Abstract
Objectives
These guidelines contain recommendations for the implementation of quality-assured hyperthermia treatments. The objective is to guarantee an internationally comparable and easily understandable method for hyperthermia treatment and for the subsequent scientific analysis of the treatment results. The guidelines describe “regional deep hyperthermia” (RHT) and MR-controlled “partial body hyperthermia” (PBH) of children, adolescents and adult patients. Hyperthermia in terms of these guidelines is defined as a treatment combining chemotherapy and/or radiation therapy.
Methods
These guidelines are based on practical experience from several hyperthermia centres in Europe. Our collaborative effort has ensured coordinated standards and quality control procedures in regional deep and partial body hyperthermia. The guidelines were developed by the Atzelsberg Research Group of the IAH (http://www.hyperthermie.org) of the German Cancer Society (“Deutsche Krebsgesellschaft”) to specifically ensure that the multi-institutional studies initiated by the Atzelsberg Research Group are executed following a single, uniform level of quality.
Results
The guidelines contain recommendations for procedural methods for treatment using hyperthermia. They commence with diagnosis, which is followed by preparation and treatment and concludes with standardised analysis for the reporting of results.
Zusammenfassung
Hintergrund
Diese Leitlinie enthält Empfehlungen zur Durchführung von qualitätsgesicherten Hyperthermiebehandlungen. Ziel ist, ein vergleichbares und nachvollziehbares Vorgehen bei der Behandlung und der wissenschaftlichen Auswertung der Hyperthermie zu gewährleisten. Die Leitlinie beschreibt die „Regionale Tiefenhyperthermie“ (RHT) und die „MR-kontrollierte Teilkörperhyperthermie“ (PBH) von Kindern, Jugendlichen und erwachsenen Patienten. Die Hyperthermie im Sinne dieser Leitlinie wird als Kombinationsbehandlung mit einer Chemo- und/oder Strahlentherapie durchgeführt.
Methodik
Die vorgestellte Leitlinie basiert auf praktischen Erfahrungen von mehreren Hyperthermiezentren. Dieses Vorgehens erlaubt gemeinsam abgestimmte Standards in der Anwendung und der Qualitätskontrolle in der Hyperthermie für Studien, die im Rahmen des Atzelsberger Arbeitskreises in der Interdisziplinären Arbeitsgruppe Hyperthermie (http://www.hyperthermie.org) in der Deutschen Krebsgesellschaft und dem Technischen Komitee der „European Society for Hyperthermic Oncology“ (ESHO) entwickelt wurden, um sicher zu stellen, dass multizentrische Studien, die vom Atzelsberger Arbeitskreis entwickelt wurden, nach einem standardisierten, einheitlichen Qualitätsmaßstab durchgeführt werden.
Ergebnisse
Diese Leitlinie enthält Empfehlungen für das Vorgehen bei Hyperthermiebehandlungen von der Indikationsstellung, der Vorbereitung, der Durchführung bis zur standardisierten Auswertung.
Die deutschsprachige Version des Beitrags ist auf SpringerLink unter „Supplemental“ zu finden.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Use of the guidelines
These guidelines were developed by the Atzelsberg Research Group of the IAH (http://www.hyperthermie.org) of the German Cancer Society (“Deutsche Krebsgesellschaft”) to specifically ensure that the multi-institutional studies initiated by the Atzelsberg Research Group are executed following a single, uniform level of quality. They are recognized by the European Society for Hyperthermic Oncology (ESHO) and as such serve as the current (pre)standard to ensure that the application and registration of the deep hyperthermia treatment is according current knowledge and experience both from technological and clinical considerations. ESHO notes that to enhance uniformity of quality in hyperthermia application at an international level, a commitment exists with their sister hyperthermia organization in the USA (STM) to design quality assurance guidelines valid for all types of hyperthermia and recognized by both STM and ESHO.
Quality guidelines are essential for physicians, physicists and technical personnel performing and supervising hyperthermia treatments.
These guidelines contain standards for implementing quality assurance measures as part of a quality management in hyperthermia [39].
The guidelines presented here are based on practical experience from several hyperthermia centres in Europe. The advantage of this coordinated procedure is in applying jointly coordinated and specified standards and a quality control in hyperthermia for the studies that were developed as part of the Atzelsberg Research Group of the Interdisciplinary Working Group Hyperthermia (IAH) in the German Cancer Society. The objective in producing these guidelines is to guarantee a comparable and traceable method of procedure when applying hyperthermia and conducting the relevant tests.
The proven effectiveness of hyperthermia in clinical studies relies exclusively on its thermal effect on tumours [30, 31, 32, 57, 60, 61]. For this reason hyperthermia treatments must be conducted using hyperthermia devices that are technically capable of controlled heating of a specific target volume defined by imaging (CT, MRT) while sparing normal tissue at the same time. Technically this can only be achieved by radiating and focusing electromagnetic waves on the target volume. Recording the temperature directly in the target volume or surrounding tissue is pivotal to treatment quality. Hyperthermia systems that are not able to achieve a temperature rise in the target volume up to between 40 and 43 °C, or devices that do not intend to measure temperatures, cannot be regarded as hyperthermia devices in terms of this recommendation.
These guidelines describes the “regional deep hyperthermia” (RHT) and the “MR-controlled partial body hyperthermia” (PBH) in children, adolescents and adult patients performed as a combined treatment using chemotherapy and/or radiation therapy [2, 13, 25, 42, 43, 44, 50, 57].
2 Responsibilities for diagnosis, planning, treatment and documentation of hyperthermia
Hyperthermia treatment is a multi-disciplinary method based on medical and technical aspects. It involves various professional groups, including radiation oncologists, medical oncologists and medical physicists, as well as engineers and technical personnel. In addition to the diagnosis, planning, treatment and documentation of hyperthermia, personnel may also be required for other responsibilities, e.g., for MR thermometry or anaesthesia.
For the patient, the benefit of the treatment must outweigh the possible risks and take other therapy modalities into consideration. Finally, it is emphasised that the recommendations given in the five websites below must be observed:
-
Guidelines of WHO (http://www.who.int),
-
Guidelines of DEGRO (http://www.degro.org),
-
Guidelines of ESHO (http://www.esho.info),
-
Declaration of Helsinki (http://www.wma.net) and
-
Guideline for Good Clinical Practice (GCP) (http://www.emea.eu.int.com).
2.1 Physicians
Hyperthermia treatments are performed under the supervision and responsibility of a physician, e.g. a radiation oncologist, internal medicine specialist or a physician trained accordingly. During the application the hyperthermia, the physician is responsible for the following:
-
past medical history,
-
diagnosis and assessment of inclusion and exclusion criteria,
-
creating an overall oncology plan that includes the hyperthermia treatment,
-
imaging for preparation of the treatment (e.g. CT, MRI, PET and PET-CT),
-
the clinical part of the hyperthermia planning, i.e. defining target volume, outlining the target volume, outlining of the organs at risk, planning approval,
-
fractionation, i.e. the number, frequency and duration of hyperthermia treatments,
-
medication,
-
documenting the medical part of the treatment/intervention in case of complaints and
-
decision on the ongoing quality of a hyperthermia application. Namely, is the thermal dose sufficient to continue the treatment, or does it need to be stopped or whether it is possible to adapt the treatment strategy.
It is emphasised that a qualified physician must supervise the hyperthermia treatments. It is also remarked that in addition to the mentioned qualification, practical training in form of active participating in at least 20 new patients at an established hyperthermia centre is required until an additional qualification in hyperthermia has been gained. Practical training includes treatment indication, therapy planning and setting-up of the initial and all following treatments. In case of a treatment of sedated patients there is a need of permanent physical presence of a physician with experience in intensive care.
2.2 Physicists/engineers
A qualified physicist or engineer (e.g. medical physics experts or physicists and engineers trained accordingly) is responsible for the physical and technical aspects of the hyperthermia system. This area of responsibility includes the following:
-
checking the control software,
-
calibrating the probes,
-
quality assurance and consistency checks on the hyperthermia system,
-
documenting the device checks, failures and repairs,
-
specifying the technical treatment parameters, i.e. frequency, target, power distribution on different channels, maximum power, phase distribution,
-
positioning the applicator, in cooperation with the physician or radiology assistant or nurse,
-
thermal dosimetry and
-
intervention in case of technical failures.
If the hyperthermia equipment is operated by a MTRA, the responsible physicist/engineer must be on-call in order to take action within 5 min, in case of technical difficulties. A physicist/engineer must always be on-site during the initial setting.
Furthermore, the physicist or engineer is responsible for the phantom measurements or the physical–technical portion of the computer-supported planning of the hyperthermia. However, this task may be delegated to another trained employee, such as a medical technical assistant or a physician. The result is then optimised and accepted together with the physicist/engineer and the responsible physician.
In addition to the physicist/engineer being qualified, as already mentioned, practical training in the form of actively participating in the work involving at least 20 new patients, including planning and first setting of the treatment, at an established hyperthermia centre is required until an additional qualification in hyperthermia has been gained.
2.3 Technical assistants
The hyperthermia treatment can be assigned to a trained assistant for example an assistant in medical–technical radiology under the direct supervision of a physician. The technical assistant should be subjected to a training programme in the application of hyperthermia covering the points listed below. The individual points in the training schedule must be documented:
-
instruction in the physical aspects of heating using electromagnetic radiation,
-
general training in the equipment technology of the hyperthermia system, e.g. training according to the German Medizinprodukte Gesetz (MPG),
-
special training with instructions about normal and also error functions of the hyperthermia systems. This will include high reflection performance with poor cable connections or faulty antennas, as well as indications of faulty temperature measurements,
-
assistance in first setting and then applying deep hyperthermia treatments for at least 20 new patients under the instruction of a qualified physician or physicist or engineer or technical/radiology assistant. A training period of at least 3 months is recommended in order to successfully guarantee assistance in different body regions and
-
localising and documenting the position of the catheters, e.g. for diagnostic X-ray imaging.
2.4 Nurses
Nurses can support medical technician to perform hyperthermia treatments after joining a training programme. Furthermore, nurses are involved in the preparation of patients for the hyperthermia treatment, i.e. placement of intralumenal catheters as instructed by the prescription of the physician. The nurses are also responsible for monitoring the patient during therapy and may need to initiate any appropriate measures should the need arise because of a problem.
2.5 Arranging substitutes
Two responsible persons of any of the previously mentioned professions must be present during treatment (see 2.1, 2.2, 2.3) in order to take care of the patients and to control the hyperthermia device. It must be guaranteed that in case of illness or vacation of the designated pair of specialists, an adequate number of qualified and trained staff of all professional groups are available to act as substitute.
3 Hyperthermia quantities and their units
Measuring temperature is of great significance, in order to verify therapeutically necessary temperatures in the target volume and to avoid unwanted hot spots in the surrounding normal tissue. This must be achieved using suitable measuring probes. The probes must be placed in the area of the treatment volume and in risk areas for monitoring temperature in the normal tissue. Defining the risk areas is the task of the responsible physician and must be defined before treatment.
One of these probes must be placed in the target volume or in the vicinity of the target volume in order to obtain the tumour-related temperature. To preserve healthy tissue and possible risk organs, other probes are placed appropriately [3, 4, 15, 39]. It is also necessary to regularly record the systemic temperature, e.g. by measuring temperature orally. Relevant parameters for determining the quality of the hyperthermia in the target volumes are as follows [51]:
-
TD43(T90) or CEM43 T90 (min),
-
TD43(T50) or CEM43 T50 (min),
-
Tmean, Tmin, Tmax, T90, T50, T20, T10 (°C) and
-
the therapeutic time (in min; definition given in the Section 4.2.9),
Whereas the relevant parameter for preserving healthy tissue is:
-
Tmax in normal tissue (°C).
Relevant features for repeating treatments are as follows:
-
power, phase, offset and frequency,
-
position of the patient,
-
applicator and applicator type and
-
position of the applicator.
Finally, it should also be noted that every applicator has individual technical features regarding effectiveness and SAR control, (see Appendix 7.1).
4 Hyperthermia treatment
Only devices technically capable of achieving targeted and controlled heating in a target volume defined by a qualified physician, while simultaneously preserving normal tissue, may be used for hyperthermia treatments. Technically this goal can only be achieved using a regionally based performance check that is based on adequate thermometry. This guideline for deep regional hyperthermia is limited to“phased array” hyperthermia systems as the authors feel that patients in the western world are more adequately treated with“phased array” systems because the surface fat layer thickness in the relevant body region is often more than 2 cm (see also appendix 7.1). This category of systems is thus generally used in the active academic hyperthermia centres and this is reflected in the examples shown in this document.
For hyperthermia treatment intralumenally/intratumourally measured target temperatures must be reached as prescribed in the treatment plan. At the same time, areas at risk must be defined and protected according to the instructions of the responsible physician [15]. A procedure must be specified by the physician as to how to act in any case of complaints, e.g. if hot spots occur during therapy.
Relative to the treatment volume, the patient must be placed before treatment in a reproducible manner in the applicator [4]. Three-dimensional (3D) images (MRI, CT, US) or orthogonal X-rays must be taken to prepare the treatment. These examinations also serve to localise metallic implants (e.g. hips, stents, clips) inside and outside the treatment volume [40].
The presence of metallic implants is in principle a contraindication, but according to the experience from Rotterdam, several distributed smaller clips (maximum 1 cm length) are no problem for deep hyperthermia. However increased caution is recommended during treatment and supervision of a physician, and treatment planning is suggested to verify whether the implants cause temperature elevations. MR compatibility must be ascertained for treatment in a hybrid system, e.g. a hyperthermia system combined with MRT. Lateral laser lines and crosses must be installed in the treatment room in order to obtain exact reproducible alignment of the patient in the applicator.
4.1 Preparation
Similar to 3D treatment planning in radiation therapy, a 3D image in the dorsal position is performed to define the treatment volume. A qualified physician must specify the extent of the examination volume [4, 16]. The 3D imaging should be made with an empty bladder, since most patients will be attached to a urethral catheter. Also, during the examination, measurement catheters such as rectal probes may be positioned in advance.
Alternatively (but not essentially), pre-planning using a hyperthermia planning system (HTP) may be used. In this case, the planning system requirements for the imaging must be followed. As a further alternative, if the patient is treated in a hybrid system, the planning data can be acquired when the patient is positioned in the hyperthermia applicator to prepare the magnetic resonance tomography (MRT).
Example of necessary individual steps
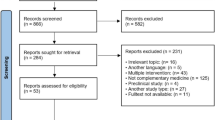
The following is an example of the necessary individual preparation steps for specifying a target point (similar to the isocentre in radiation therapy) for setting up the patient in the hyperthermia applicator (Fig. 1):
-
The first step for a combined radio-thermo therapy is defining the planning target volume (PTV) in the individual sections. Thereafter at the centre of the PTV, a hyperthermia target volume is determined, to define the hyperthermia target point. It is used to optimally position the patient relative to the centre of the applicator. For this purpose, the distance of this point in the cranio-caudal, lateral and dorso-ventral directions from a point marked on a patient that will also be identifiable in the radiation plan, is defined. From the shift a new hyperthermia target point is determined.
-
For patients who will not be receiving radiotherapy a reference point is marked the same manner as in the 3D imaging and the shift relative to this point is calculated.
-
The hyperthermia target point is defined dorso-ventrally and laterally in the 3D data set and if relevant together with the positioned measurement probe (intralumenal/intratumoural).
Imaging required for the positioning of the patient in the hyperthermia applicator. The target volume (PTV) is contoured in magenta. For the position, the distance of the reference point, which is marked on the patient during imaging, and the midpoint of the target volume must be obtained from the images. Sagittal slice upper left: Hyperthermia target point (intersection of the blue dorso-ventral line and the red cranio-caudal line), Reference point (intersection of the red dorso-ventral line and the red cranio-caudal line). Frontal slice lower left: Hyperthermia target point (intersection of the blue lateral line and the red cranio-caudal line). Transversal slice right: Hyperthermia target point (intersection of the blue lateral line and the red dorso-ventral line)
4.2 Treatment
Reproducibilty of the position of the patient with respect to the applicator is of great significance in hyperthermia treatment. It is a basic requirement for using the optimised control parameters of phase and power. The patient must always be positioned identically for all treatment fractions. The hyperthermia target point especially should always be at the same spot: a position within the active area of the applicator which can easily be heated [4].
4.2.1 Positioning the patient
For treatments using “phased array” applicators, the anterior–posterior diameter of the patient should not exceed 25 cm. Furthermore, the surface–applicator distance should be ≥ 5 cm for all applications. The applicator edges should be marked on the patient. Practical examples of procedures at the hyperthermia centres in Tübingen, Munich, Rotterdam and Amsterdam are given below.
Cranio-caudal positioning
-
Mark a reference point for the imaging
-
Position the patient relative to the reference point on the side laser
-
Mark of the cranio-caudal shift from the reference point—the hyperthermia target point, defined by the value previously specified in the imaging
-
Adjust the side laser to the hyperthermia target point
-
Position the applicator centre to the laser
-
Mark the applicator edges on the patient
Vertical positioning
Example from the Hyperthermia Centre, Tübingen:
-
Patient vertical position for the Sigma Eye applicator: with a filled bolus the patient must be lying in the centre of the applicator (measuring the distance ventral and dorsal at the cranial and caudal applicator edge), documentation of the measured values and the height of the head and foot bases of the Sigma Base (the latter facilitates adjusting the position for a second therapy fraction).
-
Patient vertical position for the Sigma-60 applicator: the patient is positioned horizontally in the applicator centre with an empty bolus. The applicator is then filled. With the uplift the patient will be positioned higher in the bolus, and therefore must sustain less pressure and is therefore able to tolerate the therapy better then when positioned in the applicator centre with a filled bolus. Measurement is made with a ruler only dorsally, on the cranial and caudal edge of applicator. Finally there is documentation of the measured values and applicable heights.
Example from the Hyperthermia Centre, Rotterdam:
-
An ultrasound distance meter is integrated in the ventral and dorsal antenna pair of the Sigma 60 applicator. This option is relevant for hyperthermia planning with pre-calculated SAR control, because the exact distance of the patient position relative to the applicator is required.
Example from the Hyperthermia Centre, Amsterdam:
-
The water bolus is filled. The patient is positioned with the os pubis in the centre of the AMC-4 applicator. This is in order to minimize the toxicity of the normal tissue.
4.2.2 Cooling
Cold packs may be applied to particularly sensitive or at-risk areas of the body surface, e.g. rectal bag.
4.2.3 Bolus control
If technically possible, the water in the bolus should be kept at room temperature. Adequate cooling of the surface, e.g. 25 °C (range 21–28 °C), must be guaranteed. This can be achieved with water circulation. For target areas on the surface, cooling may not be necessary.
Exceptions:
-
For sedated children the bolus temperature should be 33 °C at the begin of the treatment.
-
For the hybrid system with bolus circulation the thermometry measurements are stopped at least 2 min before MR thermometry. This is in order to avoid imaging artefacts.
4.2.4 Temperature measurement
Measurements using probes
The accuracy of the thermometry must be checked every day before treatment. For measuring temperature, probes which do not interfere with the HF field should be used, e.g. Bowman probes or fibre optic sensors. For other sensors the HF on/off cycle must be adjusted [41]. Usually measurements are taken at various specific predefined positions by applying a mapping method, or by using multiple sensors [53, 55, 58].
Probes are placed under the control of an imaging device (CT, US or MRI) in case an invasive measurement will be necessary.
Measurement using MR thermometry
When applying MR thermometry, at least one thermometry measurement must be carried out at regular intervals, e.g. every 10 min in the volume to be treated.
For the pelvic and thigh regions, proton resonance frequency shift (PRFS) measurement by means of uncorrected phase images of a gradient-echo sequence with two echoes and subsequent drift compensation is often suitable. However, another MR thermometry method must be used especially if high fat content regions are to be measured. This is because the PRFS does not display the temperature in fat tissue. For example a T1-measurement or a spectroscopic method may be used. For moving organs, use suitable triggering, or reduce the measurement to a smaller volume, in order to measure during a breath-hold cycle [9, 20, 21, 22, 29, 34, 46, 47, 49, 52].
The measurement T2-fat saturated, high resolution imaging in different sections before and after the therapy is helpful when the patient may have suffered subcutaneous burns. Other measurement techniques such as flow, perfusion or spectroscopy can be used as alternative methods if the study requires such methods.
The MR imaging must be checked for quality during the therapy, since movement artefacts and compatibility problems may occur. In the case of failure of the MR thermometry during therapy (e.g. due to unwanted intermediate shim or patient shift), the thermometry must also be performed with the same methods and time intervals and must be documented in the same way as with documentation of regional hyperthermia without MR control.
4.2.5 Application control with E-field probes
E-field probes may also be used for control but when using these probes it is necessary to be particularly exact when positioning the patient and probes. For the Sigma-Eye, Sigma-60 and AMC applicator it is important to align the E-field probes with the longitudinal axis of the applicator [10].
For example, when applying the AMC hyperthermia system at the Amsterdam Hyperthermia Centre, the phase settings that are needed to obtain an optimum heating of the target volume, are determined at the start of the application using an E-field probe, positioned in or near the target area. The optimum phase difference for each relevant pair of antennas pair is automatically measured. The settings determined in this way are compared to the specification from the CT-based hyperthermia planning. They are then used as the starting setting, so long as they do not significantly deviate from the planning based values.
4.2.6 Attaching the catheter
Invasive temperature measurement catheters are placed by the physician, for example under CT control. All other measurement catheters (e.g. probes on the skin and/or endolumenal probes) are placed by the physician and/or the nursing staff. At least one probe must be positioned either within or close to the tumour. It is noted that usually there is no control using X-ray imaging and also that the Amsterdam Centre uses a pelotte for cervical measurements in order to increase reproducibility.
4.2.7 Temperature measurement rules: mapping method for pelvic hyperthermia
Temperature measurement assisted by use of the so-called mapping method, in which the probe is moved in a catheter through a treatment volume, must be completed using specified conditions which are as follows:
-
firstly map before starting treatment with the power OFF in order to determine the intralumenal path and to check whether all probes are moving correctly,
-
then map only with the power ON condition,
-
mapping interval: 5–10 min and
-
mapping length: up to 16 cm.
Remark: Detailed temperature measurement regulation can be seen in the relevant study protocol which is to be used.
Remark: It is also noted that in the Berlin Charité Hyperthermia Centre the mapping procedure is performed for example, once before and once after switching the power OFF” at the end of the section.
4.2.8 Temperature performance characteristics
Temperature performance characteristics for hyperthermia treatment are specified for normal tissue for the maximum temperature and for the hyperthermia target volume the maximum and minimum temperatures are specified.
The maximum tolerable temperatures of normal tissue are assessed on the one hand by hyperthermia effects and on the other hand by the position of the target volume of the tumour, or by any ancillary medication. An important aspect is the sensitivity to pain which in normal tissue should not occur when undergoing therapy. Generally in normal tissue the temperature should not exceed 43 °C. Within hyperthermia target volumes 44 °C should not be exceeded for a prolonged period. A detailed specification of the maximum and minimum temperatures for the individual volumes/organs will be provided in the relevant study protocol.
As an example, the bladder can be the target organ for urothelial carcinoma and should receive a far greater tolerance temperature than for cervical or rectal carcinoma therapy. Alternatively, when applying toxic chemotherapy to the bladder, a far lower tolerance threshold should be applied.
4.2.9 Treatment period
The treatment period consists of the heating-up period and therapy period:
-
the heating-up period is until the target temperature is reached, or alternatively is a maximum of 30 min when the temperature is not reached and
-
the therapy period is 60 min.
4.2.10 Applicator control
With specific settings for frequency, phase and amplitude, the hyperthermia field is focussed within the treatment volume. This will result in selective heating while simultaneously preserving the surrounding normal tissue.
Hyperthermia planning
For computer supported planning, the plans must be documented. Planning must meet minimum requirements, as indicated in Appendix 7.2.
Examples for the setting of applicators
Sigma 60 and Sigma-Eye applicator type. Offset setting for a focused field in the applicator centre (e.g. by using a lamp phantom); this setting is generally used for all the following therapies. Target setting is provided according to 3D imaging (e.g. planning CT or MRI). It is noted that if the target volume is far above the navel, then the applicator may be positioned, with limitations, through the axilla, which is generally not exactly in the target volume. The resulting difference can generally be corrected using the Sigma Eye or Sigma-Eye MR applicator by means of a field shift.
Amsterdam AMC system. The target is set by E-field probes or by planning CT imaging.
4.2.11 Starting procedure for hyperthermia treatment
-
For the start of the first treatment it is recommended to start with about one-third to two-thirds of the required power for the specific tumour localisation and applicator alignment. Then from the second treatment onwards, data for the positioning and the power set are adapted from the settings used during the prior treatment.
-
Temperature increases of more than 2 °C in 5 min should be avoided. A temperature increase of 1 °C in 5 min is optimal.
-
Power should be increased in the case of a temperature increase of less than 0.6 °C in 5 min.
-
The objective is for efficient heating using the required power still tolerable for the patient.
4.2.12 Complaints caused by treatment
In the case of complaints caused by treatment, such as pressure pain or hot spots, the power must be shut off immediately, in order to determine whether the pain is caused by the radiated power. If after a short period (about 30 s) an improvement can be seen (for HF power dependent complaints), the control parameter (e.g. focus, amplitude, power) is changed. For pain caused by the tumour or positioning, pain medication may be given or the patient must be moved. Water bags with de-ionized water should be applied for complaints that occur inside the treatment region and bags filled with 0.9% NaCl outside the treatment region. Under inconvenient conditions hot spots can occur at the edge or even outside of the applicator creating enhanced oedemas. In such cases besides water bags or reduction of the amplitude a hyperthermia planning procedure can be carried out.
Detailed instructions that are applied in Rotterdam for complaints caused by the treatment have been reported [56]. Also, for example, the Amsterdam (AMC) Hyperthermia Centre has a strategy to prevent pain complaints by instructing patients to indicate normal tissue locations of high temperature before these reach the level of real pain. Power or phase settings for individual antennae are then altered to substantially reduce power at the indicated location without reducing or interrupting total power.
5 Documentation, analysis and audits
The following points should be considered for evaluating clinically relevant hyperthermia studies [3, 14, 15]. The exact evaluation procedure can be obtained from the particular study protocols.
Examples of evaluation procedures are given below:
-
tumour response according to RECIST [Response Evaluation Criteria In Solid Tumors (http://www.RECIST.com)] evaluated after 6 weeks of combined radiothermotherapy. For hyperthermia combined with chemotherapy evaluation after at least three chemotherapy cycles.
-
tumour response (CR, PR, SD, PD) evaluated after 6 weeks with assistance from clinical examinations and/or imaging,
-
local tumour control, i.e. percentage of tumours in CR at specified time intervals (1, 2, 3 years),
-
time to progression (TTP),
-
overall survival (OS) at specified time intervals,
-
local event-free survival (LEFS) and
-
disease-free survival (DFS).
-
Toxicity:
-
Grade 3–4 acute toxicity (acute means treatment related toxicity occurring during treatment and/or continued up to six weeks after completing the treatment).
-
Grade 3–4 late toxicity (late means treatment related toxicity that lasted ≥ 6 months after completing the treatment).
-
The following statement concerning this guideline has to be included in each protocol:
-
Step 1:
-
Audit of the institution on the base of the documentation after ¼ of the proposed study period.
-
The visit of the institution depends on the quality of the presented data.
-
-
Step 2: Visit of the institution, in case of a need after the examination of the documents.
-
The institution will be visited by a member of the ESHO Technical Committee, in case of a insufficiency in the adherence of this guideline.
-
The institution is responsible for the support of the auditor.
-
5.1 Procedures
Before therapy, the responsible qualified physician must define the indications for the hyperthermia treatment, taking into account inclusion and exclusion criteria. This is followed by obtaining the past medical history and patient information (see Appendix 7.3) and is completed using the study or therapy logs.
Moreover, the decision on indications for treatment should be made by a qualified physician taking any special precautionary measures into account. For example the physician should ensure that the patient is without any fever when starting the treatment. Also, there should not be any open wounds (e.g. burn, abscess, skin defect, recent surgery scar) that could possibly be in the area of the applicator during treatment. In the case when treatment is actually indicated and performed in the presence of healing/healed wounds, it is documented with pictures before and after treatment. Furthermore, skin defects, paresthesia in the target volume are monitored with temperature measurement probes.
The patient must be able to communicate during the treatment or is still responsive after an analgesic sedation (choice and dosage of the adequate drug must fulfil these requirements; when children are treated, only a physician with acceptable experience in intensive care is allowed to prescribe the drugs [45]). It is also noted that because of claustrophobia, very few patients can tolerate the therapy when being positioned in the ring applicator for one hour or longer. The feasibility of hyperthermia treatment can be determined in advance by assessing the effect of positioning the patient. A mild sedative may be very helpful. Finally, any adhesive bandages must be replaced with a simple band-aid in consultation with the nursing staff.
5.1.1 Determining the indication for hyperthermia treatment
Appendix 7.2 includes an example with the relevant information that should be obtained for the medical history and which must be taken into account when determining the indication for the hyperthermia treatment. Additional information is defined in the treatment logs.
5.1.2 CT imaging
As already described in Section 4.1 Preparation, the patient will receive a CT examination. This examination is used to prepare the patient for treatment: delineation of the target volume, documentation of the catheters and conduct (but not essentially) computer-supported hyperthermia treatment planning (HTP). The examination is performed with the patient in the dorsal position where they are positioned in the same way as in the applicator. It is also important that they have an empty bladder.
5.2 Documentation
The complete documentation of the hyperthermia treatment consists of a physical–technical and a clinical portion.
For patient-related medical data, the general data protection regulations and doctor–patient confidentiality apply: for example see Section 203 in the German regulations. Furthermore, the national hospital laws are applicable for processing and using patient data. Recording the patient data electronically with text and image information as well as with device data would be preferred. However, the national data protections laws must be met. Availability and readability of the treatment-relevant data must be ensured for a period of 30 years.
5.2.1 Physical–technical documentation
All treatment relevant system control parameters of the system (e.g. power and phase position) and all temperature measurement values must be stored. Changes to the control parameters must be documented with chronological and clinical reference. Temperatures must be documented in a manner that they can chronologically be related to the respective measurement location or catheter.
Data log of the course of treatment
Logging all temperature deviations, power or water dependent pain, pain caused by position in the applicator, treatment interruptions or stopping treatment.
Data log of the hyperthermia system
All hyperthermia device-related data must be documented in the device logbook. The recordings must be compared to the relevant national law, e.g. the German Medizinprodukte Gesetz (MPG).
5.2.2 Clinical documentation
The clinical documentation describes the patient positioning, the medication including cytotoxic drugs and all other clinical parameters of the patient, including any changes and side effects caused by the therapy. All such changes and events must be documented with a chronological reference to the hyperthermia treatment.
5.2.3 Patient positioning documentation
Patient positioning should be documented in case of special movements necessary for the treatment with all relevant markings by means of photographs or MR images. Possible skin changes (e.g. those caused by hot spots) should be documented, if possible during, but at least after ending/terminating the treatment.
5.2.4 Side effects
The hyperthermia (in terms of these guidelines) is not a separate therapy mode but supplements systemic chemotherapy or radiation therapy. The unwanted effects of the combined treatment therefore correspond primarily to the spectrum of side effects of the chemotherapy or radiation therapy, although the side effects of the primary therapy can be intensified by tissue heating during hyperthermia. Classifying the degree of severity should follow the internationally established scoring systems.
-
CTCAE version 4.03 for chemotherapy-associated side effects and
-
RTOG version 2.0 for radiation-specific side effects.
Hyperthermia-specific side effects
Additionally, side effects that are specifically caused by the hyperthermia treatment should be recorded. Unwanted higher temperature in the skin or the healthy tissue is the main risk, which is increased in patients with disturbed temperature sensitivity, for example in polyneuropathy. Low grade high temperatures are accompanied with false sensations or pain and skin irritation and/or local oedema. In the case of sustained overheating of tissue, depending on the severity, tissue damage and necrosis may result. The temperature threshold for such irreversible damage is 44–46 °C depending on the tissue type [24, 59]. The specific side effects are given in Tab. 2.
5.3 Analysis of the physical/technical data of the treatment
5.3.1 Standardization
In order to create comparable analyses for all study participants, the relevant data are extracted from the stored values and, as far as possible, analysed using the standard software (e.g. RHyThM Rotterdam Hyperthermia Thermal Modulator; d.fatehi@erasmusmc.nl) [14]. A significant feature of the software to be used is the allocation of treated organs/tissue and the normal tissue to the determined thermal data. The programme calculates and documents all necessary thermal dose parameters (e.g. Tmax, Tmean, T20/50/90, CEM43T90), the applicator control parameters and the therapy period.
If temperature is measured only on the skin’s surface, then only Tmin and Tmax must be stated. Alternative assessment modules must be based on identical calculation principles and define the same thermal dose parameters, e.g. the module used in the Amsterdam Hyperthermia Centre.
5.3.2 Example of data recording and analysis
The relevant values for the analysis (e.g. using RHyThM) must be specified in the study log which is used. An example of the data recording for a rectal carcinoma is shown in Tab. 3.
Abbreviations
- CEM43T90 :
-
Equivalent minutes at 43 °C
- CR:
-
Complete tumour response
- CT:
-
Computer tomography
- CTCAE v4.03:
-
Common toxicity criteria adverse events
- DEGRO:
-
Deutsche Gesellschaft für Radioonkologie
- DFS:
-
Disease-free survival
- E-field:
-
Electric field
- ESHO:
-
European Society of Hyperthermic Oncology
- FE:
-
Finite element
- Gy:
-
Gray
- http:
-
Hypertext transfer protocol
- HTP:
-
Computer hyperthermia planning
- IAH:
-
Interdisciplinary working group
- LEFS:
-
Local event-free survival
- LP:
-
Local tumour progression
- MPG:
-
German Medizinprodukte Gesetz
- MR:
-
Magnetic resonance
- MRI:
-
Magnetic resonance imaging
- MRT:
-
Magnetic resonance tomography
- MTRA:
-
Technician in radiology (“Medizinisch Technischer Radiologie Assistant”)
- OS:
-
Overall survival
- P:
-
Power
- PBH:
-
Partial body hyperthermia
- PET:
-
Positron emission tomography
- PRFS:
-
Proton resonance frequency
- PTV:
-
Planning target volume
- QMHT:
-
Quality management in hyperthermia (defined in this guideline)
- RECIST:
-
Response evaluation criteria in solid tumors
- RHT:
-
Regional hyperthermia
- RHyThM:
-
Rotterdam Hyperthermia Thermal Modulator
- RTOG:
-
Radiation Therapy Oncology Group
- SAR:
-
Specific absorption rate
- TTP:
-
Time to progression
- US:
-
Ultrasound
References
Balasubramaniam TA, Bowman HF (1977) Thermal conductivity and thermal diffusivity of biomaterials: a simultaneous measurement technique. J Biomech Eng 99:148–154
Bruggmoser G, Bauchowitz S, Canters R et al (2011) Quality Assurance for Clinical Studies in Regional Deep Hyperthermia. Strahlenther Onkol 187(10):605–609
Bruijne M de, Holt B van der, Rhoon GC van, Zee J van der (2010) Evaluation of CEM43 degrees CT90 thermal dose in superficial hyperthermia: a retrospective analysis. Strahlenther Onkol 186(8):436–443
Canters RA, Franckena M, Paulides MM, Rhoon GC van (2009) Patient positioning in deep hyperthermia: influences of inaccuracies, signal correction possibilities and optimization potential. Phys Med Biol 54:3923–3936
Canters RA, Wust P, Bakker JF, Rhoon GC van (2009) A literature survey on indicators for characterisation and optimisation of SAR distributions in deep hyperthermia, a plea for standardisation. Int J Hyperthermia 25:593–608
Chato JC (1968) A method for the measurement of the thermal properties of biological materials. In: Chato JC (ed) Thermal Problems in Biotechnology, ASME symposium series. American Society of Mechanical Engineers, New York
Chato JC (1990) Fundamentals of bioheat transfer. In: Gautherie M (ed) Thermal dosimetry and treatment planning. Springer, New York, p 51
Cooper TE, Trezek DJ (1971) Correlation of thermal properties of some human tissue with water content. Aerospace Med 42:24–27
Craciunescu OI, Stauffer PR, Soher BJ et al (2009) Accuracy of real time noninvasive temperature measurements using magnetic resonance thermal imaging in patients treated for high grade extremity soft tissue sarcomas. Med Phys 36:4848–4858
Crezee J, Haaren PM van, Westendorp H et al (2009) Improving locoregional hyperthermia delivery using the 3-D controlled AMC-8 phased array hyperthermia system: a preclinical study. Int J Hyperthermia 25(7):581–592
Drane CR (1981) The thermal conductivity of the skin of crocodilians. Comp Biochem Physiol 68A:107–110
Dumas A, Barozzi GS (1984) Laminar heat transfer to blood flowing in a circular duct. Int J Heat Mass Trans 27:391–398
Eckert F, Fehm T, Bamberg M, Müller AC (2010) Small cell carcinoma of vulva: curative multimodal treatment in face of resistance to initial standard chemotherapy. Strahlenther Onkol 86(9):521–524
Fatehi D, Bruijne M de, Zee J van der, Rhoon GC van (2006) RHyThM, a tool for analysis of PDOS formatted hyperthermia treatment data generated by the BSD2000/3D system. Int J Hyperthermia 22:173–184
Fatehi D, Zee J van der, Notenboom A, Rhoon GC van (2007) Comparison of intratumor and intraluminal temperatures during locoregional deep hyperthermia of pelvic tumors. Strahlenther Onkol 183(9):479–486
Franckena M, Fatehi D, Bruijne M de et al (2009) Hyperthermia dose-effect relationship in 420 patients with cervical cancer treated with combined radiotherapy and hyperthermia. Eur J Cancer 45(11):1969–1978
Gabriel C, Gabriel S, Courthout E (1996) The dielectric properties of biological tissues: I. Literature survey. Phys Med Biol 41:2231–2250
Gabriel S, Lau R-W, Gabriel C (1996) The dielectric properties of biological tissues: II. Measurements in the frequency range 10 Hz to 20 GHz. Phys Med Biol 41:2251–2269
Gabriel S, Lau R-W, Gabriel C (1996) The dielectric properties of biological tissues: III. Parametric models for the dielectric spectrum of tissues. Phys Med Biol 41:2271–2280
Gellermann J, Wlodarczyk W, Feussner A et al (2005) Methods and potentials of magnetic resonance imaging for monitoring radiofrequency hyperthermia in a hybrid system. Int J Hyperthermia 21:497–513
Gellermann J, Wlodarczyk W, Hildebrandt B et al (2005) Noninvasive magnetic resonance thermography of recurrent rectal carcinoma in a 1.5 Tesla hybrid system. Cancer Res 65:5872–5880
Gellermann J, Hildebrandt B, Issels R et al (2006) Noninvasive magnetic resonance thermography of soft tissue sarcomas during regional hyperthermia: correlation with response and direct thermometry. Cancer 107:1373–1382
Grayson J (1952) Internal calorimetry in the determination of thermal conductivity and blood flow. J Physiol 118:54–72
Haveman J, Smals OA, Rodermond HM (2003) Effects of hyperthermia on the rat bladder: a pre-clinical study on thermometry and functional damage after treatment. Int J Hyperthermia 19(1):45–57
Hoffmann K-T, Rau B, Wust P et al (2002) Restaging of locally advanced carcinoma of the rectum with MR imaging after preoperative radio-chemotherapy plus regional hyperthermia. Strahlenther Onkol 178:386–392
Holmes KR, Ryan W, Chen WW (1983) Thermal conductivity and H2O content in rabbit kidney cortex and medulla. J Therm Biol 8:311–313
Holmes KR, Chen MM (1979) Local thermal conductivity of Para-7 fibrosarcoma in hamster. Advances in Bioengineering, New York: ASME, pp 147–149
Holmes KR, Adams T (1975) Epidermal thermal conductivity and stratum corneum hydration in cat footpad. Am J Physiol 228:1903–1908
Hynynen K, McDannold N (2004) MRI guided and monitored focused ultrasound thermal ablation methods: a review of progress. Int J Hyperthermia 20:725–737
Hua Y, Ma S, Fu Z et al (2011) Intracavity hyperthermia in nasopharyngeal cancer: a phase III clinical study. Int J Hyperthermia 27:180–186
Issels RD (2008) Hyperthermia adds to chemotherapy. Eur J Cancer 44(17):2546–2554
Issels RD, Lindner LH, Verweij J et al (2010) Neo-adjuvant chemotherapy alone or with regional hyperthermia for localised high-risk soft-tissue sarcoma: a randomised phase 3 multicentre study. Lancet Oncol 11(6):561–570
Kok HP, Haaren PM van, Kamer JB van de et al (2005) High resolution temperature based optimisation for hyperthermia treatment planning. Phys Med Biol 50(13):3127–3141
Konstanczak R, Wust P, Sander B et al (1997) Thermometrie durch Messung der chemischen Verschiebung eines Lanthanidenkomplexes. Strahlenther Onkol 173(2):106–116
Kotte A, Leeuwen G van, Bree J de et al (1996) A description of discrete vessel segments in thermal modelling of tissues. Phys Med Biol 41(5):865–884
Kuroda K (2005) Non-invasive MR thermography using the water proton chemical shift. Int J Hyperthermia 21:547–560
Kvadsheim PH, Folkow LP, Blix AS (1996) Thermal conductivity of Minke whale blubber. J Therm Biol 21:123–128
Kvadsheim PH, Folkow LP, Blix AS (1994) A new device for measurement of the thermal conductivity of fur and blubber. J Therm Biol 19:431–435
Lagendijk JJW, Rhoon GC van, Hornsleth SN et al (1998) ESHO quality assurance guidelines for regional hyperthermia. Int J Hyperthermia 14:125–133
Lee ER, Sullivan DM, Kapp DS (1992) Potential hazards of radiative electromagnetic hyperthermia in the presence of multiple metallic surgical clips. Int J Hyperthermia 8:809–817
De Leeuw AAC, Crezee J, Lagendijk JJW (1993) Temperature and SAR measurements in deep-body hyperthermia with thermocouple thermometry. Int J Hyperthermia 9(5):685–697
Lutgens L, Zee J van der, Pijls-Johannesma M et al (2010) Combined use of hyperthermia and radiation therapy for treating locally advanced cervical carcinoma. Cochrane Gynaecological Cancer Group (ed) The cochrane collaboration, Issue 1. Wiley, http://www.thecochranelibrary.com
Mantel F, Frey B, Haslinger S et al (2010) Combination of ionising irradiation and hyperthermia activates programmed apoptotic and necrotic cell death pathways in human colorectal carcinoma cells. Strahlenther Onkol 186:587–599
Milani V, Pazos M, Issels RD et al (2008) Radiochemotherapy in combination with regional hyperthermia in preirradiated patients with recurrent rectal cancer. Strahlenther Onkol 184:163–168
Ott OJ, Issels RD, Wessalowski R (2010) Hyperthermia in oncology—principles and therapeutic outlook. Uni-Med Verlag AG, Bremen
Peller M, Muacevic A, Reinl H et al (2004) MRI-assisted thermometry for regional hyperthermia and interstitial laser thermotherapy. Radiologe 44:310–319
De Poorter J, Wagter CD, De Deene Y et al (1995) Noninvasive MRI thermometry with the proton resonance frequency _PRF_method: in vivo results in human muscle. Magn Reson Med 33:74–81
Pennes HH (1948) Analysis of tissue and arterial blood temperatures in the resting human forearm. J Appl Physiol 1:93–122
Quesson B, Zwart JA de, Moonen CT (2000) Magnetic resonance temperature imaging for guidance of thermotherapy. J Magn Reson Imaging 12:525–533
Rau B, Wust P, Gellermann J et al (1998) Phase-II-Studie zur pr operativen Radio-Chemo-Thermo-Therapie beim lokal fortgeschrittenen Rektum-Karzinom. Strahlenther Onkol 174(11):556–565
Sapareto SA, Dewey WC (1984) Thermal dose determination in cancer therapy. Int J Radiat Oncol Biol Phys 10(6):787–800
De Senneville BD, Quesson B, Moonen TCW (2005) Magnetic resonance temperature imaging. Int J Hyperthermia 21:515–531
Valvano JW, Cochran JR, Diller KR (1985) Thermal conductivity and diffusivity of biomaterials measured with self-heated thermistors. Int J Thermophys 6:301–311
Valvano JW, Chitsabesan B (1987) Thermal conductivity and diffusivity of arterial wall and atherosclerotic plaque. Lasers Life Sci 1:219–229
Valvano JW, Allen JT, Bowman HF (1981) The simultaneous measurement of thermal conductivity, thermal diffusivity, and perfusion in small volumes of tissue. ASME 81-WA/HT-21
Wal E van der, Frankena M, Wielheesen DHM et al (2008) Steering in locoregional deep hyperthermia: evaluation of common practice with 3D-planning. Int J Hyperthermia 24:682–693
Tilly W, Gellermann J, Graf R et al (2005) Regional hyperthermia in conjunction with definitive radiotherapy against recurrent or locally advanced prostate cancer T3 pN0 M0. Strahlenther Onkol 181:35–41
Wust P, Gellermann J, Harder C (1998) Rationale for using invasive thermometry for regional hyperthermia of pelvic tumors. Int J Radiat Oncol Biol Phys 41:1129–1137
Yarmolenko PS, Moon EJ, Landon C et al (2011) Thresholds for thermal damage to normal tissues: an update. Int J Hyperthermia 27(4):320–343
Van der Zee J, Gonzalez Gonzalez D, Van Rhoon GC et al (2000) Comparison of radiotherapy alone with radiotherapy plus hyperthermia in locally advanced pelvic tumours: a prospective, randomised, multicentre trial. Dutch Deep Hyperthermia Group. Lancet 355(9210):1119–1125
Van der Zee J (2002) Heating the patient: a promising approach? Ann Oncol 13(8):1173–1184
Acknowledgements
The authors thank the members of the Atzelsberg Clinical Circle of the IAH for their constructive comments and their continuous stimulation to prepare the quality assurance document for regional deep hyperthermia.
Conflict of interest
On behalf of all authors, the corresponding author states the following: the authors have no financial interest in any company selling hyperthermia treatment and planning equipment. The opinion of the authors is solely based upon the available scientific knowledge and their personal experience in the clinical application of hyperthermia.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors of this document are also members of the Atzelsberg Circle in the IAH of the “Deutsche Krebsgesellschaft”.
Electronic supplementary material
66_2012_176_MO1_ESM.pdf
Deutsche Version "Leitlinie für die klinische Applikation, die Dokumentation und die Analyse klinischer Studien bei der regionalen Tiefenhyperthermie" (PDF 1,9 MB)
7 Appendix
7 Appendix
7.1 Applicator requirements
7.1.1 Minimum requirements
An applicator for deep hyperthermia has to meet certain requirements with regard to the characteristics of the energy distribution in order to have the basic ability to provide preferential heat to tumours located centrally in the human body. Ideally, the energy deposition in the target volume is higher than the energy deposition in healthy tissue. To obtain this feature, focusing of the energy distribution is essential as well as the ability to steer the focus. Based on phantom results a minimum ratio of energy deposition in the target (SARtarget) and energy deposition in the healthy tissue (SARnon-target) is defined [5].
A proposal for three conditions for a standardised hyperthermia test phantom for the checking of applicator characteristics in the range 75–140 MHz is as follows:
-
phantom of diameter 20 cm and length 60 cm,
-
abdomen-equivalent tissue material (2 g/l NaCl in distilled water), i.e. effective conductivity (σ) 0.32 S/m at 20 °C and relative dielectric permittivity (εr) 80 and
-
definition of a centrally located cylindrical target volume of diameter 5 cm and length 10 cm, with the axial orientation of the target similar to that of the phantom.
Each applicator used in deep hyperthermia must be able to reach an average SAR level inside the target volume that is higher than the average SAR level in the whole phantom. Hence, for any applicator the ratio of SARtarget and SARnontarget in the phantom must be minimally above 1.5 in order to be considered as an applicator feasible to induce deep heating in the pelvic and abdominal regions. Whether an applicator fulfils this minimum criterion can be checked by measurements and simulations using the standardised hyperthermia test phantom, appropriate measuring devices and a QA protocol such as defined by the European Society for Hyperthermic Oncology (ESHO). The Rotterdam group calculated the ratio of SARtarget and SARnontarget in the phantom for the Sigma 60 and Sigma Eye applicators and found values of 3.0 and 4.3, respectively.
7.1.2 Requirements for clinical hyperthermia treatments
It is not possible to extract guidelines for hot spot levels from phantom measurements. To set a minimum requirement, the authors have therefore chosen a requirement based on current practice with the most frequently used device for deep hyperthermia, i.e. the Sigma 60, with which more than 5,000 patients have been treated with deep hyperthermia in Europe. For this device, the Rotterdam group has analysed their extensive modelling in 10 patients with locally advanced cervical cancer. This analysis provides sufficient data to select a maximum permitted SAR level for hot spots in healthy tissue in order to apply deep hyperthermia at an acceptable level of quality, i.e. to measure therapeutic temperatures in the target region. For these 10 patients Manufacturers of new deep hyperthermia equipment are expected to obtain the patients models through proper procedures and to make sure that these models are representative for the average dimensions of their patient population. these values are SARtumor = 74 ± 32 W/kg (mean ± 1 standard deviation) and for hot spots SARmax= 290 ± 100 W/kg (mean ± 1 standard deviation), with an input power to the Sigma 60 applicator of 700 W. In this analysis hot spots are defined as all hot spots with a total volume of 0.1% of the tissue volume (V0.1) with the highest SAR. This leads to the conclusion that hot spot SAR levels (in the 0.1th percentile) should generally not exceed the SARtarget by a factor of 4. Applicators that meet both criteria: SARtarget> 1.5 • SARnon-target and SAR0.1< 4 • SARtarget are generally able to heat a patient up to therapeutic temperatures.
7.2 Minimum requirements for hyperthermia treatment planning
Treatment positions are required to coincide with the position modelled in planning (maximum deviation 1 cm) in order to reliably simulate optimum treatment parameters using computer supported hyperthermia planning (HTP) [1, 7, 33]. The positioning of the patient is described in more detail in Section 4.2.1. Furthermore, control of the radio frequency emitted from the antenna is essential with an amplitude and phase accuracy better than 5%/5° in order to guarantee reliable modelling of the power distribution with HTP. Preferably, the SAR measurement sensors or the temperature measurement using non-invasive thermometry (NIT) for feedback of the current SAR or the temperature distribution calculated with the planning system can be used.
The image of a 3D dataset for the hyperthermia planning using a CT or MRT scan must be performed, as far as possible, in the treatment position during hyperthermia. This means that the imaging must be completed for example, in the patient position grid. The layer thickness of the planning data must be selected optimally for the E-field calculation method to be used later. For example, 5 mm for finite elements (FE) with tetraedral grids, or higher resolution for FDTD.
Hyperthermia planning is started by segmenting the different tissue types. Two levels of segmentation are distinguished:
-
1.
Hounsfield unit (HU) based automatic segmentation. This is based on the Hounsfield values of raw CT data records. The tissue types lung, fat, muscle and bone can be automatically segmented. The bowel volume and the organs are usually segmented as muscle.
-
2.
Full organ segmentation. Additionally for the HU based automatic segmentation, the bowel and organs of the pelvis are segmented separately.
If using the FE method on tetrahedron grids, it must be guaranteed that the side length of the tetrahedrons are smaller than 1/10th of the wavelength in the tissue, e.g. 90 MHz, muscle and smaller than 3 cm. The dielectric and temperature relevant tissue properties needed for the calculations can be obtained from well documented literature sources [6, 8, 11, 12, 17, 18, 19, 23, 26, 27, 28, 37, 38] or from individual measurements (http://www.brooks.af.mil/AFRL/HED/hedr/reports/dielectric/home.html; [53, 54, 55]).
In the case of sole SAR modelling, after segmenting and calculating the electromagnetic fields, a patient-specific optimisation routine should be implemented, which maximises the SAR coverage of the target area and minimises the energy deposit in the healthy tissue. Furthermore, it should be possible to define regions in which additional specific limit values can be specified for the optimisation.
An equivalent approach is necessary for temperature modelling, which maximises the temperature in the target area and limits it in the healthy tissue to absolute maximum temperature values [27]. That is, 44 °C in healthy tissue and 42 °C in bone marrow for 30 min. Thermal and perfusion properties can be found in the literature [37, 38, 53, 54, 55]. The impact of blood flow can be incorporated using either the bioheat equation or by modelling discrete vessels [6, 12, 35, 48].
The transfer of the optimum therapy parameter for the power control should preferably occur automatically/online, in order to minimise errors. The treatment position of the patient and the therapy parameters must be adequately documented for the patient documentation (see Section 5.2).
7.3 Documentation of medical history
Example: information about disease, previous history and treatment planning
General information:
-
patient identification
-
date of birth
-
patient identification number
Disease information:
-
current disease
-
date of diagnosis: DDMMYYYY
-
examining physician
-
histology
-
medical history of current disease
-
first symptoms
-
date of first symptoms
-
duration of symptoms
-
Karnofsky status at time of diagnosis
-
previous diseases
-
other information
-
-
-
family medical history (if relevant)
-
diseases suffered by family members (parents and siblings)
-
-
co-existing diseases
-
diabetes mellitus: yes/no
-
heart disease: yes/no
-
if yes, heart failure: yes/no
-
-
thrombosis < 3 months (embolism risk)
-
Oedema in the therapy region or directly bordering it: yes/no
-
Personal information:
-
occupation(s)
-
social history
-
living situation
-
number of children
-
-
alcohol consumption
-
nicotine consumption (cigarettes, cigars, pipe smoking)
-
height (m)
-
weight (kg)
-
pregnant: yes/no
-
currently claustrophobic: yes/no
Clinical examination results:
-
general condition
-
external examination
-
internal examination
-
neurology
Previous therapies:
-
pre-treatments
-
radiation therapy
-
chemotherapy
-
Justification for therapy:
-
curative or palliative
-
neoadjuvant: yes/no
Contraindications:
-
pacemaker/defibrillator/neurostimulator: yes/no
-
metal implants: yes/no
-
other possible contraindications
-
burning: yes/no
-
abscess: yes/no
-
skin damage: yes/no
-
recent operation scar: yes/no
-
Consent form:
-
written consent provided: yes/no
Objective of the treatment:
-
treatment as part of a study or series of case studies: yes/no
-
description of the study or case studies
-
-
information about the treatment volume based on the 3D imaging
-
target volume
-
risk volume
-
Treatment plan:
-
radiation therapy
-
CT supported 3D planning
-
planned reference dose: xx.x Gy
-
fractionation: x times per week
-
fractionation dose: x.x Gy/week
-
-
chemotherapy
-
details
-
-
hyperthermia
-
information about the treatment volume
-
planning target volume (PTV)
-
positioning of the patient in the applicator (longitudinal, vertical)
-
-
volume at risk
-
verification
-
probe thermometry, MR thermometry
-
-
Rights and permissions
About this article
Cite this article
Bruggmoser, G., Bauchowitz, S., Canters, R. et al. Guideline for the clinical application, documentation and analysis of clinical studies for regional deep hyperthermia. Strahlenther Onkol 188 (Suppl 2), 198–211 (2012). https://doi.org/10.1007/s00066-012-0176-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-012-0176-2