Abstract
Purpose
The aim of this study was to evaluate prognostic factors in patients with lung metastases who undergo lung stereotactic body radiotherapy (SBRT).
Materials and methods
A total of 87 patients with 129 lung metastases who underwent SBRT between November 2004 and May 2012 were enrolled in this retrospective study. The patient collective consisted of 54 men (62.1%) and 33 women (37.9%); the median age was 65 years (range 36–88). The Karnofsky performance index was ≥70% (median 90%) for all cases, but one (60%). Adverse effects were categorized using the CTCAE 4.0 classification system. Retrospective analyses regarding patients’ characteristics, progression-free survival (PFS), overall survival (OS), disease-specific survival (DSS), and local tumor control rates (LTC) were performed.
Results
On univariate and multivariate analysis OS, DSS, and PFS were significantly (p < 0.05) better for patients with ≤3 lung metastases; no extrathoracic metastases at the time of the SBRT; a gross tumor volume (GTV) <7.7 cm3 and patients that received a staging that included positron emission tomography with fluorine 18 fluorodeoxyglucose/computed tomography (FDG-PET/CT) imaging. Furthermore, a longer OS was observed if newly diagnosed metastases during follow-up were limited to the lung (median survival: 43.7 months versus 21.7 months; p = 0.023).
Conclusion
The number and pattern of metastases, and the size of the target volume are strong predictors for the outcome of patients receiving SBRT of lung tumors. FDG-PET/CT should be part of pretherapeutic staging before SBRT.
Zusammenfassung
Hintergrund
Ziel dieser Studie war es, prognostische Faktoren bei Patienten mit Lungenmetastasen zu evaluieren, die mit einer stereotaktischen Strahlentherapie (SBRT) behandelt wurden.
Material und Methoden
In dieser retrospektiven Studie wurden 87 Patienten mit insgesamt 129 Lungenmetastasen, die zwischen November 2004 und Mai 2012 in unserem Institut mit einer SBRT behandelt wurden, untersucht. Das Patientenkollektiv setzte sich aus 54 Männern (62,1%) und 33 Frauen (37,9%) zusammen; das mediane Alter betrug 65 Jahre (Spanne 36–88 Jahre). Mit einer Ausnahme (60%) war der Karnofsky-Index ≥70% (median 90%). Die Nebenwirkungen wurden entsprechend CTCAE V. 4.0. klassifiziert. Das progressionsfreie Überleben (PFÜ), das Gesamtüberleben (GÜ), das krankheitsspezifische Überleben (KSÜ) und die lokale Tumorkontrolle (LTK) wurden unter Berücksichtigung prognostischer Einflussfaktoren analysiert.
Ergebnisse
Patienten mit maximal 3 Lungenmetastasen ohne extrathorakale Metastasierung mit einem Gesamttumorvolumen (GTV) <7,7 cm3 und Patienten, die ein Staging mittels FDG-PET (18 Fluordesoxyglukose-Positronenemissionstomographie) vor Beginn der Behandlung erhalten hatten, zeigten ein signifikant längeres GÜ, PFÜ und KSÜ. Des Weiteren wurde für Patienten, bei denen neue Metastasen während des Follow-ups auf die Lunge begrenzt waren, ein längeres GÜ verzeichnet (median: 43,7 Monate vs. 21,7 Monate; p = 0,023)
Schlussfolgerung
Die Anzahl der Metastasen, das Metastasierungsmuster und die Größe des Zielvolumens sind wesentliche Prädiktoren hinsichtlich der Prognose bei der SBRT von Lungentumoren. Ein FDG-PET ist ein wichtiger Bestandteil des prätherapeutischen Stagings vor SBRT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The lung is a predominant target organ for metastases. Up to 54% of patients suffering from cancer develop lung metastases [1]. The prognosis and treatment of patients with pulmonary metastases hinges on the number of metastatic sites in the lung. While most patients with multiple pulmonary lesions are systemically treated, patients with oligometastatic diseases (OM) profit from a localized therapy [1,2,3,4,5]. Although surgical resection counts as the gold standard, stereotactic body radiotherapy (SBRT) has become established in recent years as a valid alternative for the treatment of OM including metastases in the lung. SBRT delivers high-dose hypofractionated radiotherapy to targets with sparing of surrounding normal tissues. Recent studies performing SBRT showed good local tumor control (LTC) rates and a low incidence of severe (grade 3–5) toxicities [4, 6,7,8,9,10]. However, the outcome varies widely among the patients included in these studies. Even though some prognostic factors have been mentioned in the previous literature, studies addressing this topic directly to confirm and to complete the current knowledge are lacking. This study was performed to evaluate prognostic factors that can be derived from pretherapeutic staging and restaging after SBRT.
Materials and methods
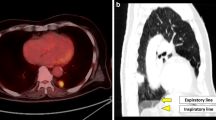
A total of 87 patients with a total of 129 lung metastases who underwent SBRT between November 2004 and May 2012 were enrolled in this retrospective study. The patient collective consisted of 54 men (62.1%) and 33 women (37.9%), whose median age was 65 years (range 36–88). The Karnofsky performance index was ≥70% (median 90%) except in one case (60%). The patients’ characteristics are summarized in Table 1. Immobilization was achieved with a vacuum couch and low pressure foil (Medical Intelligence GmbH, Schwabmünchen, Germany). During irradiation the patients received oxygen supply to further reduce respiratory movement. Before 2008 breathing motion was taken into account by sequential computed tomography (CT) scans for treatment planning and before each applied fraction with a slow, single-slice CT scan to derive an individual margin for each patient which was complemented by an additional margin of 10 mm in longitudinal and 5 mm in axial direction to derive the planning target volume. After 2008 4D-CT was performed. Setup verification was accomplished in most cases (61.2%) by on board cone beam CT (CBCT). Patients treated earlier than July 2008 received a conventional CT in treatment position and were transferred to the accelerator after stereotactic correction of treatment position. Before 2008, treatment plans were planned with a type A algorithm, afterwards with type B.
The prescribed total dose ranged between 14 and 45 Gy (median 35 Gy) on the 60% isodose, given mainly in 3 (n = 51) or 5 (n = 40) fractions. Most common dose prescriptions were 37.5 Gy in 3 fractions (n = 33; 32% of plans); 35 Gy in 5 fractions (n = 33; 32.0% of plans); 45 Gy in 3 fractions (n = 11; 10.5%), 28 Gy in 4 fractions (n = 8; 7.8%) and 30 Gy in 3 fractions (n = 6; 5.8%). The mean dose, the maximum dose to the GTV as well as the biological effective doses (BEDs) for each are summarized in Table 2.
For evaluation of the treatment success and assessment of adverse effects patients were followed up on a regular basis. The first follow-up was scheduled 6–8 weeks after the last radiation appointment. During the following 2 years, the interval between appointments was 3 months; thereafter, intervals were prolonged to 6 months (years 3–4) and 12 months (≥5 years), respectively. If patients presented with new lesions during the follow-up period, they were re-enrolled for another series of SBRT under the condition that previous metastases were locally controlled and no late adverse effects of the first radiation series were recorded. In case of local failure after SBRT, re-radiation was considered if no new metastases where found.
Adverse effects were categorized according to the CTCAE 4.0 classification system. Retrospective analyses regarding patients’ characteristics, progression-free survival (PFS), overall survival (OS), disease-specific survival (DSS) and local tumor control (LTC) were performed using SPSS Statistics v. 22 (IBM Corp, Armonk, NY, USA). Local control rate was defined as freedom of local recurrence of the treated metastases according to the CT images during follow-up. OS, PFS and LTC were depicted by Kaplan–Meier curves in which the first series of SBRT served as the starting point. To detect differences in OS the log-rank test was used. To evaluate the influence of patient, disease or treatment characteristics on OS, PFS and DSS we chose multivariate Cox regression models. The level of significance was always defined to be p ≤ 0.05.
Results
Patient characteristics
Prior to radiation all patients underwent a pretherapeutic staging. In 54% (n = 47) of all cases, this staging included a 18F-fluorodeoxyglucose positron emission tomography with computed tomography (FDG-PET/CT). The maximum of lesions included in a single treatment plan was 3. Seventy-three patients were treated once; 14 patients presented with new lesions in the lung during the follow-up period and were re-enrolled (1 × in 13 cases, 4 × in 1 case) for SBRT. Upon initiation of SBRT, 55 patients (63.2%) had a solitary lung lesion and 13 patients (14.9%) presented with pulmonary OM (≤3 lesions). The remaining 19 patients (21.8%) were staged as stable disease (SD) with multiple pulmonary or extrapulmonary metastases except for the ones treated with SBRT. The most common primary tumor site was the lung (n = 23, 26.4%) and the colorectal region (n = 20, 23%). The median gross tumor volume (GTV) diameter was 2.4 cm (range 0.7–9.4 cm). The median GTV volume was 4.5 cm3 (range 0.1–128.1 cm3).
Outcome after SBRT
Median follow-up was 20.8 months (0.8–106.1 months). In all, 61 (36) of 87 patients had a follow-up period of >1 (2) year and 16.1% of patients were lost during follow-up. LTC after 1, 2 and 3 years was 96%, 94%, and 94%, respectively. In four cases (4.6%) local progression was observed after treatment (at 3.1, 3.4, 8.7 and 16.7 months after SBRT). Median survival was 28.2 months and OS at 1, 2 and 3 years was 77%, 59%, and 43%, respectively (Fig. 1). Disease-specific survival (DSS) was 81%, 63% and 52% after 1, 2 and 3 years. Median tumor-specific survival reached 41.1 months. During follow-up (4.7–106.1 months) progressive disease was diagnosed in 67 patients (77%), while 20 (23%) remained progression-free, resulting in a progression-free survival (PFS) of 9.4 months on average and a PFS of 45%, 27% and 17% at 1, 2 and 3 years after RT.
Prognostic factors
Patients with 1–3 metastatic sites showed a significantly (p = 0.015) higher median OS (29.7 months) than patients with multiple (>3) lung lesions (12.8 months). If extrathoracic metastases were present prior to radiation treatment, OS was 13.2 months compared to 29.7 months for patients with isolated lung metastases (p = 0.008). Furthermore, the size of GTV had a significant (p = 0.001) effect on median survival. GTV smaller 7.7 cm3 were associated with a longer survival (43.8 months) compared to larger GTVs (>7.7 cm3), which were associated with a survival of 17.1 months. This cut off refers to the diameter of the largest lesion in case of multiple lung metastases. Furthermore, with respect to OS, a better prognosis was present if newly diagnosed metastases during follow-up were limited to the lung (median survival: 43.7 months versus 21.7 months; p = 0.023). Patients primarily presented to SBRT had a similar median overall survival (29 months) as compared to pretreated patients (26 months; p 0.228). The survival curves are illustrated in Fig. 2.
Nearly half of all patients (n = 47.5%) were initially staged with FDG-PET prior to SBRT (Fig. 1). These patients showed significantly improved OS of 34.8 months compared to those who did not receive a FDG-PET (21.5 months, p = 0.023; Fig. 3). These prognostic factors for the OS also held true for other outcome parameters: DSS and PFS were significantly (p < 0.05) better for patients with a maximum of 3 lung metastases, no extrathoracic metastases at the time of the SBRT, a GTV that was <7.7 cm3, staging that included FDG-PET/CT imaging as well as solely lung metastases during follow-up. These results were confirmed on multivariable Cox regression (Table 3).
Kaplan–Meier estimates of overall survival after stereotactic body radiotherapy (SBRT). a Influence of gross tumor volume (GTV), b number of metastases, c extrathoracic metastases, d primary tumor site, e metastases during follow-up and f positron-emission tomography computed tomography (FDG-PET/CT) staging on the outcome
Only few cases of adverse effects were reported. Ten patients developed a pneumonitis grade two, in four cases grade two dyspnea and in one case grade two fatigue occurred. Neither rib fractures, thoracic pain nor other adverse effects grade 3 or 4 were observed. The average mean dose (Dmean) to the ipsilateral lung was 6.2 ± 2.9 Gy. The contralateral lung average Dmean was 1.6 Gy ± 1.6. The average V20 was 7.8 ± 6.6%. The size of the GTV, the median dose to the ipsilateral lung, and the number of metastases treated (1 vs. >1) showed no significant correlation with the frequency of adverse effects (p = 0.72, p = 0.42, p = 0.67, respectively).
Discussion
With regard to OS, disease-specific survival (DSS), PFS, LCR and the frequency of adverse effects, our results are in accordance with previous studies [4, 6,7,8,9,10,11,12,13] and reinforce extracranial stereotactic RT as a valid and effective therapy option in a curative as well as in a palliative approach. Life expectancy can be improved and even cure can be accomplished in a subgroup of patients with SBRT. The number and distribution pattern of metastases as well as the size of the target volume have an important prognostic impact. This information can be obtained from pretherapeutic staging. If a FDG-PET/CT is part of the staging, the prognosis after SBRT is better due to a more accurate patient selection.
Previously published series report local control rates after SBRT in lung metastases ranging between 73.3 and 96% after 2 years [4, 7,8,9,10,11,12,13]. Some of these studies suggested that local control depends on the application of a high dose to target volume [4, 6, 14, 15]. Even though dose prescriptions varied widely in our study, PFS was higher (>94% after 3 years) than previous studies. The 2‑year overall survival of patients after SBRT varies greatly (38–84.3%) in earlier reports [4, 7, 8, 11,12,13,14, 16, 17]. Nevertheless OS was slightly lower in our study than the average values of these previous studies. This might be due to the fact that four out of nine analyzed studies [8, 11, 13, 16] used a selected subgroup of patients excluding risk factors such as extrathoracic metastases or multiple metastases in the lung (OS after 2‑year follow-up was 66.5–84.3% in these studies). Based on studies by Tree et al. [18] and Inoue et al. [17] approximately one fifth of all patients were progression free 2–3 years after SBRT. These observations were confirmed in our study: 23% of patients did not show any tumor progress within their individual follow-up period. PFS after 1, 2 and 3 years was 45%, 27% and 17%, respectively.
Previous studies dealing with SBRT of lung tumors mentioned several factors as predictors for an improved OS. These include a low number of metastases (≤3 lesions) [19], no new metastases during follow-up [7], a long event-free interval [16, 20], good overall condition [17, 20], a smaller GTV volume of less than 3.3 cm3 [13], absence of a previous systemic therapy [4] as well as an applied BED of over 90 Gy [17]. On the other hand the presence of extrathoracic metastases was found to be associated with a shorter OS [20]. Some of these prognostic factors such as the number and localization of metastases as well as target volume can be obtained from re-staging prior to SBRT. Our results confirm that these factors have an important impact on the prognosis after SBRT and therefore should be taken into account prior to treatment. We believe the major strength of our article is that we have robust data, even in a small group of patients. This is highly relevant for every radiation oncologist who performs SBRT for metastases, as we provide strong prognostic factors that also have an impact in small patient cohorts. The use of a FDG-PET/CT for pretherapeutic staging led to a significantly longer overall survival in our study. Most likely this survival benefit is caused by better patient selection. Patients who did not receive PET imaging were more likely to have a more advanced stage of disease resulting in shorter OS and PFS. Staging without a FDG-PET/CT raises the risk of treating patients in a stage of advanced disease in which systemic therapy should be preferred. New metastases after SBRT in the lung during follow-up showed a longer OS than patients with new metastasis in other organs. Therefore extrathoracic metastases are a strong negative prognostic factor regardless of whether they occur before or after treatment with SBRT. Interestingly there was no significant difference in overall survival between patients without pretreatment prior to SBRT as compared to those who had been heavily pretreated. SBRT seems to be an adequate and safe treatment option in both settings and should always also be considered in “unfavorable” patients with several other oncological pretreatments.
Our data reveal that the evaluated prognostic factors (extrathoracic metastases, the number of metastatic sites in the lung, the GTV and FDG-PET/-CT as part of the staging) are valid in terms of OS but also in terms of disease and progression-free survival. There are only few other studies taking PFS, DSS or LCR into account when prognostic factors are discussed: In a study by Kang et al. [21] 78 lesion (not exclusively in the lung) in 59 patients were treated with SBRT. The authors showed that a cumulative GTV of less than 23 cm3 was a statistically significant indicator for better local control. In accordance with these findings three of four patients with a local relapse in our study showed clearly greater gross target volumes (15 cm3, 24 cm3, 128.1 cm3) than the average GTV of 7.7 cm3. According to Ricardi et al. [13] this might be also true for PFS. In their study a smaller GTV (>3.3 cm3) was associated with significantly longer progression-free survival. Furthermore, some authors described that better local control is observed if chemotherapy was given initially and if metastases did not originate from the colon [12, 22]. Patients with breast cancer had the shortest OS and PFS after SBRT in our study. In contrast to our findings, Okunieff et al. [12] concluded that PFS after SBRT is longer if breast cancer is the primary tumor. However the total number of breast cancer patients was very low in our study (n = 7). Furthermore the treatment was in palliative intention in all cases and therefore lower doses were delivered to the GTV (Table 1). Thus, further research is needed to evaluate the primary tumor site as a prognostic factor.
All in all extracranial SBRT has proved to be a safe treatment procedure. Even though radiological changes can be seen in the majority of patients after SBRT [4, 8], these effects show no clinical correlate in most cases. Similar to our findings (no toxicities grade 3 or 4 were reported) previous studies described high-grade adverse effects (°3–°5) to be well under 10% [4, 7, 8, 11,12,13,14, 16, 17, 23]. Nevertheless, because of the retrospective nature of our data, one cannot rule out that the incidence of adverse effects is underestimated.
Conclusion
Prognostic factors should be taken into account when SBRT of lung metastases is discussed. The absence of extrathoracic metastases prior to SBRT, a low lumber of metastases sites (≤3) in the lung as well as small target volumes correlate with a better outcome after SBRT. Furthermore, patients who solely develop lung metastases subsequent to SBRT will live longer. FDG-PET/CT should be part of the staging procedure prior to SBRT since the additional information helps to identify patients suitable for stereotactic treatment.
References
Saito Y et al (2002) Pulmonary metastasectomy for 165 patients with colorectal carcinoma: a prognostic assessment. J Thorac Cardiovasc Surg 124(5):1007–1013
Pfannschmidt J et al (2003) Prognostic factors and survival after complete resection of pulmonary metastases from colorectal carcinoma: experiences in 167 patients. J Thorac Cardiovasc Surg 126(3):732–739
Corbin KS, Hellman S, Weichselbaum RR (2013) Extracranial oligometastases: a subset of metastases curable with stereotactic radiotherapy. J Clin Oncol 31(11):1384–1390
Rusthoven KE et al (2009) Multi-institutional phase I/II trial of stereotactic body radiation therapy for lung metastases. J Clin Oncol 27(10):1579–1584
Stera S et al (2017) Breathing-motion-compensated robotic guided stereotactic body radiation therapy. Patterns of failure analysis. Strahlenther Onkol 194(2):143–155
Wulf J et al (2005) Dose-response in stereotactic irradiation of lung tumors. Radiother Oncol 77(1):83–87
Hof H et al (2007) Stereotactic single-dose radiotherapy of lung metastases. Strahlenther Onkol 183(12):673–678
De Rose F et al (2016) Clinical outcome of stereotactic ablative body radiotherapy for lung metastatic lesions in non-small cell lung cancer oligometastatic patients. Clin Oncol (R Coll Radiol) 28(1):13–20
Rieber J et al (2017) Influence of institutional experience and technological advances on outcome of stereotactic body radiation therapy for oligometastatic lung disease. Int J Radiat Oncol Biol Phys 98(3):511–520
Tanadini-Lang S et al (2017) Nomogram based overall survival prediction in stereotactic body radiotherapy for oligo-metastatic lung disease. Radiother Oncol 123(2):182–188
Navarria P et al (2014) Stereotactic body radiotherapy (sbrt) in lung oligometastatic patients: role of local treatments. Radiat Oncol 9(1):91
Okunieff P et al (2006) Stereotactic Body Radiation Therapy (SBRT) for lung metastases. Acta Oncol 45(7):808–817
Ricardi U et al (2012) Stereotactic body radiation therapy for lung metastases. Lung Cancer 75(1):77–81
Nuyttens JJ et al (2015) Stereotactic body radiation therapy for oligometastases to the lung: a phase 2 study. Int J Radiat Oncol Biol Phys 91(2):337–343
Onishi H et al (2004) Stereotactic hypofractionated high-dose irradiation for stage I nonsmall cell lung carcinoma: clinical outcomes in 245 subjects in a Japanese multiinstitutional study. Cancer 101(7):1623–1631
Norihisa Y et al (2008) Stereotactic body radiotherapy for oligometastatic lung tumors. Int J Radiat Oncol Biol Phys 72(2):398–403
Inoue T et al (2013) Stereotactic body radiotherapy for pulmonary metastases. Prognostic factors and adverse respiratory events. Strahlenther Onkol 189(4):285–292
Tree AC et al (2013) Stereotactic body radiotherapy for oligometastases. Lancet Oncol 14(1):e28–e37
Salama JK et al (2012) Stereotactic body radiotherapy for multisite extracranial oligometastases: final report of a dose escalation trial in patients with 1 to 5 sites of metastatic disease. Cancer 118(11):2962–2970
Zhang Y et al (2011) Stereotactic body radiation therapy favors long-term overall survival in patients with lung metastases: five-year experience of a single-institution. Chin Med J (Engl) 124(24):4132–4137
Kang JK et al (2010) Oligometastases confined one organ from colorectal cancer treated by SBRT. Clin Exp Metastasis 27(4):273–278
Thibault I et al (2014) Predictive factors for local control in primary and metastatic lung tumours after four to five fraction stereotactic ablative body radiotherapy: a single institution’s comprehensive experience. Clin Oncol (R Coll Radiol) 26(11):713–719
Dhami G et al (2017) Framework for radiation pneumonitis risk stratification based on anatomic and perfused lung dosimetry. Strahlenther Onkol 193(5):410–418
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
K.J. Borm, M. Oechsner, K. Schiller, J.C. Peeken, H. Dapper, S. Münch, L. Kroll, S.E. Combs and M.N. Duma declare that they have no competing interests.
Ethical standards
The ethics committee of the Technical University Munich approved this retrospective study (84/16S). All patients gave their informed consent both informed and written before starting the radiotherapy that they will undergo CT radiotherapy treatment planning. Data from the CT radiotherapy treatment planning were retrospectively analyzed.
Rights and permissions
About this article
Cite this article
Borm, K.J., Oechsner, M., Schiller, K. et al. Prognostic factors in stereotactic body radiotherapy of lung metastases. Strahlenther Onkol 194, 886–893 (2018). https://doi.org/10.1007/s00066-018-1335-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-018-1335-x