Abstract
Purpose
Stent-retriever thrombectomy (SRT) for acute intracranial large artery occlusion (LAO) may not result in permanent recanalization in rare cases, e.g. due to an underlying stenosis or dissection. In this specific patient group, rescue stent angioplasty (RSA) may be the only treatment option to achieve permanent vessel patency and potentially a good clinical outcome. To date, the experience with RSA is limited.
Methods
In this retrospective analysis, interventional and clinical data of patients with acute intracranial LAO of the anterior and posterior circulation who underwent RSA after SRT due to an underlying lesion between 2012–2017 in four neurovascular centers were studied.
Results
In this study 34 patients (mean age 67 years) were included whereby 18 patients had anterior circulation LAO and 16 patients posterior circulation LAO. The SRT maneuver count ranged between 1 and 15 (median 2). Indications for RSA were an immediate re-occlusion in 25 (74%), and a persistent high-grade stenosis in 9 patients (26%). The RSA was technically feasible in 33 patients (97%). A mTICI 2b/3 result was obtained in 26 patients (76%). Median onset-to-recanalization time was 248 min (range 80–650 min). After 3 months 10/34 patients (29%) had a good clinical outcome (modified Rankin Scale, mRS 0–2). In detail, 4/18 patients (22%) with anterior circulation LAO and 6/16 patients (38%) with posterior circulation LAO were functionally independent.
Conclusion
The use of RSA can be considered for acute intracranial LAO in cases with immediate re-occlusion or high-grade stenosis after SRT alone.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Stent-retriever thrombectomy (SRT) is now recommended as the standard treatment for patients with acute stroke due to intracranial large artery occlusion (LAO). Since 2015, several randomized multicenter trials proved the superiority of SRT compared to best medical treatment [1,2,3,4,5,6,7,8,9]. These studies showed high recanalization success, with a modified Thrombolysis in Cerebral Infarction (mTICI) grade 2b or 3 [10] in up to 88% [3]. Furthermore, according to a meta-analysis of five studies, the rate of functional independence, defined as modified Rankin Scale (mRS) of 0–2, was significantly higher in the endovascular group when compared to the controls (46% versus 26.5%, p < 0.0001; [1]). Results of randomized studies dealing with acute posterior circulation LAO are not yet available; however, SRT was technically and clinically effective in non-randomized trials, with a mTICI 2b/3 result in more than 70% and a good clinical outcome (mRS 0–2) in 28–50% [11,12,13,14]. Despite the initially successful recanalization, immediate re-occlusion or residual high-grade stenosis may require further endovascular treatment in some patients [14,15,16,17,18]. The most common pathology for an immediate re-occlusion, especially in the posterior circulation, is an underlying atherosclerotic lesion [15, 16], which is much more frequent in Asian populations [16, 19, 20]. As balloon angioplasty alone is associated with high re-occlusion rates [15, 16], rescue stent angioplasty (RSA) may be the only option in order to achieve a permanent recanalization and further functional independence; however, the literature data on this topic are scarce and particularly focused on the posterior circulation [14,15,16,17,18]. Behme et al. [15] published a series of seven patients with an acute basilar artery (BA) occlusion due to an underlying atherosclerotic lesion; RSA with or without prior SRT was technically effective in all patients (mTICI 2b/3: 100%) and three patients were functionally independent after 3 months (43%). To date, only one small single center survey has compared RSA (n = 17) and non-RSA groups (n = 28) after failed SRT in acute anterior circulation LAO [21].
This article presents a retrospective multicenter study and report on our experience with RSA in patients with acute intracranial anterior and posterior circulation LAO and immediate re-occlusion after initially successful SRT.
Methods
In a retrospective analysis, all patients with acute intracranial LAO of the anterior and posterior circulation, who underwent RSA between November 2012 and August 2017, were identified from the stroke databases of four tertiary stroke centers. In all centers, a total of 1617 intracranial thrombectomies were conducted in this time period.
Inclusion criteria were:
-
National Institute of Health Stroke scale (NIHSS) of at least 4 on admission
-
Evidence of intracranial LAO and absence of intracranial hemorrhage
-
Time interval between onset of acute symptoms and groin puncture of less than 8 h in intracranial anterior circulation LAO patients and less than 12 h in intracranial posterior circulation LAO patients
-
Immediate re-occlusion or remaining high-grade stenosis after SRT due to an underlying (non-embolic) vessel pathology
The anonymized patient data were prospectively entered in the databases of the participating centers. The retrospective analysis focused on interventional data, the technical efficacy of RSA, and the clinical outcome.
Baseline Characteristics
In each patient, the responsible neurologist of the respective emergency unit and/or referring hospital diagnosed acute major stroke symptoms. The first-line imaging protocol consisted of a non-enhanced cranial computed tomography (CT) and a CT angiography of the supra-aortic arteries.
Intracranial anterior circulation LAO was defined as occlusion of:
-
the intracranial segment(s) of the internal carotid artery including the carotid T
-
the first segment of the middle cerebral artery (M1)
-
the second segment of the middle cerebral artery (M2)
Intracranial posterior circulation LAO was defined as occlusion of:
-
the basilar artery (BA)
-
the intracranial segment of the vertebral artery
The treating neurologist and neurointerventionist and the patient and/or the relatives decided in consensus for endovascular revascularization in each case. If available, the time intervals between onset of acute symptoms and groin puncture as well as final endovascular revascularization were documented. Patients received weight-adapted intravenous recombinant tissue plasminogen activator (rt-PA) prior to groin puncture, if the duration of acute symptoms of intracranial LAO did not exceed 4.5 h, and contraindications (e.g. prior surgery, metastatic tumor disease, and/or pre-existing anticoagulation/antiplatelet therapy) were absent.
Interventional and Clinical Data Analysis
Technical data including stent-retriever model, number of SRT maneuvers, individual indications for RSA, the presumed underlying vessel pathology, as well as the stent design (balloon or self-expanding) and the additional use of balloon angioplasty were evaluated. After SRT, a persistent vessel stenosis of at least 70% in diameter was defined as high-grade. A successful recanalization result was defined as mTICI 2b or 3 on the final angiogram [1, 10]. Complications including residual periprocedural stenosis, postinterventional stent occlusion and in-stent restenosis, and symptomatic intracranial hemorrhage (sICH) according to the European Cooperative Acute Stroke Study (ECASS) III criteria [22] were documented. Stent patency was usually assessed by transcranial ultrasound after 24 h and also after 3 months. In-stent restenosis was diagnosed according to the criteria of Rasulo et al. [23]:
-
Acceleration of flow velocity through the stenosis
-
Deceleration of flow velocity distal from the stenosis
-
Lateral difference of mean flow velocity
-
Disturbances in flow
The NIHSS at admission and discharge as well as the final mRS after 90 days were assessed. A NIHSS improvement of more than three points was defined as “substantial”, and a final mRS score 0–2 as “good clinical outcome”.
Endovascular Revascularization
The use of a balloon guide catheter, the choice of the respective primary clot-retrieving device, and the indication for RSA were at the neurointerventionist’s discretion in each participating center. The endovascular approach to the vessel occlusion usually consisted of a fluoroscopic, guidewire-assisted triaxial access in the sense of a 6 or 8 French guiding catheter, an intermediate or aspiration catheter, and a microcatheter. No intermediate catheter was applied when a balloon guide catheter was used. The SRT maneuvers were carried out in a standardized manner, as described by Dorn et al. [24]. In the case of an immediate re-occlusion or a persistent high-grade stenosis, the SRT maneuver was repeated and/or the neurointerventionist decided for RSA. Considering self-expanding stents, a microcatheter was placed at the anatomic site using a micro-guidewire; then the micro-guidewire was removed, and an appropriate stent was inserted and deployed while withdrawing the microcatheter. Prior to RSA, if necessary, percutaneous transluminal balloon angioplasty was performed. Regarding balloon-expanding stents, the lesion was crossed with the system and the stent was deployed by balloon inflation according to the manufacturers’ instruction using a pressure gauge.
Antithrombotic Therapy
During the intervention, heparinized saline flushes were used by default. Prior to RSA, the neurointerventionist administered either:
-
a glycoprotein IIb/IIIa inhibitor (tirofiban/Aggrastat®): as recommended by the manufacturer starting with a weight-adapted intravenous loading dose of 0.4 µg/kg/min for 30 min, followed by a maintenance dose of 0.1 µg/kg/min intravenous for at least 12 h. Overlapping, dual antiplatelet therapy with 100 mg acetylsalicylic acid (ASA) and 300 mg clopidogrel was started either orally or via the gastric tube 4 h prior to infusion stop.
-
or 500 mg ASA intravenously, followed by clopidogrel (loading dose 300 mg) via the gastric tube
-
or no additional medicinal therapy (in the case of pre-existing dual antiplatelet treatment).
If the routine control computed tomography (CT) within the following day showed major sICH, the antiplatelet therapy was stopped. Otherwise, it was continued orally with ASA 100 mg/day life long and clopidogrel 75 mg/day for at least 6 months.
Results
A total of 34 patients were included in the analysis. Mean age was 67 years and 11 patients (32%) were female. Table 1 summarizes the patients’ baseline characteristics, interventional data, and clinical outcome.
Baseline Characteristics
The mean NIHSS at admission was 13 (range 4–26). The LAO was located in the anterior circulation in 18/34 (53%) and in the posterior circulation in 16/34 patients (47%). The most common occlusion sites were the BA in 12 patients (35%), and the M1 segment of the middle cerebral artery (MCA) in 11 patients (32%). The median time between onset of symptoms and final recanalization was 248 min (range 80–650 min) and the time between groin puncture and final recanalization ranged between 20 and 300 min (median 65 min). Intravenous rt-PA prior to the recanalization procedure was administered in 11/34 patients (32%).
Interventional Data
Concerning SRT, the most commonly utilized clot-retrieving devices were the Solitaire® FR Stent (22 of 34 patients, 65%), and the Trevo® ProVue Stent (Stryker, Kalamazoo, MI, USA; 9 patients, 26%). Of the patients four underwent SRT with two different stent-retrievers (Solitaire® FR and Trevo® ProVue, each). The SRT maneuver count ranged between 1 and 15, with a median of 2, 21/34 patients received 1 or 2 SRT maneuvers and 13/34 patients 3 or more SRT maneuvers. The indications for RSA were an immediate re-occlusion after SRT at the anatomic site in 25 patients (74%), and a persistent high-grade stenosis in 9 patients (26%). Based on the angiographic morphology, the most common underlying vessel pathology was a presumed atherosclerotic lesion (28 patients, 82%), followed by presumed vessel dissection in 4 patients (12%), and presumed vasculitis in 2 patients (6%). Prior to RSA, balloon angioplasty was carried out in 28/34 patients. In 33 out of 34 patients (97%) a self-expanding permanent stent was implanted, and in 1 patient a balloon-expanding stent. The Enterprise® Stent (Codman Neuro, Raynham, MA, USA) was used in 15/34 (44%), the Solitaire® AB Stent (ev3/Medtronic, Irvine, CA, USA) in 7/34 (21%), the Wingspan® Stent (Stryker) in 6/34 (18%), the Acclino® Stent (Acandis, Pforzheim, Germany) in 6/34 (18%), the Leo® Stent (Balt, Montmorency, France) in 1/34 (3%), and the Coroflex® Blue Ultra Stent (B. Braun, Berlin, Germany) in 1/34 patients (3%). Of the patients three were treated with two permanent stents (Enterprise® + Solitaire®AB, n = 2; Enterprise® + Leo®, n = 1). Delivery and placement of the stent across the target lesion was technically successful in 33/34 patients (97%). It was technically not feasible to advance the permanent stent towards the vessel occlusion in one patient, hence balloon angioplasty alone was performed; however, this maneuver did not result in permanent vessel patency (patient 33). The final DSA run confirmed successful revascularization (mTICI 2b/3) in 26 out of 34 patients (76%). In detail, a good revascularization result was obtained in 67% of anterior and 88% of posterior circulation patients. The first-line antiplatelet therapy consisted of a glycoprotein IIb/IIIa inhibitor in 20 patients (59%), and a combination of ASA and clopidogrel in 13 patients (38%).
Complications and Clinical Outcome
In the acute post-interventional phase, 4 out of 34 patients (12%) experienced sICH of which 3 had initially received intravenous rt-PA (patients 1, 4 and 15), in combination with a glycoprotein IIb/IIIa inhibitor in 2 patients (patients 1 and 15) and 6 of the 34 patients (18%) had a post-interventional stent occlusion within 24 h. Asymptomatic in-stent restenosis occurred in another 3 patients during the 3‑month follow-up period (9%) and 2 of these patients showed a restenosis of more than 50% after 3 months and therefore received balloon angioplasty in a second intervention (patients 16 and 28). Overall, six out of nine patients with stent occlusion and restenosis had initially received ASA and clopidogrel (67%), and information on antiplatelet function testing was not available. The mean NIHSS at discharge was 10 (range, 0–27). Compared to the neurological status at admission, the NIHSS improved substantially in 16 out of 34 patients (47%). After 3 months, 10 of the 34 patients (29%) had a good clinical outcome (mRS 0–2). In detail, the functional independence rate was 22% in anterior circulation LAO (4/18 patients), and 38% in posterior circulation LAO (6/16 patients). In six patients, the neurological deficits had completely resolved (18%; patients 7, 13, 16, 26, 32 and 34). The mortality was 21% (7 out of 34 patients).
Illustrative Case 1
A 49-year-old male presented with a mild right-sided hemiparesis (patient 5, Fig. 1). Initial magnetic resonance imaging (MRI) showed circumscribed subacute ischemia in the internal capsule/putamen on the left (Fig. 1a: diffusion-weighted imaging (DWI), transversal; Fig. 1b: fluid attenuated inversion recovery (FLAIR), transversal), and a high-grade atherosclerotic stenosis of the ipsilateral M1-segment (* in Fig. 1c and d; Fig. 1c: 3D reformatted arterial time-of-flight (TOF) angiography). Dual antiplatelet therapy (ASA and clopidogrel) was initiated and 5 days later, the patient experienced acute neurological deterioration (NIHSS 21). Digital subtraction angiography (DSA) now depicted a complete postbifurcation MCA occlusion (arrow in Fig. 1d: posterior-anterior (PA) projection) distal from the pre-existing high-grade M1 stenosis. After a total of seven SRT maneuvers revascularization was achieved, but both the high-grade stenosis and thrombotic material in the M1- and M2-segment persisted (arrows in Fig. 1e: PA). Hence, RSA was performed (Enterprise®) after prior balloon dilatation, resulting in a complete revascularization with a normalized vessel diameter (Fig. 1f: PA). The neurological symptoms did not resolve substantially (NIHSS 19 at discharge, mRS 3 after 90 days).
A 49‑year-old male with mild right-sided hemiparesis. a Diffusion-weighted imaging, transverse section and b fluid attenuated inversion recovery, transverse section showing circumscribed subacute ischemia in the internal capsule/putamen on the left. c, d 3D reformatted arterial time-of-flight angiography showing high-grade atherosclerotic stenosis of the ipsilateral M1-segment (*). d After treatment digital subtraction angiography now depicted a complete postbifurcation middle cerebal artery occlusion (arrow) in posterior-anterior projection distal from the preexisting high-grade M1 stenosis. e After revascularization both the high-grade stenosis and thrombotic material in the M1 and M2 segment persisted (arrows). f Rescue stent angioplasty was performed resulting in a complete revascularization with a normalized vessel diameter
Illustrative Case 2
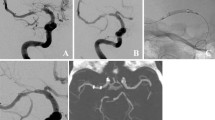
A 54-year-old male with dizziness lasting for days and now an acute onset of impaired consciousness, central oculomotor dysfunction, dysarthria and gait disturbance 1.5 h prior to admission (patient 26, Fig. 2). Initial CT revealed signs of subacute cerebellar infarctions on the left (Fig. 2a: transversal), thus IV administration of t‑PA was contraindicated. CT angiography was suggestive for chronic occlusion of the right vertebral artery and an acute occlusion of the intracranial vertebral segment on the left with extension to the BA (not shown), which was verified by DSA (Fig. 2b: PA; Fig. 2c: lateral view). After one SRT maneuver both the left vertebral artery and BA were revascularized, but an underlying atherosclerotic stenosis with progressive thrombus apposition (white arrows in Fig. 2d–f; Fig. 2d: PA, Fig. 2e and f: lateral view) was seen despite IV administration of tirofiban. Thus, balloon angioplasty and RSA (Solitaire® AB; ev3/Medtronic) was performed. Final DSA run showed full recanalization with slight residual irregularities of the vessel wall, but no relevant stenosis (black arrows in Fig. 2g: lateral view). The post-interventional MRI on day 8 revealed only small embolic ischemia in the left cerebellar hemisphere (Fig. 2h: DWI, transversal) and the neurological deficits resolved completely (mRS after 90 days = 0).
A 54‑year-old male with dizziness and acute onset of impaired consciousness. Initial computed tomography revealed signs of subacute cerebellar infarctions on the left (a transverse section). Chronic occlusion of the right vertebral artery and acute occlusion of the intracranial vertebral segment on the left was verified by digital subtraction angiography (b posterior-anterior projection, c lateral view). d–f After stent-retriever thrombectomy both the left vertebral artery and basilar artery were revascularized but an underlying atherosclerotic stenosis with progressive thrombus apposition persisted (white arrows, d posterior-anterior projection, e, f lateral view). Final digital subtraction angiogaphy (g) showed full recanalization with slight residual irregularities of the vessel wall, but no relevant stenosis (black arrows, lateral view). h Post-interventional magnetic resonance imaging on day 8 revealed only small embolic ischemia in the left cerebellar hemisphere (diffusion weighted imaging, transverse section)
Discussion
Endovascular recanalization of acute intracranial LAO was demonstrated to be effective with a high level of evidence in recent years; however, in some patients SRT alone does not result in permanent revascularization, e.g. due to an underlying lesion such as an atherosclerotic stenosis, dissection or vasculitis. In general, intracranial atherosclerotic stenosis is far more frequently located in the posterior circulation [14, 25,26,27]. Currently, data on RSA following SRT are scarce, in particular in anterior circulation LAO.
The majority of the patients in our study showed an immediate re-occlusion after primarily successful SRT (74%). It has been suggested that in patients with underlying vessel pathology, the SRT maneuver itself may actually aggravate a pre-existing local endothelial vulnerability, in the sense of further plaque instability and rupture, local thrombosis, and finally result in re-occlusion [16]; however, similar to others [14, 16, 26], we did not encounter major SRT-related complications such as arterial perforation or tearing of perforators during the SRT maneuver across the underlying lesion. The use of SRT and/or balloon angioplasty is normally not sufficient in patients with an underlying stenosis, because these procedures do not heal, but deteriorate the underlying pathology [28]. So far, RSA may therefore be the only available technique that potentially prevents re-occlusion; here, the stent covers the vulnerable vessel segment and stops the pathological cascade as described above [15, 16].
Stent angioplasty of symptomatic intracranial stenosis has been debated for several years now, particularly due to the results of the Stenting vs Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis (SAMMPRIS) trial, where the 30-day risk of recurrent stroke or death was significantly higher in the stent angioplasty than in the best medical treatment group (14.7% versus 5.8%; [29]); however, the patients’ clinical and vascular baseline data in the SAMMPRIS trial were different from those of the present study: whereas the SAMMPRIS patients had transient ischemic attacks or minor strokes due to an intracranial stenosis, the patients in our survey suffered from acute major stroke caused by a complete occlusion of an intracranial large artery. Although SRT initially resulted in reperfusion, it was not efficient due to immediate re-occlusion or remaining high-grade vessel stenosis; hence the prognosis was poor and RSA was considered as a brain or life-saving therapy [16, 21].
In our study, the technical success was high and a good revascularization result (mTICI 2b/3) was achieved in more than 75% of patients. These data confirm observations by other RSA study groups [14, 21, 25, 26]. Of the patients without stent occlusion 37% were functionally independent after 3 months. This is a higher rate than in the intervention group in the MR CLEAN study [4]; however, none of the patients had a favorable clinical outcome when stent occlusions occurred. These data are comparable to other studies: Baek et al. who analyzed 45 patients with acute anterior circulation LAO in whom SRT alone failed, reported a good clinical outcome for 35% in the RSA group (17 patients) versus 7% in the non-stent angioplasty group [21]. Concerning RSA in acute posterior circulation LAO, in the study of Möhlenbruch et al. 33% of patients were functionally independent after 3 months [25]. These data support the hypothesis that patients in whom the standard therapy is expedient may clinically benefit from RSA, given permanent stent patency. Early stent occlusion was one of the major complications in our series: nearly one third of our patients had either an early occlusion of the stent or an in-stent restenosis. As stent occlusion was not correlated with a certain stent type, we believe that stent patency rather depends on adequate inhibition of platelet aggregation. Of the patients with early stent occlusion or severe restenosis two thirds had received ASA and clopidogrel periprocedurally or postprocedurally, which may be not sufficient in the acute setting. Due to general anesthesia, clopidogrel was administered via the gastric tube, possibly resulting in delayed intestinal resorption and insufficient antiplatelet effect. We cannot prove that a more potential first-line medicinal treatment with a glycoprotein IIb/IIIa inhibitor would have resulted in stent patency in these patients; however, recently published data by Woo et al. support this assumption [18]. Antithrombotic therapy in acute stroke patients is a balancing act due to the potential risk of sICH, especially if intravenous rt-PA was given prior to the procedure [30], and to date no consistent recommendations for antiplatelet medication in the acute stroke phase are available [9]. The rate of sICH was low in our study group (12%). Out of four patients with sICH, three received intravenous rt-PA, two patients additionally a glycoprotein IIb/IIIa inhibitor. These data are comparable to the RSA series of Baek et al. (sICH rate 12%), but slightly higher than those of the large randomized anterior circulation LAO thrombectomy trials, which reported sICH rates of less than 10% in patients after thrombectomy alone [1]. In the present study, the clinical outcome was better in posterior than in anterior circulation LAO patients. This is most probably the result of both a higher recanalization success and a lower rate of postinterventional stent occlusions in the former group. In addition, there was a higher rate of underlying lesions other than atherosclerotic stenosis (presumed dissection or vasculitis) in the patients with anterior circulation LAO. Vasculitis was presumed in these patients based on the angiographic pattern and the conspicuous cerebrospinal fluid findings; however, the diagnosis was not confirmed by biopsy. In four patients pre-existing dissection was suspected based on the angiographic pattern and a highly difficult catheterization of the lumen. In general, the precise angiographic classification of the underlying lesion (atherosclerosis, dissection, vasculitis) is difficult in most cases. Particularly, the differentiation between atherosclerotic stenosis and residual/resistant thrombus is not always possible, but it may substantially affect the risk of stent occlusion or restenosis.
Patients undergoing only one or two SRT maneuvers had more commonly a favorable clinical outcome when compared to those patients receiving more than two SRT maneuvers. One explanation may be the shorter recanalization time in the former group, as supported by Dorn et al., who found that an increase of the SRT maneuver count may unnecessarily prolong the intervention and lead to a deterioration of the clinical outcome [31]. Furthermore, our results indicate that patients with onset recanalization times of less than 300 min might have a better clinical outcome after 3 months than those with longer time intervals; however, these data have to be interpreted with caution due to missing statistical significance. Furthermore, it is known that selected patients with prolonged symptoms potentially benefit from mechanical revascularization, as well [1, 32, 33].
There are several study limitations: (i) due to the retrospective study design, the following data were not available: pre-hospital mRS, comorbidities, laboratory data, ASPECT score at admission and (ii) the study population is relatively small and heterogeneous; therefore, a profound statistical analysis was not possible.
Conclusion
So far, RSA is the only chance to permanently restore blood flow in patients with underlying vessel pathology and an immediate re-occlusion or high-grade stenosis after initially successful SRT. The RSA is technically feasible, provides good recanalization results, and may be the only chance for a certain patient group to potentially achieve functional independence. Our data suggest that a quick decision for RSA, instead of numerous SRT maneuvers, may save valuable time and increase the likelihood of good clinical outcome. More data focusing on the efficacy of periprocedural antiplatelet therapy is necessary.
References
Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, Dávalos A, Majoie CB, van der Lugt A, de Miquel MA, Donnan GA, Roos YB, Bonafe A, Jahan R, Diener HC, van den Berg LA, Levy EI, Berkhemer OA, Pereira VM, Rempel J, Millán M, Davis SM, Roy D, Thornton J, Román LS, Ribó M, Beumer D, Stouch B, Brown S, Campbell BC, van Oostenbrugge RJ, Saver JL, Hill MD, Jovin TG, HERMES Collaborators. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723–31.
Wahlgren N, Moreira T, Michel P, Steiner T, Jansen O, Cognard C, Mattle HP, van Zwam W, Holmin S, Tatlisumak T, Petersson J, Caso V, Hacke W, Mazighi M, Arnold M, Fischer U, Szikora I, Pierot L, Fiehler J, Gralla J, Fazekas F, Lees KR, ESO-KSU, ESO, ESMINT, ESNR, EAN. Mechanical thrombectomy in acute ischemic stroke: consensus statement by ESO-Karolinska stroke update 2014/2015, supported by ESO, ESMINT, ESNR and EAN. Int J Stroke. 2016;11:134–47.
Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, Albers GW, Cognard C, Cohen DJ, Hacke W, Jansen O, Jovin TG, Mattle HP, Nogueira RG, Siddiqui AH, Yavagal DR, Baxter BW, Devlin TG, Lopes DK, Reddy VK, du Mesnil de Rochemont R, Singer OC, Jahan R, SWIFT PRIME Investigators. Stent-retriever thrombectomy after intravenous t‑PA vs. t‑PA alone in stroke. N Engl J Med. 2015;372:2285–95.
Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, Schonewille WJ, Vos JA, Nederkoorn PJ, Wermer MJ, van Walderveen MA, Staals J, Hofmeijer J, van Oostayen JA, Lycklama à Nijeholt GJ, Boiten J, Brouwer PA, Emmer BJ, de Bruijn SF, van Dijk LC, Kappelle LJ, Lo RH, van Dijk EJ, de Vries J, de Kort PL, van Rooij WJ, van den Berg JS, van Hasselt BA, Aerden LA, Dallinga RJ, Visser MC, Bot JC, Vroomen PC, Eshghi O, Schreuder TH, Heijboer RJ, Keizer K, Tielbeek AV, den Hertog HM, Gerrits DG, van den Berg-Vos RM, Karas GB, Steyerberg EW, Flach HZ, Marquering HA, Sprengers ME, Jenniskens SF, Beenen LF, van den Berg R, Koudstaal PJ, van Zwam WH, Roos YB, van der Lugt A, van Oostenbrugge RJ, Majoie CB, Dippel DW, MR CLEAN Investigators. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372:11–20.
Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, Roy D, Jovin TG, Willinsky RA, Sapkota BL, Dowlatshahi D, Frei DF, Kamal NR, Montanera WJ, Poppe AY, Ryckborst KJ, Silver FL, Shuaib A, Tampieri D, Williams D, Bang OY, Baxter BW, Burns PA, Choe H, Heo JH, Holmstedt CA, Jankowitz B, Kelly M, Linares G, Mandzia JL, Shankar J, Sohn SI, Swartz RH, Barber PA, Coutts SB, Smith EE, Morrish WF, Weill A, Subramaniam S, Mitha AP, Wong JH, Lowerison MW, Sajobi TT, Hill MD, ESCAPE Trial Investigators. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372:1019–30.
Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, Yan B, Dowling RJ, Parsons MW, Oxley TJ, Wu TY, Brooks M, Simpson MA, Miteff F, Levi CR, Krause M, Harrington TJ, Faulder KC, Steinfort BS, Priglinger M, Ang T, Scroop R, Barber PA, McGuinness B, Wijeratne T, Phan TG, Chong W, Chandra RV, Bladin CF, Badve M, Rice H, de Villiers L, Ma H, Desmond PM, Donnan GA, Davis SM, EXTEND-IA Investigators. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372:1009–18.
Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, San Román L, Serena J, Abilleira S, Ribó M, Millán M, Urra X, Cardona P, López-Cancio E, Tomasello A, Castaño C, Blasco J, Aja L, Dorado L, Quesada H, Rubiera M, Hernandez-Pérez M, Goyal M, Demchuk AM, von Kummer R, Gallofré M, Dávalos A, REVASCAT Trial Investigators. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372:2296–306.
Bracard S, Ducrocq X, Mas JL, Soudant M, Oppenheim C, Moulin T, Guillemin F, THRACE investigators. Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol. 2016;15:1138–47.
Fiehler J, Cognard C, Gallitelli M, Jansen O, Kobayashi A, Mattle HP, Muir KW, Mazighi M, Schaller K, Schellinger PD. European recommendations on organisation of interventional care in acute stroke (EROICAS). Int J Stroke. 2016;11:701–16.
Zaidat OO, Yoo AJ, Khatri P, Tomsick TA, von Kummer R, Saver JL, Marks MP, Prabhakaran S, Kallmes DF, Fitzsimmons BM, Mocco J, Wardlaw JM, Barnwell SL, Jovin TG, Linfante I, Siddiqui AH, Alexander MJ, Hirsch JA, Wintermark M, Albers G, Woo HH, Heck DV, Lev M, Aviv R, Hacke W, Warach S, Broderick J, Derdeyn CP, Furlan A, Nogueira RG, Yavagal DR, Goyal M, Demchuk AM, Bendszus M, Liebeskind DS, Cerebral Angiographic Revascularization Grading (CARG), STIR Revascularization working group, STIR Thrombolysis in Cerebral Infarction (TICI) Task Force. Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke. 2013;44:2650–63.
Roth C, Papanagiotou P, Behnke S, Walter S, Haass A, Becker C, Fassbender K, Politi M, Körner H, Romann MS, Reith W. Stent-assisted mechanical recanalization for treatment of acute intracerebral artery occlusions. Stroke. 2010;41:2559–67.
Costalat V, Machi P, Lobotesis K, Maldonado I, Vendrell JF, Riquelme C, Mourand I, Milhaud D, Héroum C, Perrigault PF, Arquizan C, Bonafé A. Rescue, combined, and stand-alone thrombectomy in the management of large vessel occlusion stroke using the solitaire device: a prospective 50-patient single-center study: timing, safety, and efficacy. Stroke. 2011;42:1929–35.
Mourand I, Machi P, Milhaud D, Picot MC, Lobotesis K, Arquizan C, Costalat V, Héroum C, Sablot D, Bouly S, Lalu T, Bonafé A. Mechanical thrombectomy with the Solitaire device in acute basilar artery occlusion. J Neurointerv Surg. 2014;6:200–4.
Mordasini P, Brekenfeld C, Byrne JV, Fischer U, Arnold M, Heldner MR, Lüdi R, Mattle HP, Schroth G, Gralla J. Technical feasibility and application of mechanical thrombectomy with the Solitaire FR Revascularization Device in acute basilar artery occlusion. AJNR Am J Neuroradiol. 2013;34:159–63.
Behme D, Weber W, Mpotsaris A. Acute basilar artery occlusion with underlying high-grade basilar artery stenosis: multimodal endovascular therapy in a series of seven patients. Clin Neuroradiol. 2015;25:267–74.
Gao F, Lo WT, Sun X, Mo DP, Ma N, Miao ZR. Combined use of mechanical thrombectomy with angioplasty and stenting for acute basilar occlusions with underlying severe intracranial vertebrobasilar stenosis: preliminary experience from a single Chinese center. AJNR Am J Neuroradiol. 2015;36:1947–52.
Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG, Clark W, Budzik R, Zaidat OO, SWIFT Trialists. Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet. 2012;380:1241–9.
Woo HG, Sunwoo L, Jung C, Kim BJ, Han MK, Bae HJ, Bae YJ, Choi BS, Kim JH. Feasibility of permanent stenting with solitaire as a rescue treatment for the reperfusion of acute Intracranial artery occlusion. AJNR Am J Neuroradiol. 2018;39:331–6.
Wong LK. Global burden of intracranial atherosclerosis. Int J Stroke. 2006;1:158–9.
Mattle HP, Arnold M, Lindsberg PJ, Schonewille WJ, Schroth G. Basilar artery occlusion. Lancet Neurol. 2011;10:1002–14.
Baek JH, Kim BM, Kim DJ, Heo JH, Nam HS, Yoo J. Stenting as a rescue treatment after failure of mechanical thrombectomy for anterior circulation large artery occlusion. Stroke. 2016;47:2360–3.
Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, Larrue V, Lees KR, Medeghri Z, Machnig T, Schneider D, von Kummer R, Wahlgren N, Toni D, ECASS Investigators. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317–29.
Rasulo FA, De Peri E, Lavinio A. Transcranial Doppler ultrasonography in intensive care. Eur J Anaesthesiol Suppl. 2008;42:167–73.
Dorn F, Lockau H, Stetefeld H, Kabbasch C, Kraus B, Dohmen C, Henning T, Mpotsaris A, Liebig T. Thrombectomy of M2-occlusion. J Stroke Cerebrovasc Dis. 2015;24:1465–70.
Möhlenbruch M, Stampfl S, Behrens L, Herweh C, Rohde S, Bendszus M, Hametner C, Nagel S, Ringleb PA, Pham M. Mechanical thrombectomy with stent retrievers in acute basilar artery occlusion. AJNR Am J Neuroradiol. 2014;35:959–64.
Espinosa de Rueda M, Parrilla G, Zamarro J, García-Villalba B, Hernández F, Moreno A. Treatment of acute vertebrobasilar occlusion using thrombectomy with stent retrievers: initial experience with 18 patients. AJNR Am J Neuroradiol. 2013;34:1044–8.
Andersson T, Kuntze Söderqvist Å, Söderman M, Holmin S, Wahlgren N, Kaijser M. Mechanical thrombectomy as the primary treatment for acute basilar artery occlusion: experience from 5 years of practice. J Neurointerv Surg. 2013;5:221–5.
Park JH, Park SK, Jang KS, Jang DK, Han YM. Critical use of balloon angioplasty after recanalization failure with retrievable stent in acute cerebral artery occlusion. J Korean Neurosurg Soc. 2013;53:77–82.
Chimowitz MI, Lynn MJ, Derdeyn CP, Turan TN, Fiorella D, Lane BF, Janis LS, Lutsep HL, Barnwell SL, Waters MF, Hoh BL, Hourihane JM, Levy EI, Alexandrov AV, Harrigan MR, Chiu D, Klucznik RP, Clark JM, McDougall CG, Johnson MD, Pride GL Jr, Torbey MT, Zaidat OO, Rumboldt Z, Cloft HJ, SAMMPRIS Trial Investigators. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011;365:993–1003.
Kellert L, Hametner C, Rohde S, Bendszus M, Hacke W, Ringleb P, Stampfl S. Endovascular stroke therapy: tirofiban is associated with risk of fatal intracerebral hemorrhage and poor outcome. Stroke. 2013;44:1453–5.
Dorn F, Stehle S, Lockau H, Zimmer C, Liebig T. Endovascular treatment of acute intracerebral artery occlussions with the solitaire stent: single-centre experience with 108 recanalization procedures. Cerebrovasc Dis. 2012;34:70–7.
Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, Yavagal DR, Ribo M, Cognard C, Hanel RA, Sila CA, Hassan AE, Millan M, Levy EI, Mitchell P, Chen M, English JD, Shah QA, Silver FL, Pereira VM, Mehta BP, Baxter BW, Abraham MG, Cardona P, Veznedaroglu E, Hellinger FR, Feng L, Kirmani JF, Lopes DK, Jankowitz BT, Frankel MR, Costalat V, Vora NA, Yoo AJ, Malik AM, Furlan AJ, Rubiera M, Aghaebrahim A, Olivot JM, Tekle WG, Shields R, Graves T, Lewis RJ, Smith WS, Liebeskind DS, Saver JL, Jovin TG, DAWN Trial Investigators. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018;378:11–21.
Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, McTaggart RA, Torbey MT, Kim-Tenser M, Leslie-Mazwi T, Sarraj A, Kasner SE, Ansari SA, Yeatts SD, Hamilton S, Mlynash M, Heit JJ, Zaharchuk G, Kim S, Carrozzella J, Palesch YY, Demchuk AM, Bammer R, Lavori PW, Broderick JP, Lansberg MG, DEFUSE 3 Investigators. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378:708–18.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
R. Forbrig, H. Lockau, F. Flottmann, T. Boeckh-Behrens, C. Kabbasch, M. Patzig, A. Mpotsaris, J. Fiehler, T. Liebig, G. Thomalla, O.A. Onur, S. Wunderlich, K. Kreiser, M. Herzberg, F.A. Wollenweber, S. Prothmann and F. Dorn declare that they have no competing interests.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. We declare that all patients and/or their relatives gave informed consent prior to inclusion in this study.
Additional information
Robert Forbrig and Hannah Lockau as well as Sascha Prothmann and Franziska Dorn contributed equally to the manuscript.
Part of the data was presented at the 51st annual meeting of the German Society of Neuroradiology in Cologne, Germany (October 2016).
Rights and permissions
About this article
Cite this article
Forbrig, R., Lockau, H., Flottmann, F. et al. Intracranial Rescue Stent Angioplasty After Stent-Retriever Thrombectomy. Clin Neuroradiol 29, 445–457 (2019). https://doi.org/10.1007/s00062-018-0690-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-018-0690-4