Abstract
Purpose
Modern impartation of both anatomic and radiation oncology (RO) knowledge in medical education enables a transfer of preclinical knowledge to clinical practice, which may be addressed by multidisciplinary concepts. The faculty’s “Anatomy and imaging” course attempts to integrate RO, radiology and nuclear medicine into the preclinical curriculum. The present analysis focuses on the description of the course concept and discusses the potential didactic impact of the implementation of RO.
Methods
In total 5 semester cohorts have undertaken the course since the introduction of RO in the winter semester of 2015/2016 with 682 students participating. It is designed as a small group circuit training with a teaching content of 8 h daily. Course evaluation was performed on a 100-item Likert scale.
Results
General evaluation showed an average of 9.3–12.7 on a Likert scale (0 being the best, 100 being the worst grade). Use of media, relevance for medical training, gain of interest in medicine in general and overall satisfaction with the course received excellent mean values. For RO, there was a high degree of consent with the following statements: “the course was well organized”, “subjects and presentation were well-structured”, “topics were well chosen”, “the time for exercises was sufficient” and “teaching by student tutors and physicians was adequate”.
Conclusion
The present evaluation demonstrates the feasibility of introducing RO in the preclinical part of medical education. The course concept shows excellent results in evaluation and may help in broadening RO knowledge and in recruiting new doctoral candidates and residents.
Zusammenfassung
Ziel
Die moderne Vermittlung von anatomischen und radioonkologischem (RO) Lehrinhalten schafft eine Verknüpfung von präklinischem und klinischem Wissen, was in Form interdisziplinärer Konzepte gelingen kann. Der Kurs „Anatomie und Bildgebung“ integriert RO, Radiologie und Nuklearmedizin in das präklinische Curriculum. Die vorliegende Analyse liefert eine Beschreibung des Kurskonzeptes und diskutiert die potentiellen didaktischen Auswirkungen der Implementierung der RO.
Methodik
Insgesamt durchliefen 5 Semesterkohorten mit 682 Studierenden den Kurs seit der Einführung der RO im Wintersemester 2015/2016. Der Kurs ist als Kleingruppenunterricht im Sinne eines Zirkeltrainings aufgebaut mit 8 Lehrmodulen täglich. Die Kursevaluation fand mittels einer 100-Punkt Likert-Skala statt.
Ergebnisse
Die Gesamtevaluation zeigte einen Durchschnittswert von 9,3–12,7 auf der Likert-Skala (0 als beste, 100 als schlechteste Note). Der Medieneinsatz, die Relevanz für die spätere ärztliche Tätigkeit, die Steigerung des Interesses am Studienfach Medizin sowie die Zufriedenheit mit dem Kurs wurden sehr gut bewertet. Für die RO bestand ein hoher Konsens mit den Aussagen: „Das Lehrmodul war gut organisiert“. „Lehrstoff und Präsentation waren gut strukturiert“. „Die Themen waren gut ausgewählt“. „Die Übungszeit war ausreichend“. „Die Vermittlung durch studentische Tutoren und Ärzte war adäquat“.
Schlussfolgerung
Die vorliegende Auswertung zeigt die Möglichkeit auf, die RO in die präklinische Lehre zu integrieren. Das Konzept weist exzellente Evaluationsergebnisse auf und kann dazu beitragen RO Wissen zu vermitteln und potentielle neue Doktoranden und Assistenzärztinnen und -ärzte zu rekrutieren.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Cancer is a key factor for both national and international disease burden. In Germany, approximately 475,000 individuals are diagnosed with cancer every year. [1]. Although German and American databases describe decreasing age-adjusted incidence rates for cancer in males, the German Robert-Koch Institute points out an overall increase in prevalence due to demographic changes [1, 2]. Therefore, integrating oncology education into the medical school curriculum with classes covering radiation oncology (RO) is of major importance. Considering RO, anatomical knowledge is pivotal to enable precise and correct contouring of target volumes and organs at risk. The interobserver variability in contouring/defining target volumes is considerable even among experts and may endanger sufficient dose coverage [3,4,5]. Consistently, a recent survey of the working group “youngDEGRO” of the German Society of Radiation Oncology uncovered a deficit in contouring skills with >40% of residents having only “mediocre” or “poor” competence [6]. These parallel needs both for anatomical and RO knowledge in medical education may be addressed by multidisciplinary concepts, which have been elaborated for medical disciplines such as surgery and radiology [7,8,9,10]. Established in 2001, this faculty’s “Anatomy and imaging” course has a long history of connecting preclinical and clinical subjects, thus enabling the students to transfer first or second year anatomical knowledge to clinical practice. The present analysis focuses on the description of the course concept and discusses potential didactic impact of the implementation of RO.
Material and methods
The course “Anatomy and imaging” is a compulsory preclinical course. It takes place at the end of the third semester covering 4 days with 8 h of tutoring per day. Organization and examination are within the responsibility of the Institute of Anatomy with participation of physicians from the departments of radiology, nuclear medicine and RO. Each day is designed as a circuit training with 8 modules per day. All 140 of the 2nd year students are divided into small groups (maximum 10 students) and are taught by 20 specialized student tutors, supervised by 7 lecturers. RO forms an integral part of the X‑ray and computed tomography (CT) modules. For the sake of clarity, the following description will focus on these lessons, whereas details on other modules are explained in detail elsewhere [10, 11].
An introductory lecture presents the basic principles of RO, e.g. interaction on the DNA level, fractionation concepts and their rationale, as well as the distinction between curative and palliative regimes. Afterwards, each RO session starts with a short repetition of physiological anatomy, subsequently transferring this knowledge to imaging modalities as X‑ray, CT and magnetic resonance imaging (MRI). Small group size and interactive presentation with tablet-based projection assist the individual learning process.
Day 1—Skeleton/bone metastases—55 min
The introduction of conventional X‑ray images and CT scans of the spine forms the cornerstone of this module. With an interactive case of a breast cancer patient suffering from bone metastases, the students are confronted with a typical palliative indication for radiotherapy (RT). The main goal is to find and to describe pathological findings compared to physiological anatomy, to list potential differential diagnoses and to identify the correct imaging modalities for further diagnostic steps. The radiation oncologist then underlines the importance of RT in this situation aiming at pain relief and stabilization.
Day 2—thorax/superior vena cava syndrome—115 min
On day 2, the complex intrathoracic anatomy is demonstrated on X‑ray and CT with special emphasis on the heart and mediastinal structures. The theory part focuses on topographic anatomy and explains windowing of CT scans. Afterwards, the superior vena cava syndrome illustrates the use of RT in an emergency situation with demonstration of radiation techniques, adaptive planning due to tumor shrinkage as well as general principles of emergency management in RO.
Day 3—abdomen/stereotactic body irradiation—115 min
The third day concentrates on abdominal anatomy with the gastrointestinal and urogenital tract as well as the liver and biliary tract. After having successfully mastered the identification of anatomical structures on an abdominal and pelvic CT scan, the RO part demonstrates a stereotactic body irradiation of the liver. This part discusses radiosurgery/high-precision RT, the challenge to overcome intrathoracic/abdominal movements (tracking, gating, 4D-CT) and further elaborates intensity-modulated RT.
Day 4—central nervous system/combined chemoradiotherapy for glioma—55 min
The course concludes with neuroanatomy, which is subdivided in cerebral bleeding, cerebrospinal fluid system and bone anatomy. As a pathological case, the radiation oncologist presents a high-grade glioma with combined chemoradiotherapy. The module introduces the basis of a combined modality treatment (synergistic effect with increased toxicity) and shows modern RT planning via image fusion with MRI.
Course evaluation and subsequent performance-based allocation of funds are compulsory for all lectures, seminars and practical training sessions at the faculty since 2002. Evaluation is performed on a 100-point Likert scale (with 100 being the worst grade). Additionally, a more detailed questionnaire is used, which was especially developed for “Anatomy and imaging” in 2001 (5-point Likert scale; 1: fully applies—5: does not apply at all).
Results
In total, 5 semester cohorts undertook the course since the introduction of RO in the winter semester of 2015/2016 with 682 students in total (133, 130, 148, 133, 138 students for each semester cohort). Among these, 230 were male and 438 were female (14 missing data). In the general evaluation “Anatomy and imaging” obtained an average of 9.3–12.7 (median: 6.0–10.0) on the 100-point Likert scale (0 being the best, 100 being the worst grade; Table 1).
Use of media (1.2–1.4), relevance for medical training (1.2–1.4), gain of interest in medicine in general (1.3–1.4) and overall satisfaction with the course (1.3–1.5) received excellent mean values (median did not apply, as it was 1.0 in all categories). For RO, the following statements were examined:
“The course was well organized”, “subjects and presentation were well-structured”, “topics were well chosen”, “the time for exercises was sufficient” and “teaching by student tutors and physicians was adequate”. Median results were 1.4, 1.5, 1.5, 1.6 and 1.4, respectively (Table 2 for details).
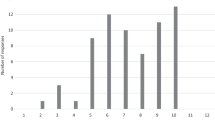
In comparison to other courses at the faculty, “Anatomy and imaging” showed superior evaluation (Fig. 1). Based on a 100-point Likert scale, mean evaluation values for seminars, practical training and all faculty courses ranged between 25.2–33.3, 22.3–28.2 and 26.6–31.5, respectively whereas “Anatomy and imaging” achieved a value between 9.3–15.4 in the last years (evaluation includes semesters before the integration of RO).
Discussion
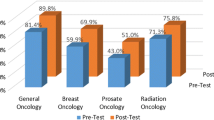
Integration of RO into the preclinical (anatomical) curriculum has been performed for the first time in Germany. Excellent results in the quality of teaching can consistently be observed and favor a multidisciplinary learning. One attempt of teaching both subjects is to integrate anatomy into the clinical , e.g. by educating physicians and medical students with a focused clinical dissection course [12]. As suggested by Dettmer et al. clinical anatomy courses may also help to highlight the key (and therefore important) anatomical structures rather than presenting details from the anatomy atlas [8]. Anyhow, this “top-down approach”, which rather refreshes former anatomical knowledge, may be impeded by its late onset. In contrast, introducing RO within the first years of medical studies may be favorable, avoiding misconceptions about the subject. It will also help to recruit potential doctoral candidates and residents. Incorrect ideas about RO are frequent, especially for first year medical students concerning the ability of RO to treat and cure cancer [13]. For example, only 29% of first year medical students and 53% of fourth year students could identify RT as part of the treatment for superior vena cava syndrome [13]. Despite an overall increase in knowledge during the medical education, common misbeliefs persist after examinations and are found (significantly) less often in those students with a RO rotation [13]. As a practical rotation is not feasible for all students and elective courses for a small number of students might not be sufficient [8, 10], presenting core principles of RO within the curriculum is crucial. In addition, the quality of education is one of the cardinal aspects for choosing RO residency [14]; however, RO concepts for undergraduate students are rare (see [15] for review) with only very few examples of integrated anatomy-RO lessons. After a preclinical oncology course led by a radiation oncologist, >70% of participants found this concept helpful to introduce principles of cancer therapy and multidisciplinary cancer management [16]. With the addition of a clinical didactic session, knowledge in RO in general but also in breast and prostate cancer could be significantly enhanced [17]. Furthermore, the implementation of a structured curriculum for clerkships significantly improves knowledge in RO [18].
Global trends in medical education see a shift from knowledge accumulation to competence-based learning which meets the need of the younger generation for personalized learning, interconnectivity and teamwork as well as transparency [19, 20]. In Germany, the ongoing “Masterplan Medizinstudium 2020” will profoundly restructure medical studies towards a practical, competence-based education [21, 22] demanding longitudinal as well as interdisciplinary concepts, of which “Anatomy and imaging” is an example. This process will require radiology, nuclear medicine and RO to develop coordinated national curricula, which have been prepared by the respective German societies [23,24,25]. In addition, the German Society of Radiation Oncology (DEGRO) has emphasized the importance of education by the establishment of a new working group redefining standardized learning objectives and key abilities in RO for future physicians. Soon, an interdisciplinary dialogue with the surgical disciplines, internal medicine, neurology etc. will be initiated, elaborating a distinctive clinical curriculum with key aspects of RO.
Concerning our institution, “Anatomy and imaging” forms the beginning of the department’s longitudinal curriculum or learning spiral, which finally leads to RO competence. The course is continued by introductory lectures and a first clinical course in the fifth semester (the first clinical semester) in which oncological anamnesis and therapeutic management are taught. In subsequent semesters, lectures on RO are organ-specific (e.g. thoracic, gastrointestinal, hematologic malignancies). Ongoing efforts for improvement are made by mapping of standardized milestones and learning objectives in accordance with the national competence-based catalogue of learning objectives [26]. This implements specific learning objectives for RO.
One major limitation of the present analysis is the lack of specific evaluation of RO knowledge pre-course and post-course, which makes the quantification of students’ knowledge gain troublesome. To address this drawback, a detailed evaluation form, as proposed by Zaorsky et al. [13], seems adequate. Zaorsky et al. introduced a multi-item evaluation for students, in which questions concerning RO job description, appropriateness of RT for different cancer types/treatment and RO toxicities must be answered by first and fourth year medical students with “yes” or “no”. A shortened version may result in a more precise evaluation and definition of learning objectives.
It has to be kept in mind that the present data include only a limited period of time so far and that the outstanding results are to be periodically re-evaluated. Nevertheless, “Anatomy and imaging” has a longstanding history at our faculty with consistently good evaluations [10, 11]. In comparison to other seminars and lectures (Fig. 1), the concept received a median evaluation of 9.3–12.7, making it the (second) best seminary format. Interestingly, neither anatomy nor any clinical seminar of radiology, nuclear medicine or RO achieves a comparable evaluation (data not shown), which emphasizes the efficiency and attractiveness of interdisciplinary learning. It has to be mentioned that these excellent results have persisted after the transformation of the course from an elective to a curricular concept. It is most unlikely to expect deterioration in the years to come.
Another aspect to be considered is the high personal need for performance of the course, involving 5 physicians and 2 scientists from the Institute of Anatomy. German regulations require 1 lecturer per 20 students, thus demanding 7 lecturers for 140 students. Small group teaching is enabled by the involvement of more than 20 specialized student tutors. The employment of peer tutors has shown to ensure equal test results in evaluation of a problem-based learning format in comparison to graduate teachers [27]. Anyhow, the concentrated 1‑week structure may be an opportunity for the teaching staff to full dedication to the course, which is rarely possible during regular working hours. Another survey of the youngDEGRO unveiled that only 21% of young radiation oncologists consented to the possibility of integrating teaching within the working hours [28]. The motivation and dedication of the teaching staff is probably one reason for the high quality and excellent evaluation results. The students’ free text commentaries reflect a high degree of recognition and appreciation for the personal involvement as well as the favorable physician/peer tutor to student ratio. In the end, the greatest challenge, as postulated by Evans and Watt, remains: finding the right mixture between clinical and preclinical subjects [29].
Conclusion
The present evaluation demonstrates the feasibility of introducing radiation oncology into the preclinical part of medical education. The course concept is highly accepted, shows excellent evaluation results and may help in broadening RO knowledge and to recruit new doctoral candidates and residents.
References
Robert Koch-Institut (2017) Krebs in Deutschland für 2013/2014 https://doi.org/10.17886/rkipubl-2017-007
Cronin KA, Lake AJ, Scott S et al (2018) Annual Report to the Nation on the Status of Cancer, part I: National cancer statistics: Annual Report National Cancer Statistics. Cancer 124:2785–2800. https://doi.org/10.1002/cncr.31551
Kim YS, Kim JW, Yoon WS et al (2016) Interobserver variability in gross tumor volume delineation for hepatocellular carcinoma: Results of Korean Radiation Oncology Group 1207 study. Strahlenther Onkol 192:714–721. https://doi.org/10.1007/s00066-016-1028-2
Schimek-Jasch T, Troost EGC, Rücker G et al (2015) A teaching intervention in a contouring dummy run improved target volume delineation in locally advanced non-small cell lung cancer: Reducing the interobserver variability in multicentre clinical studies. Strahlenther Onkol 191:525–533. https://doi.org/10.1007/s00066-015-0812-8
Spoelstra FO, Senan S, Le Péchoux C et al (2010) Variations in target volume definition for postoperative radiotherapy in stage III non-small-cell lung cancer: Analysis of an international contouring study. Int J Radiat Oncol Biol Phys 76:1106–1113. https://doi.org/10.1016/j.ijrobp.2009.02.072
Dietzel CT, Jablonska K, Niyazi M et al (2018) Quality of training in radiation oncology in Germany: Where do we stand? Strahlenther Onkol 194:293–302. https://doi.org/10.1007/s00066-017-1250-6
Dettmer S, Tschernig T, Galanski M et al (2010) Teaching surgery, radiology and anatomy together: The mix enhances motivation and comprehension. Surg Radiol Anat 32:791–795. https://doi.org/10.1007/s00276-010-0694-5
Dettmer S, Schmiedl A, Meyer S et al (2013) Radiological anatomy—Evaluation of integrative education in radiology. Rofo 185:838–843. https://doi.org/10.1055/s-0033-1335048
Rengier F, Doll S, von Tengg-Kobligk H et al (2009) Integrated teaching of anatomy and radiology using three-dimensional image post-processing. Eur Radiol 19:2870–2877. https://doi.org/10.1007/s00330-009-1507-2
Schober A, Pieper C, Schmidt R, Wittkowski W (2013) “Anatomy and Imaging”: 10 years of experience with an interdisciplinary teaching project in preclinical medical education—From an elective to a curricular course. Rofo 186:458–465. https://doi.org/10.1055/s-0033-1355567
Schober A, Schmitz M, Zimmer S, Schmidt R, Oertel M, Vrachimis A, Marschall B (2017) Vom Know-what zum Know-how – 15 Jahre „Anatomie und Bildgebung“. Joint Congress of the Gesellschaft für Medizinische Ausbildung (GMA) and the Arbeitskreis zur Weiterentwicklung der Lehre in der Zahnmedizin (AKWLZ), Münster, 20.–23.09.2017
Zumwalt AC, Marks L, Halperin EC (2007) Integrating gross anatomy into a clinical oncology curriculum: The oncoanatomy course at Duke University School of Medicine. Acad Med 82(5):469–474. https://doi.org/10.1097/ACM.0b013e31803ea96a
Zaorsky NG, Shaikh T, Handorf E et al (2016) What are medical students in the United States learning about radiation oncology? Results of a multi-institutional survey. Int J Radiat Oncol Biol Phys 94(2):235–242. https://doi.org/10.1016/j.ijrobp.2015.10.008
Brower JV, Mohindra P, Bradley KA, Golden DW (2014) Radiation oncology residency selection: A targeted assessment of factor importance among fourth-year medical students. Int J Radiat Oncol Biol Phys 88:967–968. https://doi.org/10.1016/j.ijrobp.2013.12.020
Dennis KEB, Duncan G (2010) Radiation oncology in undergraduate medical education: A literature review. Int J Radiat Oncol Biol Phys 76(3):649–655. https://doi.org/10.1016/j.ijrobp.2009.08.038
Agarwal A, Koottappillil B, Shah B et al (2015) Medical student—Reported outcomes of a radiation oncologist—Led preclinical course in oncology: A five-year analysis. Int J Radiat Oncol Biol Phys 92(4):735–739. https://doi.org/10.1016/j.ijrobp.2015.03.008
Agarwal A, Shah A, Shah B et al (2017) The impact of a radiation oncologist led oncology curriculum on medical student knowledge. J Cancer Educ. https://doi.org/10.1007/s13187-017-1227-2
Golden DW, Kauffmann GE, McKillip RP et al (2018) Objective evaluation of a didactic curriculum for the radiation oncology medical student clerkship. Int J Radiat Oncol Biol Phys 101:1039–1045. https://doi.org/10.1016/j.ijrobp.2018.04.052
Carraccio CL, Englander R (2013) From Flexner to competencies: Reflections on a decade and the journey ahead. Acad Med 88:1067–1073. https://doi.org/10.1097/ACM.0b013e318299396f
Desy JR, Reed DA, Wolanskyj AP (2017) Milestones and millennials: A perfect pairing-competency-based medical education and the learning preferences of Generation Y. Mayo Clin Proc 92:243–250. https://doi.org/10.1016/j.mayocp.2016.10.026
Bundesministerium für Bildung und Forschung (2017) Masterplan Medizinstudium 2020
Jünger J (2018) Competence-based assessment in the national licensing examination in Germany. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 61:171–177. https://doi.org/10.1007/s00103-017-2668-9
Akademie der DEGRO (2016) Curriculum zur Weiterbildung zum „Facharzt für Strahlentherapie“ der Akademie der „Deutschen Gesellschaft fur Radioonkologie’(DEGRO) zur ’Fort- und Weiterbildung in der Radioonkologie“
Ertl-Wagner B, Barkhausen J, Mahnken AH et al (2016) White paper: Radiological curriculum for undergraduate medical education in Germany. Rofo 188:1017–1023. https://doi.org/10.1055/s-0042-116026
Marienhagen J, Brenner W, Buck A et al (2018) Development of a national competency-based learning objective catalogue for undergraduate medical education in Germany. Nuklearmedizin 57(04):137–145. https://doi.org/10.3413/Nukmed-0969-18-03
MFT Medizinischer Fakultätentag der Bundesrepublik Deutschland e. V. (2015) Nationaler Kompetenzbasierter Lernzielkatalog Medizin (NKLM)
Matthes J, Marxen B, Linke R‑M et al (2002) The influence of tutor qualification on the process and outcome of learning in a problem-based course of basic medical pharmacology. Naunyn Schmiedebergs Arch Pharmacol 366:58–63. https://doi.org/10.1007/s00210-002-0551-0
Krug D, Baumann R, Rieckmann T et al (2016) Situation of young radiation oncologists, medical physicists and radiation biologists in German-speaking countries: Results from a web-based survey of the Young DEGRO working group. Strahlenther Onkol 192:507–515. https://doi.org/10.1007/s00066-016-1003-y
Evans DJ, Watt DJ (2005) Provision of anatomical teaching in a new British medical school: Getting the right mix. Anat Rec B New Anat 284:22–27. https://doi.org/10.1002/ar.b.20065
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Oertel, M. Schmitz, J.C. Becker, H.T. Eich and A. Schober declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Oertel, M., Schmitz, M., Becker, J.C. et al. Successful integration of radiation oncology in preclinical medical education. Strahlenther Onkol 195, 1104–1109 (2019). https://doi.org/10.1007/s00066-019-01492-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-019-01492-z