Abstract
Purpose
The goal of this work was to evaluate toxicity and local control following hypofractionated stereotactic radiation treatment with special focus on changes in tumor volume and hearing capacity.
Patients and methods
In all, 29 patients with unilateral acoustic neuroma were treated between 2001 and 2007 within a prospective radiation protocol (7 × 4 Gy ICRU dose). Median tumor volume was 0.9 ml. Follow-up started at 6 months and was repeated annually with MRI volumetry and audiometry. Hearing preservation was defined as preservation of Class A/B hearing according to the guidelines of the American Academy of Otolaryngology (1995).
Results
No patient had any intervention after a median imaging follow-up of 89.5 months, one patient showed radiological progression. Transient increase of tumor volume developed in 17/29 patients, whereas 22/29 patients (75.9 %) presented with a volume reduction at last follow-up. A total of 21 patients were eligible for hearing evaluation. Mean pure tone average (PTA) deteriorated from 39.3 to 65.9 dB and mean speech discrimination score (SDS) dropped from 74.3 to 38.1 %. The 5-year actuarial Class A/B hearing preservation rate was 50.0 ± 14.4 %.
Conclusion
Radiation increases only minimally, if at all, the hearing deterioration which emerges by observation alone. Presbyacusis is not responsible for this deterioration. Transient tumor enlargement is common. Today radiation of small- and medium-sized acoustic neuroma can be performed with different highly conformal techniques as fractionated treatment or single low-dose radiosurgery with equal results regarding tumor control, hearing preservation, and side effects. Hypofractionation is more comfortable for the patient than conventional regimens and represents a serious alternative to frameless radiosurgery.
Zusammenfassung
Ziel
Ziel der Studie war die Evaluierung der Toxizität und der lokalen Tumorkontrolle einer hypofraktionierten stereotaktischen Bestrahlung mit besonderem Augenmerk auf Veränderungen von Tumorvolumen und Hörvermögen.
Patienten und Methoden
Insgesamt wurden zwischen 2001 und 2007 29 Patienten mit unilateralem Akustikusneurinom innerhalb eines prospektiven Bestrahlungsprotokolls behandelt (7 mal 4 Gy ICRU-Dosis). Das mediane Tumorvolumen betrug 0,9 ml. Die Nachsorge startete nach 6 Monaten und wurde jährlich wiederholt mit MRI-Volumetrie und Audiometrie. Der Hörerhalt wurde definiert als Erhalt eines Class-A/B-Hörvermögens nach den Richtlinien der American Academy of Otolaryngology (1995).
Ergebnisse
Kein Patient benötigte eine Intervention nach einer medianen Nachbeobachtungszeit von 89,5 Monaten, ein Patient entwickelte eine radiologische Progression. Eine vorübergehende Volumenzunahme zeigte sich bei 17/29 Patienten nach 6 Monaten, eine Volumenreduktion wiesen 22/29 Patienten (75,9 %) bei der jüngsten Nachsorgeuntersuchung auf. Insgesamt waren 21 Patienten bezüglich des Hörerhalts auswertbar. Der Mittelwert im Tonaudiogramm (PTA) verschlechterte sich von 39,3 dB auf 65,9 dB, das durchschnittliche Sprachverständnis (SDS) fiel von 74,3 % auf 38,1 %. Der aktuarische 5-Jahres-Class-A/B-Hörerhalt betrug 50,0 ± 14,4 %.
Schlussfolgerung
Der Grad der Hörminderung nach Bestrahlung ist, wenn überhaupt, nur minimal deutlicher als nach alleiniger Beobachtung. Presbyakusis ist nicht verantwortlich für diese zunehmende Hypakusis. Eine vorübergehende Volumenzunahme ist häufig. Heute ist eine Bestrahlung von kleinen bis mittelgroßen Akustikusneurinomen mit jeder hochkonformalen Technik als fraktionierte oder niedrigdosierte singuläre Behandlung mit gleichwertigem Ergebnis bezüglich Tumorkontrolle, Hörerhalt und Nebenwirkungen durchführbar. Die hypofraktionierte Bestrahlung ist für den Patienten komfortabler als konventionelle Schemata und eine ernsthafte Alternative zur nichtinvasiven Radiochirurgie.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
In the course of the last decade, the reported incidence of acoustic neuroma has increased, reaching 15 to 20/million per year [49], mainly because of the more frequent use of magnetic resonance imaging (MRI). In addition to traditional microsurgery, alternative approaches like “wait and scan” or stereotactic radiotherapy are used [3, 5, 35, 36]. The goal of hypofractionated stereotactic radiotherapy is to reach a high tumor control rate and a low rate of cranial nerve toxicity with a comfortable technique in a short treatment time. Here, we report a series of hypofractionated radiotherapy for acoustic neuroma and provide long term follow-up details regarding the dynamics of tumor volumes and hearing preservation.
Patients and methods
Between July 2001 and December 2007, 29 consecutive patients (11 men, 18 women) with unilateral acoustic neuroma were treated within a prospective radiation protocol. Mean and median patient age was 57 years (range 32–75 years). Eight patients had surgery prior to radiotherapy. All patients had a growing tumor and/or increasing clinical symptoms before admission. Patients with neurofibromatosis type II were excluded. The mean maximal extrameatal tumor diameter was 13.9 mm (range 8–29 mm). The median tumor volume amounted to 0.9 ml (range 0.2–8.8 ml) and the median planning target volume (PTV) was 1.7 ml (range 0.4–12.7 ml). The stereotactic system originally described by Leibinger–Fischer (Freiburg, Germany) was applied. The patient’s head was immobilized by using an individual mask made of scotch cast (Heidelberg mask). Images for planning were generated with multiplanar T1-weighted contrast-enhanced MRI sequences (Harmony, Siemens), reconstructed with a slice thickness of 2 mm. A contrast-enhanced planning CT (XVision, Toshiba) with a slice thickness of 2 mm was obtained with the patient’s head fixed in the stereotactic mask system. CT and MR images were merged on the stereotactic planning workstation. The PTV was defined as gross tumor volume as visible on the T1-weighted MR images plus a 1–1.5 mm margin. A manually driven micro-multileaf collimator with a leaf width of 1 mm was used for field shaping. We created 4–6 fixed beams to apply 4 Gy to the ICRU reference point for 3–5 fractions per week, encompassing the PTV within the 90 % isodose volume (90 % = 3.6 Gy).
A total of 21 of 23 patients with any hearing capacity before treatment had audiological examination before radiotherapy with pure tone audiogram and evaluation of speech discrimination and were therefore eligible for the assessment of hearing preservation. All 29 patients had clinical and neurological examination before irradiation and were evaluable regarding changes of tumor volume.
Follow-up
MRI, clinical, and audiological follow-up started 6 months after irradiation and was repeated annually. Grading of the cranial nerve VII function was described according to the House–Brackmann score [18]. In addition, synkinesis—if present—was scored. Function of the cranial nerve V was noted descriptively as numbness and/or trigeminal neuropathy.
Hearing was scored according to the guidelines of the American Academy of Otolaryngology–Head and Neck Surgery Foundation (AAO-HNSF) [9]. As recommended, the pure tone average (PTA) was defined as the mean of the measured 0.5, 1.0, 2.0, and 3.0 kHz values in decibel. The speech discrimination score (SDS) was measured as the fraction of standardized words that could be understood at a sound intensity of 30–40 dB louder than the individual PTA value. The median audiological follow-up time was 71.3 months (mean 80.5 months; range 43.0–129.7 months).
Sequential MRI examinations were done with the same technique as for radiotherapy planning and the 3D tumor volume was generated from the 2 mm axial T1 contrast-enhanced images in the same manner as for the initial dose planning. All 29 patients had sequential MRI examinations with a median follow-up time of 89.5 months (mean 85.8 months; range 30.5–128.7 months). In the literature, an increase in the largest tumor diameter of > 2 mm is often taken as a criterion for progression [5]. We tried to compare this one dimensional increase of 2 mm with our measured 3D volumes by transforming these volumes to spheres with the same volume and increasing their radius by 1 mm, to make a 3D volumetric increase comparable to a one dimensional increase of 2 mm or more.
Statistics
Actuarial hearing preservation rates were calculated using the Kaplan–Meier method [23]. The differences between groups were assessed with the Fisher exact test and a 2-tailed t-test for categorical and continuous data sets, respectively. Statistical analyses were performed using IBM SPSS Statistics version 20.
Results
At last follow-up, 28 of the 29 patients were alive. One woman died 61 months after radiation treatment from metastatic extracerebral cancer; her neuroma was locally controlled.
Tumor control
No patient required salvage treatment; the intervention-free tumor control rate is 100 %. The treatment for 1 of the 29 patients was recorded as a failure according to the definition described above with increasing tumor volume at 100.9 months after treatment without neurological symptoms except for further hearing deterioration (crude tumor control rate 96.6 %).
Tumor volume
We observed transient volume enlargement in 17 of 29 patients (58.6 %) after a median MRI follow-up time of 6 months (p = 0.019), but permanent volume reduction in 22 out of 29 patients (75.9 %) after a median MRI follow-up time of 89.5 months (p < 0.001). At this late time point, only 3 out of 29 patients (10.3 %) had a larger volume compared to the volume at treatment, the volume in 4 patients was unchanged (◉ Fig. 1). Mean volume reduction per patient was 0.41 ml, while the mean maximal volume enlargement in relation to initial volume was + 21 % (◉ Fig. 2).
Hearing evaluation
Of 23 patients with hearing capacity before radiotherapy, 21 had serial pure tone and speech audiometry and were, therefore, evaluable for hearing preservation. In all, 2 of the 23 patients refused repeated audiometry. Only 1 of 8 patients with prior excisional surgery were included in the hearing evaluation. Between 5 and 11 sequential audiograms per patient (mean 7.3 audiograms per patient) were recorded. A total of 109 of 153 audiograms (71.2 %) were generated at our hospital. The mean PTA level before radiotherapy was 39.3 dB (range 9–71 dB). This level dropped to a mean of 48.3 dB (range 6–83 dB) at a median follow-up time of 7 months and to 53.6 dB (range 6–94 dB) at 20 months (p < 0.001) with further deterioration thereafter to 65.9 dB (range 15–120 dB) at 71.3 months (p < 0.001). The dynamics of the mean pure tone values for different frequencies at different time points are depicted in ◉ Fig. 3a, b. The mean PTA level before radiotherapy on the contralateral ear was 19.3 dB and changed minimally to 22.3 dB at a median of 71.3 months (◉ Fig. 3c; p < 0.001 for comparison with the ipsilateral ear). Only 3 patients were initially admitted with presbyacusis.
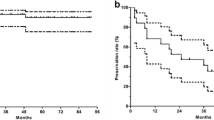
The speech discrimination score (SDS) was available for all 21 evaluated patients before and after radiotherapy. The mean SDS value before radiotherapy was 74.3 % (range 25–100 %). This value dropped at last follow-up to a mean of 38.1 % (range 0–100 %; p < 0.001). The actuarial 5-year rate of preserving Class A/B hearing (n = 12) was 50.0 ± 14.4 % (◉ Fig. 4). All 6 patients with an initial SDS of 90–100 % had their Class A/B hearing preserved, but no patient with an initial SDS of < 90 % (p = 0.002 Fisher exact test).
Cranial nerve toxicities
One of 29 patients at risk developed a new minimal facial nerve deficit grade 3 at 30 months which resumed to grade 1 after 4 years. This patient also presented with facial synkinesis between 30 and 40 months. Electromyography revealed a pathological signal for the ipsilateral nasal muscle. One other patient developed facial synkinesis between 7 and 12 months after radiotherapy. One 65-year-old woman developed severe ipsilateral facial nerve paresis grade 6 at 80 months after irradiation as a side effect of influenza vaccination [54].
Two patients developed mild partial numbness which persisted in one. One other patient reported discrete temporary symptoms of trigeminal neuropathy at 70 months after treatment and received anticonvulsive drug treatment. Cranial nerve lesions related to surgery (8 patients at risk) did not deteriorate after radiotherapy.
Other toxicities
Two patients have ongoing postoperative sicca syndrome of the ipsilateral eye. Dizziness and tinnitus were present in almost all patients at the time of admission and changed marginally after radiotherapy. Small field alopecia occurred regularly in 1 or 2 areas at the entrance site of the beam and was temporary in almost all patients. Thus far, no radiation related secondary tumor was found, but the observation time with respect to possible tumor induction is rather short.
Discussion
This study has the longest imaging and audiological follow-up of all reported hypofractionation series for acoustic neuroma. We measured a volume reduction in 76 % and a transient volume increase in 59 % with only 1/29 patients presenting with a late progression. With a median audiological follow-up time of 71 months, we found a 7-year actuarial rate for preserving a serviceable hearing (i.e., class A/B hearing) of 50 ± 14.4 %. Mean PTA level dropped from 39.2 to 65.9 dB, mean SDS from 67.1 to 38.1 %. We did not find a conspicuous hearing deterioration in the contralateral ear and presbyacusis was already present in 3 patients before irradiation. Hasegawa et al. [16] also did not observe a marked hearing deterioration in the contralateral ear in their long-term follow-up study after radiosurgery.
Several other authors reported about hypofractionated regimens in patients with acoustic neuroma [1, 4, 7, 11, 15, 19–22, 24, 25, 27, 30–34, 38–41, 46, 53]. The definition of tumor size, local control, and hearing preservation were quite different between the studies. Some initial papers had follow-up reports in abstract form only; mean or median follow-up times were less than 5 years in most studies. A crude tumor control rate of 80–100 % and actuarial 5-year rates of 88–100 % were reported. Tumor size reduction varied greatly from 10 to 81 % (◉ Table 1 and 2). A transient increase in tumor diameter was reported by Sakanaka et al. [46] in 48 % of their cases. Henzel et al. [17] compared three-dimensional volume shrinkage between radiosurgery and conventional fractionated stereotactic radiotherapy and found significantly more shrinkage in the fractionated group. Kapoor et al. [24] updated results from the John Hopkins Hospital and used the term radiological progression for any enlargement of tumors after at least 18 months of follow-up. However, a transient increase of tumor volume is common after the 18 months period. Therefore, this study could indeed not differentiate exactly between transient increase of volume and real progression. The development of tumor volume was also examined in some radiosurgery studies. Nagano et al. [37] reported on the development of the relative tumor volume over time in their study with a mean follow-up time of 7.5 years and found a transient increase of 28 % at 6 months after treatment with a final decrease of 31 % at 5 years, values quite similar to the findings in our study.
Hearing preservation was reported in some hypofractionation studies without objective data, in most studies as crude rate and in only one study [33] as actuarial rate. The period of audiological follow-up was mostly shorter than imaging follow-up or was not separately stated. Only a few studies presented specific data for PTA and SDS.
It has been postulated that conventional fractionation may preserve hearing to a greater extent than single fraction radiosurgery [12]. There are studies with actuarial 4- to 5-year hearing preservation rates of 82–94 %. These studies had objective audiological data only for a minority of patients; the final definition of hearing preservation was mainly based on a subjective questionnaire. Sequential follow-up audiometry was performed in one of such study [26] for 68/115 patients, but the final hearing outcome was again defined subjectively after a median follow-up time of 32.1 months. However, studies with subjective hearing evaluation are not able to evaluate the hearing ability of each ear separately. Studies with objective audiological evaluation and more than 3 years of follow-up [2, 28, 29, 42, 47, 51] resulted in a crude hearing preservation rate of 54 % (129/239 patients) and actuarial 3- to 5-year rates of 54.5–72 %.
Rasmussen et al. [42] stated that fractionated stereotactic radiotherapy accelerates hearing loss compared to observation alone, but their conclusion was based on their very low 2-year hearing preservation rate of 38 % in the irradiated patients.
Most authors did not find a relation between tumor volume and hearing preservation. Hearing capacity deters even in untreated patients without tumor growth [50, 52]. The question of a threshold dose to the cochlea was mainly studied in radiosurgery series, but each study found a different cut off value between 3 and 6 Gy. It is well known that there are conditions independent of radiation dose, which influence hearing ability: Goddard et al. [13] found that fluid between the neuroma and lateral end of the internal acoustic canal results in better hearing preservation in operated patients. Higher levels of fibroblast growth factor 2 were measured by Dilwali et al. [10] in patients with a better hearing capacity. Other factors for hearing deterioration are compression of the stato-acoustic nerve or of the surrounding vasculature from the tumor itself, loss of inner ear fluid or a hypointense signal on T2 MR images. Even dysfunction of the cochlea itself may contribute to hearing deterioration [45]. Long-term follow-up in radiosurgery studies revealed continuous hearing loss beyond 5 years after treatment [8, 44].
In some prospective long-term observational studies with exact audiological evaluation [14, 43, 48], a continuous hearing deterioration dependent on follow-up time was found, which is not very different to the deterioration after radiotherapy (◉ Table 3). Breivik et al. [6] did not find a difference in hearing deterioration between observation and radiosurgery.
Conclusion
Hypofractionated stereotactic radiotherapy of acoustic neuroma leads to a very small—if any—increase in hearing deterioration compared to observation alone. Presbyacusis is not responsible for this deterioration. Transient tumor enlargement is common and mostly without symptoms.
To date, considering variations and shortcomings in reporting of volumes, dose specifications and standardized recording of late sequelae, there is no strong evidence regarding superiority of any treatment schedule. Radiation of small- and medium-sized acoustic neuroma can be successfully performed by different highly conformal radiation techniques and doses as fractionated treatment or single low dose radiosurgery (both frame-based or frameless) with equal results regarding tumor control, hearing preservation, and side effects. Hypofractionation is more comfortable for the patient than time-consuming conservative fractionation regimens. It also serves as a serious alternative to frameless single dose radiosurgery.
Compliance with ethical guidelines
Conflict of interest
M. Kranzinger, F. Zehentmayr, G. Fastner, G. Oberascher, F. Merz, O. Nairz, H. Rahim, and F. Sedlmayer state that there are no conflicts of interest.
References
Anderson BM, Khuntia D, Toma WA et al (2007) Single institution experience treating 100 vestibular schwannomas with fractionated stereotactic radiation therapy or stereotactic radiosurgery. Int J Radiat Oncol Biol Phys 69(Suppl):121
Aoyama H, Onodera S, Takeichi N et al (2013) Symptomatic outcomes in relation to tumor expansion after fractionated stereotactic radiation therapy for vestibular schwannomas: single-institutional long-term experience. Int J Radiat Oncol Biol Phys 85:329–334
Arthurs BJ, Fairbanks RK, Demakas JJ et al (2011) A review of treatment modalities for vestibular schwannoma. Neurosurg Rev 34:265–279
Badakhshi H, Müllner S, Boehmer D et al (2011) Linac basierte stereotaktische Radiochirurgie und stereotaktische fraktionierte Radiotherapie in der Behandlung von vestibulären Schwannomen. Strahlenther Onkol 187 Sondernr 1:75
Bassim MK, Berliner KI, Fisher LM et al (2010) Radiation therapy for the treatment of vestibular schwannoma: a critical evaluation of the state of the literature. Otol Neurotol 31:567–573
Breivik CN, Nilsen RM, Myrseth E et al (2013) Conservative management or gamma knife radiosurgery for vestibular schwannoma: tumor growth, symptoms, and quality of life. Neurosurgery 73:48–57
Chang SD, Gibbs IC, Sakamoto GT et al (2005) Staged stereotactic irradiation for acoustic neuroma. Neurosurgery 56:1254–1263
Chopra R, Kondziolka D, Niranjan A et al (2007) Long-term follow-up of acoustic schwannoma radiosurgery with marginal tumor doses of 12 to 13 Gy. Int J Radiat Oncol Biol Phys 68:845–851
Committee on Hearing and Equilibrium guidelines for the evaluation of hearing preservation in acoustic neuroma (vestibular schwannoma) (1995) Otolaryngol Head Neck Surg 113:179–180
Dilwali S, Lysaght A, Roberts D et al (2013) Sporadic vestibular schwannomas associated with good hearing secrete higher levels of fibroblast growth factor 2 than those associated with poor hearing irrespective of tumor size. Otol Neurotol 34:748–754
Dziuba SJ, Curran WJ, Suarez O et al (2000) Single institution experience with 110 patient treated for acoustic schwannomas. Analysis of Gamma Knife stereotactic radiosurgery and Linac fractionated stereotactic radiotherapy. Int J Radiat Oncol Biol Phys 48(Suppl):254
Fuss M, Debus J, Lohr F et al (2000) Conventionally fractionated stereotactic radiotherapy (FSRT) for acoustic neuromas. Int J Radiat Oncol Biol Phys 48:1381–1387
Goddard JC, Schwartz MS, Friedman RA (2010) Fundal fluid as a predictor of hearing preservation in the middle cranial fossa approach for vestibular schwannoma. Otol Neurotol 31:1128–1134
Hajioff D, Raut VV, Walsh RM et al (2008) Conservative management of vestibular schwannomas: third review of a 10-year prospective study. Clin Otolaryngol 33:255–259
Hansasuta A, Choi CY, Gibbs IC et al (2011) Multisession stereotactic radiosurgery for vestibular schwannomas: single-institution experience with 383 cases. Neurosurgery 69:1200–1209
Hasegawa T, Kida Y, Kato T et al (2011) Factors associated with hearing preservation after Gamma Knife surgery for vestibular schwannomas in patients who retain serviceable hearing. J Neurosurg 115:1178–1186
Henzel M, Hamm K, Sitter H et al (2009) Comparison of stereotactic radiosurgery and fractionated stereotactic radiotherapy of acoustic neurinomas according to 3-D tumor volume shrinkage and quality of life. Strahlenther Onkol 185:567–573
House JW, Brackmann DE (1985) Facial nerve grading system. Otolaryngol Head Neck Surg 93:146–147
Ishihara H, Saito K, Nishizaki T et al (2004) CyberKnife radiosurgery for vestibular schwannoma. Minim Invasive Neurosurg 47:290–293
Johnson A, Ali AN, Dhabbaan A et al (2012) Short course radiation therapy for acoustic neuromas. Int J Radiat Oncol Biol Phys 84(Suppl):276
Ju DT, Lin JW, Lin MS et al (2008) Hypofractionated cyberKnife stereotactic radiosurgery for acoustic neuromas with and without association to neurofibromatosis Type 2. Acta Neurochir Suppl 101:169–173
Kalapurakal JA, Silverman CL, Akhtar N et al (1999) Improved trigeminal and facial nerve tolerance following fractionated stereotactic radiotherapy for large acoustic neuromas. Br J Radiol 72:1202–1207
Kaplan E, Meier P (1958) Nonparametric estimation for incomplete observation. J Am Stat Assoc 53:457–481
Kapoor S, Batra S, Carson K et al (2011) Long-term outcomes of vestibular schwannomas treated with fractionated stereotactic radiotherapy: an institutional experience. Int J Radiat Oncol Biol Phys 81:647–653
Karam SD, Tai A, Strohl A et al (2013) Frameless fractionated stereotactic radiosurgery for vestibular schwannomas: a single-institution experience. Front Oncol 3:121
Kopp C, Fauser C, Müller A et al (2011) Stereotactic fractionated radiotherapy and linac radiosurgery in the treatment of vestibular schwannoma—report about both stereotactic methods from a single institution. Int J Radiat Oncol Biol Phys 80:1485–1491
Lederman G, Lowry J, Wertheim S et al (1997) Acoustic neuroma: potential benefits of fractionated stereotactic radiosurgery. Stereotact Funct Neurosurg 69:175–182
Lin VY, Stewart C, Grebenyuk J et al (2005) Unilateral acoustic neuromas: long-term hearing results in patients managed with fractionated stereotactic radiotherapy, hearing preservation surgery, and expectantly. Laryngoscope 115:292–296
Litre F, Rousseaux P, Jovenin N et al (2013) Fractionated stereotactic radiotherapy for acoustic neuromas: a prospective monocenter study of about 158 cases. Radiother Oncol 106:169–174
Mahadevan A, Floyd S, Wong E et al (2011) Clinical outcome after hypofractionated stereotactic radiotherapy (HSRT) for benign skull base tumors. Comput Aided Surg 16:112–120
Makara D, Lederman G, Raden M et al (2003) Fractionated stereotactic radiosurgery (FSR) for acoustic neuroma (AN)—lack of side effects. Int J Radiat Oncol Biol Phys 57(Suppl):326
McWilliams W, Trombetta M, Werts ED et al (2011) Audiometric outcomes for acoustic neuroma patients after single versus multiple fraction stereotactic irradiation. Otol Neurotol 32:297–300
Meijer OW, Vandertop WP, Baayen JC et al (2003) Single-fraction vs. fractionated linac-based stereotactic radiosurgery for vestibular schwannoma: a single-institution study. Int J Radiat Oncol Biol Phys 56:1390–1396
Morimoto M, Yoshioka Y, Kotsuma T et al (2013) Hypofractionated stereotactic radiation therapy in three to five fractions for vestibular schwannoma. Jpn J Clin Oncol 43:805–812
Mulder JJ, Kaanders JH, vanOverbeeke JJ et al (2012) Radiation therapy for vestibular schwannomas. Curr Opin Otolaryngol Head Neck Surg 20:367–371
Murphy ES, Suh JH (2011) Radiotherapy for vestibular schwannomas: a critical review. Int J Radiat Oncol Biol Phys 79:985–997
Nagano O, Serizawa T, Higuchi Y et al (2010) Tumor shrinkage of vestibular schwannomas after gamma knife surgery: results after more than 5 years of follow-up. J Neurosurg 113(Suppl):122–127
Noren G (2011) Oral presentation at the ISRS congress. Paris
Ogino H, Shibamoto Y, Murai T et al (2011) Five-fraction cyberKnife stereotactic radiotherapy for acoustic neuroma: evaluation of three different dose levels. Int J Radiat Oncol Biol Phys 81(Suppl):286
Polovnikov ES, Anikeeva OY, Filatov PV et al (2013) Stereotactic radiosurgery and hypofractionated stereotactic radiotherapy for management of vestibular schwannomas: initial experience with 17 cases. Acta Neurochir Suppl 116:37–44
Qiu H, Redmond KJ, Batra S et al (2010) Hearing loss and tumor control following fractionated stereotactic radiation therapy (FSRT) for vestibular schwannoma (VS): The Johns Hopkins Hospital (JHH) experience. Int J Radiat Oncol Biol Phys 78(Suppl):9
Rasmussen R, Claesson M, Stangerup SE et al (2012) Fractionated stereotactic radiotherapy of vestibular schwannomas accelerates hearing loss. Int J Radiat Oncol Biol Phys 83:e607–e611
Raut VV, Walsh RM, Bath AP et al (2004) Conservative management of vestibular schwannomas—second review of a prospective longitudinal study. Clin Otolaryngol Allied Sci 29:505–514
Roos DE, Potter AE, Brophy BP (2012) Stereotactic radiosurgery for acoustic neuromas: what happens long term? Int J Radiat Oncol Biol Phys 82:1352–1355
Roosli C, Linthicum FH, Cureoglu S et al (2012) Dysfunction of the cochlea contributing to hearing loss in acoustic neuromas: an underappreciated entity. Otol Neurotol 33:473–480
Sakanaka K, Mizowaki T, Arakawa Y et al (2011) Hypofractionated stereotactic radiotherapy for acoustic neuromas: safety and effectiveness over 8 years of experience. Int J Clin Oncol 16:27–32
Sawamura Y, Shirato H, Sakamoto T et al (2003) Management of vestibular schwannoma by fractionated stereotactic radiotherapy and associated cerebrospinal fluid malabsorption. J Neurosurg 99:685–692
Stangerup SE, Caye-Thomasen P, Tos M et al (2008) Change in hearing during ‘wait and scan’ management of patients with vestibular schwannoma. J Laryngol Otol 122:673–681
Stangerup SE, Caye-Thomasen P, Tos M et al (2006) The natural history of vestibular schwannoma. Otol Neurotol 27:547–552
Sughrue ME, Kane AJ, Kaur R et al (2011) A prospective study of hearing preservation in untreated vestibular schwannomas. J Neurosurg 114:381–385
Thomas C, Di Maio S, Ma R et al (2007) Hearing preservation following fractionated stereotactic radiotherapy for vestibular schwannomas: prognostic implications of cochlear dose. J Neurosurg 107:917–926
Van de Langenberg R, de Bondt BJ, Nelemans PJ et al (2011) Predictors of volumetric growth and auditory deterioration in vestibular schwannomas followed in a wait and scan policy. Otol Neurotol 32:338–344
Williams JA (2003) Fractionated stereotactic radiotherapy for acoustic neuromas: preservation of function versus size. J Clin Neurosci 10:48–52
Zhou W, Pool V, DeStefano F et al (2004) A potential signal of Bell’s palsy after parenteral inactivated influenza vaccines: reports to the vaccine adverse event reporting system (VAERS)—United States, 1991–2001. Pharmacoepidemiol Drug Saf 13:505–510
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kranzinger, M., Zehentmayr, F., Fastner, G. et al. Hypofractionated stereotactic radiotherapy of acoustic neuroma. Strahlenther Onkol 190, 798–805 (2014). https://doi.org/10.1007/s00066-014-0630-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-014-0630-4