Abstract
Introduction
In October 2011, a 72-year-old man was referred from a peripheral hospital with subsequent diagnosis: fungal sepsis with suspicion for endocarditis of a bioprosthetic aortic heart valve. In May 2010, a bioprosthetic aortic valve implantation (Edwards Magna) and CABG (LIMA graft on LAD) were performed.
Case
At the time of admission, the patient was in good general condition; the physical examination was unremarkable. Hemoculture detected Streptococci thermophilus and Candida parapsilosis. Neither an oscillating intracardiac mass on the valve nor an abscess could be detected in several transesophageal echocardiographies (TEEs). The F18-FDG PET-CT showed an increased tracer uptake in the area of the prosthetic aortic valve. The findings argued for a fungal endocarditis of the prosthetic aortic valve.
Heart surgeons refrained from implantation of a new prosthetic aortic valve because of the unfavorable prognosis. Therefore, highdose i.v. therapy with liposomale amphotericin B (5 mg/kg BW) and voriconazol (4 mg/kg BW twice a day) was started. A new F18-FDG PET-CT after 2 weeks showed no tracer uptake in the area of the prosthetic aortic valve. The hemoculture was also negative. The patient recovered; CRP values were within normal limits. Life-long antifungal therapy with fluconazol (400 mg/day) was recommended.
Conclusion
There are no definitive treatment recommendations for fungal endocarditis. Surgical therapy is the first choice in prosthetic valve endocarditis, which however cannot be performed in all patients. In these cases high dose and life-long medical therapy is necessary to prevent re-infection of the valve, even if (transient) deterioration of renal and liver function occurs.
Zusammenfassung
Einleitung
Im Oktober 2011 wurde ein 72-jähriger Mann mit Pilzsepsis und Verdacht auf Endokarditis mit Beteiligung der biologischen Aortenklappenprothese von einem peripheren Spital an das Uniklinikum Graz transferiert. Im Mai 2010 erhielt der Patient eine biologische Aortenklappenprothese (Edwards Magna) und einen aortokoronaren Bypass (LIMA-Graft auf LAD).
Fall
Bei der Ankunft in der klinischen Abteilung für Kardiologie präsentierte sich der Patient in einem guten Allgemeinzustand. Die physikalische Untersuchung war unauffällig. Mehrere transösophageale Echokardiographien (TEEs) ergaben weder einen Hinweis auf oszillierende Klappenauflagerungen noch auf intrakardiale Abszesse. Eine F18-FDG-PET-CT-Untersuchung detektierte einen gesteigerten Tracer-Uptake im Bereich der Aortenklappenprothese. Die vorliegenden Befunde erhärteten den Verdacht auf Pilzendokarditis mit Beteiligung der Aortenklappenprothese.
Experten der Herzchirurgie nahmen Abstand von einer Reoperation mit Neuimplantation einer Aortenklappenprothese. Man entschied sich für die Einleitung einer i.v.-Therapie mit Amphotericin B (5 mg/kg Körpergewicht) und Voriconazol (4 mg/kg KG 2-mal/Tag). In einem weiteren Kontroll-F18-FDG-PET-CT nach 2 Wochen konnte kein pathologischer Tracer-Uptake im Bereich der Aortenklappenprothese mehr nachgewiesen werden. Auch die abschließende Blutkultur war negativ, die CRP-Werte lagen im Normbereich. Eine lebenslange antifungale Therapie mit Fluconazol (400 mg/Tag) wurde empfohlen.
Fazit
Es gibt keine definitiven Therapieempfehlungen für Pilzendokarditiden. Als Mittel der Wahl gilt eine chirurgische Therapie, welche allerdings nicht in jedem Fall durchgeführt werden kann. Hier ist eine hochdosierte lebenslange medikamentöse Therapie nötig, um eine Reinfektion der Klappe zu verhindern, auch wenn (vorübergehend) eine Verschlechterung der Nieren- und Leberfunktion auftritt.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
In October 2011, a 72-year-old man was referred from a peripheral hospital to the Medical University of Graz for further investigations with diagnosis of fungal sepsis and suspicion of endocarditis of a bioprosthetic aortic heart valve. Already in late August, the patient was hospitalized there for evaluation of fever (38.5 °C), fatigue, and exhaustion after vacation in Italy.
On 19 May 2010, the patient received a bioprosthetic aortic valve implantation (Edwards Magna) and CABG (LIMA graft on LAD). A month later the patient developed a retrosternal abscess with septic spreading to the hip joint. At this point, the patient was in a reduced general condition with massive increased inflammatory values, dyspnea, and severe pain in his left hip joint. After a resternotomy with sternum left open the patient was transferred to the ICU. In the same session, the trochanteric bursitis was infiltrated by orthopedic surgeons with the local anesthetic ropivacaine (Naropin®). C. parapsilosis was detectable in sputum and urine on 26 July 2010 for the first time. Sepsis led to an acute liver failure with elevation of liver enzymes and an increase of bilirubin up to 25 µmol/l. MARS therapy was evaluated but not indicated by the department of hepatology. ICU therapy and catecholamine support stabilized the patient’s condition and the sternum was closed. Thereafter, echocardiography showed left ventricular hypertrophy, an EF of 65%, aortic valve replacement with regular function, MINS 0-I, TRINS 0-I, no vegetation or effusion. In the further course liver laboratory parameters, bilirubin, and inflammatory markers decreased and the patient recovered without limitations.
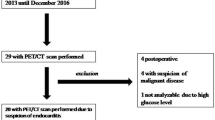
At the time of admission, the patient was in good general condition and the physical examination was inconspicuous. Blood analysis offered anemia (Hb 12.3 g/dl, RBC 4.74 T/l, MCV 81 fl, MCH 25.9 pg), altered liver and renal function (BUN 51 mg/dl; GFR 64.28 ml/min, AST 54 U/l GGT 296 U/l), and CRP was slightly increased (23.9 mg/dl). Resting ECG showed an atrial fibrillation with a ventricular rate of 72/min, left type QRS 158 ms, complete right bundle-branch block, negative T in V1, otherwise nonspecific repolarization disturbance. Former blood culture detected streptococci thermophiles (31 August 2011) and candida parapsilosis (31 August 2011; 12, 22, and 26 September 2011; 3 October 2011). Neither an oscillating intracardiac mass on the valve nor an abscess could be detected in several TEEs; however, one major criterium (positive blood culture) and two minor criteria (fever, predisposition) of the modified Duke criteria [1] for infective endocarditis existed. The enforced F18-FDG PET-CT detected an increased tracer uptake in the range of the prosthetic aortic valve (Fig. 1 a). In synopsis, all findings argue for a fungal endocarditis of the prosthetic aortic valve.
a The F18-FDG PET-CT detected a significant pathological tracer-uptake in the range of the prosthetic aortic valve. b The result of the follow up examination was substantially unchanged. c The final F18-FDG PET-CT was unsuspicious; there was no pathological tracer-uptake in the range of the valve detectable
In the peripheral hospital, a therapy with piperacillin/tazobactam and caspofungin was initially started. Caspofungin was adapted to fluconazol 400 mg/day p.o. according to the antifungigram. At our hospital, we had interdisciplinary calls between cardiology, cardiac surgery, radiology/nuclear medicine, and infectiology. Heart surgeons refrained from implantation of a new prosthetic aortic valve because of the unfavorable prognosis due to a very high perioperative risk; therefore, we decided for maximal nonsurgical therapy, only limited by tolerance and severe side effects. Ambisome therapy was decreased from initially 5 mg/kg BW to 3 mg/kg BW because of renal impairment. In addition, voriconazole (Vfend® 6 mg/kg BW twice as starting dose, then 4 mg/kg BW 2 × 1/day i.v.) was started Possible side effects were expected for liver toxicity and vision alterations, or interactions with acenocoumarol. Therefore, acenocoumarol (Sintrom®) was changed to dabigatran (Pradaxa®). For the monitoring of ambisome therapy, a further F18-FDG PET-CT scan was performed. The patient was afebrile. Comparisons with preliminary results showed deterioration. The tracer uptake at the valve was high topographically expanded and stored, conform with a local infection with fungus (Fig. 1 b). Ambisome therapy was continued as before. Two weeks later a control F18-FDG PET-CT scan followed, detecting a significant improvement in results. There was no pathological tracer-uptake in the area of the prosthetic aortic valve. The patient was afebrile and the therapy with ambisome 300 mg (now day 26) and voriconazole 2 × 400 mg i.v. (day 16) were continued. Other blood cultures were negative; ambisome was discontinued. The administered dose of voriconazole 400 mg p.o. 1–0-1 was higher than recommended but justified by the life-threatening condition of the patient (fungal infection of the bioprosthetic aortic valve implantation). The patient was discharged from the hospital.
In an outpatient control 2 weeks after discharge, the patient already felt better. He was afebrile at home and did not feel repulsed. The treatment with voriconazole 200 mg 2–0-2 p.o. was set to continue for another 3 weeks, then changed to fluconazole 200 mg 2–0-0 p.o. as a lifelong suppressive therapy. In a final PET-CT scan, the aortic valve still had no pathological tracer uptake, compared with preliminary scans. The tracer uptake in the whole body was normal (Fig. 1 c). The recent follow up on 23 April 2012 showed renal function within normal limits and slightly elevated liver markers, no changes in medication, a steady body weight, and NYHA class II. A cataract operation is planned in the near future.
In the case presented, the working diagnosis was made using the modified Duke criteria for infective endocarditis. However, the modified form of Duke criteria are not yet validated, and the Duke criteria were originally developed for epidemiological studies. Therefore, clinical findings and imaging (preferably echo/TEE) are recommended. In case of typical clinical signs symptoms and normal echo, further imaging is needed. The used PET imaging is suitable to detect inflammatory sites and to follow up the inflammation.
There is no definite therapy recommended in fungal endocarditis and most knowledge results from case reports. Although surgical therapy is the first choice in prosthetic valve endocarditis [2], this option is not available at reasonable perioperative risk in some patients and rejected by some other patients. Pharmacological therapy mostly consists of dual therapy including amphotericin and azoles. Several cases have presented successful treatment using caspofungin [3, 4], which was not suitable in the presented case due to the antifungigram. Streptococci thermophiles were only detected in a former blood culture performed in the peripheral hospital. An antibiotic therapy with piperacillin and tazobactam eradicated the germ. In our hospital the germ could not be detected in several blood cultures. In conclusion, due to the negative blood cultures and unchanged symptoms a Candida parapsilosis endocarditis was very likely.
In all these cases high dose and life-long pharmacological therapy is necessary to prevent re-infection of the valve even if (transient) deterioration of renal and liver function occurs.
The usefulness of F18-FDG PET-CT in oncology is wide accepted and established [5], whereas the role of the PET-CT in inflammatory disease is challenging, especially in diagnosis of endocarditis and infection of prosthetic valves [6, 7]. Glucose metabolism of the heart is a difficult setting. In fasting nondiabetic patients (6–12 h to overnight) with normal glucose levels, the normal myocardium FDG distribution patterns could be divided in three types: no to faint uptake, regional uptake and diffuse uptake. In cases of diffuse uptake of the heart, a diagnosis of a prosthetic valve infection is hardly possible with F18-FDG. In our case the heart had faint glucose uptake. Therefore, a clear delineation of the fungal endocarditis of a bioprosthetic aortic valve was possible. In the literature, the role of F18-FDG PET-CT in the diagnosis of infective endocarditis is limited and mostly based on cases reports. In one case, infective endocarditis diagnosed by PET-CT was confirmed by positive blood cultures [8]. Another group detected an endocarditis with F18-FDG in a mechanical aortic valve prosthesis. In this case echocardiography was inconclusive because of metal artifacts [9]. Vind et al. [10] reported a detection of endocarditis in two cases, confirmed by blood culture. The advantage of PET/CT and its tracer metabolism is the fact that there are no metal artifacts which is relevant in the presence of mechanical prosthesis [11]. On the other hand, it is important to clarify how many times is necessary after cardiac surgery for valvular disease to consider the repair process finished. If the PET is performed too early after surgery, the repair process may lead to a false-positive result. A BioGlue surgical adhesive, used to repair the aortic root, may also cause a false-positive result in the PET-CT [12]. Thus, further evaluation has to be done to clarify the clinical impact of F18-FDG PET-CT in suspicious endocarditis and prosthetic valves infection.
References
Li JS, Sexton DJ, Mick N et al (2000) Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 30:633–638
Ellis ME, Al-Abdely H, Sandridge A et al (2001) Fungal endocarditis: evidence in the world literature, 1965–1995. Clin Infect Dis 32:50–62
Lye DC, Hughes A, O’Brien D, Athan E (2005) Candida glabrata prosthetic valve endocarditis treated successfully with fluconazole plus caspofungin without surgery: a case report and literature review. Eur J Clin Microbiol Infect Dis 24:753–755
Garzoni C, Nobre VA, Garbino J (2007) Candida parapsilosis endocarditis: a comparative review of the literature. Eur J Clin Microbiol Infect Dis 26:915–926
Hustinx R, Be’nard F, Alavi A (2002) Whole-body FDGPET imaging in the management of patients with cancer. Semin Nucl Med 32:35–46
Flotats A, Knuuti J, Gutberlet M et al (2011) Hybrid cardiac imaging: SPECT/CT and PET/CT. A joint position statement by the European Association of Nuclear Medicine (EANM), the European Society of Cardiac Radiology (ESCR) and the European Council of Nuclear Cardiology (ECNC). Eur J Nucl Med Mol Imaging 38:201–212
Bengel FM, Higuchi T, Javadi MS, Lautama¨ki R (2009) Cardiac positron emission tomography. J Am Coll Cardiol 54:1–15
Yen RF, Chen YC, Wu YW et al (2004) Using 18-fluoro-2-deoxyglucose positron emission tomography in detecting infectious endocarditis/endoarteritis: a preliminary report. Acad Radiol 11:316–321
Moghadam-Kia S, Nawaz A, Millar BC et al (2009) Imaging with F-FDG-PET in infective endocarditis: promising role in difficult diagnosis and treatment monitoring. Hell J Nucl Med 12:165–167
Vind SH, Hess S (2010) Possible role of PET/CT in infective endocarditis. J Nucl Cardiol 17:516–519
Bockisch A, Beyer T, Antoch G et al (2004) Positron emission tomography/computed tomography—imaging protocols, artifacts, and pitfalls. Mol Imaging Biol 6:188–199
Schouten LR, Verberne HJ, Bouma BJ et al (2008) Surgical glue for repair of the aortic root as a possible explanation for increased F-18 FDG uptake. J Nucl Cardiol 15:146–147
Conflict of interest
On behalf of all authors, the corresponding author states that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
M. Wallner and G. Steyer contributed equally to this article.
Rights and permissions
About this article
Cite this article
Wallner, M., Steyer, G., Krause, R. et al. Fungal endocarditis of a bioprosthetic aortic valve. Herz 38, 431–434 (2013). https://doi.org/10.1007/s00059-012-3715-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-012-3715-9