Abstract
Background and purpose
In this retrospective treatment planning study, the effect of a uniform and non-uniform planning target volume (PTV) dose coverage as well as a coplanar and non-coplanar volumetric modulated arc therapy (VMAT) delivery approach for lung stereotactic body radiation therapy (SBRT) in deep inspiration breath-hold (DIBH) were compared.
Materials and methods
For 46 patients with lesions in the peripheral lungs, three different treatment plans were generated: First, a coplanar 220° VMAT sequence with a uniform PTV dose prescription (UC). Second, a coplanar 220° VMAT treatment plan with a non-uniform dose distribution in the PTV (nUC). Third, a non-coplanar VMAT dose delivery with four couch angles (0°, ±35°, 90°) and a non-uniform prescription (nUnC) was used. All treatment plans were optimized for pareto-optimality with respect to PTV coverage and ipsilateral lung dose. Treatment sequences were delivered on a flattening-filter-free linear accelerator and beam-on times were recorded. Dosimetric comparison between the three techniques was performed.
Results
For the three scenarios (UC, nUC, nUnC), median gross tumor volume (GTV) doses were 63.4 ± 2.5, 74.4 ± 3.6, and 77.9 ± 3.8 Gy, and ipsilateral V10Gy lung volumes were 15.7 ± 6.1, 13.9 ± 4.7, and 12.0 ± 5.1%, respectively. Normal tissue complication probability of the ipsilateral lung was 3.9, 3.1, and 2.8%, respectively. The number of monitor units were 5141 ± 1174, 4104 ± 786, and 3657 ± 710 MU and the corresponding beam-on times were 177 ± 54, 143 ± 29, and 148 ± 26 s.
Conclusion
For SBRT treatments in DIBH, a non-uniform dose prescription in the PTV, combined with a non-coplanar VMAT arc arrangement, significantly spares the ipsilateral lung while increasing dose to the GTV without major treatment time increase.
Zusammenfassung
Hintergrund und Ziel
In dieser retrospektiven Bestrahlungsplanungsstudie wurde der Einfluss einer homogenen und inhomogenen Dosisabdeckung des Planungszielvolumens (PTV), sowie der Effekt einer koplanaren und nichtkoplanaren volumenmodulierten Bogentherapie (VMAT) für stereotaktische Behandlungen (SBRT) in der Lunge im Atemanhalt (DIBH) miteinander verglichen.
Material und Methoden
Für 46 Patienten mit Läsionen in der peripheren Lunge wurden drei verschiedene Bestrahlungspläne erstellt: Eine koplanare 220° VMAT-Sequenz mit homogener Dosisverschreibung im Zielvolumen (UC), eine koplanare 220°-VMAT-Sequenz mit inhomogener Dosisverteilung im Zielvolumen (nUC) und eine nichtkoplanare VMAT-Sequenz mit vier Tischauslenkungen (0°, ± 35°, 90°) mit inhomogener Dosisverschreibung (nUnC). Alle Behandlungspläne wurden in Bezug auf PTV-Abdeckung und ipsilaterale Lungendosis auf Pareto-Optimalität optimiert. Die Sequenzen wurden an einem ausgleichsfilterfreien Linearbeschleuniger abgestrahlt und die Strahlzeiten bestimmt. Ein dosimetrischer Vergleich der Methoden wurde durchgeführt.
Ergebnisse
Für die drei Szenarien (UC, nUC, nUnC) betrugen die medianen makroskopischen Tumorvolumen (GTV) Dosen 63,4 ± 2,5, 74,4 ± 3,6 und 77,9 ± 3,8 Gy und die ipsilateralen V10Gy-Lungenvolumina 15,7 ± 6,1, 13,9 ± 4,7 und 12,0 ± 5,1 %. Die Wahrscheinlichkeit einer Normalgewebskomplikation in der ipsilateralen Lunge betrug 3,9, 3,1 und 2,8 %. Die Monitoreinheiten waren 5141 ± 1174, 4104 ± 786 sowie 3657 ± 710 MU und die entsprechenden Strahlzeiten 177 ± 54, 143 ± 29 und 148 ± 26 s.
Schlussfolgerung
Bei SBRT-Behandlungen in DIBH schont die Behandlung mit einer nichtkoplanaren Behandlungssequenz in Kombination mit einer inhomogenen Dosisverschreibung signifikant die ipsilaterale Lunge bei gleichzeitiger Erhöhung der Dosis im GTV ohne nennenswerte Erhöhung der Behandlungszeit.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stereotactic body radiation therapy (SBRT) is defined [1] as “a method of external beam radiotherapy (EBRT) that accurately delivers a high dose of irradiation in one or few treatment fractions to an extracranial target.” It has become an established option for treatment of lung metastases [2] and inoperable early stage non-small cell lung cancer (NSCLC) [3,4,5]. In addition, there is currently an ongoing debate as to whether it possibly presents an alternative to lobectomy [6,7,8,9,10] as a primary form of therapy. Within this context, the question of the optimal SBRT treatment planning and delivery arises. While there is an ongoing discussion about the most effective fractionation scheme and total cumulative dose [11], this article focusses on the choice of the dose delivery approach and compares different dose prescription methods.
For radiation therapy in the peripheral lung, predominantly two factors have to be optimized: The dose to the target volumes (gross tumor volume [GTV] and planning target volume [PTV]) as well as the dose to the surrounding organs at risk (OAR), the ipsilateral lung minus PTV (ILL). While one typically tries to reach a sufficiently high biologically effective dose (BED) to the GTV to achieve a high tumor control probability [12], the dose to the lung and therefore the normal tissue complication probability (NTCP) has to be minimized to maximize the therapeutic window.
For radiation therapy of potentially moving targets on standard clinical linear accelerators (LINACs), the PTV margin typically depends on the type of motion management. In AAPM reports 91 [13] and 101 [14] as well as ICRU report 91 [15] on SBRT and motion management, a detailed description of the treatment delivery options are presented: Internal target volume (ITV) definition based on 4D-CT [14], gating via breath-hold techniques such as deep inspiration breath-hold (DIBH) [16], or based on tidal volume [17], with or without body frame/gimbal, multi leaf collimator (MLC) tracking [18], or robotic tracking [19] represent suitable options. In this study, DIBH-based target volumes are considered in combination with daily 3D image guidance.
However, besides the appropriate choice of motion management to minimize the PTV volume to reduce dose and therefore toxicity to the lungs, two further questions need to be addressed: How is the dose to be delivered and how should the resulting dose distribution ideally look? With respect to delivery, the methods on LINACs have changed over the past years from a few-field 3D conformal radiation therapy (3DCRT) towards intensity-modulated arc therapy (predominantly volumetric modulated arc therapy [VMAT]) techniques. Lately, several groups have recommended the use of additional non-coplanar beams or partial VMAT arcs: While this is routinely being used on non-standard LINACs, such as robotic mounted LINACs (e.g., CyberKnife, Accuray, Sunnyvale, USA [20]) or for intracranial stereotactic radiosurgery (e.g., Gamma Knife, Elekta AB, Stockholm, Sweden), it has just recently found more widespread use on conventional C‑arm LINACs [21,22,23]. Within this context, the question has to be raised how much couch rotation is feasible in single isocenter treatments without risking couch collisions, and under these conditions, how large is the maximum dosimetric benefit for the ipsilateral lung?
With the advent of intensity modulation on conventional linear accelerators, the method of dose prescription was subject to several modifications: While in the era of 3DCRT target homogeneity was a prioritized goal as described in ICRU report 50 [24] and dosimetric deviations “should be kept within +7 and −5%” (page 20), this was already being interpreted less strictly when intensity-modulated radiation therapy (IMRT) was used. Therefore, in ICRU report 83 [25] the statement was changed to: “With IMRT, these constraints can be unnecessarily confining if the avoidance of normal tissue is more important than target-dose homogeneity” (p. 36). The recently published ICRU report 91 [15] now recommends for stereotactic treatments: “With SRT, these constraints are not in use … Therefore, the dose is currently often prescribed to the 60 to 80% isodose line that is located on the outline of the PTV” (p. 107). Choosing the appropriate prescription isodose level for normalization can be used to decrease the lung dose while maintaining full target coverage [26]. RTOG trial 0915 [27] presents a possible application of this principle for peripheral NSCLC. In RTOG 0915 the isodose line prescription is linked with a dose–volume histogram (DVH)-based prescription: The prescription isodose line has to be chosen such that at least 95% of the PTV is covered by 100% of the prescription dose.
The purpose of this work is to quantify potential dosimetric benefits of different stereotactic treatment planning approaches such as a non-coplanar partial arc VMAT delivery and a non-uniform dose prescription for patients that receive treatment in DIBH on a C-arm medical linear accelerator.
Methods and materials
In this retrospective treatment planning study, SBRT treatment plans for 46 patients with lesions in the peripheral lungs with GTV diameters between 1 and 3 cm and treatment volumes V(PTV) = 20.5 ± 17.5 cm3, V(PTV)min = 3.8 cm3, V(PTV)max = 85.4 cm3 were generated. Solely target volumes further than 2 cm away from the proximal bronchial tree were considered [27]. Treatment planning CT scans were obtained in DIBH [16, 29]. Patient positioning and treatment on the LINAC (VersaHD, Elekta AB, Stockholm, Sweden) were also performed in DIBH (with GTV-to-PTV-margins 6 mm laterally and 9 mm craniocaudally) using the active breathing coordinator (ABC, Elekta). Patients within this study were able to hold her/his breath repeatedly for 15–20 s during which imaging or delivery took place, followed by a free-breathing phase where the patient could recover. All treatment sequences were created with flattening-filter-free (FFF) dose delivery with either 6 or 10 MV nominal acceleration potential (maximum dose rates 1500MU/min or 2400 MU/min), and 0° collimator angle [28]. To obtain the highest possible plan quality and the lowest treatment times, the beam isocenter was in all scenarios set to the center of mass of the PTV. Treatment planning was performed with a Monte Carlo-based treatment planning system (Monaco, Elekta) in the following manner: A prescription template was manually generated that aimed to (a) fulfill the OAR constraints, (b) achieve the desired target coverage, and (c) minimize the dose to the ipsilateral lung. For the three planning scenarios presented below, multiple treatment plans were generated and the one with the lowest ipsilateral lung dose but still sufficient target coverage was accepted. The prescription dose to 95% of the PTV was D95%(PTV) = 60 Gy, delivered in 5 fractions [1, 29] (132 Gy BED with α/β = 10 Gy for tumor tissue [1]). For each patient, three different treatment plans were generated:
-
a)
Uniform dose coverage, coplanar VMAT (UC):
First, a treatment plan with two coplanar 220° VMAT arcs that was used to deliver a uniform dose distribution to the PTV. The planning objective was to cover all voxels in the PTV according to ICRU report 50 [24] (PTV coverage 95–107%).
-
b)
Non-uniform dose coverage, coplanar VMAT (nUC):
Second, the same VMAT arc arrangement was used to deliver a non-uniform dose distribution in the PTV. The prescribed dose to the PTV was still D95% = 60 Gy but the dose to the GTV had to be within 120 and 150% of the prescription dose as proposed in the RTOG trial 0915 [27] (and in analogy to ICRU report 91 [15]).
-
c)
Non-uniform dose coverage, non-coplanar VMAT (nUnC):
Third, a non-coplanar VMAT dose delivery with five (partial) arcs at four different couch angles (0°, ±35°, 90°) combined with a non-uniform PTV prescription as described above was used. For 0° couch angle one ipsilateral 180° arc was selected. On the ipsilateral side two partial arcs, an anterior one with 100–140° arc length and a posterior one with 25–65° arc length, were used. For the contralateral side one anterior partial arc (100–170° arc length) was used and for couch 90° a posterior arc (20–40° arc length) was chosen.
For all non-coplanar arcs the arc length depended on the lateral couch position and its height. The patient was positioned on the couch with arms above the head. To obtain the beam-on times and test for potential couch collisions, the treatment sequences were delivered with original couch angles and couch positions on the linear accelerator, with a test phantom (CIRS, model 002LFC) and treatment aids on the couch.
To compare the resulting different DVH curves of the ILL, the normal tissue complication probability (NTCP) as well as the radiation-induced pneumonitis risk according to Marks et al. [30] was determined. The NTCP of the ILL was determined with Equations (1) and (2) according to the Lyman–Kutcher–Burman model (LKB) [31].
LKB parameters for radiation pneumonitis in the ipsilateral lung [32] were m = 0.35, and the tolerance dose for a 50% complication risk TD50 = 37.6 Gy. In 2 vi is the fractional organ volume that receives the dose Di and the tissue-specific parameter that describes the volume effect n = 1. The presented DVH data need to be corrected for hypo-fractionation effects. For α/β = 3 Gy for lung tissue [33] the equivalent total dose in 2 Gy fractions (EQD2) is a factor of 3 higher. Alternatively, according to Marks et al. [30], the complication probability p for radiation-induced pneumonitis in the lung can be estimated with a logistic fit function of the mean lung dose of the total lung, converted into 2 Gy fraction doses (MLD2) as shown in Equation (3).
In Equation (3) parameters were b0 = −3.87, b1 = 0.126 Gy−1, and α/β = 4 Gy (unlike other publications, Marks et al. [30] used a factor of α/β = 4 Gy in their model for lung tissue).
Dosimetric evaluation was performed in Matlab (MathWorks, Natick, MS, USA) by importing all cumulative dose–volume histograms and determining the relevant dose–volume metrics of the individual treatment plans, performing two-sided paired t‑tests for statistical significance, generating the mean DVH, and based on the mean DVH, the biological response.
Results
In Fig. 1 dose distributions in the transversal isocenter plane for the three different treatment approaches are displayed. Each column represents a different patient with different PTV volumes V(PTV) (left: 4 cm3, middle: 24 cm3, right: 63 cm3).
Transversal isocentric CT slices for the different volumetric modulated arc therapy (VMAT) beam arrangements and the resulting dose distributions in (Gy) for three patients with different planning target volumes V(PTV) (left column: 4 cm3; middle column: 24 cm3, right column: 63 cm3). First row: unifom conplanar dose delivery (UC), second row: non-uniform coplanar dose delivery (nUC), third row: non-uniform non-coplanar dose delivery (nUnC), forth row: resulting dose volume histograms (DVH) for gross tumor volumes (GTV), planning target volumes (PTV), right and left lungs
The resulting dose–volume and delivery parameters for of the entire patient collective are presented In Table 1. In the following, all comparisons refer to the corresponding UC dose distributions. An nUC delivery prescription increases the median dose to the GTV by 11.0 Gy. Using non-coplanar beams further increases the median GTV dose by 3.5 Gy. Despite this increase in dose to the GTV, a reduction of the ILL V10Gy by 1.8% in the nUC cases and an additional 1.9% for the nUnC cases was achieved. A similar picture is true for the ILL V20Gy, where a reduction of 0.7 and 2.0% was achieved. These reductions in mean ILL dose result in a reduction of NTCP by 0.8% for nUC cases and 1.1% for nUnC, or 0.5 and 0.7% for the Marks’ complication probability, respectively.
An nUC dose delivery reduces the mean number of required monitor units by 1037 MU (20.2%). If non-coplanar beams are added this yields an additional reduction of 447 MU (8.7%). Furthermore, the nUC cases lead to a 41 s reduced beam-on time. If non-coplanar beams are added the beam-on time reduction is 26 s, since more start and stop procedures are needed. In order to estimate the number of required breath-holds, we assume that the dose delivery is stopped either after a breath-hold of 20 s, or when the end of an arc is reached. Under this assumption, a mean reduction of 2.0 breath-holds in the nUC case is achieved. The nUnC cases on the other hand require 0.2 breath-holds more than the UC case.
Two-sided, paired-sample t‑tests were performed for all presented data in Table 1. UC and nUC sequences were tested against nUnC sequences. Asterisks in Table 1 indicate that a two-sided paired-sample t‑test does not reject the null hypothesis at 5% significance level.
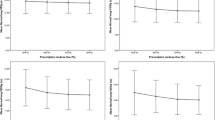
In Fig. 2 a box-plot of GTV and PTV parameters, near-minimum dose D98%, median dose D50%, and near-maximum dose D2% for the three different treatment planning strategies, as well as the ipsilateral lung V3Gy to V20Gy are displayed. For all ILL metrics the median ILL volumes of the nUC cases are lower than the UC cases. For the nUnC cases a different scenario becomes evident: While for ILL V10Gy and above median doses are even lower than the UC and nUC cases, the volume that receives lower doses is increased. The intersection with the nUnC cases is reached at 3.1 Gy in the UC cases and 4.6 Gy for the nUC cases.
Furthermore, it can be seen from Fig. 2 and the standard deviations in Table 1 that the dose metrics vary considerably within one planning strategy. To identify possible dependent parameters, Pearson correlation coefficients between different dose–volume metrics and the volume of the PTV were evaluated (Table 2). In addition, the distance between the center of mass of the PTV and the center of mass of the patient contour in the transversal isocenter plane was evaluated. The Pearson correlation between the PTV volume and its radial position was 0.17. Thus, the two variables are considered independent.
The following relevant correlations between the PTV volume and the DVH metrics in Table 2 were identified:
-
PTV near-minimum doses show a weak negative correlation for UC and nUnC and a strong negative correlation for nUC. Median PTV doses show a weak positive correlation for UC and a strong positive correlation for nUC and nUnC plans.
-
All ILL dose metrics increase with PTV size.
-
The required number of monitor units show a weak negative correlation for UC and a weak positive correlation for nUC and nUnC. For UC less MU are needed for larger target volumes since the effective field size increases. For UC and nUnC non-uniformity is originates from a superposition of even smaller segments.
The following relevant correlations were identified for the radial PTV positions:
-
GTV doses decrease with radial position for nUC (weakly correlated) but not for UC and nUnC sequences.
-
CLL, trachea, and main bronchus doses decrease with radial position, while dose to the thoracic wall increases with radial position.
-
MUs decrease with radial position (weakly correlated).
Discussion
All presented results were obtained from dose distributions that were simulated with a clinically commissioned Monte Carlo treatment planning system without any electron density overrides on a treatment planning CT in DIBH. Thus, all dosimetric data are accurate within 1% dosimetric uncertainty [34]. All treatment sequences were deliverable under realistic treatment conditions and we tried to achieve a maximum number of independent fluence angles for the nUnC cases. Beam-on times result from actual deliveries of the sequences.
The high number of monitor units in the uniform case can be explained with the fact that more small segments need to be delivered in the target periphery to compensate for the beam penumbra. This results not only in a prolonged beam-on time but also in a higher dosimetric uncertainty, since small segments close to lung tissue and water-equivalent medium interfaces are present that alter scatter conditions (cf. AAPM report 101 [14]). A more simplified delivery sequence like a dynamic conformal arc is feasible but will, in many cases, lead to a worse dose conformality and/or target uniformity.
While the three different treatment planning approaches fulfill the recommended RTOG trial 0915 [27] lung tolerances (to stay below 3.1 Gy per fraction in less than 1000 cm3 of the lungs to minimize pneumonitis risk), radiation-induced pneumonitis is a stochastic effect. Thus, any reduction in the dose to the lungs, as depicted in the presented scenarios, is beneficial, though clinical relevance increases for larger PTV volumes.
With respect to a non-uniform prescription, Craft et al. [35] recommend a reconsideration of whether a uniform dose is really needed. Within this context, we demonstrated that dose escalation in the target volume can be combined with ILL sparing if the paradigm of a uniform dose distribution in the target is omitted. Another important aspect in the context of non-uniform dose prescription is that doses within the volume outside of the GTV but within the PTV safety margin typically also receive higher doses compared to a non-uniform dose prescription. This may eventually lead to an increased amount of radiation necrosis in this lung tissue. Therefore, a close evaluation of local recurrence after treatment including PET or functional CT imaging is recommended.
Sheng et al. [36] discuss the advantages and disadvantages of a non-coplanar delivery. While a dose distribution generated by a non-coplanar delivery is typically at least as good as a coplanar delivery with respect to target coverage and OAR sparing, the following aspects limit it from a more widespread use: added treatment planning complexity, greater potential for setup errors, an increased risk of collisions, and longer treatment times. For SBRT treatments in DIBH, at least some of the concerns raised above are less problematic: As demonstrated, the average number of breath-hold phases for an nUnC delivery is comparable to the UC scenario and two additional breath-hold phases are needed in comparison to the nUC cases. Furthermore, the patient needs to breathe in between two breath-hold phases anyway. Thus, the personnel have sufficient time to go into the treatment room and manually perform the couch rotation without an extended treatment prolongation due to couch rotations, and without risking an unsupervised patient–LINAC collision. However, if the patient moves during couch rotation this may induce additional errors, which requires further investigation before clinical introduction. This problem can eventually be addressed by live tracking of the patient with optical surface scanners [37]. An increase in treatment planning complexity can be addressed with either automated beam/arc angle selection [38, 39] or with appropriate prescription templates, which depend on the lateral target position and couch height.
The use of VMAT with multiple non-coplanar partial arcs implies the maximum degree of dose “smearing” possible on a standard LINAC. This form of delivery is therefore to be positioned at an extreme end in the ongoing discussion about “a little (dose) to a lot (volume)” vs. “a lot (dose) to a little (volume)” [40]. If n = 1 in the LKB model is correct, as Semenenko et al. [32] (n = 1) or Marks et al. [30] (n = 1.03 ± 0.17) suggest, the NTCP depends solely on the mean lung dose (2) and not on the particular shape of the DVH. This means that as long as a lower mean lung dose is achieved, as presented in the above scenarios, the NTCP is also lower. If n < 1 as, e.g., Tucker et al. [41] (n = 0.41) recommend, a noncoplanar beam delivery is even more beneficial, since under this assumption high doses to small volumes are more detrimental than a smeared out dose distribution. Gordon et al. [42] on the other hand reported an enhanced damage contribution from doses lower than 20 Gy (low dose hyper-radiosensitivity), which reflects a factor n > 1 in the LKB model. In this case a classic 3DCRT would be the preferable method.
Finally, it should be highlighted that the presented data are the results of a treatment planning study. Therefore, potential delivery errors such as the repeatability of the PTV position in DIBH, residual motion errors during breath-hold, or uncompensated couch rotation errors may lead to undesired results and need to be evaluated before applying a non-uniform, non-coplanar dose delivery to SBRT patients.
Conclusion
For SBRT treatments in the lung, a non-uniform dose prescription in the PTV combined with a realistic, non-coplanar VMAT arc arrangement spares surrounding lung tissue while allowing for a maximum dose to the GTV. For treatments in DIBH it minimizes dose to the ipsilateral lung and therefore lung toxicity with only slightly prolonged treatment times.
References
Guckenberger M, Andratschke N, Alheit H et al (2014) Definition of stereotactic body radiotherapy: principles and practice for the treatment of stage I non-small cell lung cancer. Strahlenther Onkol 190:26–33
Rieber J, Streblow J, Uhlmann L et al (2016) Stereotactic body radiotherapy (SBRT) for medically inoperable lung metastases—a pooled analysis of the German working group stereotactic radiotherapy. Lung Cancer 97:51–58
Schneider BJ, Daly ME, Kennedy EB et al (2017) Stereotactic body radiotherapy for early-stage non-small-cell lung cancer: American Society of Clinical Oncology endorsement of the American Society for Radiation Oncology evidence-based guideline. J Clin Oncol. https://doi.org/10.1200/JCO.2017.74.9671
Guckenberger M, Andratschke N, Dieckmann K (2017) ESTRO ACROP consensus guideline on implementation and practice of stereotactic body radiotherapy for peripherally located early stage non-small cell lung cancer. Radiother Oncol 124:11–17
Moustakis C, Blanck O, Ebrahimi Tazehmahalleh F et al (2017) Planning benchmark study for SBRT of early stage NSCLC: results of the DEGRO Working Group Stereotactic Radiotherapy. Strahlenther Onkol 193:780–790
Guckenberger M (2017) Stereotactic body radiotherapy for early stage NSCLC—what is the evidence? Zentralbl Chir 142(S 01):17–S25
Chang JY, Senan S, Paul MA et al (2015) Stereotactic ablative radiotherapy versus lobectomy for operable stage I non-small-cell lung cancer: a pooled analysis of two randomised trials. Lancet Oncol 16:630–637
Ricardi U, Badellino S, Filippi AR (2015) Stereotactic radiotherapy for early stage non-small cell lung cancer. Radiat Oncol 33:57–65
Soldà F, Lodge M, Ashley S et al (2013) Stereotactic radiotherapy (SABR) for the treatment of primary non-small cell lung cancer; systematic review and comparison with a surgical cohort. Radiother Oncol 109:1–7
Yu XJ, Dai WR, Xu Y (2017) Survival outcome after stereotactic body radiation therapy and surgery for early stage non-small cell lung cancer: a meta-analysis. J Invest Surg 22:1–8
Ramroth J, Cutter DJ, Darby SC et al (2016) Dose and fractionation in radiation therapy of curative intent for non-small cell lung cancer: meta-analysis of randomized trials. Int J Radiat Oncol Biol Phys 96:736–747
De Ruysscher D, Faivre-Finn C, Moeller D (2017) European Organization for Research and Treatment of Cancer (EORTC) recommendations for planning and delivery of high-dose, high precision radiotherapy for lung cancer. Radiother Oncol 124:1–10
Keall PJ, Mageras GS, Balter JM et al (2006) AAPM report no. 91 the management of respiratory motion in radiation oncology. Med Phys 33:3874–3900
Benedict SH, Yenice KM, Followill D et al (2010) Stereotactic body radiation therapy: the report of the AAPM ask Group 101. Med Phys 37:4078–4101
Seuntjens J, Lartigau EF, Cora S et al (2014) ICRU report 91: Prescribing, recording, and reporting of stereotactic treatments with small photon beams. J ICRU 14:1–160. https://doi.org/10.1093/jicru/ndx010
Boda-Heggemann J, Knopf AC, Simeonova-Chergou A et al (2016) Deep inspiration breath hold based radiation therapy: a clinical review. Int J Radiat Oncol Biol Phys 94:478–492
Giraud P, Morvan E, Claude L et al (2011) Respiratory gating techniques for optimization of lung cancer radiotherapy. J Thorac Oncol 6:2058–2068
Caillet V, Keall PJ, Colvill E et al (2017) MLC tracking for lung SABR reduces planning target volumes and dose to organs at risk. Radiother Oncol 124:18–24
Stera S, Balermpas P, Chan MKH et al (2018) Breathing-motion-compensated robotic guided stereotactic body radiation therapy : patterns of failure analysis. Strahlenther Onkol 194:143–155
Temming S, Kocher M, Stoelben E et al (2018) Risk-adapted robotic stereotactic body radiation therapy for inoperable early-stage non-small-cell lung cancer. Strahlenther Onkol 194:91–97
Fitzgerald R, Owen R, Barry T et al (2016) The effect of beam arrangements and the impact of non-coplanar beams on the treatment planning of stereotactic ablative radiation therapy for early stage lung cancer. J Med Radiat Sci 63:31–40
Sheng K, Shepard DM (2015) Noncoplanar beams improve dosimetry quality for extracranial intensity modulated radiotherapy and should be used more extensively. Med Phys 42:531–533
Dong P, Lee P, Ruan D (2013) 4π noncoplanar stereotactic body radiation therapy for centrally located or larger lung tumors. Int J Radiat Oncol Biol Phys 86:407–413
International Commission on Radiation Units and Measurements (1993) ICRU report 50: prescribing, recording and reporting photon-beam therapy
Gregoire V, Mackie TR, De Neuve W et al (2010) ICRU report 83: prescribing, recording and reporting photon-beam intensity-modulated radiation therapy (IMRT). J ICRU 10:1–106
Chan M, Wong M, Leung R et al (2018) Optimizing the prescription isodose level in stereotactic volumetric-modulated arc radiotherapy of lung lesions as a potential for dose de-escalation. Radiat Oncol 13:24. https://doi.org/10.1186/s13014-018-0965-6
Videtic GM, Hu C, Singh AK et al (2015) A randomized phase 2 study comparing 2 stereotactic body radiation therapy schedules for medically inoperable patients with stage i peripheral non-small cell lung cancer: NRG Oncology RTOG 0915 (NCCTG N0927). Int J Radiat Oncol Biol Phys 93:757–764. https://doi.org/10.1016/j.ijrobp.2015.07.2260
Boda-Heggemann J, Mai S, Fleckenstein J et al (2013) Flattening-filter-free intensity modulated breath-hold image-guided SABR (Stereotactic ABlative Radiotherapy) can be applied in a 15-min treatment slot. Radiother Oncol 109:505–509
Timmerman R, Paulus R, Galvin J (2010) Stereotactic body radiation therapy for inoperable early stage lung cancer. JAMA 303:1070–1076
Marks LB, Bentzen SM, Deasy JO (2010) Radiation dose-volume effects in the lung. Int J Rad Onc Biol Phys 76:S70–S76
Li XA, Alber M, Deasy JO et al (2012) AAPM report 166: the use and QA of biologically related models for treatment planning. Med Phys 39:1386–1409
Semenenko VA, Li XA (2008) Lyman–Kutcher–Burman NTCP model parameters for radiation pneumonitis and xerostomia based on combined analysis of published clinical data. Phys Med Biol 53:737
Borst GR, Ishikawa M, Nijkamp J et al (2010) Radiation pneumonitis after hypofractionated radiotherapy: evaluation of the LQ(L) model and different dose parameters. Int J Radiat Oncol Biol Phys 77:1596–1603
Fleckenstein J, Jahnke L, Lohr F et al (2013) Development of a Geant4 based Monte Carlo Algorithm to evaluate the MONACO VMAT treatment accuracy. Z Med Phys 23:33–45
Craft D, Khan F, Young M, Bortfeld T (2016) The price of target dose uniformity. Int J Radiat Oncol Biol Phys 96:913–914
Sheng K, Shepard DM (2015) Noncoplanar beams improve dosimetry quality for extracranial intensity modulated radiotherapy and should be used more extensively. Med Phys 42:531–533
Hepp R, Ammerpohl M, Morgenstern C et al (2015) Deep inspiration breath-hold (DIBH) radiotherapy in left-sided breast cancer: dosimetrical comparison and clinical feasibility in 20 patients. Strahlenther Onkol 191:710–716
de Pooter JA, Méndez Romero A, Wunderink W et al (2015) Automated non-coplanar beam direction optimization improves IMRT in SBRT of liver metastasis. Radiother Oncol 88:376–381
Gala DG, Dirkx MLP, Hoekstra N et al (2017) Fully automated VMAT treatment planning for advanced-stage NSCLC patients. Strahlenther Onkol 193:402–409
Willner J, Jost A, Baier K, Flentje M (2003) A little to a lot or a lot to a little? An analysis of pneumonitis risk from dose-volume histogram parameters of the lung in patients with lung cancer treated with 3‑D conformal radiotherapy. Strahlenther Onkol 179:548–556
Tucker SL, Mohan R, Liengsawangwong R et al (2013) Predicting pneumonitis risk: a dosimetric alternative to mean lung dose. Int J Radiat Oncol Biol Phys 85:522–527
Gordon JJ, Snyder K, Zhong H et al (2015) Extracting the normal lung dose–response curve from clinical DVH data: a possible role for low dose hyper-radiosensitivity, increased radioresistance. Phys Med Biol 60:6719–6732
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Fleckenstein, J. Boda-Heggemann, and A. Simeonova-Chergou have received speaker honoraria and travel cost compensation from Elekta AB. F. Wenz has received research grants from Elekta AB, Nucletron, and Carl Zeiss Meditec. Furthermore, he has received personal fees from Carl Zeiss Meditec, Celegene, and Ipsen. F. Lohr has received research grants from Elekta AB, and IBA dosimetry. Furthermore, he has received personal fees from Elekta AB, IBA dosimetry, and C‑RAD. K. Siebenlist, T. Gudzheva, and N. Prakofyeva declare that they have no competing interests.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Fleckenstein, J., Boda-Heggemann, J., Siebenlist, K. et al. Non-coplanar VMAT combined with non-uniform dose prescription markedly reduces lung dose in breath-hold lung SBRT. Strahlenther Onkol 194, 815–823 (2018). https://doi.org/10.1007/s00066-018-1316-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-018-1316-0
Keywords
- Stereotactic radiotherapy
- Intensity-modulated radiotherapy
- Radiotherapy planning
- Lung neoplasms
- Non-small-cell lung carcinoma