Abstract
Purpose
To summarize the updated DEGRO consensus S2e guideline recommendations for the treatment of benign symptomatic functional disorders with low-dose radiotherapy.
Materials and methods
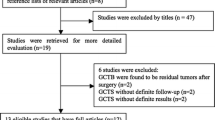
This overview reports on the role of low-dose radiotherapy in the treatment of functional disorders in cases of heterotopic ossification (HO) and Graves orbitopathy (GO). The most relevant aspects of the DEGRO S2e Consensus Guideline “Radiation Therapy of Benign Diseases 2014” regarding diagnostics, treatment decision, dose prescription, as well as performance of radiotherapy and results are summarized.
Results
For both indications (HO, GO), retrospective and some prospective analyses have shown remarkable effects in terms of symptom relief. Nevertheless, the level of evidence (LoE) and the grade of recommendation (GR) vary: LoE 1–2 and GR A-B (HO), LoE 2 and GR B (GO).
Conclusion
Low-dose radiotherapy for benign symptomatic functional disorders has proven to be effective, according to different authors, for 25–100 % of the patients studied and therefore it may be a reasonable prophylactic and therapeutic option if noninvasive or invasive methods have been used without persistent success.
For HO, a single-fraction dose of 7–8 Gy or fractionated radiation with five fractions of 3.5 Gy is recommended. For GO, single-fraction doses of 0.3–2.0 Gy, and total doses of 2.4–20 Gy/series, applied in one daily fraction are recommended.
Zusammenfassung
Zielsetzung
Zusammenfassung der Empfehlungen der DEGRO-S2e-Leitlinie zur Niedrigdosis-Radiotherapie von gutartigen symptomatischen funktionellen Erkrankungen.
Material und Methoden
Die vorliegende Leitlinie berichtet über die Bedeutung der Niedrigdosis-Radiotherapie in der Behandlung von funktionellen Erkrankungen, in diesem Fall von heterotoper Ossifikation (HO) und endokriner Orbitopathie (EO). Es werden die wichtigsten Aspekte der aktuellen DEGRO-S2e-Konsensusleitlinie „Strahlentherapie gutartiger Erkrankungen 2014“ bezüglich Diagnostik, Therapieentscheidungen, Dosisempfehlungen und Empfehlungen zur Durchführung der Radiotherapie zusammengefasst.
Ergebnisse
Für beide Entitäten (HO, EO) wurde in zahlreichen retrospektiven und einigen prospektiven Untersuchungen ein bemerkenswerter Effekt der Niedrigdosis-Radiotherapie im Sinne einer Symptomreduktion beschrieben. Je nach Entität wurden verschiedene Evidenzlevel (LoE) festgestellt, so dass unterschiedliche Empfehlungsgrade (GR) für den Einsatz der Radiotherapie ausgesprochen wurden: LoE 1–2 und GR A–B (HO), LoE 2 und GR B (EO).
Schlussfolgerung
Die Niedrigdosis-Radiotherapie von benignen symptomatischen funktionellen Erkrankungen ist nach Ansicht verschiedener Autoren bei einem Anteil von 25–100 % der untersuchten Patienten effektiv und ist eine gut begründbare Therapieoption für Patienten, bei denen konservative oder operative Verfahren zu keiner anhaltenden Verbesserung geführt haben. Für die HO wird die Einzeitbestrahlung mit 7–8 Gy oder die fraktionierte Bestrahlung mit 5 × 3,5 Gy empfohlen. Für die EO werden Einzeldosen von 0,3–2,0 Gy und Gesamtdosen von 2,4–20 Gy/Serie mit täglicher Bestrahlung befürwortet.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Heterotopic ossifications are defined as new bone formations arising in the soft tissue outside the original skeleton system [5].
“Muscle calcifications” were first reported by Goldberg in 1877 in paraplegic patients. The first attempt to classify so-called myositis ossificans was made in 1910.
Heterotopic ossifications are clinically relevant with movement restriction and pain only starting from a certain expansion. The etiology is not completely clarified, whereby it is assumed that an inflammatory stimulus, e.g., by a bone trauma, leads to the release of growth factors that cause a differentiation from undifferentiated mesenchymal stem cells or myoblasts to osteoblasts. The hypothesis for the effect of irradiation on the prophylaxis of heterotopic ossification assumes that the postulated pluripotent mesenchymal stem cells can be arrested by irradiation before entering in the differentiation phase, which takes place in the first few days after surgery. If the differentiation has already begun, it is no longer affected by the irradiation [40].
Today, several risk factors for heterotopic ossifications are recognized. A major risk factor is the already existing ipsi- or contralateral heterotopic ossification. Individual factors such as, for example, age and predisposing illnesses (e.g., chronic polyarthritis) have been reported as further risk factors.
These risk factors allow for the development of appropriate risk scores and subsequently, depending on these scores, for deciding if and when such a prophylactic therapy should be performed. Due to the frequency of occurrence of heterotopic ossifications, a primary ossification prophylaxis is indicated in the presence of one or more risk factors. Koelbl et al. [19] recommended a risk score for the development of heterotopic ossification after hip replacement surgery consisting of three different risk classes (Table 1).
Heterotopic ossifications can be differentiated into three main groups:
-
Traumatic heterotopic ossification
-
Nontraumatic heterotopic ossification
-
Neurologic heterotopic ossification
The group of heterotopic ossification caused by trauma (accident or surgery) is the most frequent and rarely causes differential diagnostic problems because of the close local and temporal relationship with the traumatic event. It occurs in up to 25 % of patients following fractured acetabulum, [14], after hip joint replacement with endoprosthesis it occurs in 16–90 % of patients depending on the risk profile [31], and after fracture of the elbow joint in 50 % of patients [16]. The frequency of heterotopic ossification after knee joint dislocation is indicated to be 26 % in the literature with [37].
Nontraumatic heterotopic ossification after burns, for example, is rare and usually occurs after burns of at least 20 % of the body surface area only and in soft tissue structures close to the joints, particularly in the proximity of the elbow. Their usual frequency of occurrence lies between 0.15 and 3 % [30].
The neurologic type of heterotopic ossification occurs in the soft parts in up to 20 % of patients with traumatic paraplegia [3].
The earliest heterotopic ossifications are visible 2 weeks after trauma on a conventional radiographic image (X-ray view). The classification of the severity of heterotopic ossification is usually deduced from the visible expansion on the X-ray view, e.g., the heterotopic ossification within the range of the hip joint after hip joint replacement based on the classification of Brooker [6]. The classification of Brooker defines four degrees (Table 2). Only grades III and IV are clinically relevant with symptoms.
Graves orbitopathy occurs at a rate of 10 % among patients suffering thyroid diseases, over 90 % of Graves orbitopathy patients exhibit Basedow’s disease, and 60 % of Graves orbitopathy cases are associated with hyperthyroidism. Genetic predisposition and tobacco consumption are risk factors.
Graves orbitopathy is a thyroid-associated autoimmune disorder. The precise pathomechanism is not known, but it is understood to be an inflammatory process with evidence of autoantibodies against TSH receptors (thyrotropin-receptor antibody, TRAK) in the conjunctive tissue of the eye muscles. Other receptor antibodies, such as insulin-like growth factors, are seemingly important. The immune response causes an increase in orbital muscles, fat, and connective tissue and thereby augments the distance between the orbital wall and ocular bulb. Exophthalmus, reduced eye motility, and double vision often appear. This clinical diagnosis mostly includes thyroid increase and tachycardia as part of Basedow’s disease. Further diagnostic imaging allows one to assess the degree of severity of the disease; magnetic resonance imaging (MRI) serves for the evaluation of the inflammatory component. For classification of disease progression and stages, no standard is settled [1]. Since 1969 the NOSPECS scheme (no signs or symptoms; only signs, no symptoms; soft tissue involvement; proptosis; extraocular muscle involvement; corneal involvement; sight loss) of the American Thyroid Association is in use (Table 3). Moreover, the LEMO classification (lid edema, exophthalmus, muscle change, optic tract involvement) is established, a practical diversification of the NOSPECS scheme and initially recommended in 1991 by Boergen and Pickardt. These two classifications play an important part before and during the course of treatment for the evaluation of response or progress of disease. They give an additional survey of the validity of significant symptoms.
More detailed information and references may be found in the complete version of the guideline, which is available on the DEGRO homepage (http://www.degro.org).
Non-radiotherapeutic treatment options
For heterotopic ossification a resection is the only causal therapy. Symptoms can be treated with pain medication. The objective of treatment is the prevention of a re-emergence of the heterotopic ossification after its removal or prophylactic therapy in the presence of high-risk factors.
The sole postoperative medication of nonsteroidal anti-inflammatory drugs (NSAID) over at least 3–6 weeks appears also potent. Indomethacin (Amuno®), an inhibitor of prostaglandin synthesis, was effective in different studies involving high-risk patients [8]. Prostaglandins are mediators of inflammation, i.e., prostaglandin suppresses the inflammatory reaction and the proliferation of mesenchymal cells. It is used in different dosages immediately after the operation for 3–6 weeks. However, it can frequently cause gastrointestinal side effects, so that patients with a medical history of gastric ulcer must be excluded from this therapy.
In Graves orbitopathy no treatment method with causal mechanism exists to date [10]. Therapy of GO in general is effective in the handling of symptoms and the application of cortisone is the treatment of choice. Other treatment options in mild cases are the use of tear substitutes or ointment. Experimental procedures include the use of biological agents, in particular rituximab.
Surgical intervention is not used until the inactive, chronic fibrotic phase of the disease is reached and the persistence of the syndrome for at least 6 months has been observed. The chronological order of and suitable intervals between appropriate surgical measures have to be respected with regard to the priorities of firstly the orbita, secondly the outer eye muscles, and finally the eyelids.
The response to different treatment methods according to the duration of symptoms and the stages found in the literature is shown in Table 4.
Antiproliferative control after low-dose radiotherapy
Pre- or postoperative radiotherapy of the hip region is one treatment modality for the reduction of the occurrence of heterotopic ossifications following hip joint replacement. Radiotherapy is most effective if applied within the time window of up to 4 h before and up to 72 h after surgery [19]. For patients with major risk factors, postoperative fractionated radiotherapy is superior to preoperative radiotherapy [25]. The rate of heterotopic ossification after hip joint replacement can be reduced from up to 90 % to under 10 % using pre- or postoperative radiotherapy in patients with risk factors.
Experiences concerning repeated radiotherapy after hip joint replacement are rare, but have been documented as also being effective. Because of the time interval between the first and second irradiation generally amounting to several years, the cumulative dose can be tolerated especially by older patients, accordingto Lo et al. [21]. However, some of the patients are younger people under the age of 40. Since the lifetime of a hip joint replacement is 10–15 years, one should bear in mind that the replacement has to be repeated several times.
With further fractures close to other joints, prophylactic treatment with radiotherapy to prevent heterotopic ossification is likewise successful [25].
Prophylactic radiotherapy is well tolerated, and impaired wound healing has not been reported. So far no patient was observed to develop a malignant tumor within the radiation field in the follow-up. Since radiation-induced tumors are extremely rare and only arise after latencies of 10–30 years, the risk is not relevant for most of the patients with a median age of 65 years.
The clinical use of radiotherapy in Graves orbitopathy is controversial. In Germany, radiation treatment is applied in mid-level cases (classes II–V according to NOSPECS) especially with dysfunction of the eye muscles [2, 4, 12]. About 65–75 % of patients with GO show good or excellent response rates after radiation [24, 26]. The response and success metrics are shown in Table 5. The anti-inflammatory as well as the anti-proliferative effect of radiotherapy should bring a benefit by decreasing the length of the inflammatory phase and preventing late complications (e.g., optic nerve compression with loss of vision or eye muscle fixation out of position) [11]. Before starting radiation treatment, euthyroid metabolism should be present.
Current recommendations on radiotherapy
The application of radiotherapy for avoidance of heterotopic ossification after hip joint replacement was first proven to be efficient in 48 high-risk patients using ten times a single daily dose of 2 Gy in a postoperative setting by Coventry and Scanlon in 1981 [9]. However, Lo et al. showed as early as in 1988 that a single dose of 7 Gy is also effective [21].
Preoperative irradiation could likewise reduce the rate of ossification if the prophylactic treatment is applied no longer than 4 h before surgery [19].
Based on many prospective studies, the general recommendations for dosage and fractionation in radiation prophylaxis of heterotopic ossification are as follows. A single radiation dose between 7 and 8 Gy within the described time window of up to 4 h before and up to 72 h after surgery should be applied. However, for patients with major risk factors, postoperative fractionated radiotherapy applying five fractions of 3.5 Gy daily in a single dose is recommended [9, 19, 35].
The most comprehensive experience in defining the planning target volume (PTV) exists for irradiation after hip joint replacement. The PTV covers the typical localizations of heterotopic ossifications [13]. Usually the field size amounts to 14 × 14 cm. The cranial field border has to be about 3 cm above the acetabulum, the caudal field border encases about two thirds of the proximal part of the implant, offering the advantage that large parts of the prosthesis shank are not inside the irradiation volume and thus the risk of a reduced shank stability is avoided. Structures at risk in the pelvic region, like the small intestine or rectum, can be spared.
The point of dosage of the anterior-posterior—posterior-anterior field technique is at the center of the body. The radiotherapy takes place at a linear accelerator with high photon energy. Other skeletal regions should be treated accordingly to the described approach for hip joint replacement.
The radiotherapy of Graves orbitopathy is carried out at a linear accelerator with 4–6 MV photons. A mask fixation system is used for positioning and acquisition of computed tomography (CT) images.
The clinical target volume (CTV) and the PTV are determined. The PTV is defined as: dorsal margin of orbita at Zinn’s zonule, including the posterior two thirds of the ocular bulb as far as 6 mm behind the corneal limbus, covering the insertion of the extraocular muscles.
During the radiation planning process, anatomical proportions in CT imaging must be considered. The distance between the cornea surface and the back face of the lens amounts to 8 mm on average. Comparison of conventional and virtual simulation demonstrates the external eyelid angle as a practical orientation for guidance of the lateral radiation field. Moreover, the corneal limbus can serve as guidance for field positioning, whereas the bony canthus is inadequate for guidance in field positioning. Three-dimensional (3D) radiation therapy planning thus results in field sizes of at least 5 × 5 cm or 6 × 5 cm for obtaining sufficient dose coverage of the entire PTV [15]. In the majority of cases, lateral opposing fields are used with compensation of divergence for optimal protection of the lenses. Further radiation techniques are: (1) half-beam technique with middle-block or (2) rotation technique with central shielding for lens protection [23, 39].
There are no general recommendations for dosage or fractionation in the radiation treatment of Graves orbitopathy. According to a representative nationwide questionnaire of the working team “benign diseases” of the DEGRO (Deutsche Gesellschaft für Radioonkologie, German Society for Radiation Oncology) in most radio-oncological institutions in Germany the radiotherapy of Graves orbitopathy is standard with total doses of 16–20 Gy and a fractionation of five fractions of 2 Gy per week. To date, it remains unclear if considerably lower doses are equally effective—depending on the stage of the disease. Lower total doses could reduce the potential risk for radiogenic induction of secondary tumors [7, 18, 20, 27, 28, 38].
Kahaly et al. in 2000 conducted a randomized three-armed study in a total of 65 patients, who showed moderate Graves orbitopathy of classes II–V according to NOSPECS. Patients of group A received 20 fractions of 1 Gy each, once a week up to 20 Gy: long duration of treatment, low single dose, high total dose. Patients of group B received ten fractions of 1 Gy each, five times a week up to 10 Gy: intermediate duration of treatment, low single dose, intermediate total dose. Patients of group C received ten fractions of 2 Gy each, five times a week up to 20 Gy: short duration of treatment, high single dose, high total dose. Patients of all three groups showed equal response rates with regard to the improvement of ophthalmological symptoms and changes on MRI. However, group A patients A were obviously superior to those of the two other groups concerning the reduction of swelling and eye motility [17].
Gerling et al. in 2003 in another randomized trial on low-dose radiotherapy checked two arms of patients as follows: radiotherapy with eight fractions of 0.3 Gy each, five times a week up to 2.4 Gy (n = 43 patients) versus standard radiation with eight fractions of 2 Gy each up to 16 Gy (n = 43 patients). The clinical results of both arms were equally effective.
Gorman et al. in 2001 conducted a double-blind randomized study, with each patient undergoing radiotherapy of one randomly selected orbit with a standard dose of 20 Gy, five times a week at 2 Gy each; whereas sham therapy (pseudo-radiation) was given to the other side. The clinical effectiveness of both modalities was the same. However, this cannot be assigned to a placebo effect solely, as the pseudo-radiated orbit received a contingent of scattered rays of approximately 0.4 Gy per fraction in the orbital cavity, constituting in fact a “low-dose radiotherapy.”
In Graves orbitopathy, the use of low-dose radiotherapy seems to achieve the highest response rates in the early inflammatory phase [34]. In advanced stages of disease, higher radiation doses are required to obtain the same effectiveness [32, 33]. The external beam radiation treatment can be combined with systemic application of glucocorticoids [22, 29, 36]. Combined modality treatment is often applied in severe cases. In a randomized trial, the potency of combined treatment was superior in contrast to glucocorticoid therapy alone [22, 29, 36].
Summary
To avoid heterotopic ossification, a single radiation dose of 7–8 Gy respecting the described time window is effective; in patients with major risk factors the postoperative fractionated radiotherapy with five fractions of 3.5-Gy daily single doses is recommended. The level of evidence (LoE) and the grade of recommendation (GR) vary: patients with endoprosthesis or resection of HO should get radiotherapy with LoE 1 and GR A; fractures close to joints should get radiotherapy with LoE 2 and GR B.
In Graves orbitopathy, retrobulbar radiotherapy is carried out using lateral opposing fields with protection of the lenses. The dosage should be adapted to the individual phase of disease: in the early inflammatory phase, single dose of 0.3–2.0 Gy, eight fractions, daily radiation, total dose 2.4–16 Gy; in advanced inflammatory phase, single dose 2.0 Gy, eight to ten fractions, daily radiation, total dose 16–20 Gy. To avoid severe ophthalmologic symptoms, the efficacy of radiation could be improved by the use of a reduced single dose of 1 Gy and the prolongation of therapy duration with radiation only once a week. In Graves orbitopathy with manifest dysfunction of the eye muscles, antiproliferative external beam radiotherapy is recommended with LoE 2 andGR B.
References
American Thyroid Association (1992) Classification of eye changes of Graves’ disease. Thyroid 2:235–236
Appelqvist P, Salmo M, Rissanen P (1990) Radiotherapy in emergency treatment of malignant exophthalmos. Strahlenther Onkol 166:190–193
Banovac K, Sherman AL, Estores IM et al (2004) Prevention and treatment of heterotopic ossification after spinal cord injury. J Spinal Cord Med 27:376–382
Bartalena L, Marcocci C, Manetti L et al (1998) Orbital radiotherapy for Graves’ ophthalmopathy. Thyroid 8:439–441
Bossche LV, Vanderstraeten G (2005) Heterotopic ossification: a review. J Rehabil Med 37:129–136
Brooker AF, Bowerman JW, Robinson RA et al (1973) Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am 55:1629–1632
Brualla L, Sempau J, Zaragoza FJ et al (2013) Accurate estimation of dose distributions inside an eye irradiated with 106Ru plaques. Strahlenther Onkol 189:68–73
Burd TA, Lowry KJ, Anglen JO (2001) Indomethacin compared with localized irradiation for the prevention of heterotopic ossification following surgical treatment of acetabular fractures. J Bone Joint Surg Am 83:1783–1788
Coventry MB, Scanlon PW (1981) The use of radiation to discourage ectopic bone. A nine-year study in surgery about the hip. J Bone Joint Surg Am 63:201–208
DeGroot LJ, Gorman CA, Pinchera A et al (1995) Therapeutic controversies. Radiation and Graves’ ophthalmopathy. J Clin Endocrinol Metab 80:339–349
Eich HT, Micke O, Seegenschmiedt MH (2007) Radiotherapy of Graves’ ophthalmopathy-state of the art and review of the literature. Rontgenpraxis 56:137–144
Friedrich A, Kamprad F, Goldmann A (1997) Clinical importance of radiotherapy in the treatment of Graves’ Disease. In: Wiegel T, Bornfeld N, Foerster MH, Hinkelbein W (eds) Radiotherapy of ocular disease. Front Radiat Ther Oncol. Basel: Karger 30:206–217
Gehl HB, Karstens JH, Casser HR et al (1991) The prevention of ectopic ossification in total hip endoprostheses. Studies on field volume, total dosage and timing of postoperative radiotherapy. Röntgenpraxis 44:117–121
Giannoudis PV, Grotz MR, Papakostidis C et al (2005) Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J Bone Joint Surg Br 87:2–9
Gripp S, Doeker R, Glag M et al (2000) Konventionelle und virtuelle Simulation bei der Retrobulbärbestrahlung. Strahlenther Onkol 176:131–134
Heyd R, Buhleier T, Zamboglou N (2009). Radiation therapy for prevention of heterotopic ossification about the elbow. Strahlenther Onkol 185:506–511
Kahaly G, Rösler HP, Pitz S et al (2000) Low versus high dose radiotherapy for Graves ophthalmopathy. J Clin Endocrinol Metab 85:102–108
Kocher M, Treuer H, Hoevels M et al (2013) Endocrine and visual function after fractionated stereotactic radiotherapy of perioptic tumors. Strahlenther Onkol 189:137–141
Koelbl O, Seufert J, Pohl F et al (2003) Preoperative irradiation for prevention of heterotopic ossification following prosthetic total hip replacement results of a prospective study in 462 hips. Strahlenther Onkol 179:767–773
Kriss JP, Petersen IA, Donaldson SS et al (1989) Supervoltage orbital radiotherapy for progressive Graves’ ophthalmopathy: results of a twenty year experience. Acta Endocrinol (Copenh) 121:154–159
Lo TC, Healy WL (2001). Re-irradiation for prophylaxis of heterotopic ossification after hip surgery. Br J Radiol 74:503–506
Marcocci C, Bartalena L, Panicucci M et al (1987) Orbital cobalt irradiation combined with retrobulbar or systematic cortico-steroids for Graves’ ophthalmopathy: a comparative study. Clin Endocrinol 27:33–42
Olivotto IA, Ludgate CM, Allen LH et al (1985) Supervoltage radiotherapy for Graves’ ophthalmopathy: CCABC technique and results. Int J Radiat Oncol Biol Phys 11:2085–2090
van Ouwerkerk BM, Wijngaarde R, Hennemann G (1985). Radiotherapy of severe ophthalmic Graves’ disease. J Endocrinol Invest 8:241–247
Pakos EE, Pitouli EJ, Tsekeris PG et al (2006) Prevention of heterotopic ossification in high-risk patients with total hip arthroplasty: the experience of a combined therapeutic protocol. Int Orthop 30:79–83
Palmer D, Greenberg P, Cornell P et al (1987) Radiation therapy for Graves’ ophthalmopathy: retrospective analysis. Int J Radiat Oncol Biol Phys 13:1815–1820
Petersen IA, Donaldson SS, McDougall IR et al (1990) Prognostic factors in the radiotherapy of Graves’ ophthalmopathy. Int J Radiat Oncol Biol Phys 19:259–264
Pfluger T, Wendt T, Toroutoglou N et al (1990) Retrobulbärbestrahlung bei endokriner Ophthalmopathie: Vergleich zwischen 10 und 16 Gy Herddosis. Strahlenther Onkol 166:673–677
Prummel MF, Mourits M, Blank L et al (1993) Randomised double-blind trial of prednisone versus radiotherapy in Graves’ ophthalmopathy. Lancet 342:949–954
Richards AM, Klaassen MF (1997) Heterotopic ossification after severe burns: a report of three cases and review of the literature. Burns 23:64–68
Rosendahl S, Christoffersen JK, Norgaard M (1977) Para-articular ossifications following hip replacement. Acta Orthop Scand 48:400–404
Sandler HM, Rubenstein JH, Fowble BL et al (1989) Results of radiotherapy for thyroid ophthalmopathy. Int J Radiat Oncol Biol Phys 17:823–827
Seegenschmiedt MH, Becker W, Gusek G et al (1995) Megavoltage radiotherapy for severe and refractory progressive Graves’ ophthalmopathy: comparison of scoring systems and long-term results. Int J Radiat Oncol Biol Phys 32:286
Seegenschmiedt MH, Keilholz L, Gusek-Schneider G et al (1998) Radiotherapie bei progredienter endokriner Orbitopathie: Langzeitresultate und Klassifikationen im Vergleich. Strahlenther Onkol 174:449–456
Seegenschmiedt MH, Makowski HB, Micke O (2001). German Cooperative Group on Radiotherapy for Benign Diseases. Radiation prophylaxis for heterotopic ossification about the hip joint—a multicenter study. Int J Radiat Biol Phys 51:756–765
Staar S, Müller RP, Hammer M et al (1997) Results and prognostic factors in retrobulbar radiotherapy combined with systemic corticosteroids for endocrine orbitopathy (Graves’ Disease). In: Wiegel T, Bornfeld N, Foerster MH, Hinkelbein W (eds) Radiotherapy of ocular disease. Front Radiat Ther Oncol. Basel: Karger, 30:206–217
Stannard JP, Wilson TC, Sheils TM et al (2002) Heterotopic ossification associated with knee dislocation. Arthroscopy 18:835–839
Trott KR (1994). Therapeutic effects of low radiation doses. Strahlenther Onkol 170:1–12
Uhlenbrock D, Fischer HJ, Rohwerder R (1984) Strahlentherapie der endokrinen Ophthalmopathie—Auswertung von 56 Fällen. Strahlentherapie 160:485–491
Zeckey C, Hildebrand F, Frink M et al (2011) Heterotopic ossifications following implant surgery-epidemiology, therapeutical approaches and current concepts. Semin Immunopathol 33:273–286
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
G. Reinartz, H.T. Eich, F. Pohl, and the German Cooperative Group on Radiotherapy for Benign Diseases state that there are no conflicts of interest.
Rights and permissions
About this article
Cite this article
Reinartz, G., Eich, H., Pohl, F. et al. DEGRO practical guidelines for the radiotherapy of non-malignant disorders – Part IV. Strahlenther Onkol 191, 295–302 (2015). https://doi.org/10.1007/s00066-014-0789-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-014-0789-8
Keywords
- Heterotopic ossification
- Graves orbitopathy
- Benign functional disease
- Low-dose radiotherapy
- German S2e guideline