organ edema, and histology data
As there were no missing values and data were being compared between two groups and did not involve multiple time points, a two-tailed paired t-test was used for comparison within groups and a two-tailed unpaired t-test was used for comparison between groups.
Post-decompression data
For statistical analysis, a least-squares regression model was used to calculate the intra-animal predicted values for animals that failed to survive for 48 h. If predicted values were negative, a value of zero was utilized for that time point. Of note, the data presented do not include predicted values. For parameters with data recorded hourly, descriptive statistics were done at values corresponding to 0, 4, 8, 12, 16, 20, 24, 28, 32, 36, 40, 44, and 48 h post-decompression; for other parameters, descriptive statistics were done at 0, 6, 12, 24, 36, and 48 h post-decompression, as the data were recorded at these time points for these parameters. A two-factor (treatment group and time [V0–V48]) repeated measures analysis of covariance using the V0 value as the covariate based on predicted–imputed data was performed. Significant results from the model were further examined at each time point after V0 following a Bonferroni correction to adjust for multiplicity.
Survival data
Log-rank and Fisher’s exact tests were performed in order to compare the survival data in this study.
Results
Pre-decompression data
Baseline weight
There were no differences in body weights between the Bogota group (34.9 ± 1.2 kg) and the NPT group (34.9 ± 1.5 kg).
Development of hemorrhagic shock
There were no significant differences between baseline MAPs in the Bogota (99.4 ± 4.5 mmHg) and NPT (88.4 ± 5.1 mmHg) groups. Additionally, there were no significant differences between the MAP achieved after hemorrhage in the Bogota (35.5 ± 0.4 mmHg) and NPT (34.1 ± 0.4 mmHg) groups.
Hemorrhage volume/time
The rate was not significantly different between the Bogota group (1.02 ± 0.08 mL/s) and the NPT group (1.05 ± 0.09 mL/s). The average volume of blood required to reach an MAP of 35 mmHg was 533.3 ± 50.7 mL. The volume was not significantly different between the Bogota (584.7 ± 83.3 mL) and NPT groups (471.6 ± 45.2 mL).
Auto-resuscitation
Prior to fluid resuscitation there was some recovery of MAP from the time of hemorrhage to the measurement immediately prior to fluid resuscitation with shed blood and crystalloid. There were no significant differences between the Bogota (49.0 ± 2.6 mmHg) and NPT (49.6 ± 2.6 mmHg) groups.
Induction of mesenteric venous hypertension
There were no significant differences in the baseline MVP in the Bogota (19.6 ± 1.4 mmHg) and NPT (21.9 ± 1.1 mmHg) groups. Additionally, there were no significant differences in the MVP when measured after resuscitation and the induction of mesenteric venous hypertension between the Bogota (31.1 ± 0.8 mmHg) and NPT (31.8 ± 0.9 mmHg) groups.
Development of intra-abdominal hypertension
There were no significant differences in the baseline IAPs between the Bogota (5.9 ± 1.1 mmHg) and NPT (6.9 ± 1.0 mmHg) groups. Additionally, there were no significant differences in the IAP when ACS was achieved, being 31.7 ± 0.5 mmHg (Bogota) versus 31.4 ± 0.3 mmHg (NPT).
Volume required for the development of abdominal compartment syndrome
The volume of fluids received during the resuscitation period (lactated Ringer’s) was not significantly different between the Bogota (85.8 ± 5.6 cc/kg/h) and NPT (92.3 ± 6.2 cc/kg/h) groups.
Time to development of ACS
The time to the development of ACS was not significantly different in the Bogota (3.3 ± 0.6 h) and NPT (2.8 ± 0.3 h) groups.
Development of new organ dysfunction
There were no significant differences at baseline in the CO, CVP, PAP, MAP, PCWP, temperature, tidal volume, PEEP, peak inspiratory pressure, infusion volume, urine output, pH, PCO2, PO2, HCO −3 , BE, SaO2, lactate, PT, INR, creatinine, BUN, glucose, Cl, Na, K, Ca, anion gap, PaO2:FiO2 ratio, and protein between the Bogota and NPT groups. Parameters for new organ dysfunction are presented in aggregate. New organ dysfunction was manifested by changes in the CVP, PAP, PCWP, MAP, peak airway pressures, P:F ratios, lactate, anion gap, and base excess. The specific values are presented in Table 2 [10].
Primary outcome measures
Mortality
The number of animals that died prior to the conclusion of the 48-h experimental period was 3/6 in the Bogota group and 2/6 in the NPT group. The average time to mortality in the Bogota group was 29.8 ± 8.2 h as compared to 40.5 ± 4.8 h in the NPT group. The difference between the two groups was not statistically significant (p = 0.39, log-rank test). Fisher’s exact test, used to compare the mortality proportion in this study, revealed that the odds ratio for survival was 2.0 (95% confidence interval 0.12–36.87; p = 1.0).
Incidence of recurrent intra-abdominal hypertension after decompression
The incidence of recurrent intra-abdominal hypertension was equal among the Bogota (n = 2/6) and NPT groups (n = 2/6).
Amount of peritoneal fluid evacuated over the study period
The amount of peritoneal fluid evacuated in the Bogota group was 312.5 ± 42.7 mL as compared to 2,946.7 ± 351.2 mL in the NPT group. The difference between groups was statistically significant (p < 0.0001).
Organ edema
Lung
There were no significant differences in the lung wet to dry ratio between the Bogota and NPT groups with regards to either superior (6.5 ± 1.6 vs. 5.8 ± 1.3, Bogota vs. NPT, p = 0.4) or inferior (6.3 ± 1.3 vs. 6.0 ± 0.8, Bogota vs. NPT, p = 0.7) lobes of the right lung.
Intestine
There were no differences in the wet to dry ratios in the duodenum (5.6 ± 1.1 vs. 5.2 ± 0.5, Bogota vs. NPT, p = 0.4), jejunum (6.8 ± 1.2 vs. 7.1 ± 2.6, Bogota vs. NPT, p = 0.7), or ileum (7.5 ± 2.0 vs. 7.1 ± 2.2, Bogota vs. NPT, p = 0.8).
Liver
There were no significant differences in the wet to dry ratios as measured in the left lobe of the liver between the Bogota and NPT groups (3.7 ± 0.4 vs. 3.6 ± 0.4, p = 0.5).
Kidney
Wet to dry ratios were measured in the central portion of the right kidney. There were no significant differences between the Bogota and NPT groups (5.4 ± 0.6 vs. 5.9 ± 0.5, p = 0.1). In addition, wet to dry ratios were also measured in the anterior and posterior sections of the right kidney; there were no significant differences noted between the two groups.
Organ histology
Lung
Histology of the dependent portion of the right lung inferior lobe was examined. There were no significant differences between the Bogota and NPT groups with regards to alveolar atelectasis, inflammation, wall thickness/cellularity, fibrin, or hemorrhage. Additionally, there were no differences observed with regards to bronchopneumonia and interstitial edema between the Bogota and NPT groups.
Intestine
Histology of the duodenum, jejunum, and ileum were evaluated. There were no significant differences in the jejunum and ileum between the NPT and Bogota groups with regards to villous structure, villous epithelial damage, villous lamina propria edema or inflammation, crypt epithelial damage, crypt lamina propria edema or inflammation, or submucosa edema and/or inflammation.
Liver
Histology was examined in the left lobe of the liver. No differences between the Bogota and NPT groups were noted in hepatocellular damage as measured by vacuolar degeneration and necrosis. Additionally, no differences in periportal/interlobular inflammation or sinusoidal congestion were noted between the two groups.
Kidney
No significant difference in kidney damage as measured by interstitial tissue edema, inflammation, capillary congestion, or tubular epithelial damage was seen among the Bogota and NPT groups. Of note, no glomerular damage was observed in either group.
Organ physiology/blood chemistry
Cardiovascular
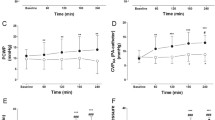
Cardiovascular function was determined by measurements of the following variables: CO, CVP, MAP, and hemoglobin. Analysis of these variables revealed no significant differences or trends between the groups, except for CVP, which demonstrated differences at V44 and V48 (CVP lower in the NPT group) (Fig. 1). Data for the cardiovascular variables are presented in Table 3 (see supplementary material).
Pulmonary
Pulmonary function was determined by PAP, PCWP, PEEP, tidal volume, peak inspiratory pressure, pH, pO2, pCO2, SaO2, and P:F ratio. No significant differences in the pulmonary variables between the groups were noted. Data for pulmonary variables are presented in Table 4 (see supplementary material).
Fluid, electrolytes, and nutrition (FEN)/gastrointestinal (GI) system
FEN/GI function was determined by IAP, MVP, serum sodium, serum potassium, and serum chloride. Significant differences between groups were noted in MVP at the V12, V24, V28, V32, V36, V40, V44, and V48 time points, with lower values being noted in the NPT group (Fig. 2). No significant differences were noted with IAP, serum sodium, serum potassium, or serum chloride. The data for FEN/GI variables are presented in Table 5 (see supplementary material).
Hepatobiliary
Hepatobiliary function was determined by PT, INR, and plasma protein. There were no significant differences between treatment groups. The data for these variables are presented in Table 6 (see supplementary material).
Ischemia
Ischemic injury was assessed by evaluating serum lactate (mmol/L). There were no significant differences between the Bogota and NPT groups, respectively, at V0 (4.9 ± 1.9 vs. 6.9 ± 1.3), V6 (1.9 ± 1.0 vs. 2.5 ± 1.1), V12 (3.2 ± 3.2 vs. 2.3 ± 2.0), V24 (0.9 ± 0.6 vs. 4.8 ± 7.5), V36 (2.9 ± 2.8 vs. 1.4 ± 1.2), or V48 (1.0 ± 0.4 vs. 0.7 ± 0.5).
Renal
Renal function was determined by the evaluation of the following variables: infusion volume, urine output, serum BUN, serum creatinine, serum anion gap, serum base excess, and serum HCO3. There were no significant differences noted with regards to any of the variables tested between the Bogota and NPT groups. The data for renal function variables are presented in Table 7 (see supplementary material).
Miscellaneous variables
Other variables measured included serum glucose and body temperature. There were no significant differences between treatment groups with regards to serum glucose or body temperature. The data for endocrine variables are presented in Table 8 (see supplementary material).
Central venous pressure (CVP). At the latter time points (V44 and V48), the CVP is significantly lower in the NPT group as compared to the Bogota group (p < 0.05). BL (baseline) represents the time period before any intervention. Tx represents the time period after hemorrhage and prior to the application of temporary abdominal coverage. Vx represents the time periods upon decompression and application of temporary abdominal coverage. The data are presented as mean ± standard deviation; n = 6/group
Mesenteric venous pressure (MVP). MVP is significantly lower in the NPT group at the V12 and V24–48 time points (p < 0.05). BL (baseline) represents the time period before any intervention. Tx represents the time period after hemorrhage and prior to the application of temporary abdominal coverage. Vx represents the time periods upon decompression and application of temporary abdominal coverage. The data are presented as mean ± standard deviation; n = 6/group
Discussion
The data presented demonstrate that the immediate application of NPT as temporary abdominal closure in the immediate post-decompression period from ACS is safe. This data is important, as it refutes recent studies suggesting that loss of intra-abdominal domain in the acute post-decompression period may be associated with an increased incidence of recurrent ACS or worsened outcomes [6, 7]. In our model of non-infectious ACS, we did not observe a significant reduction in either the inflammatory response, as measured, or the extent to injury, as determined by tissue edema. However, we did observe that the immediate post-decompression application of NPT was not associated with increased mortality or an increased incidence of recurrent intra-abdominal hypertension.
The described ACS model incorporates hemorrhage, resuscitation, and the effects of damage control surgery. This unique large-animal model relies on the pathophysiological development of ACS without the artificial installation of fluids or other substances reported with other published models [11]. The interplay of global ischemia/reperfusion injury (hemorrhagic shock/resuscitation-induced injury), third spacing of fluid into the gut lumen, interstitium, and peritoneum secondary to hemodilution and altered microvascular fluid flow, and mesenteric venous hypertension (both as a contributor to altered microvascular fluid flow resulting in edema and as a result of increasing intra-abdominal pressures) [12] contribute to the vast number of cases of non-infectious ACS. This porcine model models this pathophysiology; it also allows one to study the effect of various interventions on the course of ACS and is easily reproducible; all animals developed ACS (as evidenced by intra-abdominal hypertension and new-onset organ dysfunction) in a similar time frame. ACS is associated with significant patient morbidity and mortality (upwards of 50%), especially in those situations when decompression is delayed or symptoms go unnoticed. This model is associated with approximately 50% mortality (approximately 50% of animals did not survive the 48-h study period), which, while high, is similar to the mortality rate of the ACS patient population.
There are several technical issues that merit discussion. As per the definition of ACS, the majority of surgeons will intervene in patients with an intra-abdominal pressure of 20 mmHg or higher and co-existing new-onset organ dysfunction. In this study, we utilized an IAP of 30 mmHg prior to intervention. This was done for two major reasons. A number of studies describing porcine models of ACS use a target IAP of 30 mmHg [13–16]. Although in previous studies we have demonstrated that an IAP of 20 mmHg in swine does lead to new-onset organ dysfunction, it does not lead to the mortality that parallels the values described in the human ACS literature [8].
In this study, the IAP was measured via direct intra-peritoneal measurements with a pressure transducer. Clinically, bladder pressures are often used as a non-invasive surrogate marker for intra-abdominal pressure. We elected not to use bladder/gastric pressure measurements for two major reasons. First, these represent indirect ways to measure IAP. Secondly, these methods do not allow for continuous measurements. Our manometer setup allowed for the real-time direct measurement of IAP. Previous studies have shown that direct measurements of IAP with catheters correlate well with indirect pressure manometers in the stomach or bladder [17].
The major limitation of our study has to do with the limited sample size. The lack of significant differences does not necessarily indicate equality between groups; it may represent the lack of adequate power. Therefore, the results must be interpreted carefully. We cannot make any conclusions about a survival advantage afforded by NPT. Although NPT appeared to be associated with increased time of survival of 29.8 ± 8.2 h (Bogota group) versus 40.5 ± 4.8 h (NPT group), the odds ratio for survival was not statistically significant (likely due to our sample size). Further investigation is needed and we believe that this study forms the springboard for larger studies.
The outcomes which we observed combined with recently reported data from other groups deserves discussion. Kubiak et al. [5] recently demonstrated that NPT used as temporary abdominal closure in a large-animal model of multiple organ dysfunction driven by gut ischemia reperfusion and intra-abdominal sepsis led to improved survival. In this study, NPT (as compared to passive drainage) was associated with the preservation of organ function (including decreased lung, intestinal, and renal injury) and a significant downregulation in the systemic inflammatory response as measured by cytokine levels.
The effect of NPT may be secondary to an effect on peritoneal fluid. We have recently demonstrated that peritoneal fluid from ACS serves as a primer of naïve neutrophils and monocytes [10]. It is well documented that peritoneal fluid can be reabsorbed into the systemic circulation, primarily via lymphatic conduits [18, 19]. Given this data and evidence that peritoneal fluid is pro-inflammatory by representing a potential primer for naïve neutrophils, a potential mechanism for systemic effects of peritoneal fluid can be made, either as an initiator (i.e., intra-abdominal sepsis) or propagator of systemic inflammation. Whether the mechanism of NPT is via an effect on peritoneal fluid remains an active subject of investigation.
It is notable that there was a reduction in the CVP and MVP in the NPT group compared to the Bogota group. While the exact significance of these findings is unknown, a reduction in CVP and MVP over time may translate into augmented intestinal edema resolution secondary to a more favorable fluid flux profile that promotes decreased tissue water accumulation, increased tissue water efflux, and improved organ function [20]. Elucidation of this difference may require evaluating the effect of NPT treatment at longer time points.
In summary, using a clinically relevant, severe hemorrhagic shock model of ACS in swine, NPT therapy appears to be safe and may be associated with factors that lead to improved outcomes. Our findings using this model may be useful in developing a paradigm for looking at NPT as a protective therapy, potentially via a peritoneal fluid-related mechanism, and to better understand NPT’s mechanism of action in reducing the inflammatory cascade associated with acute trauma.
References
Malbrain ML, Cheatham ML, Kirkpatrick A, Sugrue M, Parr M, De Waele J, et al. Results from the International Conference of Experts on Intra-abdominal Hypertension and Abdominal Compartment Syndrome. I. Definitions. Intensive Care Med. 2006;32(11):1722–32. doi:10.1007/s00134-006-0349-5.
Balogh ZJ, van Wessem K, Yoshino O, Moore FA. Postinjury abdominal compartment syndrome: are we winning the battle? World J Surg. 2009;33(6):1134–41. doi:10.1007/s00268-009-0002-x.
De Waele JJ, Hoste EA, Malbrain ML. Decompressive laparotomy for abdominal compartment syndrome—a critical analysis. Crit Care. 2006;10(2):R51. doi:10.1186/cc4870.
MacLean AA, O’Keeffe T, Augenstein J. Management strategies for the open abdomen: survey of the American Association for the Surgery of Trauma membership. Acta Chir Belg. 2008;108(2):212–8.
Kubiak BD, Albert SP, Gatto LA, Snyder KP, Maier KG, Vieau CJ, et al. Peritoneal negative pressure therapy prevents multiple organ injury in a chronic porcine sepsis and ischemia/reperfusion model. Shock. 2010;34(5)525–34.
Benninger E, Laschke MW, Cardell M, Keel M, Seifert B, Trentz O, et al. Intra-abdominal pressure development after different temporary abdominal closure techniques in a porcine model. J Trauma. 2009;66(4):1118–24. doi:10.1097/TA.0b013e3181820d94.
Benninger E, Labler L, Seifert B, Trentz O, Menger MD, Meier C. In vitro comparison of intra-abdominal hypertension development after different temporary abdominal closure techniques. J Surg Res. 2008;144(1):102–6. doi:10.1016/j.jss.2007.02.021.
Shah SK, Jimenez F, Walker PA, Xue H, Uray KS, Aroom KR et al. A novel physiologic model for the study of abdominal compartment syndrome (ACS). J Trauma. 2010;68(3):682–9. doi:10.1097/TA.0b013e3181c453cb.
Kirshtein B, Roy-Shapira A, Lantsberg L, Mizrahi S. Use of the “Bogota bag” for temporary abdominal closure in patients with secondary peritonitis. Am Surg. 2007;73(3):249–52.
Shah SK, Jimenez F, Walker PA, Aroom KR, Xue H, Feeley TD, et al. A novel mechanism for neutrophil priming in trauma: potential role of peritoneal fluid. Surgery. 2010;148(2):263–70. doi:10.1016/j.surg.2010.03.019.
Schachtrupp A, Wauters J, Wilmer A. What is the best animal model for ACS? Acta Clin Belg Suppl. 2007;225–32.
Moore-Olufemi SD, Xue H, Allen SJ, Moore FA, Stewart RH, Laine GA, et al. Effects of primary and secondary intra-abdominal hypertension on mesenteric lymph flow: implications for the abdominal compartment syndrome. Shock. 2005;23(6):571–5. doi:00024382-200506000-00015[pii].
Wauters J, Claus P, Brosens N, McLaughlin M, Malbrain M, Wilmer A. Pathophysiology of renal hemodynamics and renal cortical microcirculation in a porcine model of elevated intra-abdominal pressure. J Trauma. 2009;66(3):713–9. doi:10.1097/TA.0b013e31817c5594.
Schachtrupp A, Lawong G, Afify M, Graf J, Toens C, Schumpelick V. Fluid resuscitation preserves cardiac output but cannot prevent organ damage in a porcine model during 24 h of intraabdominal hypertension. Shock. 2005;24(2):153–8. doi:00024382-200508000-00009[pii].
Schachtrupp A, Graf J, Tons C, Hoer J, Fackeldey V, Schumpelick V. Intravascular volume depletion in a 24-hour porcine model of intra-abdominal hypertension. J Trauma. 2003;55(4):734–40. doi:10.1097/01.TA.0000042020.09010.D7.
Toens C, Schachtrupp A, Hoer J, Junge K, Klosterhalfen B, Schumpelick V. A porcine model of the abdominal compartment syndrome. Shock. 2002;18(4):316–21.
Engum SA, Kogon B, Jensen E, Isch J, Balanoff C, Grosfeld JL. Gastric tonometry and direct intraabdominal pressure monitoring in abdominal compartment syndrome. J Pediatr Surg. 2002;37(2):214–8. doi:S0022346802415485[pii].
Tarpila E, Nyström PO, Ihse I. The resorption of FITC-dextran 10,000 from the peritoneum in different modifications of bile-induced acute pancreatitis and in bacterial peritonitis. Int J Pancreatol. 1991;10(3–4):229–36.
Ishimaru K, Mitsuoka H, Unno N, Inuzuka K, Nakamura S, Schmid-Schönbein GW. Pancreatic proteases and inflammatory mediators in peritoneal fluid during splanchnic arterial occlusion and reperfusion. Shock. 2004;22(5):467–71. doi:00024382-200411000-00011[pii].
Radhakrishnan RS, Shah SK, Lance SH, Radhakrishnan HR, Xue H, Radhakrishnan GL, et al. Hypertonic saline alters hydraulic conductivity and up-regulates mucosal/submucosal aquaporin 4 in resuscitation-induced intestinal edema. Crit Care Med. 2009;37(11):2946–52. doi:10.1097/CCM.0b013e3181ab878b.
Acknowledgments
This study was supported by NIH Grants T32 GM 0879201 and RO1 HL 092916; Children’s Memorial Hermann Hospital Foundation; Texas Higher Education Coordination Board; Kinetic Concepts, Inc.
Conflict of interest
Funding for this project was provided, in part, by a grant from Kinetic Concepts, Inc. (to Charles S. Cox, Jr, MD).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shah, S.K., Jimenez, F., Walker, P.A. et al. Evaluating the effects of immediate application of negative pressure therapy after decompression from abdominal compartment syndrome in an experimental porcine model. Eur J Trauma Emerg Surg 38, 65–73 (2012). https://doi.org/10.1007/s00068-011-0136-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-011-0136-z