Abstract
Purpose
Osteoarthritis is a common disease, with a prevalence of symptomatic disease of 8.9%. One treatment option is radiotherapy. Most published samples were treated with an orthovoltage technique or with a telecobalt device. A lot of radiotherapy institutions are nowadays using linear accelerators for treatment of osteoarthritis. There is a discussion on whether the treatment results achieved with a linear accelerator are comparable to those with the orthovoltage technique. The aim of this study is to analyze the results of radiotherapy for osteoarthritis with a linear accelerator and compare the results with reference to different joints.
Materials and Methods
The analysis was performed in patients of two German radiotherapy institutions and included 295 irradiated joints. Pain was documented with the numeric rating scale (NRS). Evaluation of the NRS was done before and directly after each radiation therapy course as well as for the follow-up of 24 months.
The median age of the patients was 65 years, with 39.0% male and 61.0% female patients. Most frequently, osteoarthritis of the knee (34.6%) or the finger (15.9%) was treated.
Results
We could find a significant response to radiotherapy. Median pain for the whole sample was 7 on the NRS before radiotherapy, 4 after 6 weeks, and 3 after 12 and 24 months. The percentage of patients with 0 or 1 on the NRS was 33.8% 12 months after radiotherapy. All investigated subgroups had a significant reduction of pain.
Conclusion
Radiotherapy of osteoarthritis with a linear accelerator is an effective treatment which is very well tolerated. All analyzed subgroups show a good response to radiotherapy for at least 24 months. Orthovoltage therapy seems to be superior to treatment with a linear accelerator in a case-related analysis of the published samples. Further investigations should be performed for a definitive answer to this question.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis is a common disease, especially in elderly people. The prevalence of symptomatic osteoarthritis is about 8.9% among the adult population [1]. Most frequently the knee is affected, with about 6% symptomatic knee arthritis among the adult population [1, 2]. For example, for the population older than 70 years, the prevalence of knee arthritis is about 40% [2, 3]. As life expectancy is rising and the prevalence of risk factors for osteoarthritis like overweight or inactivity is growing, an increasing prevalence of osteoarthritis can be expected in the future [3].
Several therapeutic options for treatment of osteoarthritis are in use [2]. There is good evidence for arthroplasty for advanced osteoarthritis [4, 5]. For joint-conserving therapies there is not a high level of evidence [3]. Beside ice, heat, ultrasound treatment, splinting, and physiotherapy, many patients get a drug therapy. The drug therapy can be systemic, for example with NSAIDs (non-steroidal anti-inflammatory drugs), or can consist of local injections of anesthetics or steroids [6,7,8,9].
One effective non-invasive treatment for osteoarthritis is radiotherapy [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31]. Like for several other bone and joint disorders, low-dose radiation has shown an anti-inflammatory effect [10, 13, 32,33,34,35,36,37,38,39,40].
Most of the published samples were treated with orthovoltage therapy [35, 41,42,43]. Some others were irradiated with telecobalt devices or cesium devices [18, 28, 30, 44]. Only a few relatively small samples exist where patients were treated with a linear accelerator [21, 40, 45, 46]. Detailed information is missing in some of these manuscripts and the objective was different than that of our survey.
There is one retrospective trial comparing the results of orthovoltage therapy versus radiotherapy with a linear accelerator just for osteoarthritis of the knee [47]. This trial is only available in German language and has not been published in a magazine so far.
Many radiotherapy institutions do not use orthovoltage therapy anymore [48,49,50]. The therapy with telecobalt devices is obsolete in developed countries.
The objective of this survey is to document and analyze the results of radiotherapy for osteoarthritis with a linear accelerator and to compare these results with those of orthovoltage therapy.
A second ongoing discussion is whether small or large joints respond better to radiotherapy. The risk factors and etiology seem to be somewhat different [1, 51]. For this reason, the other objective of this analysis was to compare the results upon treating different joints or joint regions with radiotherapy, with the main focus on the comparison of small and large joints.
Patients and methods
The study was approved by the Ethics Committee of the University of Regensburg.
The retrospective analysis was performed on patients of two German radiotherapy institutions. We identified all patients receiving one or more courses of radiotherapy for osteoarthritis.
Radiotherapy to different joints was separated in the analysis. Some joints were cumulated to certain regions, like Heberden or Bouchard arthrosis, upper and lower ankle joint, or omarthritis and acromioclavicular arthritis.
The patients’ data from the regular follow-up were analyzed. Additionally, the patients were questioned about their current status and constantly clinically examined. We identified the etiology of the pain and registered possible risk factors for a lack of response to radiation.
Pain was documented with the numeric rating scale (NRS). Evaluation of the NRS was done before and directly after each radiation treatment as well as for the follow-up. Follow-up was done 6 weeks, 12 weeks, 6, 12, and 24 months after treatment. An arthroplasty was defined as end of follow-up.
We performed descriptive statistics, calculating median, range, and interquartile range (IQR) of NRS for all time periods. To analyze significant differences in the chronological sequence of NRS, the paired Wilcoxon test for dependent variables was used. The Mann–Whitney U test for independent variables was used for subgroup analyses and the Fisher–Yates test or chi2 test for testing of binomial variables. We postulated that p < 0.05 was significant. Statistical analyses were performed with IBM SPSS Statistics 23.0 (IBM, Armonk, NY, USA).
We defined several subgroups by gender, age (separated by the median age of 65 years), etiology, and the other parameters listed in Table 1.
Hip, knee, ankle, and shoulder were classified as large joints, whereas the finger, thumb, and big toe were categorized as small joints.
Results
In total, 159 patients could be identified, questioned, and clinically examined. 295 joints or joint regions were treated due to the fact that some patients were irradiated on more than one joint or region.
The median age of the patients was 65 years with a range from 21 to 91 years and an IQR from 56 to 73 years. 97 of the patients were female and 62 male. Most frequently patients suffered from arthritis of the knee (102 courses, 34.6%), followed by Bouchard and Heberden arthritis (47 courses, 15.9%) and arthritis of the shoulder (36 courses, 12.2%; Table 1).
94.2% of the joints were pretreated before radiotherapy. Most of the time patients had taken non-steroidal drugs for a long time, had had intraarticular injections with hyaluronidase, or had used orthoses.
The median follow-up was 19 months.
Radiotherapy was performed with a linear accelerator (Siemens Primus and Elekta Synergy) using 6‑ or 15-MV photons. Dose calculation was done to the isocentrer or middle of the joint. Joints or regions were either treated with a fractionated dose of 0.5 Gy (62 joints, 21.0%) to a total dose of 3.0 Gy (56 joints, 19.0%) or 5.0 Gy (4 joints, 1.4%) or 1.5 Gy (2 joints, 0.7%) or with a fractionated dose of 1.0 Gy (233 joints, 79.0%) to a total dose of 6.0 Gy (229 joints, 77.6%) or 5.0 Gy (3 joints, 1.0%) or 1.0 Gy (1 joint, 0.3%). In the majority of cases the treatment time was 2 weeks (median 13 days, IQR 12 to 15 days). 66 (22.4%) of the joints received a second or even third course of radiotherapy, most of the time within a 6–12-week interval after the initial radiation course.
Acute or long-term side effects did not occur in our sample.
The median pain before irradiation was 7 on the NRS (IQR 5 to 8). On the last day of radiation, the median was 5 (IQR 3 to 7) and 6 weeks after radiotherapy it was 4 (IQR 2 to 5). After 12 weeks it was 3 (IQR 1 to 5), after 6 months 3 (IQR 1 to 5.75), and after 12 and 24 months 3 (IQR 1 to 6). At the time of the last follow-up (median 19 months), NRS was 4 (IQR 2 to 7; Fig. 1).
Pain reduction compared to the pain level before irradiation was significant, with p < 0.0001 during the entire follow-up.
The pain improved continuously up to 6 months after radiotherapy (p < 0.0001).
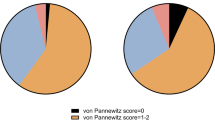
The percentage of patients being free of pain (NRS 0) or scoring pain 1 on the NRS increases with time (Fig. 2).
6 weeks after radiotherapy, 47 joints out of 288 (16.3%) scored 0 or 1 on the NRS. After 12 weeks it was 72 out of 271 joints (26.6%), after 6 months 81 out of 256 joints (31.6%), after 12 months 73 out of 216 (33.8%), and after 24 months it was 41 out of 142 joints (28.9%). Compared with the level before radiotherapy, there was a significant increase (p < 0.001 during the entire follow-up period) in the percentage of joints with no pain (NRS 0) or very little pain (NRS 1).
The general response rate was 45.7% directly after radiotherapy, 63.2% after 6 weeks, and 65.7% after 12 weeks. 6 months after radiotherapy it was 64.8%, 12 months after radiotherapy 63.4%, and 24 months after radiotherapy 64.8%, respectively.
In 32.5% of the patients no improvement of joint mobility could be detected. A distinct improvement could be achieved in 32.9% and a slight improvement of joint mobility could be achieved in 31.3% of the patients.
There was no significant difference in the remaining pain level and absence of pain for gender and age (patients older or younger than 65 years) during the entire follow-up. Male as well as female patients older and younger than 65 years (median age of our sample) had a significant reduction in pain (p < 0.0001 for all categories and the entire follow-up).
Patients were analyzed separately for different joints affected by osteoarthritis. Patients with osteoarthritis of the knee as well as patients with osteoarthritis of the shoulder or acromioclavicular joint showed positive responses to radiotherapy during the entire follow-up (p < 0.001). Patients with osteoarthritis of the hip had significant reduction of pain for the entire follow-up except at 24 months (p < 0.05).
Patients with osteoarthritis of the finger (Bouchard arthritis or Heberden arthritis) as well as patients with osteoarthritis of the base of the thumb (rhizarthritis) showed significant reduction of pain during the entire follow-up (p < 0.001). There was no significant difference for absence of pain and remaining NRS level.
Both idiopathic and secondary osteoarthritis had a significant reduction of pain (p < 0.0001 for the entire follow-up). Twelve weeks and 6 months after radiotherapy there was a significantly better pain reduction in favor of idiopathic osteoarthritis (p < 0.05).
Both large Joints and small joints had a significant reduction in pain for the entire follow-up (p < 0.0001). There was no significant difference in pain reduction for the entire follow-up. The remaining NRS level was significantly lower for small joints 12 and 24 months after radiotherapy (p < 0.05). There was no significant difference for the other times (Fig. 3).
Patients irradiated with 0.5 Gy fractionated dose to a total dose of 3 Gy had a significant response from treatment with p < 0.005 for the entire follow-up. Patients irradiated with 1.0 Gy fractionated dose to a total dose of 6 Gy also had a significant response with p < 0.0001 during the entire follow-up.
There is no significant difference in pain reduction between 3.0 Gy in 6 fractions compared to 6.0 Gy in 6 fractions. The remaining NRS level 12 weeks and 6 and 12 months after radiotherapy was worse for 6 times 1.0 Gy compared to 6 times 0.5 Gy (p < 0.05).
There was no significant difference in the long-term response (6, 12, and 24 months after completion of radiotherapy) between patients treated with one course of radiotherapy or those patients with the need for two courses of radiotherapy.
Discussion
The role of radiotherapy for osteoarthritis is under discussion [52]. Recently, two randomized trials for osteoarthritis of the knee and hand were published, both showing no significant benefit from radiotherapy [53, 54]. Despite this, there are data about measurable shrinkage of Baker’s cyst after RT for osteoarthritis of the knee, which represents a surrogate marker for the effect of RT in this indication [55].
With less than 60 patients in each study, the statistical power is somewhat limited. Furthermore, details about radiation technique, especially the machine used for treatment, are lacking and could not be inquired about.
There are many retrospective studies and some prospective studies strongly assuming radiotherapy to be an effective treatment for osteoarthritis. Beside this, there are prospective trials showing the effectiveness of low-dose radiotherapy by means of objective response criteria [55, 56]. There are many presently unanswered questions. It might be that there is a difference in response due to the use of orthovoltage therapy or a linear accelerator. Maybe just some subgroups, like for example those with activated arthrosis, have a benefit from radiotherapy. All in all, there is need for further investigation.
To our knowledge, this sample is one of the first and largest in which radiotherapy of osteoarthritis with a linear accelerator has been systematically examined. We could identify only the verifiable data of 149 patients treated with a linear accelerator, published by Kaltenborn et al., Keilholz et al., and Bartmann [40, 45, 47]. Only Bartmann investigated the problem of orthovoltage therapy versus radiotherapy with a linear accelerator. But he included only patients with knee arthritis in his survey. Besides that, the study has not yet been fully published and is available only in German language. Kaltenborn focused on rhizarthritis, and in the survey of Keilholz, only seven patients with hip arthritis had been treated with a linear accelerator.
Summarizing the patients of all published samples of radiotherapy of osteoarthritis with linear accelerators we could identify, our sample seems to be larger than the sum of all other samples.
Among other parameters, the dose rate, depth dose, and energy are different between orthovoltage devices and linear accelerator. There is a discussion on whether the published results can be transferred for treatment of osteoarthritis with a linear accelerator [57].
Nevertheless, many German radiotherapy institutions use linear accelerators for treatment of osteoarthritis. In the patterns of care analysis of 2016, only 27 institutions in Germany (23%) stated that they have the opportunity to use orthovoltage therapy. Beside this, most of the orthovoltage devices were quite old, with a median age of 17 years [58].
A retrospective comparison between orthovoltage therapy and treatment with a linear accelerator has already been done for heel spur syndrome and humeral epicondylitis. For heel spur syndrome, it was published only in German language and showed no significant difference between the groups [59]. For humeral epicondylitis, it was mainly a review of the literature, the results seeming to be superior for orthovoltage therapy [60]. Nevertheless, these results can’t easily be transferred to radiotherapy of osteoarthritis, because it is a different disease with different target volumes and target structures.
Our sample seems to be comparable to other published samples with respect to patients’ parameters. For example, the median age of 65 years is nearly equal to that of the samples of Micke et al., a clinical quality assessment (average age 63.3 years) [46]. In addition, the samples of Keilholz et al. (median age 64 years), Mahler et al. (median age 62 years), and Minten et al. (mean age 65 years) show a similar age distribution [40, 53, 54]. Also, the proportion of male to female patients with a ratio of approximately 1:2 is representative [46, 53].
The radiation technique and dose concept are equivalent to the recommended concept of the German Cooperative Group on Radiotherapy for Benign Diseases. Most of the published samples, especially the published samples of recent decades, were treated that way [61].
Radiotherapy of osteoarthritis with linear accelerators has proven beneficial to our sample. The median pain level on the NRS decreases with time and seems to reach a stable low level 6 months after the end of radiotherapy. The median follow-up of 19 months allows a statement of long-term results.
Most of the patients have a response to radiation and about one quarter of the patients are free of pain or score very low pain with NRS 1 during the long-term follow-up period. This effect lasts for at least 2 years.
The overall response rate of our sample (approximately 65%) is within the range or slightly lower than that of most other published studies (case-related average 77.7%) and seems to be comparable with the results of orthovoltage therapy.
Because of the different anatomical regions, it is difficult to give a universal recommendation for target volumes and radiation dose or technique. We used 6‑ or 15-MV photons in opposing fields or with a single field. Initially, patients were treated with 6 times 1.0 Gy in both institutions. In analogy to the data presented by Ott et al. for the radiotherapy of other non-malignant disorders, the dose concept was changed to 6 × 0.5 Gy [62,63,64]. There was a higher remaining NRS level for patients treated with 6.0 Gy in 6 fractions. Anyhow, a general recommendation cannot be given. Regarding the results of Ott et al. for other non-malignant diseases, we would rather recommend applying a fractionated dose of 0.5 Gy to a total dose of 3.0 Gy for reasons of radiation protection [62,63,64].
Whether orthovoltage therapy is superior to treatment with a linear accelerator is an interesting question. We could identify just one direct comparison of both modalities for osteoarthritis of the knee [47]. This study found no significantly different results for treatment with a linear accelerator compared to orthovoltage therapy. A slight tendency toward radiotherapy with a linear accelerator is speculated by the author. He states that it was a small sample and therefore does not have enough power to detect a difference.
For that reason, we did a case-related analysis of the published samples irradiated because of osteoarthritis. Altogether, 11,909 published patients could be identified. 9802 patients were verifiably treated with orthovoltage therapy, 429 patients (excluding our sample) were treated with photons or gamma rays (Table 2).
Most of the 429 patients were irradiated with a telecobalt or cesium device. We could identify only 149 cases, published in three samples, for which it is clearly stated that they were treated with a linear accelerator [40, 45, 47]. Detailed information is missing in some other samples [21, 46, 53, 54, 65]. We found data of complete response and partial response for 89% of all published patients. We performed statistical comparison with the chi2 test.
For all published samples in the literature the average response rate was 78%, for the joints treated with orthovoltage therapy it was 77.7%, for all other (photons and gamma ray), including our sample, it was 60%. There was a significant difference between these groups in favor of treatment with orthovoltage therapy (chi2 = 144.9). We could find a significant benefit for orthovoltage for complete response (chi2 = 56.4) and for partial response (chi2 = 30.5).
Just comparing the response rate of patients treated with orthovoltage therapy and a linear accelerator, a significant difference in favor of treatment with orthovoltage therapy can be identified for the entire time period (chi2 = 57.9).
If one just compares the newer studies since 1995 and just include patients with quite a similar dose concept to that recommended in the German guideline (fractionated dose 0.5 to 1.0 Gy and total dose 3.0 to 6.0 Gy), a significant difference (59.6% versus 64%; chi2 = 3.2) could no longer be found in the response rate between patients treated with orthovoltage (n = 1016) and photons/gamma rays (n = 444).
There are limitations to comparing all the published samples receiving radiotherapy for osteoarthritis. Beside different dose concepts, inclusion criteria, and radiation techniques, the response criteria were also different, as are the follow-up periods and the timepoints at which the response was evaluated.
Over all published samples, excluding our sample, a significant difference between the samples treated with orthovoltage therapy compared to those treated with photons or gamma rays in favor of orthovoltage therapy could be found. But less than 10% of the joints had been treated with photons or gamma rays, and it was a heterogenous group by itself. The lack of a significant difference upon comparing the newer studies since 1995 might be due to the relatively small number of cases with sufficient information in this period.
It might be interesting to conduct a prospective trial comparing orthovoltage therapy and radiotherapy with photons by a linear accelerator.
Differences between orthovoltage therapy and photon therapy are the different peak energies, dose distributions (mostly due to different absorption), and dose rates, among others. One reason for the possible superiority of orthovoltage therapy might for example be the higher absorption of X‑rays within the tissue—in particular the bone tissue—compared to photons.
Another reason might be the higher absorption in the soft tissues, with a better anti-inflammatory effect of the surrounding organs. Also, the dose rate might be one possible explanation.
Further investigations of the finding that orthovoltage therapy might be superior to photons in the radiotherapy of osteoarthritis seem to be reasonable. A prospective study to clarify a possible different effect of these modalities should be performed.
A significant difference in the response between small and large joints could not be detected. The remaining lower NRS level for small joints 12 and 24 months after radiotherapy might be random. A certain joint or joint region with clear better or worse response to radiotherapy could not be detected in our survey. It appears, that radiotherapy of osteoarthritis can be offered to patients independently of the localization of the degenerative affected joint or joint region.
Conclusion
Radiotherapy of osteoarthritis with a linear accelerator is widely used and is an effective treatment which is very well tolerated. A clear difference in the response rate between small and large joints could not be detected. All analyzed subgroups show a good response to radiation for at least 24 months. A fractionated dose of 0.5 Gy and a total dose of 3.0 Gy seem to be recommendable. Comparing treatment with a linear accelerator and orthovoltage therapy in a case-related analysis, orthovoltage therapy seems to be beneficial. Upon just comparing recent literature (since 1995), no significant difference can be detected.
References
Andrianakos AA, Kontelis LK, Karamitsos DG et al (2006) Prevalence of symptomatic knee, hand, and hip osteoarthritis in Greece. The ESORDIG study. J Rheumatol 33(12):2507–2513
Michael JW‑P, Schlüter-Brust KU, Eysel P (2010) The epidemiology, etiology, diagnosis, and treatment of osteoarthritis of the knee. Dtsch Arztebl Int 107(9):152–162
Rabenberg M (2013) Arthrose. Gesundheitsberichterstattung des Bundes vol 54. Robert Koch-Inst, Berlin
Grayson CW, Decker RC (2012) Total joint arthroplasty for persons with osteoarthritis. PM R 4(5 Suppl):97–103
Gutowski CJ, Parvizi J, Purtill JJ (2015) Protocol-based arthroplasty. Less is more. Orthopedics 38(10):631–638
Taruc-Uy RL, Lynch SA (2013) Diagnosis and treatment of osteoarthritis. Prim Care 40(4):821–836, vii
Smelter E, Hochberg MC (2013) New treatments for osteoarthritis. Curr Opin Rheumatol 25(3):310–316
Schuh A, Jezussek D, Fabijani R et al (2007) Bleiben Sie kritisch bei der Wahl Ihrer Therapie! MMW Fortschr Med 149(25–26):31–32
Rehart S, Arnold I, Fürst M (2007) Die konservative Lokaltherapie des entzündeten Gelenks. Lokal-invasive Therapieformen. Z Rheumatol 66(5):382–387
Trott KR, Parker R, Seed MP (1995) Die Wirkung von Röntgenstrahlen auf die experimentelle Arthritis der Ratte. Strahlenther Onkol 171(9):534–538
Valtonen EJ, Lilius HG, Malmio K (1975) The value of roentgen irradiation in the treatment of painful degenerative and inflammatory musculoskeletal conditions. A double-blind study. Scand J Rheumatol 4(4):247–249
Stech H (1954) Zur Frage der Röntgen-Ganzkörper-Abschnittsbestrahlung (RöGKAB.) bei gutartigen Erkrankungen (chronische Ekzeme, Heuschnupfen, Akne vulgaris, Psoriasis, endogen bedingte Arthrosen und Depressionen). Wien Klin Wochenschr 66(43):829–832
Seegenschmiedt MH, Micke O (2012) Strahlentherapie nichtmaligner Erkrankungen. Vergangenheit, Gegenwart und Zukunft. Strahlenther Onkol 188(Suppl 3):272–290
Mücke R, Seegenschmiedt MH, Heyd R et al (2010) Strahlentherapie bei schmerzhafter Kniegelenkarthrose (Gonarthrose). Ergebnisse einer deutschen Patterns-of-Care-Studie. Strahlenther Onkol 186(1):7–17
Minten MJM, Mahler E, den Broeder AA et al (2016) The efficacy and safety of low-dose radiotherapy on pain and functioning in patients with osteoarthritis. A systematic review. Rheumatol Int 36(1):133–142
Merte H, Pfab R (1995) Strahlentherapie degenerativ-entzündlicher Gelenkerkrankungen im Alter. Eine lohnende Therapiemassnahme. Fortschr Med 113(22–23):323–324
Fischer U, Kamprad F, Koch F et al (1998) Effekte einer niedrig dosierten Co-60-Bestrahlung auf den Verlauf einer aseptischen Arthritis am Kniegelenk des Kaninchens. Strahlenther Onkol 174(12):633–639
Lindner H, Freislederer R (1982) Langzeitergebnisse der Bestrahlung von degenerativen Gelenkerkrankungen. Strahlentherapie 158(4):217–223
Krautzun K, Elingshausen HP (1955) Beitrag zur Röntgentherapie der Kniegelenkarthrosen. Strahlentherapie 96(1):82–85
Kern PM (2013) Wie Strahlen gegen Entzündung wirken. MMW Fortschr Med 155(1):47–48
Keller S, Müller K, Kortmann R‑D et al (2013) Efficacy of low-dose radiotherapy in painful gonarthritis. Experiences from a retrospective East German bicenter study. Radiat Oncol 8:29
Keller HL (1974) Röntgenbestrahlung bei Arthrosis deformans. Med Klin 69(20):930
Kapatkin AS, Nordquist B, Garcia TC et al (2016) Effect of single dose radiation therapy on weight-bearing lameness in dogs with elbow osteoarthritis. Vet Comp Orthop Traumatol 29(4):338–343
Hess P, Bonmann KH (1955) Die Röntgentherapie der Arthrosen, Spondylosen, der Periarthritis humeroscapularis und der Epikondylitis. Strahlentherapie 96(1):75–81
Grosu AL (2001) Radiotherapie ausserhalb der Onkologie. Wann ist sie sinnvoll? (interview by Waltraud Paukstadt). MMW Fortschr Med 143(48):16
Gibson TJ, Winter PJ, Grahame R (1972) Radiotherapy in the treatment of osteoarthrosis of the knee. Ann Rheum Dis 31(5):423–424
Fuchs G (1951) Zur Strahlenbehandlung der Arthrosis deformans. Wien Klin Wochenschr 63(16):295–296
Keim H (1965) Mitteilung ueber die Durchfuehrung der Entzuendungsbestrahlung mit dem Telekobaltgeraet. Strahlentherapie 127:49–52
Weitmann HD, Niewald M (2013) Nicht nur bei Arthrosen erfolgversprechend. MMW Fortschr Med 155(1):43–46
Wieland C, Kuttig H (1965) Hochvolttherapie bei Arthrosen und Entzuendungen. Strahlentherapie 127:44–48
Thurmayr R, Bohmert H (1966) Zur konservativen Behandlung der Arthrosis deformans. Vergleichende Untersuchungen über die therapeutische Wirksamkeit von Eleparon und Röntgenbestrahlungen. Munchener Medizinische Wochenschrift 108(4):213–216
Schertel L, Roos A (1968) Strahlenbehandlung bei degenerativen Skeletterkrankungen? Med Klin 63(28):1112–1115
Schäfer U, Micke O, Seegenschmiedt HM et al (2010) Low-dose radiotherapy. Dtsch Arztebl Int 107(34–35):603–604
Schäfer U, Micke O, Willich N (1996) Schmerzbestrahlung bei degenerativ bedingten Skeletterkrankungen. Rontgenpraxis 49(10):251–254
Ruppert R, Seegenschmiedt MH, Sauer R (2004) Radiotherapie von Arthrosen. Indikation, Technik, klinische Ergebnisse. Orthopäde 33(1):56–62
Rossi F, Cancedda S, Leone VF et al (2018) Megavoltage radiotherapy for the treatment of degenerative joint disease in dogs. Results of a preliminary experience in an Italian radiotherapy centre. Front Vet Sci 5:74
Robson PN, van Miert PJ (1962) Treatment of osteo-arthritis of the hip by interstitial cobalt 60 irradiation. Br J Surg 49:624–636
Prokein B, Holtmann H, Hautmann MG et al (2017) Strahlentherapie des Fersensporns mit 2 Fraktionierungsschemata. Ergebnisse einer randomisierten Multizenterstudie nach 48 Wochen Follow-up. Strahlenther Onkol 193(6):483–490
von Pannewitz G (1970) Strahlentherapie der Arthrosis deformans. Technik und Ergebnisse. Radiologe 10(2):51–54
Keilholz L, Seegenschmiedt H, Sauer R (1998) Radiotherapie bei schmerzhaften degenerativ-entzündlichen Gelenkerkrankungen. Indikation, Technik und klinische Ergebnisse. Strahlenther Onkol 174(5):243–250
Schultze J (2000) Ergebnisse der Strahlentherapie degenerativer Skeletterkrankungen. Strahlenther Onkol 176(Sondernummer 1):192
Yaneva M, Vlaikova M, Dimitrova M et al (1986) X‑ray therapy in degenerative-distrophic diseases of the bones and joints. Folia Med 28(2):26–28
Keiner K, Schalldach U, Schumann E (1982) Ergebnisse der Strahlentherapie der Arthrosis deformans des Kniegelenkes. Dtsch Gesundheitsw Z Klin Med (10):445–447
Sautter-Bihl ML, Liebermeister E, Scheurig H et al (1993) Analgetische Bestrahlung degenerativentzündlicher Skeletterkrankungen. Nutzen und Risiko. Dtsch Med Wochenschr 118(14):493–498
Kaltenborn A, Bulling E, Nitsche M et al (2016) The field size matters: low dose external beam radiotherapy for thumb carpometacarpal osteoarthritis. Strahlenther Onkol 192(8):582–588
Micke O, Ugrak E, Bartmann S et al (2018) Radiotherapy for calcaneodynia, achillodynia, painful gonarthrosis, bursitis trochanterica, and painful shoulder syndrome—early and late results of a prospective clinical quality assessment. Radiat Oncol 13(1):71
Bartmann S (2016) Langzeiteffekte der niedrigdosierten Schmerzbestrahlung bei Gonarthrose und Bursitis trochanterica – Vergleich der Resultate nach bestrahlung am Linearbeschleuniger versus Orthovoltgerät. Dissertation, Ruhr-Universität Bochum, Medizinische Fakultät. https://hss-opus.ub.ruhr-uni-bochum.de/opus4/frontdoor/index/index/docId/5496
Seegenschmiedt MH, Micke O, Willich N (2004) Radiation therapy for nonmalignant diseases in Germany. Current concepts and future perspectives. Strahlenther Onkol 180(11):718–730
Seegenschmiedt MH, Katalinic A, Makoski HB et al (1999) Strahlentherapie von gutartigen Erkrankungen: eine Bestandsaufnahme für Deutschland. Strahlenther Onkol 175(11):541–547
Seegenschmiedt MH, Katalinic A, Makoski H et al (2000) Radiation therapy for benign diseases: patterns of care study in Germany. Int J Radiat Oncol Biol Phys 47(1):195–202
Arnold I (2016) Arthrose. Was gibt es Neues? Dtsch Arztebl 113(44):A-1976/B-1658/C-1645
Ott OJ, Micke O, Mücke R et al (2019) Low-dose radiotherapy. Mayday, mayday. We’ve been hit! Strahlenther Onkol 195(4):285–288
Minten MJM, Leseman-Hoogenboom MM, Kloppenburg M et al (2018) Lack of beneficial effects of low-dose radiation therapy on hand osteoarthritis symptoms and inflammation. A randomised, blinded, sham-controlled trial. Osteoarthr Cartil 26(10):1283–1290
Mahler EAM, Minten MJ, Leseman-Hoogenboom MM et al (2019) Effectiveness of low-dose radiation therapy on symptoms in patients with knee osteoarthritis. A randomised, double-blinded, sham-controlled trial. Ann Rheum Dis 78(1):83–90
Hautmann MG, Jung E‑M, Beyer LP et al (2019) Ist die Strahlentherapie eine effektive Behandlungsoption der Bakerzyste? Strahlenther Onkol 195(1):69–76
Riesterer O, Eberle B, Rogers S, Vogt DR (2019) Schmerz- und Funktionsverbesserung durch analgetische, entzündungshemmende Radiotherapie bei Patienten mit Fingerarthrosen, Epicondylitis radialis/ulnaris oder mit Fasziitis plantaris – Ergebnisse einer prospektiven single center Studie. Strahlenther Onkol 195(Suppl 1):49
Reichl B, Block A, Schäfer U et al (2015) DEGRO practical guidelines for radiotherapy of non-malignant disorders. Part I: physical principles, radiobiological mechanisms, and radiogenic risk. Strahlenther Onkol 191(9):701–709
Kriz J, Seegenschmiedt HM, Bartels A et al (2018) Updated strategies in the treatment of benign diseases‑a patterns of care study of the german cooperative group on benign diseases. Advances in Radiation Oncology 3(3):240–244
Schlöcker I (2008) Vergleich der Wirksamkeit von Orthovoltbestrahlung und Hochvoltbestrahlung bei schmerzhaftem Fersensporn (FS) anhand des Parameters Schmerzbefreiung. doctoral thesis, Universität Halle. https://sundoc.bibliothek.uni-halle.de/diss-online/08/08H107/of_index.htm
Hautmann MG, Beyer LP, Süß C et al (2019) Strahlentherapie der Epicondylitis humeri. Analyse von 138 mit Linearbeschleuniger bestrahlten Ellenbogen. Strahlenther Onkol 195(4):343–351
Ott OJ, Niewald M, Weitmann H‑D et al (2015) DEGRO guidelines for the radiotherapy of non-malignant disorders. Part II. Painful degenerative skeletal disorders. Strahlenther Onkol 191(1):1–6
Ott OJ, Jeremias C, Gaipl US et al (2015) Radiotherapy for benign achillodynia. Long-term results of the Erlangen Dose Optimization Trial. Strahlenther Onkol 191(12):979–984
Ott OJ, Hertel S, Gaipl US et al (2014) The Erlangen Dose Optimization Trial for radiotherapy of benign painful shoulder syndrome. Long-term results. Strahlenther Onkol 190(4):394–398
Ott OJ, Hertel S, Gaipl US et al (2014) The Erlangen Dose Optimization Trial for low-dose radiotherapy of benign painful elbow syndrome. Long-term results. Strahlenther Onkol 190(3):293–297
Wieland C (1966) Indikationsstellung und Ergebnisse der Strahlentherapie bei Arthrosen. Z Rheumaforsch 25(9):324–329
Heidenhein L (1923) Über die Arthritis senilis bilateralis symetrica. Langenbecks Arch Klin Chir 127:514–528
Kreuzwald T (1926) Röntgenbestrahlung der Arthristis deformans. Fortschr Röntgenstr 35:102
Kahlmeter G, Åkerlund Å (1930) The roentgen treatment of arthritis. Acta Medica Scandinavica https://doi.org/10.1111/j.0954-6820.1930.tb14931.x
Fried G (1934) Die Röntgentherapie der Arthritis. Strahlenther 49:634–675
(1939) Über die Röntgenbehandlung chronischer unspezifischer Gelenkleiden. Acta radiologica 20:357–364
Toschke G (1941) Zur Röntgenbehandlung von Gelenkerkrankungen. Strahlenther 70:443–456
Cocchi U (1943) Erfolge und Mißerfolge bei der Röntgenbestrahlung nicht krebsiger Leiden. I. gutartige nicht tuberkulöse nicht aktinomykotische Prozesse. Strahlenther 73:255–305
Reichel WS (1949) Radiotherapy for pain. Strahlentherapie. 80(4):483–534
Glauner R (1951) Die Entzündungs-Bestrahlung. Stuttgart: Thieme
Pape R, Gölles D (1954) Direkte und indirekte Röntgentherapie bei Gelenkserkrankungen. Radiol Aust 6:245–254
Hess P, Bonmann KH (1955) Roentgen therapy of arthroses, spondyloses, periarthritis humeroscapularis and epiconsylitis. Strahlentherapie 96(1):75–81
Geyer E, Landgraf K (1955) Results of radiotherapy and ultrasonic therapy in 1000 cases of arthrosis deformans of the knee. Z Arztl Fortbild (Jena) 49(8):273–6
Pizon P (1957) La roentgenthérapie des affections rhumatismales. Mason & Cie, Paris, p 142–143
Murley AH (1957) Results of radiotherapy in osteo-arthritis of the hip. Lancet 272(6973):818–819
Barth G, Kern W, Schnoeckel F (1961) Results of roentgen irradiation in arthrosis deformans. Med Welt 11:506–509
Thurmayr R, Bohmert H (1966) On the conservative treatment of arthrosis deformans. Comparative studies on the therapeutic effectiveness of Eleparon and radiotherapy. Munch Med Wochenschr 108(4):213–216
Mitrov G, Harbov I (1967) Our experiences with radiation treatment of non-tumorous diseases. Radiobiol Radiother (Berl) 8(4):419–422
Schertel L, Roos A (1968) Radiotherapy in degenerative skeletal diseases. Med Klin 63(28):1112–1115
Goldie I, Rosengren B, Moberg E, et al (1970) Evaluation of the radiation treatment of painful conditions of the locomotor system. Acta Radiol Ther Phys Biol 9:311–322
Grasshoff H (1971) Results of x-ray treatment in cox- and gonarthroses. Beitr Orthop Traumatol 18(2):72
Zschache H (1972) Results of low-intensity roentgen irradiation. Radiol Diagn (Berl) 13(2):181–186
Hartweg H, Faust H, Renner K, Renner H (1973) Radiotherapy of gonarthrosis. Strahlentherapie 145(4):373–7
Hassenstein E, Nüsslin F, Renner K. (1974) Radiation treatment of coxarthrosis (author’s transl). Strahlentherapie 147(3):213–218
(1976) Radiotherapy of inflammatory diseases – indicated still today? Med Klin 71(26):1117–1119
Lindner H, Freislederer R. (1982) Long term results of radiotherapy of degenerative joint diseases (author’s transl). Strahlentherapie 158(4):217–223
Gärtner C, Schüttauf M, Below M, Motorina LI, Michina ZP (1988) The radiotherapeutic treatment of chronically relapsing, degenerative skeletal changes at the Oncology Clinic (Charité) [Article in German]. Radiobiol Radiother (Berl) 29(6):689–698
Merte H, Pfab R (1995) Radiotherapy of degenerative inflammatory joint diseases in the elderly. A worthwhile therapeutic measure. Fortschr Med 113(22–23):323–324
Glatzel M, Fröhlich D, Bäsecke S, et al. (2004) Ergebnisse der Strahlentherapie der Gonarthrose. Strahlenther Onkol 177(Sondernr. 1):27
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M.G. Hautmann, P. Rechner, U. Neumaier, C. Süß, B. Dietl, F.J. Putz, M. Behr, O. Kölbl, and F. Steger declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Hautmann, M.G., Rechner, P., Neumaier, U. et al. Radiotherapy for osteoarthritis—an analysis of 295 joints treated with a linear accelerator. Strahlenther Onkol 196, 715–724 (2020). https://doi.org/10.1007/s00066-019-01563-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-019-01563-1