Abstract
Purpose
To evaluate the feasibility of hypofractionation with SIB in all settings in Germany to prepare a multicenter treatment comparison.
Methods
Eligible patients had histopathologically confirmed breast cancer operated by BCS. Patients received WBI 40.0 Gy in 16 fractions of 2.5 Gy. A SIB with 0.5 Gy per fraction was administered to the tumor bed, thereby giving 48.0 Gy in 16 fractions to the boost-PTV sparing heart, LAD, lung, contralateral breast. The primary study objective was feasibility, administration of specified dose in 16 fractions within 22–29 days with adherence to certain dose constraints (heart; LAD; contralateral breast); secondary endpoints were toxicity, QoL.
Results
151 patients were recruited from 7 institutions between 07/11-10/12. 10 patients met exclusion criteria prior to irradiation. All but two patients (99 %) received the prescribed dose in the PTVs. Adherence to dose constraints and time limits was achieved in 89 % (95 % CI 82 % to 93 %). 11 AE were reported in 10 patients; five related to concurrent endocrine therapy. Two of the AEs were related to radiotherapy: grade 3 hot flushes in two cases. QoL remained unchanged.
Conclusion
Hypofractionation with a SIB is feasible and was well tolerated in this study.
Zusammenfassung
Hintergrund
Die ARO-2010-01-Studie prüfte die Durchführbarkeit einer hypofraktionierten Bestrahlung mit simultan-integriertem Boost (SIB) in unterschiedlichen Versorgungseinrichtungen zur Vorbereitung einer multizentrischen Vergleichsstudie.
Methoden
In die Studie rekrutiert wurden Patientinnen mit histopathologisch gesichertem Mammakarzinom nach brusterhaltender Operation. Bestrahlt wurde die Brust mit 40,0 Gy in 16 Fraktionen à 2,5 Gy Einzeldosis; zusätzlich wurde bei jeder Fraktion ein simultan- integrierter Boost mit 0,5 Gy appliziert, so dass im Boost-PTV (Planungszielvolumen) eine Dosis von 48 Gy in 16 Fraktionen erreicht wurde. Das primäre Zielkriterium war die Durchführbarkeit, definiert als Verabreichung von 48 Gy GD in 16 Fraktionen in mindestens 22 d bis maximal 29 d Therapiezeit unter Einhaltung von Grenzdosen (Lunge, Herz, LAD, kontralaterale Brust); sekundäre Endpunkte waren Toxizität und Lebensqualität.
Ergebnisse
Zwischen 07/2011 und 10/2012 wurden 151 Patientinnen in 7 Prüfzentren rekrutiert. Bei 10 Patientinnen wurden vor der Strahlentherapie Ausschlusskriterien festgestellt. Fast alle Patientinnen (99 %) erhielten die verschriebene Dosis im PTV. Grenzdosen und Zeitlimits wurden in 89 % (95 % CI 82 % bis 93 %) eingehalten. 11 unerwünschte Ereignisse wurden bei 10 Patientinnen gemeldet; fünf in Verbindung mit gleichzeitiger endokriner Therapie. In 2 Fällen wurde eine kausale Beziehung zur Strahlentherapie angegeben: Grad-3-Hitzewallungen. Die Lebensqualität blieb unverändert.
Schlussfolgerungen
Die hypofraktionierte Bestrahlung mit simultan-integriertem Boost konnte in dieser multizentrischen Studie in Praxen und Strahlenkliniken problemlos durchgeführt werden. Die Verträglichkeit war in dieser Studie gut.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Adjuvant radiotherapy after breast-conserving surgery (BCS) is a cornerstone of breast-preserving treatment. According to standard guidelines, radiotherapy is administered as normofractionated whole breast irradiation (WBI) in 25–28 fractions up to 50 Gy followed by a sequential boost to the tumor bed with 5–8 fractions up to 10–16 Gy. Radiotherapy consistently reduces the risk of local relapse in the ipsilateral breast and improves overall survival in high-risk patients [1–3]. The boost further improves local control [4–6].
Recently, results of four randomized trials recruiting 7,095 patients treated by whole breast hypofractionation have shown local control and adverse effects to be comparable with a conventional regimen [7–10]. Doses of 39.0–42.0 Gy in 13–16 fractions are considered to be equivalent to 50.0 Gy in 25 fractions by conventional fractionation but the 13 × 3 Gy regimen (39 Gy in 5 weeks) or 13.3 × 3 Gy (42.9 Gy in 5 weeks) was associated with lower local control rates (local failure rates of 7.1 and 9.1 %) [10]. However, the hypofractionation regimens referred only to homogenous WBI. The issue of boost radiation was not addressed in these studies primarily due to the uncertain priority of the boost at the time of conceptual design phase of these trials.
According to the current statement of the German and the Austrian Societies of Radiooncology (DEGRO/ÖGRO), two hypofractionated regimens can be recommended for shortening time: either conventionally fractionated WBI with a simultaneous-integrated boost (SIB) or hypofractionated WBI plus a sequential normofractionated boost as alternative for selected patients [11, 12]. Both regimens reduce the overall treatment time to about 5 weeks. The combination of hypofractionated WBI with a SIB can further shorten the treatment time down to about 3 weeks, but this regimen is currently considered as investigative and its use is so far recommended only within clinical trials. Recently, first clinical results of three prospective studies (one of these was a randomized trial) investigating similar approaches (hypofractionation plus SIB) have been published [13–15]. All trials confirm in small patient groups that incorporating SIB into hypofractionation is feasible with a tendency for fewer side effects. The results of the small randomized trial hint at a benefit with regard to late lung toxicity [14].
We initiated this prospective trial to investigate the feasibility of hypofractionation with SIB in patients with early breast cancer. ARO 2010-01 is one of the first German trials evaluating this combined experimental hypofractionation regimen. The primary endpoint of this multicenter phase II study was feasibility.
Patients and methods
The study was conducted according to the principles of the Declaration of Helsinki and Good Clinical Practice guidelines. The Ethics Committee, University of Lübeck (No. 09-194) and all local review boards of the participating institutions approved of this study. Each patient gave written informed consent before being included. The study has been awarded the “Certificate of Quality A” by the German Cancer Society as proof of compliance to clinical trial guidelines and scientific impact.
Patients
The eligibility criteria included women aged 18 years or older with histopathologically confirmed breast cancer operated by BCS with clear margins and indication to adjuvant radiotherapy including boost radiotherapy but without indication for radiotherapy of the regional lymph nodes or history of prior breast or thoracic radiotherapy. Pretreatment evaluation included a complete history and physical examination; pre-operative imaging by CT or MRI was required.
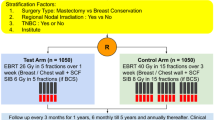
Treatment protocol
The whole breast received a dose of 40.0 Gy in 16 fractions of 2.5 Gy. A SIB with a single dose of 0.5 Gy per fraction was administered to the tumor bed, thereby giving a total dose of 48.0 Gy in 16 fractions to the boost-PTV (Fig. 1). This hypofractionation approach is equivalent to about 46.0 Gy total dose to the breast with 25–26 fractions of 1.8 Gy and also equivalent to about 60.0 Gy to initial tumor region (boost) with 25–26 fractions of 1.8 Gy plus 6–7 fractions of 2.0 Gy assuming the α/β ratio of 3.0 Gy for normal tissue.
Radiotherapy could be given either in 3D-conformal RT (3D-CRT) or IMRT technique. For the 3D-CRT plan, we used 2 tangent fields with dynamic wedges for the whole breast and in most cases 1–3 conformal fields for the boost. Radiotherapy was delivered by a linear accelerator with a minimal energy of 6 MeV using either photons/electron or photon/photon combination depending on optimal PTV coverage. Organs at risk, which had to be contoured, were heart, lung, contralateral breast, and the anterior branch of the LAD (RIVA) from its origin over a length of 3 cm and certain dose parameters (median dose, maximum dose, and percentage of organ receiving > 20 Gy had to be documented (heart median dose < 5 Gy, heart maximum dose ≤ 40 Gy, RIVA median dose < 5 Gy, RIVA maximum dose ≤ 40 Gy, and contralateral breast gland median dose < 3 Gy).
During treatment, patients were evaluated weekly regarding history and clinical examination. Patients continue to be followed-up at regular intervals according to the German guidelines. Toxicities were assessed by National Cancer Institute Common Toxicity Criteria (NCI-CTC), version 3.0. For patient self-assessment of disease specific quality of life (QoL), questionnaires EORTC-QLQ C30 and EORTC-QLQ BR23 were used.
Study design, endpoints, and statistical analysis
The primary endpoint of this prospective multicenter study of hypofractionation with SIB was feasibility across settings. Feasibility was defined as application of 48 Gy in 16 fractions within 22–29 days (date difference + 1) while respecting five dose constraints. Sample size was chosen so that a 95 % confidence interval for the feasible proportion had length 10 percentage points when feasibility was 90 %. Software nQuery Advisor recommended 139 observations. Inclusion of 150 patients was planned to offset screening failures. Missing data on feasibility was counted as not feasible. Modified score-function 95 % confidence intervals were computed for proportions and for differences of proportions among predefined strata radiation type and chemotherapy. Such subgroup analyses explored possible sources of bias. Quality of life statistics included exact 95 % confidence intervals for the median and Hodges–Lehman estimates of differences.
Results
Patient characteristics
A total of 151 patients were enrolled into the study at 7 investigation centers (private practices, local hospitals, and academic centers) from July 2011 to October 2012. Ten patients were found to be ineligible prior to start of radiotherapy. Four of these patients withdrew consent after inclusion, five patients were excluded because of findings during treatment planning (large seroma detected at radiotherapy planning in two patients, inability to precisely delineate the boost volume in three patients), and one patient could not be treated due to pending local ethical vote. Therefore, the intention-to-treat population consists of 141 patients. For all of these patients, the primary endpoint was evaluated. The per-protocol population consisted of 125 patients, who received the complete treatment within 22–29 days and within dose constraints. Safety analyses considered 141 patients receiving at least one treatment application. ITT and safety populations did not differ. The flow of patients is shown in Fig. 2.
The median age was 61 years (range 33–87 years) at registration. Of the patients, 9% had nodal involvement and all patients were M0. The patient characteristics are listed in Tables 1 and 2.
Safety: toxicity and adverse events
Among the 141 patients starting hypofractionated treatment with SIB, dose reduction or permanent treatment discontinuation were never necessary in any patient. Treatment was completed after an interruption in three patients; interruptions were due to concomitant medical problems, not to toxicity. Up to five patients were missing at regular interim assessment visits. For these observations, the worst value seen in the respective patient was assumed.
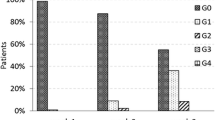
The most frequent adverse reaction reported in the period up to the end of radiotherapy was skin toxicity in 68 patients (48 %), none of whom experienced grade 3 or 4, followed by pressure sensations on the breast in 11 patients (7.8 %), none grade 3 or 4. Any grade 3 or 4 adverse reactions were grade 3 flushing experienced by 2 patients (1.4 %; Table 3). Most cases of hot flushes existed before radiotherapy and were in part due to chemotherapy. The development of skin toxicity over time is illustrated in Fig. 3. Skin toxicity of grade 2 occurred in 22 % (95 % CI 11.7–38.1 %) of patients treated by 3D-CRT and 9 % (95 % CI 4.5–17.8 %) of patients treated with IMRT. Risk difference was 13 percentage points (95 % CI 7–32 %). Chances of skin toxicity grade 2 increased with tumor size by OR 1.03/mm (95 % CI 1.01–1.05 %) in a logistic regression. Other toxicities, mostly fatigue (n = 25), were observed in 67 patients at some point.
Eleven adverse events (AE) were recorded for 10/141 patients (6.5 %). AEs lasted a mean 25 days (range 4–65 days) and were resolved during treatment in 8 AE and ongoing with no treatment necessary in 3 AE. Longer follow-up on toxicity is the primary focus of ongoing study. Intensity was moderate in 6 AE and severe in 5 AE. No deaths were documented. Two AE were caused by treatment, while this was improbable in 9 AE. Their distribution across system organ classes is shown in Table 4.
Feasibility
The number of fractions was 16 in 141/141 of patients (100 %). The administered dose to the whole breast was exactly per protocol (40 Gy) in 141/141 (100 %); the total dose in the boost volume was exactly per protocol (48 Gy) in 139/141 (99 %) patients with slight deviations (47 Gy and 46.7 Gy, respectively) in two patients.
Dose constraints were respected in almost all cases. The median dose in the heart was < 5 Gy in 141 of 141 patients (100 %), maximum dose to the heart was ≤ 40 Gy in 135 of 141 patients (96 %). In the RIVA, median dose was < 15 Gy in 138 of 141 patients (98 %) and maximum dose was ≤ 40 Gy in 140 of 141 patients (99 %). In all 141/141 patients (100 %), the median dose to the contralateral breast gland was < 3 Gy. A description of doses to organs at risk is given in Table 5. Dose intensity and fractionation was per protocol and dose constraints were respected in 130/141 patients (95 % CI 87–96 %). Fractions were applied within time limits in 128/141 of patients (91 %) with an overall treatment time of 22 days (the minimum time according to the protocol) in 83 cases (59 %) and 23 days in 42 of 141 patients (30 %) across all settings. Composite endpoint feasibility was met in 125 of 141 patients (89 %) perfectly performed treatments (95 % CI 82–93 %).
Feasibility with 3D-CRT, 81 % (34/42; 95 % CI 67–90 %), and IMBT, (90/98; 95 % CI 85–96 %) was comparable (95 % CI for the difference − 11 % from − 29 to 7 %). Doses to target volumes and organs at risk depending on radiotherapy technique (3D-CRT vs. IMRT) did not differ significantly (Table 5). Feasibility when the boost consisted of just 6 MeV photons was 87 % (95 % CI 77–93 %) and 91 % (95 % CI 82–96 %) when other photons were used as well.
Quality of life
Quality of life remained largely unchanged by radiotherapy. The 95 % confidence intervals for median change covered zero change for all 23 scales of QLQ-C30 and QLQ-BR23 save the one for breast symptoms (BR23), which improved slightly by 8.33 (95 % CI 4.17–16.67 %) index points. Medians and 95 % confidence intervals for dimension scales before and after radiotherapy are depicted in Fig. 4.
Discussion
ARO 2010-01 is the first completed German multicenter trial evaluating hypofractionation in breast cancer. The primary endpoint of this phase II study was feasibility, defined as application of 48 Gy in 16 fractions within 22–29 days while respecting certain dose constraints. The prescribed dose per protocol was exactly administered in 99 % of patients; adherence to dose constraints for heart, LAD, and contralateral breast was achieved in 92 %. Protocol-conform therapy was feasible for 125 patients or 89 %. One randomized trial reported all of 69 evaluable patients completed radiotherapy; however, details of radiotherapy components were defined neither completely nor conclusively, and treatment lasted 22 days on average, ranging from 18 to 36 days [14]. The present study (with one more fraction) had essentially the same mean, 22.6 days, and less variation: range 21–32 days. The protocol allowed 3D-CRT or IMRT, but strict dose constraints not only for the ipsilateral lung and heart, but also for the contralateral breast had to be met. The majority of patients were treated by IMRT, but dose constraints were respected in comparable manner as with 3D-CRT. This feasibility study lacked a control group, so that general conclusions are limited; another target population might have been sampled than in a randomized trial. We plan a randomized trial with the same inclusion and exclusion criteria.
The hypofractionated regimen was well tolerated in our study with no severe adverse events and a low number of minor adverse events which were mainly not related to radiotherapy. Hypofractionation with SIB has been investigated in a few trials and appears to be safe and feasible with less lung toxicity in smaller studies [13–15]. Van Parijs et al. recently reported the feasibility of a 3-week accelerated schedule for 70 stage I–II breast cancer patients. In that monocenter randomized trial comparing conventional radiotherapy (25 × 2 Gy/5 weeks plus sequential boost 8 × 2 Gy/2 weeks if BCS, cumulative dose 66 Gy in 7 weeks) versus hypofractionated tomotherapy (15 × 2.8 Gy in 3 weeks plus SIB of 0.6 Gy if BCS, cumulative dose 51 Gy in 3 weeks), skin toxicities of grade ≥ 1 at 2 years were seen in 60 % after conventional radiotherapy (CR) vs. 30 % of patients after accelerated tomotherapy (TT). Decrease in heart function of grade ≥ 1 (left ventricular ejection fraction) at 2 years were CR 4.8 % vs. TT 4.6 %, pulmonary function decrease was of grade ≥ 1 when defined by FEV1 change at 2 years in 21 % of CR vs. 15 % of TT and when based on DLco in 29 % of CR vs. 7.4 % of TT patients. Thus, the experimental hypofractionated TT arm with SIB did not show unexpected severe toxicity and confirmed feasibility with tendency to less pulmonary toxicity. Chadha et al. [13] compared acute toxicity of 3-week hypofractionated accelerated WBI (15 × 2.7 Gy plus concomitant boost in 15 × 0.3 Gy, cumulative dose 45 Gy) to a non-randomized group with conventional radiotherapy schedule (26 × 1.8 Gy plus sequential boost in 7 × 2.0 Gy, cumulative dose 60.8 Gy). The authors reported similar results regarding skin toxicity (grade ≥ 2 in 4 % of patients receiving accelerated RT vs. 24 % CR, not randomized) and breast pain with lower incidence in the accelerated hypofrationated treatment. Peak skin erythema occurred 10–14 days after the end of hypofractionated treatment.
An additional finding of our study is the low dose to the heart and coronary artery, which is surely a consequence of modern treatment techniques rather than fractionation regimens although the 20 % reduction in total dose due to hypofractionation contributes in part. The issue of late cardiac toxicity has recently been extensively discussed after a publication in the New England Journal of Medicine [16]. In a population-based case-control study, mean heart dose was 4.9 Gy (range 0.03–27.72 Gy) and rates of major coronary events increased linearly with mean heart dose (increase of relative risk 7.4 % per Gy) without an apparent threshold. However, that analysis refers to a time with older technologies in radiotherapy. Radiation exposure in relevant areas should be lower now except for individual risk constellations, e.g., involvement of parasternal lymph nodes and their inclusion into the PTV. In our investigation, the median heart dose was 1.46 Gy on average (range 0–4.6 Gy); such low doses bear only a minimal risk of cardiac side effects. Thus, our study confirms that the radiation exposure of the heart is generally very low and within an acceptable range even in a multicenter setting if contemporary treatment techniques are used.
We are aware of the limitations of our study. We tested only feasibility defined as the adherence to the protocol criteria. Although the study confirmed the feasibility and protocol compliance, we have limited data on acute and subacute toxicity as compared to conventional fractionation regimens and no data on long-term side effects. However, other studies have reported lower acute side effects and a tendency towards less late sequelae [13, 14].
In summary, our study has demonstrated the feasibility of a combination of hypofractionation with SIB. Although hypofractionated treatment is discouraged at the moment, large ongoing randomized trials (IMPORT-HIGH and RTOG 1005) hypothesize its efficacy is non-inferior to current WBI schemes.
Conclusion
Hypofractionated radiotherapy with SIB after surgery for early stage breast cancer can be applied as planned while respecting dose constraints in all settings in all of Germany. It is experimental but warrants further investigation in randomized trials.
Abbreviations
- 3D-CRT:
-
Three-dimensional conformal radiotherapy
- AE:
-
Adverse event
- ARO:
-
Arbeitsgemeinschaft Radiologische Onkologie (Research Group on Radiological Oncology in the German Cancer Society)
- BCS:
-
Breast-conserving surgery
- CR:
-
Conventional radiotherapy
- DLco:
-
Diffusing capacity of the lung for carbon monoxide
- DVH:
-
Dose–volume histogram
- EORTC:
-
European Organisation for Research and Treatment of Cancer
- FEV1:
-
Forced expiratory volume in 1 s
- IMRT:
-
Intensity modulated radiotherapy
- LAD:
-
Left coronary artery
- NCI-CTC:
-
National Cancer Institute Common Toxicity Criteria
- PTV:
-
Planning target volume
- RIVA:
-
Ramus interventriculares anterior
- SIB:
-
Simultaneous integrated boost
- TT:
-
Tomotherapy
- VMAT:
-
Volumetric modulated arc therapy
- WBI:
-
Whole breast irradiation
References
Clarke M, Collins R, Darby S et al, Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) (2005) Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet 366:2087–2106
Darby S, McGale P, Correa C et al (2011) Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet 378:1707–1716
Whelan TJ, Julian J, Wright J et al (2000) Does locoregional RT improve survival in breast cancer? A meta-analysis. J Clin Oncol 18:1220–1229
Bartelink H, Horiot JC, Poortmans P et al (2007) Impact of a higher radiation dose on local control and survival in breast-conserving therapy of early breast cancer: 10-year results of the randomized boost versus no boost EORTC 22881-10882 trial. J Clin Oncol 22:3259–3326
Livi L, Borghesi S, Saieva C et al (2009) Benefit of radiation boost after whole-breast radiotherapy. Int J Radiat Oncol Biol Phys 75:1029–1034
Azria D, Auvray H, Barillot I et al (2008) Ductal carcinoma in situ: role of the boost. Cancer Radiother 12:571–576
Whelan TJ, Pignol JP, Levine MN et al (2010) Long-term results of hypofractionated radiation therapy for breast cancer. N Engl J Med 362:513–520
START Trialists’ Group, Bentzen SM, Agrawal RK, Aird EG et al (2008) The UK Standardization of Breast Radiotherapy (START) Trial A of radiotherapy hypofractionation for treatment of early breast cancer: a randomised trial. Lancet Oncol 9:331–341
START Trialists’ Group, Bentzen SM, Agrawal RK, Aird EG et al (2008) The UK Standardization of Breast Radiotherapy (START) Trial B of radiotherapy hypofractionation for treatment of early breast cancer: a randomised trial. Lancet 371:1098–1107
Owen JR, Ashton A, Bliss JM et al (2006) Effect of radiotherapy fraction size on tumour control in patients with early-stage breast cancer after local tumour excision: long-term results of a randomized trial. Lancet Oncol 7:467–471
Sedlmayer F, Sautter-Bihl ML, Budach W et al (2013) Breast Cancer Expert Panel of the German Society of Radiation Oncology (DEGRO). Is the simultaneously integrated boost (SIB) technique for early breast cancer ready to be adopted for routine adjuvant radiotherapy? Statement of the German and the Austrian Societies of Radiooncology (DEGRO/ÖGRO). Strahlenther Onkol 189:193–196
Sedlmayer F, Sautter-Bihl ML, Budach W et al (2013) Breast Cancer Expert Panel of the German Society of Radiation Oncology (DEGRO). DEGRO practical guidelines: radiotherapy of breast cancer I. Radiotherapy following breast conserving therapy for invasive breast cancer. Strahlenther Onkol 189:825–833
Chadha M, Vongtama D, Friedmann P et al (2012) Comparative acute toxicity from whole breast irradiation using 3-week accelerated schedule with concomitant boost and the 6.5-week conventional schedule with sequential boost for early-stage breast cancer. Clin Breast Cancer 12:57–62
Van Parijs HM, Vinh-Hung V et al (2012) Short course radiotherapy with simultaneous integrated boost for stage I–II breast cancer, early toxicities of a randomized clinical trial. Radiat Oncol 7:80
Scorsetti M, Alongi F, Fogliata A et al (2012) Phase I–II study of hypofractionated simultaneous integrated boost using volumetric modulated arc therapy for adjuvant radiation therapy in breast cancer patients: a report of feasibility and early toxicity results in the first 50 treatments. Radiat Oncol 28:145
Darby SC, Ewertz M, McGale P et al (2012) Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med 368:987–998
Compliance with ethical guidelines
Conflict of interest
K. Dellas, R. Vonthein, J. Zimmer, S. Dinges, A.D. Boivcev, P. Andreas, D. Fischer, C. Winkler, A. Ziegler, and J. Dunst state that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
ARO Study Group
Rights and permissions
About this article
Cite this article
Dellas, K., Vonthein, R., Zimmer, J. et al. Hypofractionation with simultaneous integrated boost for early breast cancer. Strahlenther Onkol 190, 646–653 (2014). https://doi.org/10.1007/s00066-014-0658-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-014-0658-5