Abstract
Background and Purpose
Nerve root compression by lumbar disc herniation (LDH) induces a series of clinical symptoms, seriously affecting the patient’s life and work. The purpose of this study is to investigate microstructural changes and fiber bundle abnormalities of the compressed L5 and S1 nerve roots in young patients with unilateral LDH by using diffusion tensor imaging (DTI).
Methods
Forty young patients with unilateral LDH and 17 healthy volunteers participated in the study, and 33 patients received follow-up DTI examination after one month of conservative treatment. Fractional anisotropy (FA), apparent diffusion coefficient (ADC) and trace weight (TraceW) values of the L5 and S1 nerve roots were measured on FA maps.
Results
The mean FA, ADC and TraceW values of the affected nerve roots were 0.259 ± 0.047, 1.79 ± 0.252 and 0.076 ± 0.025, respectively. Compared to the contralateral side and volunteers, the affected nerve roots showed a decreased FA (P < 0.01), an increased ADC (P < 0.01) and TraceW (P < 0.05). The compression severity had a moderately negative correlation with FA (r = −0.646, P < 0.01) and positive correlation with ADC (r = 0.408, P < 0.01) but not with TraceW (r = 0.298, P = 0.06). For 33 patients with follow-up study after conservative treatment, FA (0.286 ± 0.06) and ADC (1.630 ± 0.046) in the affected nerve roots showed an increasing and a decreasing trend, respectively. Moreover, FA values (14 cases; 0.246 ± 0.015, P = 0.213) in the severe compression group had no significant changes between initial and follow-up data.
Conclusions
DTI is able to assess microstructural abnormalities of the compressed nerve roots and has potentially practical value for prognostic evaluation after treatment in patients with LDH.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lumbar disc herniation (LDH) is a common and frequently occurring disease which often causes sciatica and radicular symptoms affecting the patient’s quality of life [1, 2]. Given the influence of several factors, such as anatomy and exercise load, the best predilection site for LDH is the L5/S1 intervertebral disc followed by the L4/L5 intervertebral disc (about 90–95% of all LDH) [3, 4]. Traditionally, the diagnosis of LDH often relies on conventional computed tomography (CT) and magnetic resonance imaging (MRI). At present, conventional MRI technology encounters difficulty in the quantitative evaluation of the microstructural changes of nerve tissues and fiber tractography, although magnetic resonance neurography (MRN) can provide certain valuable morphological information [5,6,7]. Moreover, nonconformity between clinical symptoms and MRI findings occurs occasionally in patients with LDH [8].
Diffusion tensor imaging (DTI), which is based on a tensor model to characterize random microscopic motion of water molecules in tissues, has been widely applied in the evaluation of the central nervous system diseases, such as acute brain stroke, diffuse axonal injury and glioma preoperative navigation [9,10,11]. Diffusion tensor tractography (DTT) can clearly display the course of nerve fibers and provide vivid anatomical information and probable location of nerve damage as a novel and noninvasive technique [12, 13]. Previous studies have demonstrated that DTI parameters, such as fractional anisotropy (FA) and apparent diffusion coefficient (ADC), were significantly correlated with degeneration and regeneration of crushed sciatic nerves in vivo rats and rabbits [14,15,16]. Recently, several studies have demonstrated that a decrease in mean FA values was observed in injured peripheral neuropathy [13, 17,18,19].
To our knowledge, a few previous studies focused on the relationship between diffusion indices and the degree of nerve root compression and most reports lacked of follow-up imaging studies. Furthermore, measuring DTI data was often influenced by many confounding factors, such as multiple lumbar intervertebral disc herniations and degeneration, hyperostosis and osteoporosis. Therefore, young patients and volunteers were selected to eliminate possible interfering factors. The purpose of this study is to investigate the correlation between DTI metrics and the severity of nerve roots compression with symptomatology, and further to assess the changes of diffusion indices for prognostic purposes.
Materials and Methods
Subjects
Approval from the Institutional Review Board and Ethics Committee was obtained prior to the study. Young patients with unilateral LDH who had accepted routine MRI or CT examination were selected as subjects for our study. The exclusion criteria included prior surgical history, spinal trauma and tumor, absence of disc herniation, and contraindication to MRI. Forty young patients (25 males, 15 females; mean age 27.7 ± 5.5 years; age range 18–42 years; 17 cases of L4/5 disc herniation; 23 cases of L5/S1 disc herniation; 26 cases of paracentral LDH; 14 cases of foraminal LDH, n = 80 bilateral nerve roots) who suffered from acute low back pain or unilateral sciatica participated in the study. Seventeen healthy volunteers (10 males, 7 females; mean age 26.1 ± 4.2 years; age range 19–32 years; n = 68 bilateral L4/5 and L5/S1 nerve roots) served as control subjects. Low back and leg pain scores in patients were recorded by using the clinical visual analogue scale (VAS). Seven cases did not undergo follow-up MRI examination. Of them three patients had undergone surgery so that the pedicle screw artifact would obviously influence the image quality and other four cases refused to take DTI examination for financial reasons. Thus, only 33 patients received follow-up DTI examination one month after conservative treatment (drug therapy, sleeping on a hard bed, rehabilitation exercise).
The degree of nerve root compression based on the relationship between disc herniation and nerve root on axial three-dimensional T2-weighed (3D-T2W) image was divided into two groups [20]: (1) mild compression group (n = 23): contact with the disc material deforms the nerve but with a displacement of less than 2 mm. There was mild foraminal or lateral recess stenosis. (2) Severe compression group (n = 17): contact with the disc material displaces the nerve by 2 mm or more. The nerve root is compressed or obscured by the disc protrusion, and the interspace of intervertebral foramen or lateral recess showed moderate or severe stenosis.
MR Acquisition
All patients and volunteers underwent 3.0 T magnetic resonance (MR) examination (Magnetom Verio, Siemens, Germany) in the supine position with the head first and arms alongside the body. A TIM surface coil was used to cover the pelvis and lower abdomen in all imaging instances. Sagittal T1-weighted (TR/TE, 650/9.8 ms) and sagittal T2-weighted (TR/TE, 3000/101 ms) fast spin-echo sequences were obtained with a 320 × 224 matrix, 300 × 100 mm field of view (FOV) and 3.5/0.4 mm section thickness/gap. The 3D anatomical axial or coronal T2-weighted sequences were obtained with TR/TE: 30/12 ms, 228 × 256 matrix, 240 × 100 mm FOV, and 2/0 mm section thickness/gap. The anatomical axial T2 and DTI images were then merged.
DTI Protocol
DTI was performed on the axial plane with a single-shot spin-echo diffusion-weighted echo-planar imaging (SS SE-EPI) sequence with a b-value of 700 s/mm2 and 20 different diffusion gradient orientations. The acquisition parameters were as follows: 11,600 and 88 ms for TR and TE, respectively; axial section orientation of 2.5; 1 mm section thickness/gap; 240 × 100 mm FOV; 128 × 128 matrix; 1.9 × 1.8 × 2.5 mm3 voxel size; two averages; 80 total sections; and 8 min 35 s scan time.
Data Processing and Analysis
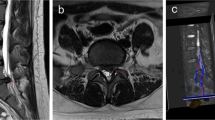
Neuro 3D imaging workstation (Syngo Multimodality Workplace, Siemens Healthcare; software version B17_43.1_1.0) was utilized for DTI data postprocessing. The DTI tensor was fused with the 3D-T2 anatomical image. The region of interest (ROI) of seeding points was placed on the dorsal root ganglion (DRG) of the L5 and S1 nerve roots and similarly on the contralateral side as shown in FA images (Fig. 1). FA, ADC and TraceW values were measured in both proximal L5 and S1 nerve roots ROIs in healthy volunteers and patients. The measurements of all DTI data and tractography of lumbosacral nerve roots were repeated twice by two trained radiologists. The size of ROIs ranged from 25 mm2 to 50 mm2 in the respective nerve roots to avoid partial volume effects. The diffusion tractography properties were as follows: FA threshold = 0.2, angle threshold = 30°, tube radius = 0.85, and diffusion tracts longer than 10 mm.
The spinal nerve MIP figure clearly displayed the bilateral dorsal root ganglion (DRG) on the left side in a 28-year-old male volunteer. Coronal and axial FA maps can clearly show the bilateral L5 nerve roots on the right side; regions of interest (ROIs) were placed on the level of L5 DRG (yellow arrow)
Statistical Analysis
Statistical analyses were performed with SPSS 17.0 software (SPSS Inc., Chicago, IL, USA). The descriptive statistics of all variables were expressed as means ± standard deviation (SD). The Shapiro–Wilk test was performed to test the normality of data distribution. Comparisons of DTI parameters between volunteers and patients were performed by an independent samples t‑test, while a paired samples t‑test was performed between the affected and contralateral sides in patients and between the right and left sides in volunteers. The diagnostic performance of diffusion parameters were assessed using receiver operating characteristic (ROC) curve analysis with Medcalc version 15.6 (MedCalc Software, Mariakerke, Belgium). The optimal cut-off values were determined depending on Youden index and comparisons of DTI metrics using area under the ROC curve (AUC) were performed by the binomial exact test. A two-tailed P < 0.05 was considered statistically significant.
Results
DTI Metrics and DTT in Healthy Volunteers and Patients
The mean FA, ADC and TraceW values (mean ± SD) of the L5 and S1 nerve roots in 17 volunteers and 40 patients are shown in Table 1. In healthy volunteers, the mean FA, ADC and TraceW values of the 68 proximal nerve roots (bilateral L5 and S1 nerve roots, n = 68) in all 17 volunteers were 0.397 ± 0.074, 1.484 ± 0.256 and 0.062 ± 0.04, respectively. No significant differences were found in DTI metrics between left and right nerve roots in volunteers at the same level (P > 0.05). In patients, the mean FA value of the affected side was significantly lower than that of the contralateral roots (P < 0.001) and the corresponding volunteers (P < 0.001). While the mean ADC and TraceW values were significantly higher in the affected nerve roots compared with the contralateral side (ADC, P < 0.01; TraceW, P = 0.025) and the volunteers (ADC, P < 0.001; TraceW, P = 0.046).
The bilateral L4–S1 nerves in 15 volunteers and 35 patients (87.7%, tracking failure in 7 cases) were successfully tracked on postprocessing workstation using DTT. The fiber tractography vividly showed L4–S1 nerves symmetrically coursed downward to enter the lumbosacral plexus (Fig. 2). In 35 patients, the abnormal descriptions (distortion, rarefaction or disruption) of the compressed nerve roots at the level of intervertebral disc herniation are illustrated in Table 2 and Fig. 3. The incidence rate of nerve fibers disruption in severe compression group (50%, 7/14) was higher than that in mild compression group (19%, 4/21).
a, b A 24-year-old man with slight lower limb numbness. The three-dimensional T2-weighted (3D-T2W) image clearly showed a mild compression in the left S1 nerve root (a). Diffusion tensor tractography (DTT) illustrated that the bilateral S1 nerve roots were normal (b). c, d A 31-year-old woman with left leg radiation pain. The 3D-T2W image showed a crush and narrowing in the left S1 nerve root by L5/S1 disc posterolateral protrusion (c). DTT illustrated that the compressed S1 nerve root presented rarefaction and narrowing compared with the contralateral side (d). e, f A 27-year-old man with low back pain and sciatica. The 3D-T2W image showed that the left L5 nerve root was submerged with dural sac compression (e). The entrapped nerve roots showed disruption and rarefaction at the level of intervertebral disc herniation by tractography (red arrow) (f)
Performance Analyses of DTI Metrics
According to ROC curve analyses, the performance analyses of DTI metrics for detecting nerve roots damage in total subjects are illustrated in Table 3. Fig. 4 illustrates that the AUC of FA (0.973) was significantly greater than those of ADC (0.754) and TraceW (0.686) (p < 0.001). No significant difference was observed in AUCs between ADC and TraceW (p = 0.34). The sensitivity and specificity of FA value (90%, 91.2%) were higher than those of ADC (80%, 61.8%) and TraceW (85%, 50%) values in performance evaluation of the compressed nerve roots.
Correlations Among DTI Metrics, Compression Severity and VAS Scores
Fig. 5 illustrates the correlations among DTI metrics, compression severity and VAS scores. Spearman correlation analysis indicated that compression severity of nerve roots had a moderately negative correlation with FA (r = −0.646, P < 0.01; Fig. 5a) and a positive correlation with ADC (r = 0.408, P < 0.01; Fig. 5c) but no correlation with TraceW (r = 0.298, P = 0.06; Fig. 5e). Pearson correlation analyses showed that VAS scores in patients correlated weakly with FA (r = −0.327, P = 0.04; Fig. 5b) and ADC (r = 0.345, P = 0.03; Fig. 5d) but not with TraceW (r = 0.177, P = 0.27; Fig. 5f).
The compression severity had a moderately negative correlation with FA (r = −0.646, P < 0.01) and positive correlation with ADC (r = 0.408, P < 0.01) but not with TraceW (r = 0.298, P = 0.06) (a, c, e). The visual analogue scale (VAS) scores in patients correlated weakly with FA (r = −0.327, P = 0.04) and ADC (r = 0.345, P = 0.03) but not with TraceW (r = 0.177, P =0.27) (b, d, f)
In all 33 cases with follow-up study of one month, the diffusion parameters of the affected side illustrated an increased FA value (0.286 ± 0.06, P = 0.036; Fig. 6a), decreased ADC value (1.630 ± 0.046, P = 0.01; Fig. 6b) and no significant difference in TraceW value (0.069 ± 0.022, P = 0.234; Fig. 6c) compared with those before treatment. However, FA values (14 cases; 0.246 ± 0.015, p = 0.213) in the severe compression group had no significant changes compared with those before conservative treatment.
a–c The diffusion parameters in all 33 patients with follow-up study showed an increased FA value (0.286 ± 0.06, P = 0.036), decreased ADC value (1.630 ± 0.046, P = 0.01) and no significant difference in TraceW value (0.069 ± 0.022, P = 0.234) compared with those in 40 patients before conservative treatment
Discussion
Lumbosacral nerve root compression by LDH can induce a series of clinical symptoms, such as ischialgia, lower limb radiating pain, and sensory disorder, which seriously affect patients’ life and work [21]. At present, DTI is more likely to reflect the microstructural changes of the nerve root compression, and DTT is more suitable to visualize the abnormalities of nerve fiber injury at the level of intervertebral disc herniation compared to conventional MRI [7, 14, 19, 22].
Our study demonstrates that when using tractography, the risk of nerve fiber disruption is proportional to the degree of compression. Compared to contralateral and healthy nerve roots, the affected nerve roots showed a significant decrease in mean FA values and an increase in mean ADC and TraceW values, which was consistent with previous articles from the literature [6, 18, 23].
When spinal nerve roots suffer from persistent compression, the integrity of myelin structure and axonal membrane barrier will be damaged by the ischemia, edema and demyelination, which increase diffusion isotropy of water molecules leading to a decrease in the FA value along the nerve fibers [23, 24]. Animal models of sciatic nerve injury have demonstrated that FA and ADC values correlated with histological and functional microstructural changes (i. e., demyelination, low axonal density and enlarged extracellular space) [16, 25, 26]. Moreover, ADC value mainly reflects the diffusion ability of water molecules in tissues [11, 12]. Mechanical compression and chemical inflammation of the spinal nerve roots can induce intraneural edema, axon swelling, myelinolysis and dilated intercellular space, increasing diffusion ability of intraneural and extraneural water molecules resulting in a high ADC value in fiber tissues [6, 18, 27]. TraceW value is used to describe the diffusion trajectory of water molecules in nerve tissue [28]. Our findings indicated that the TraceW values had a lower diagnostic efficiency in evaluating nerve roots injury compared to the FA and ADC values.
However, due to various factors (i. e., magnetic intensity, scanning parameters, motion and chemical shift artifacts and ROI differences), the differences of the results in DTI metrics were frequently reported in previous studies [13, 23, 28,29,30]. One previous study [18] found a significant decrease in FA (0.186) and an increase in ADC (0.986) in the compressed L5 or S1 nerve roots with unilateral sciatica at 1.5 T, which were different from those (FA, 0.259; ADC, 1.79) obtained in our study. Another MRI study indicated that a lower signal-to-noise ratio (SNR) at 1.5 T might increase the measurement deviations in FA and ADC values [29]. Shi et al. [23] even found that FA values show a decreasing trend from proximal to distal in symptomatic nerve roots, which indicated that differences might exist in data measurement when scanning parameters or placement of ROIs are different. Eguchi et al. [22] reported that mean FA value was significantly lower in the entrapped roots than in the intact side, but FA values of proximal nerves were lower than those of distal nerves in 8 patients with lumbar foraminal stenosis. Moreover, a study showed that automatic techniques have a higher repeatability and sensibility for detecting research indexes on cervical spinal cords than ROI-based segmentation [31]. Therefore, there were some controversies regarding DTI metrics in evaluating microstructural changes of the compressed nerve roots. A study reported that there was no significant difference in ADC values between the affected nerve roots and the contralateral side [27]. Sakai et al. [32] thought that FA and ADC values of the compressed nerve roots in asymptomatic patients, without edema, demyelination degeneration or radicular neuritis, might have no significant changes. The sensitivity and specificity of the FA value were higher than that of ADC value for detecting abnormalities in acute spinal cord injury [33]. Our study also found that FA had a better diagnostic performance compared with ADC and TraceW in dealing with lumbosacral radiculopathy. However, another study suggested that ADC values seemed more reliable than FA values for DTI-derived parameters evaluation [13].
Previous studies have suggested that DTI was able to assess the degeneration and regeneration in peripheral neuropathy [14, 17, 25]. Dallaudiere et al. [34] found that FA and MD values appeared to be correlated with clinical symptoms, independent of age, nerve root segment and visible anatomical discoradicular conflict on MRI. A recent study showed that the Oswestry Disability Index (ODI) scores and symptom duration in patients with LDH had a significant negative association with FA values and a positive correlation with ADC values in the compressed nerve roots [27]. In our study, FA and ADC had a significant correlation with the degree of nerve roots compression, but a weak correlation with VAS scores, which is consistent with other studies [22, 34]. A month later following conservative treatment, some severely compressed nerve roots still showed lower FA values, although their clinical symptoms improved. However, some mildly compressed nerve roots presented the recovery of DTI parameters after conservative treatment. Thus, a patient with nerve compression syndromes can receive timely surgical treatment to remove pressure, which is helpful for functional and histological recovery of the injured nerve. Identifying lesions early will permit for more effective treatment.
Our study has several limitations. First, the study sample is small; thus some experimental error may influence the results. Second, DTI parameters measurement is possibly influenced by the partial volume effects, motion and chemical shift artifacts and artificial postprocessing because of different manipulators. Budzik et al. [35] reported that the quality of DTI images became much better with reduced FOV (rFOV: 100 × 53 mm) than that with full FOV (fFOV: 200 × 200 mm) due to a drastic reduction of the susceptibility and chemical shift artifacts. Finally, manual fiber tracking may cause a false appearance of nerve fiber loss because many small nerve branches and fibers cross intricately, although DTT can visualize the courses of fiber bundles.
Conclusions
In our study, it can be concluded that DTI metrics are able to indirectly reflect microstructural changes of the compressed nerve roots. DTT can visualize the abnormalities of fiber bundles at the location of nerve compression, providing vivid anatomic information. The mean FA, ADC and TraceW values of the affected nerve roots showed significant differences compared with normal nerve roots. The FA value was more reliable than ADC and TraceW values for the evaluation of lumbosacral radiculopathy. DTI metrics especially the FA value possess potentially practical value for prognostic evaluation after treatment.
References
Zhang YG, Sun Z, Zhang Z, Liu J, Guo X. Risk factors for lumbar intervertebral disc herniation in Chinese population: a case-control study. Spine (Phila Pa 1976). 2009;34:E918–E922.
Schoenfeld AJ, Weiner BK. Treatment of lumbar disc herniation: evidence-based practice. Int J Gen Med. 2010;3:209–14.
Michopoulou SK, Costaridou L, Panagiotopoulos E, Speller R, Panayiotakis G, Todd-Pokropek A. Atlas-based segmentation of degenerated lumbar intervertebral discs from MR images of the spine. IEEE Trans Biomed Eng. 2009;56:2225–2231.
Menezes-Reis R, Salmon CE, Carvalho CS, Bonugli GP, Chung CB, Nogueira-Barbosa MH. T1ρ and T2 mapping of the intervertebral disk: comparison of different methods of segmentation. AJNR Am J Neuroradiol. 2015;36:606–611.
Landman BA, Bogovic JA, Wan H, El Zahraa ElShahaby F, Bazin PL, Prince JL. Resolution of crossing fibers with constrained compressed sensing using diffusion tensor MRI. Neuroimage. 2012;59:2175–2186.
Chuanting L, Qingzheng W, Wenfeng X, Yiyi H, Bin Z. 3.0 T MRI tractography of lumbar nerve roots in disc herniation. Acta Radiol. 2014;55:969–975.
Mürtz P, Kaschner M, Lakghomi A, Gieseke J, Willinek WA, Schild HH, Thomas D. Diffusion-weighted MR neurography of the brachial and lumbosacral plexus: 3.0 T versus 1.5 T imaging. Eur J Radiol. 2015;84:696–702.
Arana E, Royuela A, Kovacs FM, Estremera A, Sarasíbar H, Amengual G, Galarraga I, Martínez C, Muriel A, Abraira V, Gil Del Real MT, Zamora J, Campillo C. Lumbar spine: agreement in the interpretation of 1.5-T MR images by using the Nordic Modic Consensus Group classification form. Radiology. 2010;254:809–817.
Pierpaoli C, Jezzard P, Basser PJ, Barnett A, Di Chiro G. Diffusion tensor MR imaging of the human brain. Radiology. 1996;201:637–648.
Le Bihan D, Mangin JF, Poupon C, Clark CA, Pappata S, Molko N, Chabriat H. Diffusion tensor imaging: concepts and applications. J Magn Reson Imaging. 2001;13:534–546.
Tournier JD, Mori S, Leemans A. Diffusion tensor imaging and beyond. Magn Reson Med. 2011;65:1532–56.
Mori S, Zhang J. Principles of diffusion tensor imaging and its applications to basic neuroscience research. Neuron. 2006;51:527–39.
Tagliafico A, Calabrese M, Puntoni M, Pace D, Baio G, Neumaier CE, Martinoli C. Brachial plexus MR imaging: accuracy and reproducibility of DTI-derived measurements and fibre tractography at 3.0-T. Eur Radiol. 2011;21:1764–1771.
Sta M, Cappaert NL, Ramekers D, Baas F, Wadman WJ. The functional and morphological characteristics of sciatic nerve degeneration and regeneration after crush injury in rats. J Neurosci Methods. 2014;222:189–198.
Sun C, Hou Z, Hong G, Wan Q, Li X. In vivo evaluation of sciatic nerve crush injury using diffusion tensor imaging: correlation with nerve function and histology. J Comput Assist Tomogr. 2014;38:790–796.
Yamasaki T, Fujiwara H, Oda R, Mikami Y, Ikeda T, Nagae M, Shirai T, Morisaki S, Ikoma K, Masugi-Tokita M, Yamada K, Kawata M, Kubo T. In vivo evaluation of rabbit sciatic nerve regeneration with diffusion tensor imaging (DTI): correlations with histology and behavior. Magn Reson Imaging. 2015;33:95–101.
Khalil C, Hancart C, Le Thuc V, Chantelot C, Chechin D, Cotten A. Diffusion tensor imaging and tractography of the median nerve in carpal tunnel syndrome: preliminary results. Eur Radiol. 2008;18:2283–2291.
Balbi V, Budzik JF, Duhamel A, Bera-Louville A, Le Thuc V, Cotten A. Tractography of lumbar nerve roots: initial results. Eur Radiol. 2011;21:1153–1159.
Chhabra A, Thakkar RS, Andreisek G, Chalian M, Belzberg AJ, Blakeley J, Hoke A, Thawait GK, Eng J, Carrino JA. Anatomic MR imaging and functional diffusion tensor imaging of peripheral nerve tumors and tumorlike conditions. AJNR Am J Neuroradiol. 2013;34:802–807.
Beattie PF, Meyers SP, Stratford P, Millard RW, Hollenberg GM. Associations between patient report of symptoms and anatomic impairment visible on lumbar magnetic resonance imaging. Spine. 2000;25:819–828.
Weber H. Lumbar disc herniation: a controlled, prospective study with ten years of observation. SAS J. 2009;3:30–40.
Eguchi Y, Ohtori S, Orita S, Kamoda H, Arai G, Ishikawa T, Miyagi M, Inoue G, Suzuki M, Masuda Y, Andou H, Takaso M, Aoki Y, Toyone T, Watanabe A, Takahashi K. Quantitative evaluation and visualization of lumbar foraminal nerve root entrapment by using diffusion tensor imaging: preliminary results. AJNR Am J Neuroradiol. 2011;32:1824–1829.
Shi Y, Zong M, Xu X, Zou Y, Feng Y, Liu W, Wang C, Wang D. Diffusion tensor imaging with quantitative evaluation and fiber tractography of lumbar nerve roots in sciatica. Eur J Radiol. 2015;84:690–695.
Zhang J, Jones M, DeBoy CA, Reich DS, Farrell JA, Hoffman PN, Griffin JW, Sheikh KA, Miller MI, Mori S, Calabresi PA. Diffusion tensor magnetic resonance imaging of Wallerian degeneration in rat spinal cord after dorsal root axotomy. J Neurosci. 2009;29:3160–3171.
Lehmann HC, Zhang J, Mori S, Sheikh KA. Diffusion tensor imaging to assess axonal regeneration in peripheral nerves. Exp Neurol. 2010;223:238–244.
Li X, Chen J, Hong G, Sun C, Wu X, Peng MJ, Zeng G. In vivo DTI longitudinal measurements of acute sciatic nerve traction injury and the association with pathological and functional changes. Eur J Radiol. 2013;82:e707–e714.
Wu W, Liang J, Ru N, Zhou C, Chen J, Wu Y, Yang Z. Microstructural changes in compressed nerve roots are consistent with clinical symptoms and symptom duration in patients with lumbar disc herniation. Spine (Phila Pa 1976). 2016;41:E661–E666.
Pfefferbaum A, Adalsteinsson E, Sullivan EV. Replicability of diffusion tensor imaging measurements of fractional anisotropy and trace in brain. J Magn Reson Imaging. 2003;18:427–33.
Landman BA, Farrell JA, Jones CK, Smith SA, Prince JL, Mori S. Effects of signal-to-noise ratio on the accuracy and reproducibility of diffusion tensor imaging derived fractional anisotropy, mean diffusivity, and principal eigenvector measurements at 1.5 T. J Magn Reson Imaging. 2007;26:756–767.
Chen YY, Lin XF, Zhang F, Zhang X, Hu HJ, Wang DY, Lu LJ, Shen J. Diffusion tensor imaging of symptomatic nerve roots in patients with cervical disc herniation. Acad Radiol. 2014;21:338–344.
Van Hecke W, Leemans A, Sijbers J, Vandervliet E, Van Goethem J, Parizel PM. A tracking-based diffusion tensor imaging segmentation method for the detection of diffusion related changes of the cervical spinal cord with aging. J Magn Reson Imaging. 2008;27:978–991.
Sakai T, Miyagi R, Yamabe E, Fujinaga Y, N Bhatia N, Yoshioka H. Diffusion-weighted imaging and diffusion tensor imaging of asymptomatic lumbar disc herniation. J Med Invest. 2014;61:197–203.
Facon D, Ozanne A, Fillard P, Lepeintre JF, Tournoux-Facon C, Ducreux D. MR diffusion tensor imaging and fiber tracking in spinal cord compression. AJNR Am J Neuroradiol. 2005;26:1587–1594.
Dallaudière B, Lincot J, Hess A, Balbi V, Cornelis F, Larbi A, Laissy JP, Cotten A, Schouman-Claeys E. Clinical relevance of diffusion tensor imaging parameters in lumbar disco-radicular conflict. Diagn Interv Imaging. 2014;95:63–68.
Budzik JF, Verclytte S, Lefebvre G, Monnet A, Forzy G, Cotten A. Assessment of reduced field of view in diffusion tensor imaging of the lumbar nerve roots at 3 T. Eur Radiol. 2013;23:1361–1366.
Funding
This study was supported by grants from the National Natural Science Foundation of China (81371517) and from Clinical science and technology innovation project of Shanghai Shen Kang Hospital Development Center (SHDC22015026, 16CR4029A).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Zhang, F. Zhang, F. Xiao, Z. Xiong, D. Liu, T. Hua, N. Indima and G. Tang declare that they have no competing interests.
Additional information
Jiulong Zhang and Feng Zhang contributed equally to this study and should be considered co-first authors.
Rights and permissions
About this article
Cite this article
Zhang, J., Zhang, F., Xiao, F. et al. Quantitative Evaluation of the Compressed L5 and S1 Nerve Roots in Unilateral Lumbar Disc Herniation by Using Diffusion Tensor Imaging. Clin Neuroradiol 28, 529–537 (2018). https://doi.org/10.1007/s00062-017-0621-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-017-0621-9