Abstract
Purpose
Low-dose external beam radiotherapy (ED-EBRT) is frequently used in the therapy of refractory greater trochanteric pain syndrome (GTPS). As studies reporting treatment results are scarce, we retrospectively analyzed our own patient collectives.
Patients and methods
In all, 60 patients (74 hips) received LD-EBRT (6 × 0.5 Gy in 29 hips, 6 × 1 Gy in 45). The endpoint was the patient’s reported subjective response to treatment. The influence of different patient and treatment characteristics on treatment outcome was investigated.
Results
At the end of LD-EBRT, 69% reported partial remission, 4% complete remission, no change 28%. A total of 3 months later (n = 52 hips), the results were 37, 33, and 30% and 18 months after LD-EBRT (n = 47) 21, 51, and 28%. In univariate analysis “inclusion of the total femoral head into the PTV” and “night pain before LD-EBRT” were correlated with symptom remission at the end of LD-EBRT, while “initial increase in pain during LD-EBRT” was significantly associated with treatment failure. In multivariable modeling “initial increase in pain” was identified as a risk factor for treatment failure (p = 0.007; odds ratio [OR] 0.209; 95% confidence interval [CI] 0.048–0.957), while “night pain” was an independent factor for remission (p = 0.038; OR 3.484; 95% CI 1.004–12.6). Three months after LD-EBRT “night pain” and “inclusion of the complete femoral neck circumference into the PTV” were predictive for remission.
Conclusion
LD-EBRT represents a useful treatment option for patients suffering from GTPS. Three months after therapy two-thirds of the patients reported a partial or complete symptom remission. Especially patients who suffered from nocturnal pain seemed to benefit. Treatment appeared to be more effective when the entire circumference of the femoral neck was encompassed.
Zusammenfassung
Hintergrund
In der Behandlung des therapierefraktären Trochanter-major-Schmerzsyndroms (GTPS) spielt die niedrig dosierte „Reizbestrahlung“ (LD-EBRT) eine wichtige Rolle, obwohl nur wenige Studien dazu vorliegen. Deshalb analysierten wir retrospektiv die Therapieergebnisse in unseren Kollektiven.
Patienten und Methoden
Insgesamt 60 Patienten (74 Hüften) erhielten eine Reizbestrahlung (6 × 0,5 Gy bei 29 Hüften, 6 × 1 Gy bei 45). Endpunkt war das subjektive Therapieansprechen. Verschiedene potentielle Einflussfaktoren auf das Therapieansprechen wurden untersucht.
Ergebnisse
Bei Abschluss der LD-EBRT berichteten 69% eine partielle Remission, 4% eine vollständige Remission und 28% keine Veränderung. Nach 3 Monaten (n = 52) waren es 37, 33 und 30 %, nach 18 Monaten (n = 47) 21, 51 und 28%. In der univariaten Analyse waren „Einschluss des Femurkopfs in das Zielvolumen“ und „Nachtschmerz vor LD-EBRT“ signifikant mit einem Ansprechen bei Abschluss der LD-EBRT korreliert, „initiale Schmerzverstärkung unter LD-EBRT“ hingegen mit einem Therapieversagen. In der multivariablen Analyse wurden „initiale Schmerzverstärkung“ als Risikofaktor (p = 0,007; Odds Ratio [OR] 0,209; 95%-Konfidenzintervall [KI] 0,048–0,957) und „Nachtschmerz“ als unabhängiger positive prädiktiver Faktor (p = 0,038; OR 3,484; 95%-KI 1,004–12,6) identifiziert. „Nachtschmerz“ und „Einschluss des gesamten Femurhalsumfangs in das Zielvolumen“ waren 3 Monate nach LD-EBRT mit einer Remission korreliert.
Schlussfolgerung
LD-EBRT ist eine wichtige Therapieoption für Patienten mit GTPS. Drei Monate nach Therapie berichten zwei Drittel der Patienten eine partielle oder vollständige Remission. Besonders profitieren Patienten, die zuvor unter nächtlichen Schmerzen gelitten hatten. Der Therapieerfolg schien abhängig zu sein vom Einschluss der gesamten Zirkumferenz des Femurhalses in das Zielvolumen.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Between 10 and 25% of the general population suffer from hip pain [1]. A high percentage can be assigned to gluteal tendon pathologies. The leading clinical symptom is persistent pain and tenderness in the vicinity of the greater trochanter in the lateral hip region, especially at the extreme of rotation, abduction (against resistance) or adduction, radiating into the lateral leg [1–3]. This syndrome has been formerly referred to as “bursitis trochanterica”. In contemporary studies, it is termed “greater trochanteric pain syndrome” (GTPS) [1]. GTPS is underestimated and underdiagnosed, resulting in a chronic undertreatment of these patients, not to forget the social and economic fallout that comes with chronic pain and limitation of mobility [2].
A variety of conditions is known to contribute to GTPS, e. g., osteoarthritis of the hip, degeneration or injuries of the lumbar spine, or rheumatoid arthritis [1]. Anatomic variances like discrepancies in leg lengths, pes planus, or snapping hip syndrome have also been associated with GTPS [1]. For pathogenesis, tears in the abductor’s tendons (gluteus medius and minimus muscles) and friction between these tendons, their bursae, the iliotibial fascia, and the trochanter seem to play a crucial role [2, 4].
Understanding of the complex morphology of these bursae located in proximity to the greater trochanter has increased considerably during the past 15 years. Traditionally, only two bursae were considered to be located in this region, the subgluteus maximus bursa and the subgluteus medius bursa (review in [5]). However, systematic anatomical dissections revealed a much higher density of bursae associated with the insertions of the gluteal tendons at the greater trochanter [5, 6]. In a landmark study with meticulous dissections of 18 embalmed hips of 15 donors, not less than two bursae were identified beneath the distal tendons of each of the three gluteal muscles [6]. Not all dissected hip contained all of these bursae. On average, six bursae were found per anatomical preparation.
Low-dose external beam radiotherapy (LD-EBRT) with six fractions of 0.5–1 Gy is known to ameliorate clinical symptoms of tendinitis. Several molecular biological mechanisms have been proposed (review in [7]). In painful plantar fasciitis, a randomized trial tested the clinical results after 6 × 0.1 Gy (comparable to sham irradiation) with 6 × 1 Gy [8], thus, providing clinical proof of the efficacy of LD-EBRT. Other randomized trials have shown similar effects of 6 × 1 Gy in comparison with 6 × 0.5 Gy in painful heel spur [9, 10], achillodynia [11], painful shoulder [12], and painful elbow syndromes [13]. Randomized trials on LD-EBRT in GTPS are lacking; in the German S2 guideline on EBRT of benign diseases, only two abstracts comprising 60 patients are cited [14]. Nonetheless, LD-EBRT is widely used in Germany to treat patients with GTPS after the failure of other therapeutic options. It is a well-accepted therapeutic option in daily clinical practice.
As data on the efficacy of LD-EBRT in GTPS are scarce and literature on target volume definition is missing, we evaluated and analyzed our collective retrospectively. Moreover, we investigated the influence of field definition on treatment outcome. To our knowledge, this has not been previously done.
Patients and methods
This is a multicenter, retrospective, observational study including 60 patients suffering from GTPS between 2007 and 2015 in three radiotherapy centers in northwestern Germany. Of these, 14 patients were treated bilaterally, so the effect of LD-EBRT was analyzed in 74 joints.
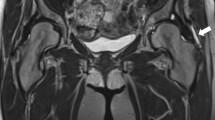
GTPS was diagnosed clinically; just a few patients had received magnetic resonance imaging of the hip joint. The included patients were referred to the radiotherapy centers from their general practitioners and orthopedic clinics for treatment.
Inclusion and exclusion criteria
Included were all consecutively treated patients during the defined study period. Exclusion criteria were age <30 years (n = 0), a radiological proven fasciitis of the fascia lata (n = 3), or generalized polyarthritis (n = 2).
Study endpoints
The primary study endpoint was the patient’s reported subjective response to treatment. It was classified according to complete symptom remission of pain (CR), some remission (partial remission, PR), and no remission (no change, NC). For statistical analysis, CR and PR were grouped together as “response”. Before initiation of LD-EBRT, different pain characteristics were evaluated as pain during exercise, at rest, or at night. Response to treatment was documented at the end of the LD-EBRT series, and after 3 and 18 months. In all, 74 joints (100%) were available for evaluation at the end of the LD-EBRT. However, at 3 months after LD-EBRT 22 joints (29.7%) were lost to follow-up, these patients did not respond to the invitation for a follow-up visit at the treating radiotherapy center. At 18 months after LD-EBRT, 47 joints (64%) were available for re-evaluation.
Radiation procedures
All patients were treated twice weekly, with a single dose of 1 Gy amounting to a total dose of 6 Gy; 39% were irradiated with 6 × 0.5 Gy up to a total dose of 3 Gy (according to the publication of the randomized studies cited in the introduction section). A linear accelerator (Siemens, Erlangen, Germany) was used to administer 6 MVX photons.
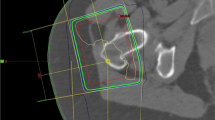
All patients received three-dimensional (3D) treatment planning. Planning CT scans were done with 5 mm slice distance (Siemens, Nürnberg, Germany) in the supine position. Delineation and planning were performed with routine software (Focal contouring®, XIO® treatment-planning [ELEKTA]). As clinical target volume, the region of the affected trochanter and the femur was delineated, according to the respective consultant. A safety margin of 1.5 cm in all directions was added to create the planning target volume. Of the plans 85% were done with a predominant anterior–posterior/posterior–anterior field technique. The other plans received further fields from lateral gantry positions.
Statistical methods
Pretreatment data on patient demographics as well as the underlying diseases and LD-EBRT-specific data were prospectively collected and retrospectively complemented in a study database. All continuous data were assessed for normal distribution applying the Kolmogorov–Smirnov test. If this test is significant (p < 0.05), the data is not normally distributed. Normally distributed data is presented as the mean and standard deviation and was analyzed with the independent Student’s t‑test, whereas nonparametric data are presented as median and range and were analyzed with the Mann–Whitney U test. Pearson’s χ2 tests were applied were appropriate. Possible relevant risk factors for outcome of LD-EBRT were identified by univariate binary logistic regression analyses using an α level of 0.20. Hence, all variables with a p-value <0.20 were included in multivariable regression analyses. In multivariate analyses, a p-value <0.05 was defined as statistically significant. The Hosmer–Lemeshow test was applied to evaluate goodness-of-fit of the regression models: if the model has good model fit, the p-value should be >0.05 [15]. Furthermore, multivariate principle component analysis was applied to identify independent risk factors for impaired outcome. In this graphical analysis, the effects of evaluated variables on the study endpoint are depicted as diverging vectors, which imply statistical independence in the multivariate model. The SPSS statistics software 23.0 (IBM, Somers, NY, USA) and SAS JMP Pro 11 software (SAS Institute, Cary, NC, USA) were used to perform statistical analyses.
Ethics statement
As a retrospective observational study, according to the Professional Code of the German Medical Association (article B.III. § 15.1), neither informed consent nor approval of the ethics committee was needed for this study.
Results
Patient characteristics are given in Table 1. A total of 35 left hips and 39 right hips were irradiated. Body height and weight were not documented in 26 patients, which is why the body mass index of 28 kg/m² is based on the data of just 34 patients. To evaluate the influence of “body size,” a surrogate parameter was calculated using the planning CT scans. At the height of the greater trochanter, the maximal mediolateral and posteroanterior diameters were measured and multiplied with each other (so-called “surface of planning CT scan”).
The continuous variables distance between inferior field border and greater trochanter, distance between inferior field border and minor trochanter, and distance between superior field border and socket edge were all not normally distributed according to significant Kolmogorov–Smirnov tests (all p < 0.001). Therefore, medians and ranges are reported, and nonparametric tests were applied. All other continuous variables were normally distributed. Table 1 summarizes the descriptive statistics of the study population (n = 74 joints) as well as the comparison of the response cohort (n = 53; 72%) and the nonresponse cohort (n = 21; 28%) at the end of LD-EBRT.
Treatment response
Fig. 1 shows the distribution of partial (PR) and complete remissions (CR) at the end of LD-EBRT, and 3 months as well as 18 months after that.
At the end of LD-EBRT, in 53 hips (72%) a remission had occurred: 51 (69%) reported PR and 2 (4%) CR. No changes (NC) in symptoms were observed in 21 cases (28%).
Three months after LD-EBRT, 22 cases (30%) did not follow the invitation for control visits at the treating center and did not respond to phone calls. Of the remaining 52 hips, a remission could be observed in 36 cases (70%), of which 19 cases were in PR (37%) and 17 in CR (33%). In 16 hips (30%), NC was reported by the patients.
At 18 months (mean) after LD-EBRT, 47 hips (64%) were available for re-evaluation. A remission could be observed in 34 cases (72%): in 10 (21%) PR, and in 24 (51%) CR. NC was reported in 13 hips (28%).
In all, 26 hip joints (35%) received a second LD-EBRT series during follow-up, a mean of 6 months after the first course. At the end of the second course, 19 (73%) reported remission: in 16 (61%) PR, in 3 (12%) CR. NC was observed in 7 hips (27%).
Eight months (mean) after the second LD-EBRT 18 hips were re-evaluated. PR was observed in 5 (28%) of these, CR in 6 (33%), and NC in 7 (39%).
Factors associated with remission
Remission (PR and CR) vs. no remission at the end of LD-EBRT was correlated in univariate analysis with inclusion of the total femoral head into the PTV (Table 1). None of the parameters reflecting the longitudinal extension of the PTV (distance between inferior field border and greater trochanter or minor trochanter, distance between superior field border, and socket edge) had any influence on treatment outcome. Even PTV volume was not predictive. Furthermore, the treatment technique (anterior–posterior vs. additional lateral fields), the fractionation (6 × 0.5 Gy vs. 6 × 1 Gy), and the duration of LD-EBRT had no influence on outcome. The only patient characteristic that was correlated with a successful therapy was night pain before LD-EBRT. All other variables showed no impact, especially duration of symptoms before LD-EBRT (<3 months vs. 3–12 months vs. >12 months), and BMI (or surface of planning CT as a surrogate parameter for missing BMI values). On the other hand, an initial increase in pain during LD-EBRT was significantly associated with treatment failure.
The results of univariable and multivariable binary logistic regression analyses for the identification of factors associated with successful RT for GTPS are summarized in Table 2. All variables with an α level below 0.2 were included in multivariable, risk-adjusted modeling. Hence, night pain before LD-EBRT and initial pain increase during LD-EBRT were considered in multivariable, risk-adjusted binary regression analysis. The developed multivariable regression model had good model fit regarding the prediction of remission as shown by the Hosmer–Lemeshow test.
In risk-adjusted analysis, an initial increase of symptoms at the beginning of LD-EBRT could be identified as statistically significant risk factor for failure of LD-EBRT (p = 0.007; OR 0.209; 95% CI 0.048–0.957). On the other hand, night pain before LD-EBRT was a statistically significant, independent factor for remission after LD-EBRT (p = 0.038; OR 3.484; 95% CI 1.004–12.6). These patients had a 3.5 higher chance to experience an amelioration of symptoms. All included variables in the multivariate regression model were independent of the endpoint remission as well as each other as shown in Fig. 2.
Shown is the loading plot of multivariable principal component analysis. No vectors are pointing in the same direction. Therefore all investigated variables in the multivariable binary regression analysis are independent of each other. Moreover, there is no co-linearity between the studied factors. Compl. fem. circumference in treatment portal complete femoral neck circumference included in PTV
Factors associated with three-month remission
Three months after LD-EBRT, pain at night before initiation of therapy (univariate analyses) and inclusion of the whole femoral neck circumference into the PTV in comparison to treatment of only the lateral aspect of the femoral neck and the soft tissue mantle (univariable and multivariable analyses) were predictive for remission (data not shown).
Discussion
To our knowledge, only two other series of LD-EBRT in GTPS have been published in the recent years. Treatment efficacy was quite comparable to our results. The first study comprised 34 patients who were treated with kilovoltage (kV) LD-EBRT with 1 Gy 3 times weekly up to a total dose of 6 Gy [16]. After 3 months only 15% experienced no change, while 38% reported complete and 53% partial remission. The second series of 26 patients reported response rates of 30% no change and about 40% complete remission during follow-up [17].
A historical series comprising about seven hips with calcareous deposits in the tendons of the gluteus and piriformis muscles dates back into 1937 [18]. Nearly all patients experienced pain relief under LD-EBRT.
These retrospective data are quite promising; however, randomized studies comparing LD-EBRT with shame irradiation or with other treatment modalities of GTPS to prove the efficacy of LD-EBRT have not been published to the best of our knowledge.
Furthermore, there is no information on target volume definition in LD-EBRT for this entity. Due to “common sense”, the greater trochanteric region has to be encompassed by the treatment portals. The specific interpretation of the area has been left to the treating radiation oncologist.
However, in the above-mentioned landmark studies by Dunn et al. [5] and Weeley et al. [6], at least two bursae are rather consistently to be found in each of three different anatomical areas:
-
Beneath the gluteus maximus muscle and the fascia lata:
-
The “deep bursa” (formerly described as “the trochanteric bursa” or “subgluteus maximus bursa”): centered over the lateral surface of the trochanter, separated from the bone by the distal tendon of the gluteus medius muscle and the origins of the vastus lateralis (Fig. 3a).
-
The “secondary deep bursa”: posterior to the deep bursa, covering the posterior border of the trochanter (Fig. 3b).
-
The “superficial subgluteus maximus bursa”: lateral to the deep bursa, located superficially, beneath the distal fibers of the gluteus maximus muscle/fascia lata.
-
And the so-called “gluteofemoral bursa”: located in the plane of the gluteus maximus muscle it is situated more caudally than all the other bursae (Fig. 3c). With its superior portion, it covers this lower third. While the other bursae are located within a mean distance of 3 cm (SD 2 cm) between the apex of the trochanter and the center of the respective bursa, the center of the gluteofemoral bursa is situated 5.7 cm (SD 0.3 cm) caudally of the apex. It is one of the largest bursa with about 10 cm² (SD 4.2 cm²).
-
-
Beneath the tendon of the gluteus medius muscle:
-
The “anterior subgluteus medius bursa”: separating the gluteus medius tendon from the gluteus minimus insertion and the anterior lateral surface of the trochanter (Fig. 3a).
-
The “posterior subgluteus medius bursa” (so-called “piriformis bursa”): covers parts of the superolateral part of the trochanter. Located between the deep surface of the gluteus medius tendon and the piriformis tendon (Fig. 3a).
-
-
Deep to the gluteus minimus tendon:
-
Two bursae: the “subgluteus minimus bursa” and the “secondary subgluteus minimus bursa”, covering the anterior aspect of the trochanter, located deep to the anterior border of the tendon of the gluteus minimus muscle (Fig. 3a).
-
a Location of several bursae in a planning CT scan of the right hip at apex of the greater trochanter. The gluteus maximus muscle is depicted in red, the gluteus medius in light green, and the gluteus minimus muscle in dark blue (more medial the iliopsoas muscle, also in dark blue). In bluish green, the fascia lata is delineated. In light purple the “deep bursa” is marked, in red the “anterior subgluteus medius bursa”, in light blue the “posterior subgluteus medius bursa”, and in yellow the “subgluteus minimus bursa”. b CT slice 0.6 cm more distal than in a. In addition to the structures in a, the “secondary deep bursa” is depicted in cyan (*). Please note the dorsal location of this bursa. c CT slice 2 cm more distal than in a. The gluteus maximus muscle is depicted in red, the iliopsoas muscle in dark blue. In bluish green, the fascia lata is delineated. The location of the “gluteofemoral bursa” is marked in brown (+)
Concerning these studies, the German guideline for radiotherapy of nonmalignant disorders recommends that “the superficial and deep, primary and secondary bursae of the gluteus maximus region” be included into the PTV [14]. Especially the distal localization of the gluteofemoral bursa is highlighted, as there is a high risk of missing its caudal edge.
However, there is no clinical evidence to support the claim to treat the entire bursae regions associated with the gluteus maximus muscle. Furthermore, two theoretical assumptions challenge this recommendation:
-
First, other therapeutic options like topic injections of steroids do not aim to treat all of the respective bursae of the affected tendinous insertion but are placed just into the most painful area [19].
-
Second, the main reason for GTPS are tears or inflammation in the tendons of the medius and minimus gluteus muscles [20]. At least their respective bursae should be irradiated, and not only the “… bursae of the gluteus maximus region”.
Still, our own data seem to support the above-mentioned recommendations. The inclusion of the entire femoral neck circumference reflects a generous inclusion especially of the more dorsally located secondary deep subgluteus maximus bursa and the gluteofemoral bursa, both associated with the gluteus maximus muscle and tendons (Fig. 3b and c). The coverage of these bursae was significantly associated with treatment success 3 months after LD-EBRT in our patients in comparison with the treatment of only the lateral aspect of the femoral neck and the corresponding soft tissue mantle.
As the deep bursa and the superficial subgluteus maximus bursa are located in close anatomical relation to the bursae of the gluteus medius and minimus tendons, and due to the anterior–posterior/posterior–anterior treatment planning technique, the medius, and minimus bursae will receive a sufficient dose in daily clinical practice. Taken together, our data partially support the field definition recommendations by the above cited German guidelines [14].
We investigated other, quite simply measured factors associated with field definition like distances between field borders and the greater trochanter, the minor trochanter, the socket edge, or inclusion of the entire femoral head into the PTV. Only the latter was predictive of treatment response at the end of the LD-EBRT series in univariate analysis. However, there is no convincing explanation for this result, as the bursae are not anatomically linked to the femoral head. The only explanation (besides a random effect) is that some patients in our collective also suffered from coxarthrosis—without being identified in anamnesis, clinical examination, or imaging. This is why we do not recommend to include the entire femoral head into the treatment volumes unless this result is confirmed in other studies.
Clinical factors associated with treatment response were initial pain increase during LD-EBRT and pain at night before start of LD-EBRT. The latter is very interesting, as night pain reflects a serious course of GTPS by interfering with restful night sleep. LD-EBRT has been particularly beneficial in these patients.
Data on treatment results of LD-EBRT in dependence of changes in pain intensity during the treatment series are scarce in contemporary studies. Our finding might be explained by the early date of first evaluation of treatment efficacy (last LD-EBRT day). Three months later, initial increase of symptoms during LD-EBRT was no longer correlated with treatment response. However, we reported a similar observation of a negative correlation between pain increase and treatment outcome in patients receiving LD-EBRT for thumb carpometacarpal osteoarthritis [21]. In the risk-adjusted analysis, an initial increase of symptoms at the beginning of EBRT was a statistically significant risk factor for failure of LD-EBRT. This is contrasted by observations of LD-EBRT in peritendinitis humeroscapularis [22]. In 73 patients (86 shoulders) initial increase of pain during the treatment course was significantly associated with a good response.
The main shortcoming of our study is its retrospective approach, which is why our results must be interpreted as a “generating hypothesis”. Only a prospectively randomized trial could prove that the inclusion of the entire femoral head is associated with a higher treatment response than just the irradiation of the lateral aspects of the femoral neck and the soft tissue mantle.
Furthermore, treatment response was just a graduation of the subjective impressions reported by the patients. We did not use the visual analog scale or validated questionnaires to try to objectify these results (e. g., modified Harris Hip Score or Hip Outcome Score). However, relying on the patients’ evaluation when differentiating between CR, PR, and NC is the mainstay of evaluating treatment efficacy of LD-EBRT in benign diseases since the landmark study by von Pannewitz in 1933 [23].
Conclusion
LD-EBRT represents a useful treatment option for patients suffering from GTPS. Three months after therapy two-thirds of the patients reported partial or complete symptom remission. Especially patients who suffered initially from nocturnal pain seemed to benefit. Concerning the definition of the treatment volume, our data suggest better treatment efficacy when the entire circumference of the femoral neck is encompassed.
References
Williams BS, Cohen SP (2009) Greater trochanteric pain syndrome: a review of anatomy, diagnosis and treatment. Anesth Analg 108:1662–1670
Kaltenborn A, Gutcke A (2014) Trauma in elderly patients – relevance for military surgery. Wehrmed Monatsschr 58:413–415
Strauss EJ, Nho SJ, Kelly BT (2010) Greater trochanteric pain syndrome. Sports Med Arthrosc 18:113–119
Chowdhury R, Naaseri S, Lee J et al (2014) Imaging and management of greater trochanteric pain syndrome. Postgrad Med J 90:576–581
Dunn T, Heller CA, McCarthy SW et al (2003) Anatomical study of the “trochanteric bursa”. Clin Anat 16:233–240
Woodley SJ, Mercer SR, Nicholson HD (2008) Morphology of the bursae associated with the greater trochanter of the femur. J Bone Joint Surg Am 90:284–294
Rödel F, Frey B, Gaipl US et al (2012) Modulation of Inflammatory Immune Reactions by Low-Dose Ionizing Radiation: Molecular Mechanisms and Clinical Application. Curr Med Chem 19:1741–1750
Niewald M, Seegenschmiedt MH, Micke O et al (2012) Randomized, multicenter trial on the effect of radiation therapy on plantar fasciitis (painful heel spur) comparing a standard dose with a very low dose: Mature results after 12 months’ follow-up. Int J Radiat Oncol Biol Phys 84:e455–e462
Heyd R, Tselis N, Ackermann H et al (2007) Radiation therapy for painful heel spurs. Strahlenther Onkol 183:3–9
Ott OJ, Jeremias C, Gaipl US et al (2014) Radiotherapy for benign calcaneodynia: long-term results of the Erlangen Dose Optimization (EDO) trial. Strahlenther Onkol 190:671–675
Ott OJ, Jeremias C, Gaipl US et al (2015) Radiotherapy for benign achillodynia. Long-term results of the Erlangen Dose Optimization Trial. Strahlenther Onkol 191:979–984
Ott OJ, Hertel S, Gaipl US et al (2014) The Erlangen Dose Optimization Trial for radiotherapy of benign painful shoulder syndrome. Long-term results. Strahlenther Onkol 190:394–398
Ott OJ, Hertel S, Gaipl US et al (2014) The Erlangen Dose Optimization trial for low-dose radiotherapy of benign painful elbow syndrome. Long-term results. Strahlenther Onkol 190:293–297
Ott OJ, Niewald M, Weitmann H‑J et al (2015) DEGRO guidelines for the radiotherapy of non-malignant disorders. Part II: painful degenerative skeletal disorders. Strahlenther Onkol 191:1–6
Hosmer DW, Lemeshow S (2013) Applied logistic regression. Wiley, New York
Glatzel M, Baesecke S, Krauss A (2000) Ergebnisse der Strahlentherapie bei therapierefraktärer Insertionstendopathie am Trochanter Major. Strahlenther Onkol 176(Suppl. 1):92
Olschewski T, Klein II (2010) Funktionelle Radiotherapie bei der Bursitis trochanterica. Strahlenther Onkol 186(Suppl. 1):40
de Lorimier AA (1937) Roentgen therapy in acute para-arthritis. Am J Roentgenol 38:178–195
Shbeeb MI, O’Duffy JD, Michet CJ Jr (1996) Evaluation of glucocorticosteroid injection for the treatment of trochanteric bursitis. J Rheumatol 23:2104–2106
Williams BS, Cohen SP (2009) Greater trochanteric pain syndrome: A review of anatomy, diagnosis and treatment. Anesth Analg 108:1662–1670
Kaltenborn A, Bulling E, Nitsche M et al (2016) The field size matters: low dose external beam radiotherapy for thumb carpometacarpal osteoarthritis: Importance of field size. Strahlenther Onkol 192:582–588
Seegenschmiedt MH, Keilholz L (1998) Epicondylopathia humeri (EPH) and peritendinitis humeroscapularis (PHS): evaluation of radiation therapy long-term results and literature review. Radiother Oncol 47:17–28
von Pannewitz G (1933) Die Röntgentherapie der Arthritis deformans. Klinische und experimentelle Untersuchungen. Ergeb Med Strahlenforsch 6:62–126
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. Kaltenborn, U.M. Carl, T. Hinsche, M. Nitsche and R.M. Hermann declare that they have no competing interest.
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Kaltenborn, A., Carl, U.M., Hinsche, T. et al. Low-dose external beam radiotherapy for greater trochanteric pain syndrome. Strahlenther Onkol 193, 260–268 (2017). https://doi.org/10.1007/s00066-016-1071-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-016-1071-z
Keywords
- Bursitis trochanterica
- Greater trochanteric pain syndrome
- Low-dose radiotherapy
- Target volume definition
- Bursae