Abstract
Background
The liver is the most frequently affected organ during blunt abdominal trauma. Blunt liver trauma management has changed in the last two decades with the introduction of the computed tomography (CT) scan and non-operative management of stable patients.
Objective
To determine the incidence, efficacy, and failure rate of blunt liver trauma non-operative management as well as the risk factors associated with such treatment in a level 1 trauma center in Colombia.
Methods
We conducted an observational descriptive study on patients with blunt liver trauma who were admitted to a level 1 trauma center in Colombia. The evaluated outcomes were indications of immediate surgical treatment and the success of non-operative management.
Results
A total of 73 patients were studied. The most common mechanism of trauma continues to be motor vehicle crashes. In 14 patients (19.2%), immediate surgical intervention was necessary and we observed a Revised Trauma Score (RTS) above 7.8 and intra-abdominal injuries as risk factors. Three patients died (21.4%). Fifty-nine patients (80.8%) received non-operative management, which failed in seven patients (11.2%). Age, severity of liver injury, and intra-abdominal injuries were not risk factors in the failure of non-operative management. Mortality in the non-operative management group was 1.7%.
Conclusion
Non-operative management is the treatment of choice for polytraumatized patients with blunt liver trauma who are hemodynamically stable. Non-operative management is an effective and safe treatment strategy. However, patients with an RTS score under 7.8 and other intra-abdominal non-liver injuries are at increased risk for an immediate surgical intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The liver is the most frequently affected organ in blunt abdominal trauma. Since the introduction of computed tomography (CT) scans in the 1980s, non-operative management of blunt liver trauma has emerged as an alternative to surgery in hemodynamically stable trauma patients [1, 2]. During the last two decades, studies have found that the efficacy of non-operative management in blunt liver trauma on hemodynamically stable patients is between 87 and 98%, and the failure rate is between 10 and 25% [1–3]. Failure of non-operative management is defined as the need for surgical treatment for a patient who was offered a non-operative alternative at the beginning of treatment. Failure of non-operative management has been associated with several factors, including transfusion of more than two units of red blood cells in the first 6 h of trauma, a positive focused abdominal sonograph of trauma (FAST), an associated spleen injury, an Injury Severity Score (ISS) over 18, and over 300 cc of free fluid in the CT scan [4–6].
The incidence of complications during non-operative management of blunt liver trauma is low (0–11%) [7, 8]. Risk factors such as severity of liver injury have been associated with an increased incidence of complications for non-operative management of blunt liver trauma. We conducted an observational study to assess the incidence, efficacy, and failure rate of blunt liver trauma non-operative management and the risk factors of non-operative management in the Hospital Universitario San Vicente de Paúl, a level 1 trauma center in Colombia.
Materials and methods
We conducted an observational descriptive study with a retrospective phase between January 2005 and June 2007 and a prospective phase from July 2007 to December 2008. We included all patients over 15 years of age with blunt abdominal trauma who arrived at the level 1 trauma center in the emergency room of the Hospital Universitario San Vicente de Paúl. Liver trauma was confirmed by CT scan or from a surgeon’s report. We excluded patients with more than 24 h of trauma, patients who received surgical treatment in a different hospital, and individuals who decided not to participate in the study. The ethics committee of the Hospital Universitario San Vicente de Paúl accepted this study.
All patients’ charts were reviewed. We considered demographic variables such as age, gender, history of medical or abdominal procedures, and trauma mechanism. We also recorded the Revised Trauma Score (RTS), ISS, volume and type of fluids used for resuscitation, and the use of FAST. Liver injury was categorized using the Organ Injury Scale (OIS) of the American Association for the Surgery of Trauma (AAST) [9]. For patients who received non-operative management, the level of injury was determined according to the findings of the CT scan. For patients who received surgical management, we recorded the level of injury according to the surgical report.
Patients were treated according to the Advanced Trauma Life Support (ATLS) guidelines [10]. Resuscitations began with crystalloids; if the patient remained unstable, we performed an FAST. When ultrasonography showed free fluid in the abdominal cavity, the trauma surgeon decided whether to operate on the patient. Patients who underwent surgery entered this study under immediate surgical management.
After resuscitation, stable patients had an abdominal CT scan and began non-operative management. When CT showed contrast blush, the patient underwent radiological intervention.
Patients were monitored daily until discharge. We recorded the values of excess base, hemoglobin, amount of intravenous (IV) fluids received, number of red cell packs transfused, imaging studies performed, complications related or unrelated to liver trauma, and the need for operative management.
The evaluated outcomes were indications of immediate surgical treatment and failure of non-operative management was defined by surgical treatment 24 h after admission to the hospital or after initial resuscitation [3, 5, 7, 11, 12].
The study was approved by the ethics and research committee of the hospital and the Universidad de Antioquia.
Statistical analysis
Analysis included a descriptive and analytic phase. In the descriptive phase, we studied all qualitative variables, which were presented as frequencies, means, medians, standard deviations (SDs), and ranges. In the analytical phase, we performed bivariate analysis, in which we explored risk factors related to the outcomes using the risk ratio (RR). Statistical analyses were done with SPSS version 17.0 software. Categoric variables were compared using Fisher’s exact test.
Results
Demographic variables
Between January 2005 and December 2008, we found 73 patients (54 males and 19 females) with blunt liver trauma (36 retrospective and 37 prospective). The mean age was 32.1 years (SD 15.78) and the age ranged from 15 to 80 years.
The most common trauma mechanisms were motor vehicle crashes (35 cases, 47.9%) and pedestrian accidents (22 cases, 30.1%) (Table 1).
Six patients (8.2%) had medical records of previous abdominal surgery. Patients admitted to the emergency room for abdominal trauma had a median RTS of 7.55 (25th percentile of 6.37, 75th percentile of 7.84) and a median ISS of 22 (25th percentile of 13, 75th percentile of 27).
Extra-abdominal injuries associated with blunt liver trauma included mild brain trauma injury in eight patients (11%), moderate brain trauma injury in four patients (5.5%), and severe brain trauma injury in 11 patients (15.1%). There were seven patients with spinal cord injuries and 13 patients with pelvic fractures. FAST was performed on 19 patients (26%).
Immediate surgical interventions
Fourteen patients (19.2%) with blunt liver trauma required immediate laparotomies at admission to the hospital. Of these patients, five (35.8%) had liver trauma only and nine (64.2%) had associated injuries such as kidney (3), bowel (2), spleen (3), and pancreatic (1) trauma.
Of these 14 patients, three died (21.4%). The first patient had only liver trauma grade V; the second patient had liver trauma grade V and kidney and diaphragm injuries; and the third had a grade IV liver injury and pancreatic trauma.
We explored risk factors associated with the need for immediate surgical intervention (Table 2) and found that RTS under 7.8 (RR 6.2, 95% confidence interval [CI] 1.3–30.2), and intra-abdominal associated injuries are risk factors for immediate surgical treatment in blunt liver trauma.
Non-operative management
Out of 73 patients in total, 59 patients (80.8%) with blunt liver trauma were chosen for non-operative management. Of these, 30 patients (51%) were diagnosed with mild liver injuries (grade I–II) according to the AAST classification [9]. No patient demonstrated grade V injuries (Table 3).
One patient required a selective embolization of one branch of the hepatic artery. From the non-operative management group, 19 patients (32.2%) had other organ injuries: six patients (31.5%) had spleen trauma, 12 patients (63%) had kidney trauma, and one patient had (5.2%) pancreas trauma.
Failure of non-operative management
Non-operative management failed in seven patients (11.86%). Four patients had isolated liver injuries that required surgery; the indication of surgery in three patients was hemodynamic instability and the indication of surgery in the fourth patient was abdominal pain caused by bilioperitoneum. The other three patients had associated injuries that required operative management: one had a late diagnosis of intra-peritoneal bladder rupture, one had post-traumatic pancreatitis, and one had a contained aortic rupture. This last patient died during the surgical procedure, which occurred 3 days after his admission to the hospital. Mortality in the non-operative management group was 1.7%.
Of the 52 patients who experienced successful non-operative management, there were four complications (7.7%): two liver abscesses that required percutaneous drainage, one catheter-related sepsis, and one case of nosocomial pneumonia.
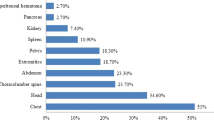
The outcomes are presented in Fig. 1.
Risk factors for failure of non-operative management
We explored the relationship between failure of non-operative management with the following variables: gender, age, ISS, RTS, presence of associated intra-abdominal injuries, severity of liver injury, associated brain trauma injury, number of intra-abdominal quadrants occupied by blood on the FAST exam, and number of transfused red blood cell units in the first 24 h. None of the factors studied was associated with the failure of non-operative management (Table 4).
Discussion
Management of blunt liver trauma has changed over the past two decades. Advances in CT imaging have allowed non-operative management to be used as an alternative to surgery. Studies report that the efficacy of non-operative blunt liver trauma management is between 87 and 98% [1, 2, 5, 13–19].
In agreement with previous findings, we achieved successful non-operative management in 80.2% of our patients and a success rate of 88.1%.
As blunt liver trauma occurs more frequently in males (1.5–2:1 ratio), gender has been explored as a risk factor for non-operative management failure. However, in this and other studies, gender was not a risk factor [6, 10, 12–14].
Geriatric patients have been considered to be a high-risk group in trauma management because of their higher tendency for severe trauma and prolonged hospitalization [20]. The cardiovascular, respiratory, renal, nutritional, and immunological changes related to trauma require close monitoring of these patients. Several studies have failed to associate age with non-operative management failure [17, 21–23]. In the present study, age was not found to be a predictive factor for immediate surgical management, nor as a risk factor for non-operative management failure.
The most common indication for immediate surgical management is hemodynamic instability [5, 7, 10]. In this study, we demonstrated that physiologically compromised patients (RTS < 7.8 and RR 6.2, 95% CI 1.3–30.2) and patients with associated intra-abdominal injuries required immediate surgical treatment more frequently. The association between hemodynamic instability and immediate surgical treatment may be explained by the relation of these factors with the severity of trauma. Demetriades et al. [24] demonstrated that an ISS > 15 was associated with higher mortality in general trauma patients.
In this study, ISS > 20 and RTS < 7.8 were not risk factors for non-operative management failure.
Traditionally, non-operative management has been prescribed for mild liver trauma injuries (levels I, II, and III according to the AAST) [7, 25–28]. The severity of the liver injury is an independent risk factor for the failure of non-operative management [8, 13, 14]. However, recent studies have shown successful non-operative management in patients with more severe liver injuries (levels IV and V according to the AAST) [7, 13]. Even observations in pediatric liver injuries suggest that hemodynamic instability, rather than the level of injury, should guide decisions regarding non-operative management [29]. As in other studies, we did not find an association between the severity of liver injury and the failure of non-operative management.
Velmahos et al. [19] described the presence of associated intra-abdominal injuries as a risk factor for the failure of non-operative management of blunt liver trauma. The incidence of missed intra-abdominal injuries in the non-operative management of liver trauma is between 0.5 and 3.5% [13, 15, 30]. Schnüriger et al. [7] found a higher rate of laparotomies associated with other intra-abdominal injuries rather than the severity of liver trauma. The CT scan is a reliable method for the diagnosis and follow-up of associated intra-abdominal injuries. Cox et al. suggest that a new CT scan should be performed in the case of increasing abdominal pain, a drop in hemoglobin, or liver function abnormalities [29, 31]. In our study, the frequency of associated injuries in the non-operative management group was 32.2%, and kidney trauma was the most commonly associated injury. Other intra-abdominal injuries that caused failure of non-operative management were post-traumatic pancreatitis, intra-peritoneal bladder rupture, and aortic disruption.
In conclusion, non-operative management of blunt liver trauma is the treatment of choice when an immediate intervention is not required due to hemodynamic instability or an associated intra-abdominal injury. Non-operative management of blunt liver trauma yields excellent results and is safe and effective. When performing a non-operative management, it is important to perform a strict follow-up with clinical, laboratory, and radiologic parameters of patients.
References
Trunkey DD. Hepatic trauma: contemporary management. Surg Clin North Am. 2004;84:437–50.
Kleppel NH. The genesis of nonoperative management of penetrating abdominal trauma. Arch Surg. 2004;139:800–1.
Christmas AB, Wilson AK, Manning B, Franklin GA, Miller FB, Richardson JD, et al. Selective management of blunt hepatic injuries including nonoperative management is a safe and effective strategy. Surgery. 2005;138:606–11.
Robinson WP III, Ahn J, Stiffler A, Rutherford EJ, Hurd H, Zarzaur BL, et al. Blood transfusion is an independent predictor of increased mortality in nonoperatively managed blunt hepatic and splenic injuries. J Trauma. 2005;58:437–45.
Malhotra AK, Latifi R, Fabian TC, Ivatury RR, Dhage S, Bee TK. Multiplicity of solid organ injury: influence on management and outcomes after blunt abdominal trauma. J Trauma. 2003;54:925–9.
Kozar RA, Moore JB, Niles SE, Holcomb JB, Moore EE, Cothren CC, et al. Complications of nonoperative management of high-grade blunt hepatic injuries. J Trauma. 2005;59:1066–71.
Schnüriger B, Inderbitzin D, Schafer M, Kickuth R, Exadaktylos A, Candinas D. Concomitant injuries are an important determinant of outcome of high-grade blunt hepatic trauma. Br J Surg. 2009;96:104–10.
Velmahos GC, Toutouzas KG, Radin R, Chan L, Demetriades D. Nonoperative treatment of blunt injury to solid abdominal organs: a prospective study. Arch Surg. 2003;138:844–51.
Tinkoff G, Esposito TJ, Reed J, Kilgo P, Fildes J, Pasquale M, et al. American Association for the Surgery of Trauma Organ Injury Scale I: spleen, liver, and kidney, validation based on the National Trauma Data Bank. J Am Coll Surg. 2008;207:646–55.
American College of Surgeons Committee on Trauma. Advanced Trauma Life Support for Doctors: ATLS course manual. 8th ed. Chicago: American College of Surgeons; 2008.
Hawkins ML, Wynn JJ, Schmacht DC, Medeiros RS, Gadacz TR. Nonoperative management of liver and/or splenic injuries: effect on resident surgical experience. Am Surg. 1998;64:552–6.
Scollay JM, Beard D, Smith R, McKeown D, Garden OJ, Parks RW. Eleven years of liver trauma: the Scottish experience. World J Surg. 2005;29:744–9.
Pachter HL, Knudson MM, Esrig B, Ross S, Hoyt D, Cogbill T, et al. Status of nonoperative management of blunt hepatic injuries in 1995: a multicenter experience with 404 patients. J Trauma. 1996;40:31–8.
Kozar RA, Moore FA, Cothren CC, Moore EE, Sena M, Bulger EM, et al. Risk factors for hepatic morbidity following nonoperative management: multicenter study. Arch Surg. 2006;141:451–8.
Croce MA, Fabian TC, Menke PG, Waddle-Smith L, Minard G, Kudsk KA, et al. Nonoperative management of blunt hepatic trauma is the treatment of choice for hemodynamically stable patients. Results of a prospective trial. Ann Surg. 1995;221:744–53.
Feliciano DV, Mattox KL, Jordan GL Jr, Burch JM, Bitondo CG, Cruse PA. Management of 1000 consecutive cases of hepatic trauma (1979–1984). Ann Surg. 1986;204:438–45.
Malhotra AK, Fabian TC, Croce MA, Gavin TJ, Kudsk KA, Minard G, et al. Blunt hepatic injury: a paradigm shift from operative to nonoperative management in the 1990s. Ann Surg. 2000;231(6):804–13.
Richardson JD, Franklin GA, Lukan JK, Carrillo EH, Spain DA, Miller FB, et al. Evolution in the management of hepatic trauma: a 25-year perspective. Ann Surg. 2000;232:324–30.
Velmahos GC, Toutouzas K, Radin R, Chan L, Rhee P, Tillou A, et al. High success with nonoperative management of blunt hepatic trauma: the liver is a sturdy organ. Arch Surg. 2003;138:475–81.
MacKenzie EJ, Morris JA Jr, Smith GS, Fahey M. Acute hospital costs of trauma in the United States: implications for regionalized systems of care. J Trauma. 1990;30:1096–101.
Schulman CI, Alouidor R, McKenney MG. Geriatric trauma. In: Mattox K, Feliciano D, editors. Trauma. 6th ed. New York: McGraw-Hill; 2008. p. 1004–18.
Sharma OP, Oswanski MF, Singer D, Raj SS, Daoud YAH. Assessment of nonoperative management of blunt spleen and liver trauma. Am Surg. 2005;71:379–86.
Carrillo EH, Wohltmann C, Richardson JD, Polk HC Jr. Evolution in the treatment of complex blunt liver injuries. Curr Probl Surg. 2001;38:1–60.
Demetriades D, Martin M, Salim A, Rhee P, Brown C, Doucet J, et al. Relationship between American College of Surgeons trauma center designation and mortality in patients with severe trauma (Injury Severity Score >15). J Am Coll Surg. 2006;202:212–5.
Al-Mulhim AS, Mohammad HAH. Non-operative management of blunt hepatic injury in multiply injured adult patients. Surgeon. 2003;1:81–5.
Tsugawa K, Koyanagi N, Hashizume M, Ayukawa K, Wada H, Tomikawa M, et al. Anatomic resection for severe blunt liver trauma in 100 patients: significant differences between young and elderly. World J Surg. 2002;26:544–9.
Pachter HL, Spencer FC, Hofstetter SR, Liang HG, Coppa GF. Significant trends in the treatment of hepatic trauma. Experience with 411 injuries. Ann Surg. 1992;215:492–500.
Durham RM, Buckley J, Keegan M, Fravell S, Shapiro MJ, Mazuski J. Management of blunt hepatic injuries. Am J Surg. 1992;164:477–81.
Cox JC, Fabian TC, Maish GO 3rd, Bee TK, Pritchard FE, Russ SE, et al. Routine follow-up imaging is unnecessary in the management of blunt hepatic injury. J Trauma. 2005;59:1175–80.
Miller PR, Croce MA, Bee TK, Malhotra AK, Fabian TC. Associated injuries in blunt solid organ trauma: implications for missed injury in nonoperative management. J Trauma. 2002;53:238–42.
Matthes G, Stengel D, Seifert J, Rademacher G, Mutze S, Ekkernkamp A. Blunt liver injuries in polytrauma: results from a cohort study with the regular use of whole-body helical computed tomography. World J Surg. 2003;27:1124–30.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morales, C., Barrera, L., Moreno, M. et al. Efficacy and safety of non-operative management of blunt liver trauma. Eur J Trauma Emerg Surg 37, 591–596 (2011). https://doi.org/10.1007/s00068-010-0070-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-010-0070-5